Abstract
Background
Patients receiving 5-aminosalicylic acid (5-ASA) require long-term therapy to achieve good outcomes. Persistency (duration of time from initiation to discontinuation of therapy) is therefore an important consideration.
Aim
To evaluate persistency in patients receiving various oral 5-ASA formulations.
Methods
This retrospective, 12-month, cohort study examined new-starter patients (any age and diagnosis) from a large United States pharmacy database who filled a prescription for oral 5-ASA [Lialda®, Asacol®, Pentasa® 250 or 500 mg, balsalazide (generic and Colazal®), and olsalazine (Dipentum®)] between March and September 2007. Persistency was evaluated monthly on the basis of prescription refill rates.
Results
Prescription and refill records were identified for 44,191 patients receiving oral 5-ASA. After 1 year, 20% of patients receiving Lialda were considered persistent and classified as continuing (refilling within a timeframe of up to twice the duration of the prescription), compared with 9% receiving Asacol, 7 (250 mg) and 10% (500 mg) receiving Pentasa, 10% receiving balsalazide, and 10% receiving Dipentum.
Conclusions
Overall persistency with oral 5-ASA therapy was low. However, patients receiving once-daily Lialda had significantly higher persistency after 1 year of treatment than patients receiving other oral 5-ASA therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ultimate goal of treatment in patients with ulcerative colitis (UC) is to achieve and maintain clinical and endoscopic remission, as there is accumulating evidence to suggest that both sustained symptom resolution and complete mucosal healing are necessary in order to achieve the most favorable long-term outcomes [1, 2]. The principal medical therapy used to treat mild-to-moderate UC is 5-aminosalicylic acid (5-ASA) [3, 4], an anti-inflammatory treatment (available in a range of oral and rectal formulations). 5-ASA is thought to act topically on the colonic mucosa to reduce tissue inflammation [5].
Because 5-ASA is quickly and easily absorbed in the stomach and small intestine, several oral formulations have been developed to protect the drug as it passes through the gastrointestinal (GI) tract to the colon [6, 7]. Commonly available oral 5-ASA formulations include: bacterially cleaved, diazo-bonded prodrugs (balsalazide and olsalazine); pH-dependent, delayed-release, enteric-coated, mesalamine therapies (e.g., Asacol®; Warner Chilcott, Rockaway, NJ, USA); time-dependent, controlled-release, ethylcellulose-coated, mesalamine microgranules (Pentasa®; Shire Pharmaceuticals, Wayne, PA, USA, trademark licensed from Ferring BV); and pH-dependent, enteric-coated, mesalamine drug incorporating a polymer matrix core (e.g., Lialda®; also known as Mezavant XL® in the UK and Ireland, and as Mezavant® elsewhere; Shire Pharmaceuticals).
Formulations of 5-ASA are potentially highly efficacious in the treatment of mild-to-moderate UC; however, they require continued regular administration to maintain remission. This introduces two principal behaviors in the management of UC: adherence (medication taken as prescribed), and persistency (duration of time from initiation to discontinuation of therapy).
The importance of adherence has been explored previously [8–13]. However, despite the expected benefits, between 40 and 60% of patients with UC do not take their oral 5-ASA medication as prescribed [11–18]. The lowest adherence rates have been reported in patients with quiescent UC, who may not understand the need for continuing their medication after the remission of symptoms [11, 16, 19].
Similar concerns arise when considering persistency: patients may take their medication in the short-term, but fail to continue their medication over the long-term. Poor persistency with medication is often reported in chronic diseases with prolonged asymptomatic periods [20–22], but has not been studied in patients receiving 5-ASA therapies. The objective of this analysis was, therefore, to evaluate persistency in a large number of patients who have been prescribed common oral formulations of 5-ASA. In particular, we were interested in examining persistency with Lialda (1.2 g/tablet) compared with the other formulations, as this is the first approved once-daily formulation available.
Methods
Study Design
This retrospective, 12-month, cohort study evaluated persistency with oral 5-ASA therapy using prescription refill data from a large, national, pharmacy database in the United States (Patient Parameters™; SDI, Plymouth Meeting, PA, USA). This database receives information on approximately 2 billion prescription claims (provider and hospital) per year, representing more than 150 million unique patients. Data are obtained from various providers and sample nearly 59,000 US pharmacies (encompassing >99% of retail stores). Cash, Medicaid (plus other publicly funded healthcare programs), and third-party (e.g., insurance) transactions are all included. Mail order prescriptions were excluded from this analysis. Within the database, information was available on: type of utilization (i.e. patients who were starting, continuing, restarting, switching, adding on, discontinuing, or titrating their medication); medication switching (switching to and from a product); patient demographics (age and gender); and physician specialty.
