Abstract
Background
Tumors involving the pyloric channel have been considered as difficult lesions for successful endoscopic resection. We studied the feasibility of endoscopic submucosal dissection (ESD) using retroflexion in the duodenum to resect the gastric neoplasia involving the pyloric channel.
Aim
To compare the treatment outcomes of a new ESD technique using retroflexion to those without retroflexion in the duodenum.
Methods
Twenty-four cases of gastric neoplasia involving the pyloric channel were resected by ESD. In 14 cases, ESDs were performed from both the antrum and duodenal bulb using retroflexion (retroflexion group). In ten cases, ESDs were performed conventionally only from the side of the antrum (conventional group). We compared the outcomes between the two methods.
Results
There was no complication regarding retroflexion in the duodenum. In the retroflexion group, the en bloc and complete resection rate was 100%, respectively. The rate of complete resection was significantly higher in the retroflexion group than in the conventional group (P = 0.01). In the conventional group, three patients with early gastric cancer underwent additional subtotal gastrectomy for positive lateral margin, and one patient with perforation was treated additionally by surgical repair. In the retroflexion group, microperforation and pyloric channel stenosis occurred in one patient, which resolved with conservative treatment.
Conclusions
Tumors involving the pyloric channel could be successfully resected by ESD using retroflexion in the duodenum without severe complication. This technique appears to be a feasible and effective method for the treatment of tumors involving the pyloric channel.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pyloric channel is the anatomic location with abrupt narrowing in the lumen of the stomach, and lesions involving the pyloric channel cannot be well visualized by the conventional forward-viewing method. Although endoscopic submucosal dissection (ESD) has been considered as a technique with high en bloc resection rates, this anatomical characteristic has been a problem in the successful resection of tumors because the lesion beyond the pyloric ring may not be completely seen. So, the tumor can be resected with the conventional method, but the safe margin on the far side of the specimen may not be assured. Retroflexion in the duodenum can allow complete assessment of the size and extent for the tumor involving the pyloric channel. The use of this method has been reported in a few case studies [1–3]. However, there has been no report comparing the outcomes of ESD between the conventional forward-viewing resection and the new resection technique approaching from both the antrum and duodenal bulb using retroflexion.
In this study, we evaluated the feasibility of ESD using retroflexion in the duodenum to resect the gastric neoplasia involving the pyloric channel, and the treatment outcomes by the new ESD technique using retroflexion were compared to those without retroflexion in the duodenum.
Methods
Patients
Between June 2005 and April 2011, consecutive patients with gastric dysplasia or early gastric cancer involving the pyloric ring were enrolled at Seoul St. Mary’s Hospital in Korea. Pyloric ring involvement was defined as <5 mm from the pyloric channel considering the safety of the lateral margin. Patients who had acute duodenal ulcer, prior history of duodenal ulcer, or ulcer scar at the duodenum were excluded. Informed consent was obtained from all of the patients before the procedure. ESDs were performed conventionally only from the side of the antrum in the first ten enrolled patients, who were assigned to the conventional group. Thereafter, all patients were treated with ESDs from both the antrum and duodenal bulb using retroflexion and assigned to the retroflexion group.
This study was approved by the Institutional Review Board of Seoul St. Mary’s Hospital, Seoul, Korea (KC10RISI0662).
ESD Procedures
All patients underwent ESD procedures under sedation with the intravenous administration of midazolam (3–5 mg, Bukwang Pharm. Co., Ltd., Seoul, Korea) and pethidine (50 mg, Myungmoon Pharm. Co., Ltd., Seoul, Korea). The ESD procedure was carried out using a forward-viewing endoscope (GIF-Q240/Q260 J; Olympus Optical Co., Ltd., Tokyo, Japan) with a transparent disposable attachment (D-201-11804; Olympus) fitted onto the tip of the endoscope for a fixed endoscopic view. Several spots were marked 5–10 mm outside the margin of the lesion with a needle knife or by a hook knife. After the injection of a normal saline with 0.0025% epinephrine into the submucosa, mucosal resection and submucosal dissection was done with an insulated-tip (IT) or a hook knife. Injections were repeated as needed and further resection was carried out to ensure total removal of the lesion. An electrosurgical current was applied using a high-frequency generator with an automatically controlled system for cutting and coagulation (ERBE 200D; ERBE Elektromedizin GmbH, Tübingen, Germany).
