Abstract
Background
Endoscopic submucosal resection with a ligation device (ESMR-L) is effective for rectal neuroendocrine tumors (NETs); however, its effectiveness for duodenal NETs is unclear. This study evaluated the efficacy and safety of ESMR-L for duodenal NETs.
Methods
A total of 32 consecutive patients with duodenal NETs were treated in our hospital between December 2010 and August 2015. Among these 32 patients, we retrospectively analyzed the data of all patients who underwent ESMR-L for the treatment of duodenal NETs. ESMR-L was considered for patients in whom (1) the lesion size was ≤10 mm in diameter, (2) the lesion was located within the submucosal layer, and (3) no lymph node metastasis or distant metastasis was detected.
Results
Five patients underwent ESMR-L for the treatment of duodenal NETs. The en bloc complete resection rate was 100 %. The median procedure time for ESMR-L was 15 min (range 10–30 min). In all patients, perforation during and after the operation, and intraoperative bleeding were not observed; however, one patient experienced postoperative bleeding. During follow-up, no local recurrence or distant metastasis was noted in any of the patients.
Conclusion
ESMR-L is feasible, effective, and safe for duodenal NETs measuring ≤10 mm in diameter that are confined to the submucosal layer without metastasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Treatment for duodenal neuroendocrine tumors (NETs) typically involves surgical resection or endoscopic resection, including endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) [1]. However, surgical resection is invasive, and EMR and ESD are associated with a high rate of perforation [2, 3].
Endoscopic submucosal resection with a ligation device (ESMR-L) has been reported to be effective for the treatment of rectal NETs [4, 5]; however, few reports exist on the safety and efficacy of ESMR-L for the treatment of duodenal NETs. Therefore, in the present retrospective study, we evaluated the efficacy and safety of ESMR-L for the treatment of duodenal NETs.
Patients and methods
A total of 32 consecutive patients with duodenal NETs were treated in our hospital between December 2010 and June 2015. Among these 32 patients, we retrospectively analyzed the data of all patients who underwent ESMR-L for the treatment of duodenal NETs. All patients were examined with endoscopy and endoscopic ultrasonography (EUS) before undergoing ESMR-L. Additionally, abdominal computed tomography was performed to rule out metastatic lesions. ESMR-L was considered for patients in whom (1) the lesion size was ≤10 mm in diameter, (2) the lesion was located within the submucosal layer, and (3) no lymph node metastasis or distant metastasis was detected.
The patients’ characteristics, clinical courses, and adverse events, such as perforation and bleeding, were assessed. The resected specimens were cut into 2-mm slices after formalin fixation and were stained with hematoxylin and eosin. They were then examined microscopically for depth of invasion, lateral and vertical resection margins, and lymphovascular invasion. Histological diagnosis was performed according to the classification system of the World Health Organization. Complete resection was histopathologically defined as no lateral and vertical margin involvement of the resected tumor.
The study protocol was approved by the medical ethics committee of our hospital, and written informed consent was obtained from all the patients before ESMR-L was performed. This study was performed in accordance with the ethical principles outlined in the Declaration of Helsinki.
ESMR-L procedure
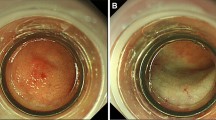
ESMR-L was performed as described previously. All patients received 35 mg pethidine hydrochloride and 2–3 mg midazolam before starting ESMR-L to reduce the discomfort associated with the procedure. A conventional single-channel endoscope (GIF-Q260J; Olympus Medical Systems, Tokyo, Japan) with an attached band-ligator device (MD-48710 EVL Device, Sumitomo Bakelite Co. Ltd, Tokyo, Japan) was used for the procedure. First, saline solution was injected beneath the tumor in the submucosal layer, and then, the tumor was aspirated into the ligator device, followed by deployment of the elastic band. Thereafter, snare resection was performed below the band by using a blended electrosurgical current. Finally, the tumor was removed by aspirating it into a cap or retrieving it with grasping forceps (Fig. 1).
A A neuroendocrine tumor is seen in the duodenal bulb. B Saline solution is injected beneath the tumor in the submucosal layer. C The tumor is aspirated into the ligator device, followed by deployment of the elastic band. D Snare resection is performed below the band by using a blended electrosurgical current, and the tumor is then removed by aspirating it into a cap. E The lesion is completely removed. F The surface of the resected tumor is seen
Results
Five patients (4 men and 1 woman) underwent ESMR-L for the treatment of duodenal NETs. The median age of the patients was 68 years (range 55–80 years). Tumors were located in the duodenal bulb in four patients and the descending portion in one patient, and the median diameter of the tumors was 9 mm (Table 1).
