Abstract
Background and objective
To determine the impact of non-adherence to 5-Aminosalicylates (5-ASA) on the risk of flares and to identify risk factors of non-adherence.
Methods
Observational, cohort study of ulcerative colitis (UC) patients in clinical remission at least 6 months on 5-ASA monotherapy maintenance prescribed by an electronic management program. Adherence was considered when 80% of the prescribed 5-ASA had been dispensed at the pharmacy. The study analyzed the existence and degree of 5-ASA adherence, disease course, UC phenotypic expression, and 5-ASA dose and regimen, and consumption of non-UC chronic drugs during 2-year follow-up.
Results
The study included 274 patients, 49% males with a median age of 38 (27–49) years old. Overall, 41% of patients were non-adherent to 5-ASA. Risk of flares was reduced in the adherent group (36% vs 54%; OR = 0,484; p = 0,004), mainly the mild ones (26% vs 38%; OR = 0,559; p = 0,031). Non-adherence was associated with younger age at diagnosis (32 (26–45) vs 41.5 (21–50), p = 0.000) and no-consumption of other chronic treatments (1.1 vs 2.1; OR = 1709; p = 0,048).
Conclusion
Non-adherence to 5-ASA evaluated by the pharmaceutical management system was at 41% with a higher risk of relapse. Younger patients and patients who do not receive non-UC chronic treatments showed lower adherence rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) characterized by an unpredictable course marked by periods of flare and remission. The goal of maintenance therapy is to keep steroid-free remission, clinically and endoscopically defined [1, 2]. 5-Aminosalicylates (5-ASA) represent the first-line maintenance treatment in patients responding to 5-ASA or steroids due to its beneficial effect in inducing remission and preventing relapse [3, 4]. Moreover, maintenance treatment with 5-ASA has proven to prevent long-term complications such as colorectal cancer (CRC) [5]. Thus, patients are required to take medication for long periods of time and, in most cases, indefinitely [1].
Patient adherence to treatment is defined as the rate of cooperation in following the physician’s prescriptions and recommendations over a specific period of time [6]. The adherence rate to 5-ASA varies from 23 to 93% based on different cohorts [7.8]. Adherence to 5-ASA therapy is essential to improve disease outcomes. Non-adherence to 5-ASA is related to a higher risk of disease relapse [9,10,11,12], CRC [13], worsening quality of life, and increased medical health care costs [11, 14, 15]. Other pharmacological factors such as 5-ASA dose have shown to impact on disease course together with adherence to medication [16]. However, several studies have investigated adherence to UC treatment using indirect and subjective methods such as patient self-reporting, questionnaires, or medical records [7, 8, 10, 17,18,19,20]. Adherence evaluation with these methods has come up with disperse adherence rates and controversial results about risk factors and impact of non-adherence in UC.
We hypothesized that non-adherence to 5-ASA can be evaluated objectively and reliably with a pharmaceutical electronic management system. The main aim of this study was to determine the impact of non-adherence to 5-ASA on the risk of flares. The secondary aim was to identify risk factors of non-adherence.
Material and methods
Study design and population
An observational, analytical, retrospective with prospectively gathered data, single tertiary center, cohort study of 2-year follow-up was performed. All consecutive patients with UC diagnosis, followed in the Inflammatory Bowel Disease (IBD) Unit of the University Clinic Hospital of Valencia in January 2016, were screened for eligibility. Inclusion criteria were firm UC diagnosis, age ≥ 18 years, clinical remission for at least 6 months before the study, 5-ASA monotherapy as maintenance treatment at the beginning of the study, and prescription made with a pharmaceutical electronic management program with a regular follow-up of at least every 6 months in the out-patient clinic. Exclusion criteria were history of colon surgery and hypersensitivity or intolerance to 5-ASA.
Epidemiological and clinical data were collected from the ENEIDA registry. ENEIDA is a registry of the Spanish Working Group in Crohn’s and Colitis (GETECCU), which includes patients with IBD. The database prospectively records clinical characteristics, outcomes, and treatments. Adherence to treatment was evaluated with a pharmaceutical electronic management program. With this method, we calculated the percentage of the prescribed doses of the 5-ASA that the patient dispensed at the pharmacy. Non-adherence was considered when 5-ASA dispensed was less than 80% of the prescribed [6]. Adherence was measured until relapse or until the end of the study period in cases under remission. No motivation for adherence to treatment was present during the study period reflecting a real clinical practice situation.