ESD procedures were performed by two experienced endoscopists, who had performed more than 200 cases of ESD before treating these patients. The used knives were the IT knife (KD-610L; Olympus) and hook knife (KD-620LR; Olympus).
ESD Using Retroflexion in the Duodenum
In ESDs using retroflexion in the duodenum, marking was performed at the prepyloric antrum and the duodenal bulb with the endoscope retroflexed in the duodenum; then, the resection was attempted at the duodenal bulb with the endoscope retroflexed in the duodenum after precutting at the duodenal bulb and then resection was made at the prepyloric antrum.
Outcome Parameters
In our study, the primary outcome parameter was the rate of en bloc with tumor-free margin. The secondary outcome parameters were procedure time, complications related with the procedure, such as bleeding and perforation.
The gross tumor type was assessed according to the Paris classification of superficial neoplastic lesions in the digestive tract [4]. Resected specimens were systematically sectioned at 2-mm intervals, centered on the part of the lesion closest to the margin and the site of deepest invasion.
En bloc resection was defined when the tumor was resected in one piece, without fragmentation. Piecemeal resection was noted if two or more pieces were needed to achieve resection. Complete resection was defined when the tumor was removed by en bloc or piecemeal resection with which the horizontal and vertical margins were histologically free of neoplasia.
In terms of complications, overt perforation was determined if the intra-abdominal space or mesenteric fat was visible endoscopically during the procedure. Microperforation was diagnosed when perforation was not noted endoscopically but the presence of free air was observed on a radiographic imaging just after the resection. Procedure-related bleeding was defined as clinical evidence of bleeding after ESD, such as hematemesis or melena that required endoscopic treatment or surgical intervention.
Post-ESD Follow-Up
All of the patients received, intravenously, a normal dose of proton pump inhibitor (PPI) for 3 days and switched to oral PPI for 4 weeks after the ESD procedure. Endoscopic follow-up examinations were performed 1 day after ESD. To see whether pyloric stenosis was developed after ESD, we followed up the patients after 2 months. Thereafter, the patients underwent endoscopic examination 6 months after the ESD and every 12 months thereafter. Patients were asked for dyspepsia symptoms during every visit. The dyspepsia score was recorded using a 10-cm visual analog scale.
Statistical Analysis
Rates and proportions were calculated for categorical data, and median and range for continuous data. Fisher’s exact test and the Mann–Whitney test were used to compare the retroflexion and the conventional group. All statistical analyses were performed using SAS software (SAS Institute, Cary, NC, USA).
Results
Twenty-five patients were enrolled in our study. One patient who had a duodenal ulcer scar was excluded. Among a total of 24 patients, 14 patients were included in the retroflexion group and ten in the conventional group. None of the patients had severe concomitant diseases. The clinical features of the patients are summarized in Table 1. In the endoscopic findings, ulcer was observed in only one patient in the retroflexion group. The pathologic diagnoses of these lesions were 13 gastric adenomas and 11 early gastric cancers, all of which were limited in the mucosal layer and did not involve the lymphovascular system. There was no significant difference in age, gender, procedure time, size of the resected specimen, and tumor size between the two groups.
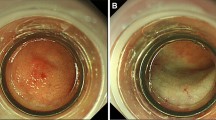
As shown in Table 2, the rate of en bloc and the complete resection rate was 100% in the retroflexion group, respectively. One example is shown in Fig. 1. One patient with early gastric cancer (patient no. 2, Table 1) had undergone endoscopic mucosal resection (EMR) for adenoma at the pyloric channel 5 years ago, and the lesion had developed again on the ulcer scar, which could hinder the successful lifting of the submucosal layer. This lesion was successfully treated by the new method with a hook knife using retroflexion in the duodenum (Fig. 2).
