Abstract
Background
Endoscopic retrograde cholangiopancreatography (ERCP) is a frequent procedure in elderly patients.
Aims
We aimed to determine the safety and efficacy of acute ERCP in older patients.
Methods
A prospectively managed, hospital-based registry containing all ERCP procedures and complications at a tertiary referral center was used to form the study population, which consisted of consecutive elderly (≥65 years) patients undergoing acute ERCP during the 5-year study period. Indications, details, outcome, and complications of the procedure were analyzed in relation to patient age, gender, and co-morbidities.
Results
A total of 480 elderly patients (median age 78; range 65–97; 48 % men) underwent 531 ERCPs during the study period. The most common indications were bile duct stones (56.1 %) and biliary obstruction caused by malignancy (33.7 %). Successful stone extraction was achieved in 72.8 %, and with an additional, planned ERCP in 96.6 % of the patients. Post-ERCP complications developed in 3.4 % of the patients. These included pancreatitis in 1.7 %, hemorrhage in 0.6 %, and duodenal perforation in 0.2 % of the patients. One of these (0.2 %) was considered severe as this patient required invasive treatments and prolonged hospital stay. The risk of complications was associated with chronic obstructive pulmonary disease and difficult cannulation. Procedure-related mortality was zero, but overall 30-day mortality was 10 %, being 24 % in the patients with malignancy.
Conclusions
ERCP can be safely and efficaciously performed on elderly patients. The high mortality should be taken into consideration when selecting therapeutic options.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is a routinely used diagnostic and therapeutic technique for biliary and pancreatic diseases. Typical indications, such as biliary obstruction caused by biliary stones or malignancy, are more common in elderly patients [1]. In spite of some decline in the need for ERCP as noninvasive diagnostic methods (such as MRI and endoscopic ultrasonography) might have replaced ERCP in some cases [2], population aging may increase demand as the typical indications become more common.
ERCP remains the riskiest routinely used endoscopic procedure, and elderly patients have depleted resources to recover from any operations, especially if the outcome is complicated. Therefore, the possible benefits and risks need to be carefully assessed for every patient. In terms of performing acute ERCP on elderly patients, little is known about the safety and efficacy. Our aim was to study the role and risk factors for ERCP in elderly patients in a prospective setting in a Finnish tertiary hospital.
Methods
A prospectively managed, hospital-based registry containing all ERCP procedures and complications in Tampere University Hospital (average catchment area during the study period was 496,000 inhabitants, of whom 93,000 elderly people) was used to form the study population. This consisted of all consecutive patients undergoing acute ERCP at the age of over 65 years between January 2010 and December 2014. ERCP was considered acute when it was performed during a period of hospitalization beginning with an acute admission.
The following information was prospectively collected and registered: indication for ERCP, all procedures performed, difficulty of cannulation, outcome of the procedure, post-ERCP complications, and other adverse events. Patients’ medical records were retrieved and reviewed for comorbidities. Cannulation was considered difficult if it either took more than 5 min, if there were more than five cannulation attempts on the papilla, or if the pancreatic duct was cannulated more than twice [3]. The medical director of Tampere University Hospital approved the protocol for the registry.
The primary outcome was incidence of procedure-related complications or death. The secondary outcome was the success of the procedure. The success rate was defined according to achievement of the pre-procedural goal set. ERCP complications (pancreatitis, hemorrhage, cholangitis, and perforation) were defined and classified according to Cotton et al. [4], and were prospectively recorded for 30 days after the procedure. Procedure-related mortality and overall 30-day mortality were extracted from the hospital records and the Population Register Centre.
All the ERCP procedures were performed by experienced endoscopists in this high-volume center. During the study period, five endoscopists performed majority of the operations (85 %), while the total number of ERCPs at the study hospital during the study period was approximately 2000. A single dose of intravenous antibiotics (i.v. cefuroxime 1.5 g; Orion Pharma, Finland) and an anti-inflammatory suppository (diclofenac 100 mg; Voltaren, Novartis, Finland) was administered to all patients before ERCP. Most ERCP procedures were performed under conscious sedation according to the local practice. The patient was sedated with i.v. midazolam (Dormicum, Roche Pharma AG, Germany) together with oxycodone (Oxanest, Takeda, Austria) and monitored by the endoscopy team. Duodenal peristalsis was reduced by administering i.v. hyoscinebutylpromide (20–40 mg; Buscopan, Boehringer Ingelheim, Germany) or i.v. glucagon (0.3 mg; Glucagen, Novo Nordisk, Denmark). Patients were monitored by pulse oximetry, and supplementary oxygen was provided when needed.
