Abstract
Background
Therapies that can slow the progression of liver fibrosis in chronic liver disease are needed. Evidence suggests that the renin-angiotensin system (RAS) contributes to inflammation and fibrosis in chronic liver disease. Both animal and limited human studies have shown that RAS inhibition with angiotensin-converting enzyme inhibitors (ACEi) and angiotensin receptor-1 [AT-1] blockers (ARBs) has antifibrogenic properties.
Aims
In this study, we evaluated the effects of continuous ACEi/ARB use for 3.5 years on histological liver fibrosis progression in the HALT-C Trial cohort.
Methods
In the HALT-C Trial, subjects with chronic hepatitis C and advanced hepatic fibrosis (Ishak stage ≥3) underwent serial liver biopsies at baseline, 1.5 years, and 3.5 years after randomization. The primary outcome was a ≥2-point increase in Ishak fibrosis score in at least one of the two serial biopsies. Sixty-six subjects were continuously taking ACEi/ARBs over the observation period, 126 were taking other antihypertensive medications, and 343 subjects took no antihypertensive medications.
Results
The three groups were similar in baseline fibrosis scores, and the two groups being treated with antihypertensives were taking a similar number of antihypertensive medications. Fibrosis progression occurred in 33.3% of the ACEi/ARB group, 32.5% of the other antihypertensive medications group, and in 25.7% of subjects taking no antihypertensive medications. No significant associations between ≥2-point increases in fibrosis scores and continuous ACEi/ARB use were apparent at either 1.5 or 3.5 years in diabetes-adjusted and unadjusted odds ratios.
Conclusions
ACEi/ARB therapy did not retard the progression of hepatic fibrosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The effectiveness of current therapies for some of the common causes of chronic liver disease, such as hepatitis C virus (HCV) infection and steatohepatitis, is limited. Therefore, the need for therapies that can prevent or slow the progression of liver fibrosis in these populations commands a high priority. Substantial evidence suggests that the renin-angiotensin system (RAS), through its key effector peptide angiotensin II, acts as a mediator of inflammation and fibrosis in chronic liver disease. RAS mediates its fibrogenic effects through the activation of hepatic stellate cells (HSC) with their proinflammatory and profibrotic potential [1–5].
Angiotensin-converting enzyme inhibitors (ACEi) and angiotensin receptor-1 [AT-1] blockers (ARBs) are two commonly used RAS inhibitors with well-established safety and efficacy profiles. Extensive data in established animal models of hepatic fibrosis and AT1-knockout mice have demonstrated the hepatic antifibrogenic properties of these classes of medications [6–12]. In addition, limited data supporting the antifibrotic properties of these medications in humans have been reported. However, these reports are based on retrospective studies with small sample sizes, most of which lacked appropriate controls and liver histologic data, which remain the best available standard for the evaluation of liver fibrosis [5, 13–18].
In this study, we evaluated the effects of continuous ACEi/ARB use on progression of histological liver fibrosis in the Hepatitis C Antiviral Long-term Treatment against Cirrhosis (HALT-C) Trial cohort. This cohort is ideal for evaluating the antifibrogenic properties of these medications, given its large size, availability of prospectively collected data on continuous ACEi/ARBs use documented at each of the study visits every 3 months, length of follow-up (48 months), and the availability of serial liver biopsies at baseline, 1.5, and 3.5 years to enable accurate histological assessment of liver fibrosis progression in study subjects taking these medications.