Oral 5-ASA brands that were prescribed to patients included mesalamine formulations (Lialda, Asacol, and Pentasa; 250 or 500 mg), balsalazide (generic balsalazide disodium and Colazal®; Salix Pharmaceuticals, Morrisville, NC, USA), and olsalazine (Dipentum®; UCB, Smyrna, GA, USA).
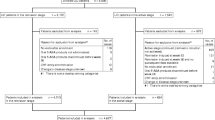
Patients
Patients who started a new prescription for oral 5-ASA therapy between March and September 2007 were eligible for inclusion in the study. Patients included in this study were not necessarily treatment naïve, but had not filled a prescription for their cohort product in the prior 6 months. This study required that any eligible patient could be followed in the database for a period of at least 18 months. No diagnosis information was available, however, as mesalamine formulations are only indicated for UC, but it was expected that most of the included patients have this diagnosis and would form the majority of eligible subjects.
In compliance with the US Health Insurance Portability and Accountability Act, secure encryption methods were used to ensure patient anonymity at all times. Secure patient identifiers allowed patients to be tracked through changes in pharmacy or health plan.
Assessments and Classification
After the patient’s initial prescription, patient prescription and refill records were examined continually over a 12-month study period. Based on their prescription refill activity, patients were classified each month according to the following criteria:
-
1.
Continuing (a patient who filled at least two prescriptions and refilled prescriptions within a timeframe of up to twice the duration of the prescription).
-
2.
Restarting (a patient who refilled prescription after the grace period of twice the time of their number of days’ supply of medication had elapsed).
-
3.
Switching (a patient who switched from one product to another and did not fill their cohort product again. Therefore, in this analysis, patients who switched were considered to have discontinued their cohort formulation).
-
4.
Titrating (Pentasa only; a patient whose dose was titrated from one strength of Pentasa to another).
-
5.
Discontinuing (a patient who discontinued therapy with that brand; patients were categorized in the first month in which they failed to refill their prescription. Discontinuing patients could subsequently be considered as ‘restarting’ if they resumed their medication during the study period).
-
6.
No activity (a patient that could not be classified as any other patient type during a given month but who is later observed to restart their cohort product).
Statistical Analysis
The prescription claim data are owned and were analyzed by SDI. Persistency with 5-ASA therapy was evaluated on the basis of prescription refill rates (i.e. the percentage of patients refilling their prescriptions). Persistency rates were calculated for each month of the 12-month study period. Only patients that were classified as continuing or restarting are reported in this analysis. Patients who switched therapy were considered to have discontinued their existing therapy. The mean number of filled prescriptions and mean cumulative days of therapy per patient for all patients starting treatment were also calculated for each 5-ASA formulation after 12 months of treatment. Due to the availability of generic balsalazide formulations from January 2008, data for generic balsalazide disodium and Colazal were combined for all analyses (termed the ‘all balsalazide’ cohort).
A two-tailed z test was used to evaluate differences between the brand associated with the highest persistency rate and other oral 5-ASA therapies for all outcome measures. P values of <0.001 were considered to be statistically significant. Statistical analyses were performed using SAS v9.1 (SAS Institute, Cary, NC, USA).
Exploratory Analyses
Post hoc, exploratory subset analyses were subsequently undertaken to investigate the influence of patient age (0–17, 18–25, 26–40, 41–55, and 56+ years), patient gender, and specialty of the prescribing physician [gastroenterologist, internist, primary care physician (PCP; general practitioner, family practitioner or osteopathic physician), surgeon, or other practitioner] on persistency rates. Additional post hoc analyses were undertaken to evaluate the effect prescription length had on persistency rates among patients. Data for Pentasa were combined for all exploratory analyses, as two dose formulations of Pentasa (250 and 500 mg) are commercially available, compared with a single dose for the other formulations included.
Results
Patients
Prescription and refill records were identified for 44,191 patients who had been prescribed oral 5-ASA therapy: Asacol, n = 25,887; Pentasa, n = 7,218; Lialda, n = 6,170; all balsalazide, n = 4,557; and Dipentum, n = 359. No patients received generic balsalazide disodium at enrollment; however, patients who subsequently switched from Colazal to a generic balsalazide were considered ‘persistent’ with balsalazide therapy and were not considered to be ‘switching’. Patient characteristics are shown in Table 1.