All statistical analyses were performed using SPSS Statistics version 22 for Windows (IBM Corp, Armonk, NY, USA. Differences among different patient cohorts were determined by using the Fisher’s exact test for categorical variables, and for non-categorical variables with the Mann–Whitney U test. Variables of potential significance (p value ≤0.10) were entered into a multivariate analysis (logistic regression analysis, enter method). Statistical significance was set at p < 0.05. Multiple statistical comparisons were performed using multivariate logistic regression analysis (binary logistic regression, enter method).
Results
A total of 480 patients underwent 531 ERCPs during the study period. The median age of patients was 78 years (range 65–97) and 48 % of patients were men. Fifty-one patients underwent multiple ERCPs (41 patients underwent two, and five patients three procedures). The most common comorbidities were hypertension (n = 299, 59.3 %), coronary artery disease (n = 114, 21.5 %), atrial fibrillation (n = 114, 21.5 %), and diabetes (n = 132, 24.9 %). Only 106 patients (22.1 %) had no co-existing diseases. The clinical characteristics of patients are summarized in Table 1.
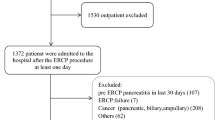
The two most common indications for ERCP were presence or suspicion of bile duct stones (n = 298, 56.1 %) and biliary obstruction caused by malignancy (n = 179, 33.7 %). The most common sites for malignancy were pancreas (n = 101, 56.4 %) and biliary tract (n = 40, 22.3 %). The majority of the malignancies (72.7 %) were inoperable, with the most common reason being advanced disease (86.2 %). Ten percent of the procedures were performed for other indications. These included bile leak after cholecystectomy (n = 22, 4.1 %) and benign biliary strictures (n = 28, 5.3 %). Of patients with bile leak, one had a lateral injury to the common hepatic duct (Strasberg–Bismuth D) and the rest cystic duct leak (Strasberg–Bismuth A). Figure 1 presents the distribution of diagnoses.
The procedures included sphincterotomy (n = 388), balloon extraction (n = 354), and lithotomy (n = 180) as the most common maneuvers. Cannulation was graded difficult in 172 cases, and despite multiple attempts and different techniques, 97 cannulation attempts (18.3 %) eventually failed in the index ERCP. The most common reason for cannulation failure was tumor growth (n = 49, 50.5 %). Procedure-related characteristics are presented in Table 2.
Successful extraction of bile duct stones was achieved in 72.8 % of the patients in the acute index ERCP procedure and with additional scheduled ERCPs in 96.6 % of the patients. Ten patients (3.4 %) required surgical treatment or could not be treated, most often because of poor physiological status. Endoscopic procedure was successful for treating acute malignancy-related jaundice in 59.4 % of patients, while 40.0 % of patients required percutaneous biliary drainage. Among the patients with successful cannulation, a successful release of biliary obstruction was achieved in 83.6 % of cases. Out of these, 16 % later required percutaneous drainage. All the bile leaks were caused by surgery. Endoscopic procedure was sufficient for treating bile leak in 93.8 % of patients. The success remained unproven in one patient who died of sepsis a day after the procedure. However, even with this patient, bile drain output was significantly reduced after the procedure. In three patients, sphincterotomy (with no stenting) was sufficient for treatment. The others were treated with both sphincterotomy and stenting. Procedure-related outcome is presented in Table 3.
Complications occurred in 3.4 % of the patients. The most common complication was pancreatitis (n = 9, 1.7 %). One of these (0.2 %) was severe. The patient was hospitalized for 27 days and required percutaneous drainage of a post-pancreatitis pseudocyst, but was eventually cured. Three patients (0.6 %) had post-ERCP bleeding (all classified as moderate, requiring transfusion of less than 4 units of blood and no invasive treatments). Only one patient (0.2 %) had mild post-ERCP cholangitis. In one case (0.2 %), there was a slight leak of contrast from the CBD during the procedure, but no treatment was required. Cardiopulmonary and sedation-related complications were registered in three patients (0.6 %; allergic reaction to anesthetics in one patient, atrial fibrillation in one patient, and stroke in one patient), and one patient suffered from esophageal perforation (n = 1, 0.2 %; treated with stenting). There were no significant differences in postoperative morbidity in according to patients’ age (Table 4).