Informed consent to participate in the database was obtained from all patients. The study was approved by the institutional ethics committee of the hospital on August 28, 2016. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution’s human research committee.
Variables
Variables included were adherence to 5-ASA, gender and age at diagnosis, risk factors for IBD, phenotypic expression of the disease, presence of extraintestinal manifestations, complications, 5-ASA dose, formulation and regimen, consumption of other non-UC chronic treatments, and disease course evaluated as relapse rate, severity of flares, and interval since the beginning of the study until relapse.
Definitions
Diagnosis of UC was made by local gastroenterologists based on standard clinical, endoscopic, and pathological criteria according to the European Crohn’s and Colitis Organization (ECCO) consensus guidelines [1].
A positive family history was defined as the presence of one or more relatives of first or second degree with either UC or Crohn’s disease (CD). Patients were classified as smokers if they had smoked more than seven cigarettes per week for at least 6 months and ex-smokers if they had stopped smoking for at least 12 months at the time of the evaluation.
Disease extent was determined with ileocolonoscopy and classified according to the Montreal classification [21]. The maximum extent of disease at any time since diagnosis was assigned for each patient. The extraintestinal manifestations (EIMs) taken into account were peripheral arthropathy, ankylosing spondylitis, sacroilitis, erythema nodosum, pyoderma gangrenosum, aphthous stomatitis, iritis, episcleritis, primary sclerosing cholangitis, and thrombosis. Complications considered were megacolon, intra-abdominal abscesses, bowel perforation, or major acute hemorrhage defined as hematochezia or melena with hemodynamic instability (hypotension or orthostatic change in vital signs) and/or an acute decrease in hemoglobin concentration of at least 2 mg/dL compared with baseline. Neoplasia was defined as the presence of high-grade dysplasia or colon carcinoma during follow-up surveillance colonoscopy.
Relapse was defined based on previous cohort studies according to the Mayo score that led to the initiation of remission-induction therapy [2]. A mild flare was considered whether an increase in the 5-ASA dose or combination therapy was needed. A moderate-severe flare was considered when steroids, immunomodulators, or biologic treatments were added. Flares that required hospitalization were considered in a separate group.
The treatment regimen for UC in the follow-up period was the same in all patients, based on Spanish-developed guidelines [22], which are in agreement with ECCO guidelines [1].
Statistical analysis
The distribution of the variables was obtained by the analysis of normality with the Kolmogorov-Smirnov and the Shapiro-Wilk test. Qualitative variables were expressed as frequencies (%) and quantitative variables as mean and standard deviation (SD) or median and interquartile range (IQR).
Univariate analysis was performed to study demographic variables, risk factors for IBD, phenotypic expression, treatment regimen, and disease course differences according to the existence and degree of 5-ASA adherence. Either chi-square test or Fisher’s test (variables that showed more than 25% of the categories with an expected value lower than 5) was performed with qualitative variables. Measures of association between qualitative variables were reported as odds ratio (OR) with 95% confidence intervals (95CI). Comparison between groups of quantitative variables was made with the t test, Mann-Whitney U test, or Kruskal-Wallis test, as required. A multivariate logistic regression model was applied to discriminate adherence condition including in the model significant risk factors of the univariate analysis.
A Spearman’s rank correlation coefficient analysis was performed to correlate percentage of adherence with relapse rates.
Kaplan-Meier curves were used to compare the time free of relapse among 5-ASA adherence, with statistical comparison being made using the log-rank test. Cox proportional hazard models were used to assess the relationships between non-adherence and clinical relapse as well as other potential prognostic factors.
All statistical tests were two-sided. A p value of < 0.05 was considered statistically significant. Analyses were performed with the SPSS V22.0 software package.
Results
Study population and prevalence of adherence
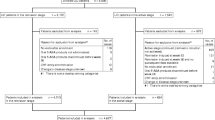
The cohort included 542 patients at the beginning of the study. From the initial eligible population, 268 patients did not meet the inclusion criteria and were excluded; 274 patients were finally enrolled (Fig. 1).
Baseline characteristics of the cohort population are shown in Table 1.
Overall, 112 (41%) (95CI = 35–47) patients were non-adherent to 5-ASA during the 2-year follow-up. The median adherence rate was 65% (49–74) and 94% (88–100) in the non-adherent and adherent group, respectively (p = 0,000).