Methods
The HALT-C Trial was a prospective, randomized, controlled, ten-center trial that enrolled 1,050 subjects with chronic hepatitis C and advanced hepatic fibrosis (Ishak fibrosis score ≥3), who had failed to achieve a sustained virologic response (SVR) after previous interferon ± ribavirin treatment [19]. After a 24-week lead-in phase, during which all subjects were treated with peginterferon alfa-2a (180 μg weekly) and ribavirin (1–1.2 g daily), 1,050 subjects in this trial were assigned randomly to receive maintenance therapy with peginterferon alfa-2a (90 μg weekly) or to no treatment for 42 months. All subjects had a liver biopsy performed prior to enrollment and repeated at 1.5 and 3.5 years. All biopsy specimens were reviewed by a panel of 12 hepatic pathologists, who used the Ishak scoring system to stage fibrosis (0–6) [20]. In this trial, no significant difference in liver fibrosis progression was observed between the peginterferon alfa-2a treatment group and the control group [19].
Although entry into the HALT-C Trial was limited to patients with Ishak fibrosis stage ≥3, staging of biopsies by local pathologists at individual sites was reclassified if a central reassessment by all study pathologists examining the specimen together resulted in a different consensus; as a result of consensus reassessment, a stage of 2 was assigned to 79 baseline biopsies [21].
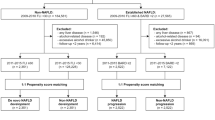
Randomized HALT-C Trial subjects with Ishak fibrosis scores between 2 and 4 were included in this analysis if liver biopsy data were available at two or more time points (baseline, 1.5 years, or 3.5 years) to assess progression of liver fibrosis. A total of 535 subjects of the 1,050 randomized met inclusion to our study. For the HALT-C Trial, progression of fibrosis required a ≥2-point increase. Subjects were seen every 3 months during the 42 months of the randomized trial. Use of ACEi/ARBs by study participants was elicited as part of a comprehensive medication history obtained at each of the study visits. However, no dose information was collected. Continuous ACEi/ARBs use required sustained use of the drug(s) throughout the 48-month trial.
Odds ratios (OR) were calculated to test whether the odds of liver fibrosis progression decreased with long-term continuous use of ACEi or ARBs. Three comparisons were made: (1) continuous use of ACEi/ARBs versus other antihypertensive medications, (2) continuous use of ACEi/ARBs versus no use of any antihypertensive medications, (3) continuous use of any antihypertensive medications versus no use of any antihypertensive medications. Because of the frequent use of ACEi/ARBs in diabetics, we calculated ORs adjusted for diabetic status. Adjusted odds ratios were calculated with the Breslow Day Test, which allowed us to determine whether the ORs for fibrosis progression and ACEi/ARB use were equivalent in diabetics and nondiabetics. Three-way ANOVA was used to compare mean fibrosis stage at baseline between those on ACEi/ARBs, other antihypertensive medications, and subjects not taking any antihypertensive medications at baselines. Chi-square and Fisher’s exact tests were used to compare the baseline characteristics between groups. Statistical significance was set at a two-sided p value ≤0.05.
Results
In this study, we examined the association between continuous ACEi or ARBs use and ≥2-point increases in Ishak fibrosis score at two serial biopsies 1.5 and 3.5 years apart. Table 1 shows the baseline characteristics among the three groups, continuous ACEi/ARB users, users of other antihypertensive medications, and those taking no antihypertensive medications. The continuous ACEi/ARB use group had a statistically significantly higher percentage of diabetics, consistent with the recommended use of these agents for their renal protective effects in diabetics. The groups were similar in baseline fibrosis scores, and the two groups treated with antihypertensive medications were taking similar numbers of antihypertensive medications, a surrogate marker for the severity of hypertension. 33.3% of continuous ACEi/ARB users had ≥2-point increase in Ishak fibrosis score, compared to 32.5 and 25.7% in users of other antihypertensive medications and non-users, respectively (p = 0.21).
The first step in our analysis was to examine the cross-sectional association between ACEi/ARB use at baseline and liver fibrosis stage at baseline biopsy. Ninety subjects were on ACEi/ARB at baseline, 102 subjects were on other antihypertensive medications, and 343 subjects were on no antihypertensive medications. The mean baseline liver fibrosis stage between these groups were 3.10, 3.22, and 3.15, respectively (p = 0.44).