Procedure-related mortality was zero. One patient died within the same day after the ERCP, but in the autopsy, no signs of ERCP complication were found; the cause of death (both immediate and underlying cause of death) was malignancy. One-month and 1-year mortality rates were 10.0 % (n = 53) and 33.5 % (n = 178), respectively. There was a significant difference between diagnoses: 1-month mortality of patients with bile duct stones was 2.7 %, compared to 23.5 % in patients with malignancy (p < 0.001). Median survival of patients with malignancy was 170 days (3–1635 days) overall and 144 days (3–1195 days) in patients with inoperable malignancy. Patients with pancreatic malignancy deemed inoperable had a median survival of 121 days (5–997 days, one patient alive). Of the patients with malignancy, 46 (25.7 %) were alive a year after the ERCP. Table 4 presents the prevalence of post-ERCP complications and deaths.
Complications were more common in patients with chronic obstructive pulmonary disease (p = 0.030), postoperative bile leak (p = 0.034) and less common in patients with malignancy-related biliary obstruction (p = 0.006). Complication risk increased also after pancreatic sphincterotomy (p = 0.006) and if the cannulation was considered difficult (p = 0.003). In multivariate analysis (binary logistic regression analysis, enter method), chronic obstructive pulmonary disease (p = 0.041, OR 5.1, 95 % CI 1.1–24) and difficult cannulation (p = 0.045, OR 5.1, 95 % CI 1.0–25) were found to be independent risk factors for post-ERCP complications (Table 5).
Discussion
No prospective results of ERCP performed in acute circumstances in the elderly have so far been reported. In this study, a prospective hospital database was used to analyze the outcome of ERCPs performed on elderly patients after acute admission. We found that procedure-related complications were rare; ERCP was in most cases performed safely and efficaciously. Chronic obstructive pulmonary disease and difficult cannulation were independent risk factors for post-ERCP complications in this patient population. Procedure-related mortality was zero, but overall 30-day mortality was 10 %, being 24 % in the patients with malignancies.
The need for ERCP is heavily age dependent. The two typical indications, biliary obstruction caused by either bile duct stones or malignancy, accounted 90 % of all procedures performed in our series. As stated before, both indications increase with age [1]. In our study approximately 115 per 100,000 elderly inhabitants (aged 65 years or more) required acute ERCP each year. According to Statistics Finland, during the study period, the proportion of elderly people in our district rose from 17.5 to 19.8 % (+14,058 elderly inhabitants). This change is not only a characteristic of our district but also is a global trend [5]. Although there has been some decrease in the need for ERCP as noninvasive diagnostic methods, such as MRI and endoscopic ultrasonography, have replaced ERCP as a diagnostic procedure [2], there will presumably be an increase in the need for therapeutic and acute ERCPs in the future as the older population grows.
In our study, all the ERCPs were performed in an acute setting, meaning that patients were admitted to hospital from the emergency room. In this setting, ERCP seems to be safe in the elderly, and even safer than reported in earlier studies: post-ERCP complications developed in 3.4 % of the patients. An earlier meta-analysis of 21 prospective studies (also including non-acute procedures) reported 6.9 % morbidity in all adult patients [6], while prior studies on the elderly have reported 2.5–8.4 % morbidity rates [7–14]. As shown before, in our study, pancreatitis was the most common complication (1.7 %) [15]. According to a systematic review of post-ERCP complications in the elderly [16] the risk of post-ERCP pancreatitis ranges from 1.2 to 1.8 % depending on patient’s age. In our data, the outcome was similar regardless of age; very old patients (aged 80 years or more) had similar outcomes than elderly patients (aged 65–79 years). It has been suggested that elderly people are at lower risk of post-ERCP pancreatitis than their younger counterparts, but at a similar risk of other complications. In contrast to this, in our study, all the typical complications (hemorrhage in 0.6 % and duodenal perforation in 0.2 %) were also less common than previously reported [17].