Example of endoscopic submucosal dissection (ESD) using retroflexion in the duodenum. Early gastric cancer was overlying on the pyloric ring (a, b). After marking of the resection margin (c, d), precutting in the antral (e) and duodenal sides (f) was done. Then, dissection using retroflexion (g, h) and conventionally (i, j) was performed. Resected (k) and the final mapping specimen (l) are shown
Endoscopic finding during and after ESD using retroflexion in the duodenum for a case with recurrent early gastric cancer at the pyloric channel (patient no. 2, Table 1). A lobulated lesion found was at the pyloric channel, including the duodenal bulb (a, b). ESD was performed (c–e, precut and dissection at the duodenal bulb; f, g, precut and dissection at the prepyloric antrum). Complete resection was done (h, i). Resected specimen (j)
In the conventional group, the en bloc resection rate was 80% (Table 2). The rate of complete resection was significantly lower in the conventional group than in the retroflexion group (60 and 100%, respectively; P = 0.01). The rate of en bloc with tumor-free margin was 50% in the conventional group, which was significantly lower than that of the retroflexion group (P = 0.03). A case with adenocarcinoma (patient no. 19, Table 1) failed to achieve both en bloc and complete resection. In another case, en bloc resection was achieved, but cancer (patient no. 21) was exposed in the lateral margin. One patient with adenoma (patient no. 17) failed to achieve en bloc resection, but the resection margin was free of tumor. All of these cases were resected with an IT knife. The patients who failed to achieve tumor-free margin underwent additional subtotal gastrectomy.
The complication rate was not different between the two groups. Significant bleeding was not observed in both groups. In each group, there was one case of perforation. In the retroflexion group, one patient (patient no. 5) had microperforation, which was found only in the follow-up chest X-ray after the ESD procedure. Because the site of perforation was not visible in esophagogastroduodenoscopy (EGD) and the patient was tolerable without symptoms, the patient was treated conservatively. The free air disappeared after 2 days, and diet was started after 5 days of the procedure. There was no retroflexion-related complication. In the conventional group, perforation in the ESD site (patient no. 16, Table 1) was treated with additional surgical repair.
In the post-resection stenosis, a small amount of food remaining in the stomach was observed without any dyspeptic symptoms in one patient from the retroflexion group (patient no. 5). However, the passage of a transnasal endoscope (GIF-XP260N; Olympus) was possible. After additional acid suppression therapy, follow-up EGD performed 1 month later showed resolved stenosis of the pyloric channel without food stasis in the stomach.
Discussion
This study showed the successful treatment of gastric tumors involving the pyloric channel by ESD using retroflexion in the duodenum with a hook knife. This new technique achieved a significantly higher rate of complete resection compared to the conventional method. There was no complication associated with retroflexion in the duodenum in our study.
Enabled by the new resection technique, ESD, recent indications for the endoscopic resection of early gastric cancer have been expanded, especially upon the size limitation [5]. En bloc resection of gastric tumor is important in endoscopic therapy because it reduces the risk of tumor recurrence [6]. Thus, the distal margin of the lesion should be determined thoroughly, and when the distal margin is not visualized with forward-view endoscopy, other approaches such as retroflexion in the lumen or the use of a side-viewing instrument can be an alternative treatment. The retroflexion method has been used for tumors in the stomach and colon, of which the lumen allows the endoscope to flex fully [7–9].
The tumor involving the pyloric channel has been considered to be difficult to achieve en bloc resection, since the lesion beyond the pyloric ring is not able to be seen entirely. To assess the lesion over the pyloric ring completely, endoscopists have tried to flex the endoscopy with a J-turn in the duodenal bulb side [1]. Recently, successful treatment of a gastric tumor which involved the pyloric channel has been reported with the new technique using retroflexion of endoscopy in the duodenal bulb [2, 3]. However, there has been no report comparing this new method with the conventional resection method. We supposed that, with retroflexion in the duodenal bulb, complete assessment of the lesion may be possible, resulting in successful treatment outcomes. Our study revealed the superiority of this new retroflexion method compared to the conventional method.
The superiority of this new resection method was shown in patient no. 2. This patient had recurrent early gastric cancer on the previous endoscopic resection site in another hospital. With the new retroflexion method, the lesion could be resected completely. This case is consistent with the previous report that ESD for residual/local recurrent early gastric cancer after EMR is a safe and effective procedure [5].
Technically, the location of the lesion can help the decision regarding the resection method. The lesions located in the anterior wall are relatively easy to resect without retroflexion. However, it may be better to use the retroflexion method to resect the lesions located in the posterior wall.
There may be cases in which it is difficult to retroflex in the duodenum. There is some concern about the possibility of iatrogenic perforation in the duodenum during this procedure, when operator retroflexed roughly. Although there was no retroflexion-related complication occurring in our study, endoscopists must realize that perforations can be associated with this procedure [10]. To lower this possible complication, we excluded the patients with a duodenal ulcer scar which can narrow the lumen or cause the friability to the iatrogenic damage. For the benign lesion in which retroflexion in the duodenum is difficult, conventional methods should be selected and the use of a side-viewing instrument or repeated partial EMR may be an alternative. For the malignant mucosal lesion with difficulty in retroflexion, conventional methods must be tried and the surgical approach can be considered if the lesion was not resected as a body or completely.