The majority of patients received medication lasting for up to 30 days (Asacol 93%, all balsalazide 91%, Dipentum 88%, Lialda 96%, Pentasa 95%). Slightly more patients who were prescribed azo-bonded formulations received prescriptions lasting between 31 and 90 days (all balsalazide 9% and Dipentum 12%, compared with Asacol 7%, Lialda 4% and Pentasa 5%).
Persistency
The overall persistency with 5-ASA as a class of drug, (regardless of the brand or patients switching between different formulations over time), was 13% at 12 months. After 1 year of therapy, 20% of patients receiving Lialda were classified as continuing compared with 9% receiving Asacol, 7 (250 mg) and 10% (500 mg) receiving Pentasa, 10% receiving all balsalazide, and 10% receiving Dipentum (Fig. 1a). The differences in persistency between Lialda and all other 5-ASA therapies were statistically significant (P < 0.001).
When considering the persistency of patients using 5-ASA as a class of drug (regardless of the brand or patients switching between different formulations over time), 25% were considered continuing or restarting at 12 months. A similar pattern was observed when both continuing and restarting patients were considered; those receiving Lialda had the highest persistency (32%), compared with Asacol (19%), Pentasa (250 mg: 15%; 500 mg: 19%), all balsalazide (19%), and Dipentum (16%; Fig. 1b). Again, the 12-month persistency rate associated with Lialda was statistically higher than those associated with other oral 5-ASA therapies (P < 0.001).
Days of Therapy and Number of Prescription Fills
Patients receiving Lialda received significantly more days of therapy (mean 136 days; Table 2) and collected a significantly higher number of prescriptions (mean 4.4 per patient; Table 2) compared with those receiving other 5-ASA formulations (P < 0.001 for all comparisons). The largest treatment group (patients receiving Asacol) collected a mean of 2.7 prescriptions per patient and received a mean of 86 days of therapy (Table 2). Given that the average prescription length was highly similar between all treatment groups (mean 30 days, range 1–100 days), it is unlikely that these results were confounded by length of prescription. In the post hoc analysis of patients whose initial prescription was limited to 30 days only, similar results to the main findings of this study were observed; 20% of patients receiving Lialda remained persistent after 1 year, compared with 7–10% of patients who received other 5-ASA therapies (Fig. 2).
Exploratory Analyses
Overall, over half the patients were prescribed 5-ASA therapy by a gastroenterologist (n = 25,111). One-fifth (20%) of patients prescribed Lialda by a gastroenterologist were persistent after 1 year of therapy; this was higher than for patients receiving Asacol (10%), all balsalazide (10%), Pentasa (10%), or Dipentum (12%) (Fig. 3a). Overall, similar patterns of persistency were observed between prescribing physicians, however, persistency among patients receiving their prescription from an internist was often higher than in other groups (Fig. 3b). Indeed, the most persistent subgroup (22%) received Lialda from internists.
a Continuing persistency with 5-aminosalicylic acid therapy during the 12 months following treatment initiation in patients who received their prescription from a gastroenterologist. b Continuing persistency with Lialda® during the 12 months following treatment initiation, according to prescribing physician specialty
Persistency was highest with Lialda across all age subgroups. The most persistent subgroup after 1 year of therapy (21%) was patients aged 41–55 years (Fig. 4a); this was also the largest Lialda subgroup. Persistency with Lialda in patients of this age group was higher than in patients of the same age receiving Asacol (9%), all balsalazide (10%), Pentasa (9%), or Dipentum (8%) (Fig. 4b).
Male patients receiving Lialda remained more persistent than female patients (24 vs. 18%, respectively) after 1 year of therapy. A similar pattern was observed in patients receiving Asacol (11 vs. 8%), all balsalazide (11 vs. 9%), Pentasa (11 vs. 9%), or Dipentum (12 vs. 9%).
Similar trends in persistency by prescribing speciality, age and gender were also seen in patients whose initial prescription was limited to 30 days only.
Discussion
Administrative healthcare databases have been used to evaluate persistency with medication across various diseases [23–26], but have rarely been used for this purpose in patients receiving 5-ASA therapies. Importantly, the data obtained from these databases are considered to provide an accurate, objective indication of medication consumption in a large number of patients within a real-life, clinical practice setting.