Interestingly, there were no deaths directly associated with the procedure. Earlier studies on the elderly have reported similar, but somewhat poorer outcomes, with procedure-related mortality varying from 0.6 to 1.6 % [7–9]. Despite the zero ERCP-related mortality, 10 % of the patients in our study died within 1 month of the procedure. Not surprisingly, the mortality was highest in patients with malignancy and lowest in patients with bile duct stones. Regardless of this, mortality was higher among patients with bile duct stones than among elderly Finns on average. When compared to annual reports by Statistics Finland, these patients were two to six times more likely to die within 1 year than their elderly counterparts. The significance of bile duct stone disease is debatable as there was also a high incidence of comorbidities, such as diabetes and coronary artery disease, which may explain the higher mortality in the study group.
We identified risk factors for complicated outcome. Difficult cannulation increased the risk of post-ERCP complications, as shown before [17–19]. In our study, the risk of pancreatitis was almost sevenfold (4.1 vs. 0.6 %) in patients with whom cannulation was difficult. The same was evident in other complications. Only two patients with non-difficult cannulation had subsequent complications. It should be noted that there is no globally accepted definition of difficult cannulation. In this study, we used the definition of the Scandinavian Association for Digestive Endoscopy, which includes time, cannulation attempts and pancreatic guidewire passages [3]. Complications were also more common in patients with chronic obstructive pulmonary disease.
In our study, ERCP was an excellent therapeutic procedure for treating acute biliary obstruction in the elderly. Most of the bile duct stones were retrievable in the index operation. For patients undergoing difficult procedures and with unretrievable stones, we recommend a safer approach using temporary stenting and delayed elective endoscopic stone removal. Seventy percent of the remaining stones were removable in secondary ERCP in our series, and 96.6 % of stones were removable with ERCP.
In patients with malignancy-related biliary obstruction, endoscopic stenting, if successful, provided effective long-term palliation. However, in this study, failure seemed to be surprisingly common. In most cases, cannulation failed because of tumor growth (in some cases only EGD was performed). In case of successful ERCP, several guidelines recommend using plastic stents in patients with short life expectancy and self-expanding metal stents in patients with longer life expectancy or poor physiological status contraindicating surgical treatment [20]. The main advantage of plastic stents has been considered to be their low cost. On the other hand, a recent study by Walter et al. [21] stated that higher initial costs of self-expanding metal stents are covered by longer functional time. Therefore, they concluded that self-expanding metal stents should be used for palliation in all patients, regardless of estimated survival. Further studies or updates to existing guidelines on this subject are needed. In contrast to metastatic disease, in patients with operable malignancy, there is a broad consensus that the possible risks and benefits in placing the stent should be carefully assessed, as ERCP and its possible post-procedural complications should not delay the imminent surgery [20, 22].
ERCP was moreover an excellent procedure for the treatment of cystic duct leakage in elderly patients. In one patient, the success of the procedure was undeterminable, but the rest healed after the ERCP procedure. Elderly patients have not been studied before in this regard. However, similar results have been reported in earlier studies focusing on all patients undergoing ERCP due to postoperative bile leak [23, 24]. According to the Guidelines by the European Society of Gastrointestinal Surgery, ERCP should be attempted if no transection of the CBD exists [20]. The guidelines recommend using a plastic stent without sphincterotomy or sphincterotomy alone in selected patients. During the procedure, associated lesions and obstacles should also be detected and treated. The stent should be removed within 1–2 months.
This study has a few limitations. First, the study was a single-center study with limited population. The small number of post-ERCP complications makes it difficult to compare treatment modalities. Several options are available and should be considered case-by-case depending on the severity and nature of the complication. More studies on this subject are definitely needed. The main strength is the prospective nature of the study. This is the first prospective study reporting results in this precise setting. All the ERCPs in the health care district were performed in the study hospital and all the complications, techniques, maneuvers and such were precisely documented. We were also able to access data on post-discharge events.
In conclusion, this prospective study shows that ERCP can indeed be performed safely on elderly patients. The most common complication is pancreatitis, which in comparison to earlier reports, and especially in comparison to younger cohorts, seems to be less common. Nevertheless, complications occur even in the oldest patients and therefore, the probable benefits and possible risks of the procedure need to be carefully assessed. In our series, the procedures were performed by high-volume endoscopists using appropriate techniques, which may partly explain the excellent results. The high 30-day mortality in patients with malignancies should be taken into consideration when selecting therapeutic options such as stents.