Disease flares according to adherence
During the follow-up period, 124 patients experienced relapse. For all patients, the cumulative relapse rate was 45.3% (95CI = 39–51). Eighty-eight (32%) patients suffered a mild relapse, of whom 71 (81%) required a combination of 5-ASA therapy and 63 (72%) increased doses. Fifty-five patients (20%) experienced a moderate-severe flare that required steroids, of whom 9 (16%) were prescribed immunomodulation, 7 (13%) biologics, and 5 (9%) combination therapy of immunomodulators and biologics. Two patients (0.7%) required hospitalization.
Risk of flares was reduced in the adherent group (36% vs 54%; OR = 0.48; 95CI = 0.29-0.80; p = 0.004). Differences were mainly seen in the risk of mild flares (26% vs 38%; OR = 0.56; 95CI = 0.33-0.95; p = 0.031); while no statistically differences were observed in the risk of moderate-severe (18% vs 21%; OR = 0.79; 95CI = 0.43-1,47; p = 0.461) and flares that required hospitalization (0.7% vs 0.9%; OR = 0.70; 95CI = 0.04-11,38; p = 0.804).
Rank correlation showed a limited inversed relationship between adherence rate to 5-ASA and number of relapses (r = − 0.20, 95CI = − 0.32–− 0.09, p = 0.001). Kaplan-Meier analysis showed differences in terms of survival function free of relapse with a mean of 16 vs 18 months in non-adherent vs adherent group, respectively (log-rank 7.67; p = 0.006; hazard ratio 1.66, 95CI = 1.15–2.41, p = 0.007) (Fig. 2).
Univariate analysis of demographical data, risk factors of IBD, phenotypic expression, and treatment regimens according to disease flares is shown in Table 1.
Younger age at diagnosis, 5-ASA in a unique daily dose, no-treatment for other chronic diseases, and 5-ASA non-adherence were associated with an increased risk of flares. No differences were observed for gender, family history of IBD, smoking habits, appendectomy, disease duration and extent, perianal involvement, EIM, complications, CRC, and 5-ASA dose or formulation among both groups. A multivariable Cox regression analysis was performed, including statistically significant variables of Table 1. This analysis showed that adherence condition and number of 5-ASA takes per day remained as independent predictive factors of relapse (Table 2). Survival function free of relapse showed a mean of 16 vs 18 months in non-divided vs divided doses of 5-ASA, respectively (log Rank 4.83; p = 0.028) (Fig. 3).
Means of daily dose were 2.8 g, 2.7 g, 3 g, and 2.9 g per day in those patients taking 1, 2, 3, or 4 takes per day respectively. Cox regression excluded daily dose as an independent risk factor for disease flare (HR = 1.00; 95CI = 1.00–1.00; p = 0.077) and maintained non-adherence (HR = 1.77; 95CI = 1.21-2.58; p = 0.003) and number of 5-ASA takes per day (HR = 0.74; 95CI = 0.59–0.93; p = 0.010) as predictors of relapse.
Risk factors for non-adherence
Univariable analysis comparing demographical data, risk factors of IBD, phenotypic expression, and treatment regimens according to adherence is shown in Table 1. Younger age at diagnosis and no-treatment for other chronic diseases were associated with non-adherence to 5-ASA. No differences were observed for gender, family history of IBD, smoking habit, appendectomy, disease duration and extent, perianal involvement, EIMs, complications, CRC, and 5-ASA dose or formulation and 5-ASA regimen. The multivariable logistic regression analyses showed that younger age at diagnosis (OR = 1.03; 95CI = 1.01–1.04; p = 0.010) and no-consumption of other chronic treatments (OR = 1.71; 95CI = 1.004–2.91; p = 0.048) remained as independent risk factors of non-adherence to 5-ASA. The discriminant function model showed that independent factors distinguish 5-ASA adherence condition in 65% of the cases.
Discussion
With this study, we obtained that 41% (95CI = 35–47) of the UC patients were non-adherent to 5-ASA during the 2-year follow-up and non-adherence was associated with an increased risk of disease flare and shorter time free of relapse.
The two recent Spanish studies of Bermejo F et al. [17] and Algaba A et al. [18], which based their studies on the same population, showed a discordant adherence rate of 31% and 81%, respectively, measured by a self-reporting questionnaire. To avoid subjective data which may lead to very different results, we used the pharmaceutical electronic management system. This is an objective method that reports the percentage of dispensed medication by the patient in the pharmacy and therefore provides a good estimation of the medication consumption. It is costless and easy to apply in routine clinical care for evaluating adherence without an influence on patients’ attitude, showing real-life data about the impact and risk factors of non-adherence in UC.