In this analysis, patients receiving Lialda had significantly higher persistency, collected significantly more refills, and received significantly more days of therapy after 1 year of treatment compared with patients receiving other oral 5-ASA formulations, irrespective of how persistency was defined (i.e. using continuing or continuing plus restarting patients). Persistency was approximately twofold higher in the Lialda group (20%) compared with all other 5-ASA groups (7–10%) in continuing patients, and over 1.5-fold higher in continuing and restarting patients combined (32 vs. 15–19%, respectively).
Recent patient survey data indicate that many patients do indeed consider less frequent dosing and fewer pills to be very important attributes of treatment, and feel challenged by complex dosing regimens [27, 28]. In a clinical setting, data from two prior observational studies have demonstrated an association between multiple-daily dosing and medication nonadherence [8, 12]. However, other studies have reported conflicting results [16, 29–31]. The results presented here include a large number of patients receiving both once- and multiple-daily regimens in a ‘real-life’ setting, and appear to be consistent with a link between persistency and dosing complexity.
Although interesting differences in persistency appear to exist across the formulations, long-term persistency with 5-ASA therapy was generally low, suggesting that strategies need be implemented to improve persistency with medication. The low persistency rates are, however, consistent with results obtained in other ‘real-world’ studies and surveys that assessed persistency or adherence [11–16, 18, 19, 27, 28, 32]. Approaches to improve adherence and persistency have been proposed, but at present there are no universally accepted strategies in widespread clinical use [17]. Potential strategies include improving the relationship between the patient and their physician, improving patients’ health literacy, empowering patients to take control of their disease management, regular follow-up/monitoring, financial reimbursement from the healthcare center as an incentive to take medication, and simplifying/facilitating the dosing regimen [17, 19, 33]. A systematic review of interventions to enhance medication adherence in chronic medical conditions published in 2007 found the most effective interventions to be those that aimed to simplify the dose administration regimen [34].
The results of the exploratory analyses also provided some intriguing findings. When the data were analyzed according to physician specialty, persistency was generally similar between prescribing groups; however, it was noted that prescriptions from internists often resulted in higher persistency rates. As many adults in the USA see internists for primary healthcare, and may not see a gastroenterologist for quiescent uncomplicated UC, internists may have a particularly close relationship with patients and could be well positioned to provide follow-up and support. Data to support this theory come from a recent 7-year study in the Kaiser system in northern California, which reported, for patients with inflammatory bowel disease (IBD), an increase of over 400% in the number of visits to an internist over time compared with number of visits to a gastroenterologist. This suggests that, following diagnosis, patients with IBD are receiving most of their care from a physician other than a gastroenterologist [35].
Overall, persistency in all subgroups was low. There are a number of factors not explored in this study that could affect patient decisions about whether to continue taking their medication. Despite potentially good relationships with prescribing physicians, many patients fail to take their medication as prescribed, suggesting a possible failure in the overall communication regarding the importance of persistency. Previous studies have shown that adherence to treatment for GI disorders, including IBD, is strongly linked to the relationship between the patient and their physician [11, 36, 37]. Furthermore, it has previously been shown that the fastest decline in 5-ASA prescription refill rates occurs during the first 3 months of treatment and continues thereafter, albeit at a slower rate [30]. All patients may therefore benefit from ‘interval empathy’ techniques, whereby patients are scheduled for follow-up appointments (including at least one visit within the first 3 months of treatment) even if they are well. Prior studies have shown that adherence to medical treatment can be improved by introducing more frequent follow-up visits [38].
The exploratory analyses also showed that the overall highest persistency, by age, was achieved in older patients (41–55 years) who were prescribed Lialda. With the exception of those patients receiving Dipentum, an age-related trend toward higher persistency was not observed with the other formulations. Persistency with all oral 5-ASA therapies was higher in male patients compared with female patients. There are conflicting reports in the literature regarding the influence of age and gender on 5-ASA adherence and persistency [11, 15, 16, 29, 32, 39], highlighting the complexity of persistency and the need to individualize therapy.