Table 2 shows the unadjusted odds ratios and odds ratios adjusted for diabetes for ≥2-point increases in Ishak fibrosis score and continuous use of ACEi/ARB compared to other antihypertensive medications use, or no antihypertensive medications use. No significant associations were apparent between ≥2-point fibrosis progression and continuous ACEi/ARB use at both 1.5 and 3.5 years. The odds ratios at the two time points remained insignificant even after adjusting for diabetes.
Finally, the unadjusted and diabetes adjusted odds ratios for ≥2-point increases in Ishak fibrosis score among subjects continuously taking any antihypertensive medication (including ACEi/ARB), compared to no antihypertensive medication use were not significantly different (p = 0.83) (Table 2).
Conclusions
Contrary to reports in the literature, including one from our own group [18], we were unable to demonstrate a benefit for ACEi/ARBs use in retarding progression of liver fibrosis. Furthermore, no association between ACEi/ARBs use at baseline and liver fibrosis stage on entry to the HALT-C trial was observed. Compared to previous studies designed to address this question, our study has the advantage of well-documented continuous ACEi/ARBs use recorded prospectively at each HALT-C Trial study visit and the availability of three separate liver biopsies over a 3.5-year period to assess liver fibrosis progression histologically.
In a recent letter to the editor by Cholongitas and colleagues in response to our previous publication [18], they reported their observed effects of ARBs use on histological progression of liver disease in a cohort of 102 consecutive hypertensive patients with recurrent HCV after liver transplantation. Their patients underwent at least two consecutive liver biopsies with a median time between biopsies of 13 months (range 1–18). Administration of an ARB, compared with the other antihypertensive drugs, was associated with less progression in inflammation but not in fibrosis [22]. To our knowledge, this is the only other report in the literature that prospectively evaluated histological progression of liver disease with ACEi/ARBs use.
Despite its strengths, our study has several limitations, including the absence of precise information on ACEi/ARBs doses and the relatively high baseline Ishak fibrosis scores (≥2 in some, ≥3 in the vast majority) for the study cohort compared to other cohorts described previously in which the impact of ACEi/ARB use on histological progression of liver fibrosis was evaluated [13]. Thus, conceivably, if these agents exert their maximal antifibrogenic effects early in the fibrosis process, and this effect diminishes at later stages of fibrosis, our study would have missed such an effect. Furthermore, the HALT-C Trial was powered to assess the impact of long-term peginterferon alfa-2a use on a composite of fibrosis progression and clinical outcomes in 1,050 patients. A subset of 535 HALT-C patients met inclusion to our study, and 66 of them were continuously using ACEi/ARB with a relatively limited number of outcomes; hence, our study could have been underpowered to detect a difference in liver fibrosis progression with ACEi/ARB use.
However, given the strengths inherent to this study design and the high quality of the data on ACEi/ARB exposure and sequential histologic outcome provided by relying on the HALT-C Trial cohort, we conclude that ACEi/ARBs do not appear to have a beneficial effect on progression of hepatic fibrosis.
Abbreviations
- ACEi:
-
Angiotensin-converting enzyme inhibitors
- ARBs:
-
Angiotensin receptor blockers
- HALT-C:
-
Hepatitis C Long-term Treatment Against Cirrhosis
- HSC:
-
Stellate cells
- OR:
-
Odds ratio
- RAS:
-
Renin-angiotensin system
- SVR:
-
Sustained virologic response
References
Bataller R, Gines P, Nicolas JM, Gorbig MN, Garcia-Ramallo E, Gasull X. Angiotensin II induces contraction and proliferation of human hepatic stellate cells. Gastroenterology. 2000;118:1149–1156.
Bataller R, Gabele E, Schoonhoven R, Morris T, Lehnert M, Yang L. Prolonged infusion of angiotensin II into normal rats induces stellate cell activation and proinflammatory events in liver. Am J Physiol Gastrointest Liver Physiol. 2003;285:G642–G651.