The median procedure time for ESMR-L was 15 min (range 10–30 min). All tumors were located in the submucosal layer, and the pathological diagnoses were NET G1 in four patients and NET G2 in one patient. The en bloc complete resection rate was 100 %. The median hospitalization duration was 5 days (range 3–11 days), and the median follow-up period after ESMR-L was 22 months (range 8–57 months). During follow-up, no local recurrence or distant metastasis was noted in any of the patients (Table 2). Regarding complications, postoperative bleeding occurred in one patient; however, bleeding was successfully managed with endoscopic hemostasis, and no blood transfusion was necessary. Perforation during and after the operation, and intraoperative bleeding were not observed in any of the patients (Table 3).
Discussion
In the present study, ESMR-L was feasible and successful for the treatment of duodenal NETs. Perforation during and after the operation, and intraoperative bleeding did not occur in any of the patients. Postoperative bleeding occurred in only one patient; however, bleeding was successfully managed with endoscopic hemostasis, and no blood transfusion was necessary.
Duodenal NETs are rare and account for approximately 15 % of all gastrointestinal NETs [6]. Burke et al. [7] reported that involvement of the muscularis propria, tumors over 20 mm in diameter, and the presence of mitotic figures are associated with a high risk of metastasis. Soga [6] reported that the metastatic rates of duodenal NETs are proportional to their size; the rate was 8.3 % for tumors ≤5 mm in diameter, and 10.5 % for tumors between 5.1 and 10 mm in diameter. However, Zyromski et al. [8] reported a recurrence rate of 0 % in patients with tumors <2 cm in diameter, who underwent local excision. Thus, there has been no consensus regarding the relationship between the tumor diameter and the rate of occurrence of lymph node metastasis. European guidelines recommended that duodenal carcinoids <10 mm in diameter confined to the submucosa as seen on EUS should be treated with endoscopy in the absence of apparent lymph node invasion and distant metastases [9]. Therefore, if a duodenal NET measuring ≤10 mm in diameter is identified within the submucosal layer on EUS and no metastasis is noted on computed tomography, endoscopic resection can be considered as a treatment option.
Endoscopic resection has been reported to be safe, less invasive, and effective for the treatment of duodenal NETs measuring <10 mm in diameter, with no evidence of invasion of the muscle layer on EUS [10]. However, endoscopic treatment of duodenal lesions is associated with a high incidence of complications, because of the poor operability of lesions in this region using a scope and the thinness of the duodenal wall [11]. En bloc resection is recommended for duodenal NETs because it enables accurate pathological assessment of the vertical and lateral margins of the resected lesions [12]. The pathological complete resection rate is lower with EMR than with ESD, and EMR is sometimes associated with margin involvement and crush injury of the resected tumor, which leads to difficulty in pathological evaluation [13, 14]. Kim et al. reported that the pathological complete resection rate of duodenal NETs was only 56 % with EMR, in spite of a high endoscopic complete resection rate (89 %) [15]. Shroff et al. reported that 40 % of duodenal NETs had positive margins following EMR [16]. Therefore, ESD may be preferable for the endoscopic treatment of duodenal NETs. However, ESD for duodenal tumors is technically difficult and the duodenal wall is thin; therefore, duodenal ESD requires a long procedure time and has a high risk of perforation. Suzuki et al. [17] reported that perforation occurred in 2 of 3 patients during ESD for duodenal NETs. Additionally, Matsumoto et al. reported that perforation occurred in 2 of 5 patients during ESD for duodenal NETs; one patient was treated with simple closure after ESD, and the other underwent local excision after discontinuing ESD [3]. These authors reported a mean resection time of 96.2 ± 54.5 min [3]. In contrast, a significantly deeper vertical resection margin and, theoretically, a higher rate of curative resection can be achieved with ESMR-L than with EMR [4]. Additionally, in our patients, the median procedure time was 15 min and no perforations were noted. Therefore, ESMR-L is superior to ESD in terms of procedural simplicity and the occurrence of perforations.
The limitations of this study include its single-center retrospective design, the small number of patients, and the inadequate follow-up period. Furthermore, this was a non-comparative study without the inclusion of controls or randomization, and the follow-up period was short. Studies with a long follow-up period are needed to rule out metastasis. Nonetheless, this study showed the effectiveness and safety of ESMR-L for the treatment of duodenal NETs. The en bloc complete resection rate was 100 %. Perforations during and after the operation, and intraoperative bleeding were not observed in any of the patients, and postoperative bleeding occurred in only one patient. Additionally, there was no recurrence of a duodenal NET after ESMR-L.
In conclusion, ESMR-L is feasible, effective, and safe for the treatment of duodenal NETs. ESMR-L could be used for treating patients with duodenal NETs measuring ≤10 mm in diameter that are confined to the submucosal layer without metastasis.