This study has several limitations. Firstly, this analysis is limited primarily by the use of prescription refill data to evaluate persistency, but these data do not provide information on whether or not patients actually took their medication, or how they took it. Secondly, this was a descriptive analysis and the results could be confounded by a number of factors that are not under the control of this study, for example, lack of information on diagnosis, disease duration, severity or the requirement for additional medication. Finally, drug costs have previously been observed to play a role in patient adherence [40]. As the data in this study include prescriptions funded by a number of sources (e.g., Medicaid, third parties), there is the potential for payor type to act as a confounder. Examination of these factors (Table 1) suggests that payment methods and drug costs were largely similar between the formulation groups. However, drug costs and co-payment schemes vary over time (and location) and this database did not capture the true cost to the patient after savings schemes or coupons. Despite these limitations, this study examined a large number of patients who were prescribed various 5-ASA agents and some valuable observations have been made.
In conclusion, this large retrospective study suggests that patients receiving once-daily Lialda have higher persistency after 1 year of treatment than patients receiving other oral 5-ASA formulations. However, overall persistency rates associated with each of the oral 5-ASA therapies was low. The improved persistency rates associated with Lialda may have important implications for patients, including fewer relapses. We hypothesize that formulations that offer a lower pill burden and less frequent dosing improve persistency; however, prospective well-controlled studies will be required to investigate this hypothesis further.
References
Lichtenstein GR, Rutgeerts P. The importance of mucosal healing in ulcerative colitis. Inflamm Bowel Dis. 2009;16:338–346.
Rutgeerts P, Vermeire S, Van AG. Mucosal healing in inflammatory bowel disease: impossible ideal or therapeutic target? Gut. 2007;56:453–455.
Carter MJ, Lobo AJ, Travis SP. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004;53:V1–V16.
Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105:501–523.
Lichtenstein GR, Kamm MA. Review article: 5-aminosalicylate formulations for the treatment of ulcerative colitis–methods of comparing release rates and delivery of 5-aminosalicylate to the colonic mucosa. Aliment Pharmacol Ther. 2008;28:663–673.
Cohen RD. Review article: evolutionary advances in the delivery of aminosalicylates for the treatment of ulcerative colitis. Aliment Pharmacol Ther. 2006;24:465–474.
Qureshi AI, Cohen RD. Mesalamine delivery systems: do they really make much difference? Adv Drug Deliv Rev. 2005;57:281–302.
Kane S, Huo D, Aikens J, Hanauer S. Medication nonadherence and the outcomes of patients with quiescent ulcerative colitis. Am J Med. 2003;114:39–43.
Kane S, De Vos M, Riley S, Frieri G, Mittmann U. Compliance issues in inflammatory bowel disease. Rev Gastroenterol Disord. 2005;5:101–106.
Kane S, Shaya F. Medication non-adherence is associated with increased medical health care costs. Dig Dis Sci. 2008;53:1020–1024.
Sewitch MJ, Abrahamowicz M, Barkun A, et al. Patient nonadherence to medication in inflammatory bowel disease. Am J Gastroenterol. 2003;98:1535–1544.
Shale MJ, Riley SA. Studies of compliance with delayed-release mesalazine therapy in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18:191–198.
van Hees PA, van Tongeren JH. Compliance to therapy in patients on a maintenance dose of sulfasalazine. J Clin Gastroenterol. 1982;4:333–336.
Bernal I, Domenech E, Garcia-Planella E, et al. Medication-taking behavior in a cohort of patients with inflammatory bowel disease. Dig Dis Sci. 2006;51:2165–2169.
Cerveny P, Bortlik M, Kubena A, Vlcek J, Lakatos PL, Lukas M. Nonadherence in inflammatory bowel disease: results of factor analysis. Inflamm Bowel Dis. 2007;13:1244–1249.
Kane SV, Cohen RD, Aikens JE, Hanauer SB. Prevalence of nonadherence with maintenance mesalamine in quiescent ulcerative colitis. Am J Gastroenterol. 2001;96:2929–2933.
Kane SV. Strategies to improve adherence and outcomes in patients with ulcerative colitis. Drugs. 2008;68:2601–2609.
Stone MA, Mayberry JF, Baker R. Prevalence and management of inflammatory bowel disease: a cross-sectional study from central England. Eur J Gastroenterol Hepatol. 2003;15:1275–1280.
Kane SV, Brixner D, Rubin DT, Sewitch MJ. The challenge of compliance and persistence: focus on ulcerative colitis. J Manag Care Pharm. 2008;14:s2–s12.
Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens. 2006;19:1190–1196.
Cramer JA, Silverman S. Persistence with bisphosphonate treatment for osteoporosis: finding the root of the problem. Am J Med. 2006;119:S12–S17.