Post-ESD stenosis is thought to be caused by resecting a large area near the cardia or the pylorus. Although there has been limited reports about post-ESD stenosis in tumors involving the pyloric channel [11, 12], one study reported a circumferential extent of the mucosal defect of >3/4 or longitudinal extent of >5 cm in length as risk factors for post-ESD stenosis in pyloric resections [5]. In our study, post-ESD stenosis occurred in a patient in whom about 3/4s of the pyloric channel ring circumference was resected. Post-ESD stricture can be effectively treated by balloon dilation, sometimes requiring surgical intervention [1, 5]. In our case, the symptoms of the patient were resolved after additional acid suppression therapy without other intervention.
Our study has some limitations. First, a small number of cases was enrolled. However, the number shown in this study is enough to illustrate the safety and efficacy of this new technique, since the tumors involving the pyloric channel are not frequently encountered. Second, the outcome of ESDs may be different according to the operators when considering the characteristics of an operator-dependent procedure. In our study, both operators had enough experience in ESD. Third, the patients were not divided into the two groups randomly.
The dissection property of the two knives also may attribute to this different outcome. The IT knife may result in complications when the cutting direction is not in line with the submucosal plane. The hook knife has an advantage in terms of safety aspects, because hooking up the mucosa before cutting is possible. In our study, two cases of incomplete resection were performed with the IT knife. In a previous study in which ESDs were performed with a IT knife, complete resection was not achieved in some cases, even with the retroflexion method [3].
In conclusion, tumors involving the pyloric channel could be successfully treated by ESD with a hook knife using retroflexion in the duodenum without severe complications. When a gastric tumor involves the pyloric channel, endoscopic resection with retroflexion in the duodenum appears to be a safe and effective treatment method.
References
Brandt LJ, Gotian A. Retroflexion in the duodenum for evaluation of duodenal bulb lesions. Gastrointest Endosc. 2002;55:438–440.
Onozato Y, Ishihara H, Iizuka H, et al. A large flat adenoma located on the pylorus ring successfully treated by endoscopic submucosal dissection. Dig Dis Sci. 2007;52:1738–1740.
Jung SW, Jeong ID, Bang SJ, et al. Successful outcomes of endoscopic resection for gastric adenomas and early cancers located on the pyloric ring (with video). Gastrointest Endosc. 2010;71:625–629.
Endoscopic Classification Review Group. Update on the Paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy. 2005;37:570–578.
Oka S, Tanaka S, Kaneko I, et al. Endoscopic submucosal dissection for residual/local recurrence of early gastric cancer after endoscopic mucosal resection. Endoscopy. 2006;38:996–1000.
Ono H, Kondo H, Gotoda T, et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225–229.
Burke EL, Chappelka AR Jr, Levine SM. Examination of the esophago-gastric junction area and fundus by retroflexion of the flexible-tip gastroscope: an analysis of 100 consecutive attempts. Gastrointest Endosc. 1970;16:130–134.
Cutler AF, Pop A. Fifteen years later: colonoscopic retroflexion revisited. Am J Gastroenterol. 1999;94:1537–1538.
Rex DK, Khashab M. Colonoscopic polypectomy in retroflexion. Gastrointest Endosc. 2006;63:144–148.
Fu K, Ikematsu H, Sugito M, et al. Iatrogenic perforation of the colon following retroflexion maneuver. Endoscopy. 2007;39:E175.
Tsunada S, Ogata S, Mannen K, et al. Case series of endoscopic balloon dilation to treat a stricture caused by circumferential resection of the gastric antrum by endoscopic submucosal dissection. Gastrointest Endosc. 2008;67:979–983.
Coda S, Oda I, Gotoda T, et al. Risk factors for cardiac and pyloric stenosis after endoscopic submucosal dissection, and efficacy of endoscopic balloon dilation treatment. Endoscopy. 2009;41:421–426.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lim, CH., Park, J.M., Park, CH. et al. Endoscopic Submucosal Dissection of Gastric Neoplasia Involving the Pyloric Channel by Retroflexion in the Duodenum. Dig Dis Sci 57, 148–154 (2012). https://doi.org/10.1007/s10620-011-1863-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1863-z