References
Siegel JH, Kasmin FE. Biliary tract diseases in the elderly: management and outcomes. Gut. 1997;41:433–435.
Mazen Jamal M, Yoon EJ, Saadi A, et al. Trends in the utilization of endoscopic retrograde cholangiopancreatography (ERCP) in the United States. Am J Gastroenterol. 2007;102:966–975.
Halttunen J, Meisner S, Aabakken L, et al. Difficult cannulation as defined by a prospective study of the Scandinavian Association for Digestive Endoscopy (SADE) in 907 ERCPs. Scand J Gastroenterol. 2014;49:752–758.
Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393.
Christensen K, Doblhammer G, Rau R, et al. Ageing populations: the challenges ahead. Lancet. 2009;374:1196–1208.
Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102:1781–1788.
Fritz E, Kirchgatterer A, Hubner D, et al. ERCP is safe and effective in patients 80 years of age and older compared with younger patients. Gastrointest Endosc. 2006;64:899–905.
Katsinelos P, Paroutoglou G, Kountouras J, et al. Efficacy and safety of therapeutic ERCP in patients 90 years of age and older. Gastrointest Endosc. 2006;63:417–423.
Rodriguez-Gonzalez FJ, Naranjo-Rodriguez A, Mata-Tapia I, et al. ERCP in patients 90 years of age and older. Gastrointest Endosc. 2003;58:220–225.
Lukens FJ, Howell DA, Upender S, Sheth SG, Jafri SM. ERCP in the very elderly: outcomes among patients older than eighty. Dig Dis Sci. 2010;55:847–851.
Grönroos JM, Salminen P, Laine S, Gullichsen R. Feasibility of ERCP procedures in patients 90 years of age and older. J Clin Gastroenterol. 2010;44:227–228.
Sugiyama M, Atomi Y. Endoscopic sphincterotomy for bile duct stones in patients 90 years of age and older. Gastrointest Endosc. 2000;52:187–191.
Finkelmeier F, Tal A, Ajouaou M, et al. ERCP in elderly patients: increased risk of sedation adverse events but low frequency of post-ERCP pancreatitis. Gastrointest Endosc. 2015;82:1051–1059.
Garcia CJ, Lopez OA, Islam S, et al. Endoscopic retrograde cholangiopancreatography in the elderly. Am J Med Sci. 2016;351:84–90.
ASGE Standards of Practice Committee, Anderson MA, Fisher L, et al. Complications of ERCP. Gastrointest Endosc. 2012;75:467–473.
Day LW, Lin L, Somsouk M. Adverse events in older patients undergoing ERCP: a systematic review and meta-analysis. Endosc Int Open. 2014;2:28–36.
Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425–434.
Williams EJ, Taylor S, Fairclough P, et al. Risk factors for complication following ERCP; results of a large-scale, prospective multicenter study. Endoscopy. 2007;39:793–801.
Wang P, Li ZS, Liu F, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009;104:31–40.
Dumonceau JM, Tringali A, Blero D, et al. Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2012;44:277–298.
Walter D, van Boeckel PG, Groenen MJ, et al. Cost efficacy of metal stents for palliation of extrahepatic bile duct obstruction in a randomized controlled trial. Gastroenterology. 2015;149:130–138.
Adler DG, Baron TH, Davila RE, et al. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005;62:1–8.
Kaffes AJ, Hourigan L, De Luca N, et al. Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest Endosc. 2005;61:269–275.
Sandha GS, Bourke MJ, Haber GB, et al. Endoscopic therapy for bile leak based on a new classification: results in 207 patients. Gastrointest Endosc. 2004;60:567–574.
Acknowledgments
This study was financially supported by the Competitive Research Funding of the Pirkanmaa Hospital District, Finland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors disclosed no financial relationships relevant to this publication.
Rights and permissions
About this article
Cite this article
Ukkonen, M., Siiki, A., Antila, A. et al. Safety and Efficacy of Acute Endoscopic Retrograde Cholangiopancreatography in the Elderly. Dig Dis Sci 61, 3302–3308 (2016). https://doi.org/10.1007/s10620-016-4283-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4283-2