The results of our study, in accordance with previous results [9,10,11,12], show that non-adherence to 5-ASA is an independent predictive factor of disease relapse. However, unlike other studies [10, 18, 20], we excluded patients with adjuvant maintenance treatment with immunomodulators or biologic therapies or less than 6 months clinical remission before inclusion not due to the lack of validity of the method in this population but to assess the direct effect of 5-ASA non-adherence in disease outcomes. We found that non-adherence to 5-ASA monotherapy was mainly related to an increased risk of mild flares. The pathophysiology of the disease could explain the differences shown according to the severity of the relapse. A pooled analyses of individual participant data from clinical trials have shown no benefit of concomitant 5-ASA in patients with UC escalated to biologic therapy [23]. Therefore, while mild flares depend on 5-ASA adherence; moderate or severe flares trigger regardless of the 5-ASA not only adherence but also treatment prescription. The higher number of patients that experienced a mild flare compared with those who suffered a moderate or severe one could also explain a stronger statistical power in the mild group.
A major finding in our study is that both non-adherence and the number of times 5-ASA is taken per day are independent predictors of disease flare. A higher survival function free of relapse was seen in patients taking divided 5-ASA dosing compared with once daily dose. On the contrary, the meta-analysis of Li W et al. [22] found that once daily dosing of 5-ASA was as effective and safe as multiple dosing for inducing and maintaining remission of mild to moderate UC. However, some of the studies included were of low quality and the inclusion criteria of patients with UC and relapse or remission definitions were not uniform among the studies included in the meta-analysis. A limitation of our study is that no subgroup analysis of 5-ASA type was done. Nevertheless, other pharmacological variables were analyzed, and we observed no differences in the 5-ASA total dose, route of administration, or adherence rate among once vs multiple daily dosing that could explain the higher risk of relapse. Therefore, future trials will need to explore the optimal 5-ASA administration regimen.
As it is well known, adherence to treatment in chronic disease is a complex issue in which a wide variety of factors play a role. Previous studies have tried to identify demographic and clinical characteristics predictive of non-adherence to 5-ASA in UC. However, these studies have provided contradictory results about the influence of some factors such as gender, age, social status, or number of daily doses [7, 8, 17,18,19,20, 24, 25]. The pharmaceutical electronic management system allows physicians to reliably asses the percentage of topical medication dispensed by the patient in the pharmacy. Moreover, no differences were found in the adherence rate or in their risk factors depending on the route of 5-ASA administration, so therefore patients with only topical formulation were also included. Factors that showed independent association with non-adherence to 5-ASA in our study were younger age at diagnosis and no-consumption of other chronic treatments. Patients with no other chronic treatments showed up to 2.2 times higher risk of non-adherence than patients taking other chronic diseases medication which may imply that patients with other chronic disease are more aware of the relevance of taking their medication.
Adherence concept implies a wide range of behaviors, from a patient that misses occasionally a dose to a patient who does not take any of their medication. Moreover, adherence rates not only vary between patients but also over time. A limitation of our study is that disease relapse was defined retrospectively according to the treatment changes and variations of the adherence condition over time after disease flares were not measured. Thus, the effect of disease relapse in the patients’ behavior was not evaluated. In addition, patients have different reasons for not taking their medication, which could be unintentional and intentional [26]. Combining a self-reported method with an electronic management system to evaluate adherence to 5-ASA will help understand the relationship between patients’ beliefs, concerns, and behaviors. Identifying the specific reason behind non-adherence may help to individualize measures to improve adherence.
In summary, there is 41% (95CI = 35–47) non-adherence to 5-ASA evaluated with a pharmaceutical electronic management program. Younger patients who do not receive other non-UC chronic treatment show a lower adherence rate. Non-adherence to 5-ASA is associated with a higher risk of disease flares, although mainly mild. A higher time-to-relapse is present in patients taking divided 5-ASA doses compared with a once daily dose. The electronic management system may be considered a useful tool in the clinical practice evaluation, mainly to be applied in patients with non-adherence risk factors, in order to recognize their reasons for inadequate adherence and increase awareness of its consequences in disease evolution.