References
Bourke MJ (2013) Endoscopic resection in the duodenum: current limitations and future directions. Endoscopy 45(2):127–132. doi:10.1055/s-0032-1326177
Hatogai K, Oono Y, Fu KI, Odagaki T, Ikematsu H, Kojima T, Yano T, Kaneko K (2013) Unexpected endoscopic full-thickness resection of a duodenal neuroendocrine tumor. World J Gastroenterol 19(26):4267–4270. doi:10.3748/wjg.v19.i26.4267
Matsumoto S, Miyatani H, Yoshida Y, Nokubi M (2011) Duodenal carcinoid tumors: 5 cases treated by endoscopic submucosal dissection. Gastrointest Endosc 74(5):1152–1156. doi:10.1016/j.gie.2011.07.029
Ono A, Fujii T, Saito Y, Matsuda T, Lee DT, Gotoda T, Saito D (2003) Endoscopic submucosal resection of rectal carcinoid tumors with a ligation device. Gastrointest Endosc 57(4):583–587. doi:10.1067/mge.2003.142
Mashimo Y, Matsuda T, Uraoka T, Saito Y, Sano Y, Fu K, Kozu T, Ono A, Fujii T, Saito D (2008) Endoscopic submucosal resection with a ligation device is an effective and safe treatment for carcinoid tumors in the lower rectum. J Gastroenterol Hepatol 23(2):218–221. doi:10.1111/j.1440-1746.2008.05313.x
Soga J (2005) Early-stage carcinoids of the gastrointestinal tract: an analysis of 1914 reported cases. Cancer 103(8):1587–1595. doi:10.1002/cncr.20939
Burke AP, Sobin LH, Federspiel BH, Shekitka KM, Helwig EB (1990) Carcinoid tumors of the duodenum. A clinicopathologic study of 99 cases. Arch Pathol Lab Med 114(7):700–704
Zyromski NJ, Kendrick ML, Nagorney DM, Grant CS, Donohue JH, Farnell MB, Thompson GB, Farley DR, Sarr MG (2001) Duodenal carcinoid tumors: how aggressive should we be? J Gastrointest Surg 5(6):588–593
Delle Fave G, Kwekkeboom DJ, Van Cutsem E, Rindi G, Kos-Kudla B, Knigge U, Sasano H, Tomassetti P, Salazar R, Ruszniewski P (2012) ENETS Consensus Guidelines for the management of patients with gastroduodenal neoplasms. Neuroendocrinology 95(2):74–87. doi:10.1159/000335595
Dalenback J, Havel G (2004) Local endoscopic removal of duodenal carcinoid tumors. Endoscopy 36(7):651–655. doi:10.1055/s-2004-814539
Matsumoto S, Miyatani H, Yoshida Y (2013) Endoscopic submucosal dissection for duodenal tumors: a single-center experience. Endoscopy 45(2):136–137. doi:10.1055/s-0032-1310123
Lepilliez V, Chemaly M, Ponchon T, Napoleon B, Saurin JC (2008) Endoscopic resection of sporadic duodenal adenomas: an efficient technique with a substantial risk of delayed bleeding. Endoscopy 40(10):806–810. doi:10.1055/s-2008-1077619
Matsui K, Iwase T, Kitagawa M (1993) Small, polypoid-appearing carcinoid tumors of the rectum: clinicopathologic study of 16 cases and effectiveness of endoscopic treatment. Am J Gastroenterol 88(11):1949–1953
Iishi H, Tatsuta M, Yano H, Narahara H, Iseki K, Ishiguro S (1996) More effective endoscopic resection with a two-channel colonoscope for carcinoid tumors of the rectum. Dis Colon Rectum 39(12):1438–1439
Kim GH, Kim JI, Jeon SW, Moon JS, Chung IK, Jee SR, Kim HU, Seo GS, Baik GH, Lee YC (2014) Endoscopic resection for duodenal carcinoid tumors: a multicenter, retrospective study. J Gastroenterol Hepatol 29(2):318–324. doi:10.1111/jgh.12390
Shroff SRKV, Brunt EM et al (2012) Efficacy of endoscopic mucosal resection (EMR) for management of small duodenal carcinoids. Gastrointest Endosc 75:AB143–AB144
Suzuki S, Ishii N, Uemura M, Deshpande GA, Matsuda M, Iizuka Y, Fukuda K, Suzuki K, Fujita Y (2012) Endoscopic submucosal dissection (ESD) for gastrointestinal carcinoid tumors. Surg Endosc 26(3):759–763. doi:10.1007/s00464-011-1948-y
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Shozo Osera, Yasuhiro Oono, Hiroaki Ikematsu, Tomonori Yano, and Kazuhiro Kaneko have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Osera, S., Oono, Y., Ikematsu, H. et al. Endoscopic submucosal resection with a ligation device for the treatment of duodenal neuroendocrine tumors. Surg Endosc 30, 3928–3932 (2016). https://doi.org/10.1007/s00464-015-4703-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4703-y