Cramer JA, Benedict A, Muszbek N, Keskinaslan A, Khan ZM. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. Int J Clin Pract. 2008;62:76–87.
Breekveldt-Postma NS, Koerselman J, Erkens JA, Lammers JW, Herings RM. Enhanced persistence with tiotropium compared with other respiratory drugs in COPD. Respir Med. 2007;101:1398–1405.
Esposito D, Wahl P, Daniel G, Stoto MA, Erder MH, Croghan TW. Results of a retrospective claims database analysis of differences in antidepressant treatment persistence associated with escitalopram and other selective serotonin reuptake inhibitors in the United States. Clin Ther. 2009;31:644–656.
Hassan M, Madhavan SS, Kalsekar ID, et al. Comparing adherence to and persistence with antipsychotic therapy among patients with bipolar disorder. Ann Pharmacother. 2007;41:1812–1818.
Lee PP, Walt JG, Chiang TH, Guckian A, Keener J. A gap analysis approach to assess patient persistence with glaucoma medication. Am J Ophthalmol. 2007;144:520–524.
Loftus EV Jr. A practical perspective on ulcerative colitis: patients’ needs from aminosalicylate therapies. Inflamm Bowel Dis. 2006;12:1107–1113.
Rubin DT, Siegel CA, Kane SV, et al. The impact of ulcerative colitis from patients’ and physicians’ perspectives: results from the UC: NORMAL survey. Inflamm Bowel Dis. 2009;15:581–588.
Ediger JP, Walker JR, Graff L, et al. Predictors of medication adherence in inflammatory bowel disease. Am J Gastroenterol. 2007;102:1–10.
Magowan SKS, Lange J. 5-ASA prescription refill rates of ulcerative colitis are independent of formulation and dosing regimens. Am J Gastroenterol. 2006;101:S447. (Abstract 1144).
Gray JR, Leung E, Scales J. Treatment of ulcerative colitis from the patient’s perspective: a survey of preferences and satisfaction with therapy. Aliment Pharmacol Ther. 2009;29:1114–1120.
Kane SV, Accortt NA, Magowan S, Brixner D. Predictors of persistence with 5-aminosalicylic acid therapy for ulcerative colitis. Aliment Pharmacol Ther. 2009;29:855–862.
Collinson S. Payment for treatment adherence: incentives help vulnerable patients to stay well. BMJ. 2007;335:317.
Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167:540–550.
Herrinton LJ, Liu L, Fireman B, et al. Time trends in therapies and outcomes for adult inflammatory bowel disease, Northern California, 1998–2005. Gastroenterology. 2009;137:502–511.
Levy RL, Feld AD. Increasing patient adherence to gastroenterology treatment and prevention regimens. Am J Gastroenterol. 1999;94:1733–1742.
Nguyen GC, Laveist TA, Harris ML, Datta LW, Bayless TM, Brant SR. Patient trust-in-physician and race are predictors of adherence to medical management in inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:1233–1239.
DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: results from the Medical Outcomes Study. Health Psychol. 1993;12:93–102.
D’Inca R, Bertomoro P, Mazzocco K, Vettorato MG, Rumiati R, Sturniolo GC. Risk factors for non-adherence to medication in inflammatory bowel disease patients. Aliment Pharmacol Ther. 2008;27:166–172.
Kane SV. Systematic review: adherence issues in the treatment of ulcerative colitis. Aliment Pharmacol Ther. 2006;23:577–585.
Acknowledgments
Initial data analyses were undertaken by Michael Cheyne and Matthew Hauben who are employees of SDI and received funding from Shire Pharmaceuticals Inc., USA. Writing and editorial support was provided by Duncan Campbell of GeoMed and funded by Shire Pharmaceuticals Inc., USA.
Conflict of interest
Sunanda Kane has served as a consultant for and has received research support from Shire Pharmaceuticals Inc., USA. Michael Sumner, Dory Solomon, and Matt Jenkins are all employees of Shire Pharmaceuticals Inc., USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kane, S.V., Sumner, M., Solomon, D. et al. Twelve-Month Persistency with Oral 5-Aminosalicylic Acid Therapy for Ulcerative Colitis: Results from a Large Pharmacy Prescriptions Database. Dig Dis Sci 56, 3463–3470 (2011). https://doi.org/10.1007/s10620-011-1877-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1877-6