References
Hardbord M, Eliakim R, Bettenworth D, Karmiris K, Katsanos K, Kopylov U, Kucharzik T, Molnár T, Raine T, Sebastian S, de Sousa HT, Dignass A, Carbonnel F, European Crohn’s and Colitis Organisation (ECCO) (2017) Third European evidence-based consensus on the diagnosis and management of ulcerative colitis part 2: current management. J Crohn Colitis 11:769–784. https://doi.org/10.1093/ecco-jcc/jjx009
Travis SP, Higgins PD, Orchard T, Van Der Woude CJ, Panaccione R, Bitton A, O’Morain C, Panés J, Sturm A, Reinisch W, Kamm MA, D’Haens G (2011) Review article: defining remission in ulcerative colitis. Aliment Pharmacol Ther 34:113–124. https://doi.org/10.1111/j.1365-2036.2011.04701.x
Ford AC, Achkar JP, Khan KJ, Kane SV, Talley NJ, Marshall JK, Moayyedi P (2011) Efficacy of 5-ASA in UC: a meta-analysis. Am J Gastroenterol 106:601–616. https://doi.org/10.1038/ajg.2011.67.
Wang Y, Parker CE, Feagan BG, MacDonald JK (2016) Oral 5-aminosalicylic acid for induction of remission in ulcerative colitis. Cochrane Database Syst Rev 4:CD000543. https://doi.org/10.1002/14651858.CD000544.pub4.
Velayos FS, Terdiman JP, Walsh JM (2005) Effect of 5-aminosalicylate use on colorectal cancer and dysplasia risk: a systematic review and metaanalysis of observational studies. Am J Gastroenterol 100:1345–1353
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353:487–497. https://doi.org/10.1056/NEJMra050100
Cerveny P, Bortlik M, Vlcek J, Kubena A, Lukás M (2007) Nonadherence in inflammatory bowel disease: results of factor analysis. Inflamm Bowel Dis 13:1244–1249. https://doi.org/10.1016/j.crohns.2007.08.002.
Bager P, Julsgaard M, Vesteergard T, Christensen LA, Dahlerup JF (2016) Adherence and quality of care in IBD. Scand J Gastroenterol 51(11):1326–1331. https://doi.org/10.1080/00365521.2016.1195870
Kane S, Huo D, Aikens J, Hanauer S (2003) Medication nonadherence and the outcomes of patients with quiescent ulcerative colitis. Am J Med 114:39–43
Kawakami A, Tanaka M, Nishigaki M, Naganuma M, Iwao Y, Hibi T, Sanada H, Yamamoto-Mitani N, Kazuma K (2013) Relationship between non-adherence to aminosalicylate medication and the risk of clinical relapse among Japanese patients with ulcerative colitis in clinical remission: a prospective cohort study. J Gastroenterol 48:1006–1015. https://doi.org/10.1007/s00535-012-0721-x
Higgins P, Rubin DT, Kaulback K, Schoendfield PS, Kane SV (2008) Systematic review: impact of non-adherence to 5-aminosalicylic acid products on the frequency and costs of ulcerative colitis flares. Aliment Pharmacol Ther 29:247–257. https://doi.org/10.1111/j.1365-2036.2008.03865.x.
Khan N, Abbas AM, Bazzano LA, Koleva YN, Krousel-Wood M (2012) Long-term oral mesalazine adherence and the risk of disease flare in ulcerative colitis: nationwide 10-years retrospective cohort from the veterans affairs healthcare system. Aliment Pharmacol Ther 36:755–764. https://doi.org/10.1111/apt.12013
Van Staa TP, Card T, Logan RF, Leufkens HG (2005) 5-Aminosalicylate use and colorectal cancer risk in inflammatory bowel disease: a large epidemiological study. Gut 54:1573–1578
Mitra D, Hodgkins P, Yen L, Davis KL, Cohen RD (2012) Association between oral 5-ASA adherence and health care utilization and costs among patients with active ulcerative colitis. BMC Gastroenterol 12:132. https://doi.org/10.1186/1471-230X-12-132
Kane S, Shaya F (2008) Medication non-adherence is associated with increased medical health care costs. Dig Dis Sci 53:1020–2024
Khan N, Abbas AM, Koleva YN, Bazzano LA (2013) Long-term mesalamine maintenance in ulcerative colitis: which is more important? Adherence or daily dose. Inflamm Bowel Dis 19(6):1123–1129. https://doi.org/10.1097/MIB.0b013e318280b1b8
Bermejo F, López-San Román A, Algaba A, Guerra I, Valer P, García-Garzón S, Piqueras B, Villa C, Bermejo A, Rodríguez-Agulló JL (2010) Factors that modify therapy adherence in patients with inflammatory bowel disease. J Crohn Colitis 4:422–426. https://doi.org/10.1016/j.crohns.2010.01.005
Algaba A, Guerra I, Garcia Garcia de Pareces A, Hernández Tejero M, Ferre C, Bonillo D, Aguilera L, López-Sanromán A, Bermejo F (2017) What is the real life manteinance mesalazine dose in ulcerative colitis? Rev Esp Enferm Dig 109(2):114–121. https://doi.org/10.17235/reed.2016.4620/2016.
Ediger JP, Walker JR, Graff L, Lix L, Clara I, Rawsthorne P, Rogala L, Miller N, McPhail C, Deering K, Bernstein CN (2007) Predictor of medication adherence in inflammatory bowel disease. Am J Gastroenterol 102(7):1417–1426
Li W, Zhang ZM, Jiang XL (2016) Once daily versus multiple daily mesalamine therapy for mild to moderate ulcerative colitis: a meta-analysis. Color Dis 18(7):0214–0223. https://doi.org/10.1111/codi.13393
Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR, Caprilli R, Colombel JF, Gasche C, Geboes K, Jewell DP, Karban A, Loftus EV Jr, Peña AS, Riddell RH, Sachar DB, Schreiber S, Steinhart AH, Targan SR, Vermeire S, Warren BF (2005) Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a working party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol 19(Suppl):5A–36A
Gomollón F, García-López S, Sicilia B, Gisbert JP, Hinojosa J (2013) Therapeutic guidelines on ulcerative colitis: a GRADE methodology based effort of GETECCU. Gastroenterol Hepatol 36:1–47. https://doi.org/10.1016/j.gastrohep.2012.09.006
Singh S, Proudfoot JA, Dulai PS, Jairath V, Fumery M, Xu R, Feagan BG, Sandborn WJ (2018) No benefit of concomitant 5-aminosalicylates in patients with ulcerative colitis escalated to biologic therapy: pooled analysis of individual participant data from clinical trials. Am J Gastroenterol. https://doi.org/10.1038/s41395-018-0144-2
Jackson CA, Clatworthy J, Robinson A, Horne R (2010) Factors associated with non-adherence to oral medication for inflammatory bowel disease: a systematic review. Am J Gastroenterol 105:525–539. https://doi.org/10.1038/ajg.2009.685
Keil R, Keil R, Wasserbauer M, Zádorová Z, Kojecký V, Hlava Š, Št'ovíček J, Chudý J, Roznětinská M, Drábek J, Kubišová N, Lochmannová J (2018) Adherence, risk factors of non-adherence and patient's preferred treatment strategy of mesalazine in ulcerative colitis: multicentric observational study. Scand J Gastroenterol 53(4):459–465. https://doi.org/10.1080/00365521.2018.1451915
Kane SV, Robinson A (2010) Review article: understanding adherence to medication in ulcerative colitis – innovative thinking and evolving concepts. Aliment Pharmacol Ther 32(9):1051–1058. https://doi.org/10.1111/j.1365-2036.2010.04445.x
Author information
Authors and Affiliations
Contributions
Conception and design of the study: Ballester MP, Martí-Aguado D, Fullana M, Bosca-Watts MM, and Minguez M
Acquisition of data: Ballester MP, Martí-Aguado D, Fullana M, Romero E, Sanchez A, Navarro P, and Anton R
Analysis and interpretation of data: Ballester MP, Martí-Aguado D, Bosca-Watts MM, Tosca J, and Minguez M
Manuscript writing: Ballester MP, Martí-Aguado D, Bosca-Watts MM, Tosca J, Mora F, and Minguez M
All listed authors approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
M. Minguez has served as a speaker, a consultant, and advisory member for or has received research funding from MSD, Abbvie, Pfizer, Janssen, Shire Pharmaceuticals, Allergan.
M.M. Bosca-Watts declares educational activities, research projects, scientific meetings, and advisory boards sponsored by MSD, Ferring, Abbvie, Janssen, and Takeda.
Informed consent statement
All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Institutional review board approval
The study was reviewed and approved by the University Clinic Hospital of Valencia, Institutional Review Board.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ballester, M.P., Marti-Aguado, D., Fullana, M. et al. Impact and risk factors of non-adherence to 5-aminosalicylates in quiescent ulcerative colitis evaluated by an electronic management system. Int J Colorectal Dis 34, 1053–1059 (2019). https://doi.org/10.1007/s00384-019-03271-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03271-9