Bataller R, Schwabe RF, Choi YH, Yang L, Paik YH, Lindquist J. Nadph oxidase signal transduces angiotensin II in hepatic stellate cells and is critical in hepatic fibrosis. J Clin Invest. 2003;112:1383–1394.
Bataller R, Sancho-Bru P, Gines P, Lora JM, Al-Garawi A, Sole M. Activated human hepatic stellate cells express the renin-angiotensin system and synthesize angiotensin II. Gastroenterology. 2003;125:117–125.
Yokohama S, Tokusashi Y, Nakamura K, Tamaki Y, Okamoto S, Okada M. Inhibitory effect of angiotensin II receptor antagonist on hepatic stellate cell activation in non-alcoholic steatohepatitis. World J Gastroenterol. 2006;12:322–326.
Wei HS, Li DG, Lu HM, Zhan YT, Wang ZR, Huang X. Effects of AT1 receptor antagonist, losartan, on rat hepatic fibrosis induced by CCL(4). World J Gastroenterol. 2000;6:540–545.
Yoshiji H, Kuriyama S, Yoshii J, Ikenaka Y, Noguchi R, Nakatani T. Angiotensin-II type 1 receptor interaction is a major regulator for liver fibrosis development in rats. Hepatology. 2001;34:745–750.
Jonsson JR, Clouston AD, Ando Y, Kelemen LI, Horn MJ, Adamson MD. Angiotensin-converting enzyme inhibition attenuates the progression of rat hepatic fibrosis. Gastroenterology. 2001;121:148–155.
Croquet V, Moal F, Veal N, Wang J, Oberti F, Roux J. Hemodynamic and antifibrotic effects of losartan in rats with liver fibrosis and/or portal hypertension. J Hepatol. 2002;37:773–780.
Kanno K, Tazuma S, Chayama K. AT1A-deficient mice show less severe progression of liver fibrosis induced by CCL(4). Biochem Biophys Res Commun. 2003;308:177–183.
Wei YH, Jun L, Jun L. Effect of losartan, an angiotensin II antagonist, on hepatic fibrosis induced by CCL4 in rats. Dig Dis Sci. 2004;49:1589–1594.
Yang L, Bataller R, Dulyx J, Coffman TM, Gines P, Rippe RA. Attenuated hepatic inflammation and fibrosis in angiotensin type 1a receptor deficient mice. J Hepatol. 2005;43:317–323.
Terui Y, Saito T, Watanabe H, Togashi H, Kawata S, Kamada Y. Effect of angiotensin receptor antagonist on liver fibrosis in early stages of chronic hepatitis C. Hepatology. 2002;36:1022.
Debernardi-Venon W, Martini S, Biasi F, Vizio B, Termine A, Poli G. AT1 receptor antagonist candesartan in selected cirrhotic patients: Effect on portal pressure and liver fibrosis markers. J Hepatol. 2007;46:1026–1033.
Yokohama S, Yoneda M, Haneda M, Okamoto S, Okada M, Aso K. Therapeutic efficacy of an angiotensin II receptor antagonist in patients with nonalcoholic steatohepatitis. Hepatology. 2004;40:1222–1225.
Rimola A, Londono MC, Guevara G, Bruguera M, Navasa M, Forns X. Beneficial effect of angiotensin-blocking agents on graft fibrosis in hepatitis C recurrence after liver transplantation. Transplantation. 2004;78:686–691.
Yoshiji H, Noguchi R, Fukui H. Combined effect of an ace inhibitor, perindopril, and interferon on liver fibrosis markers in patients with chronic hepatitis C. J Gastroenterol. 2005;40:215–216.
Corey KE, Shah N, Misdraji J, Abu Dayyeh BK, Zheng H, Bhan AK. The effect of angiotensin-blocking agents on liver fibrosis in patients with hepatitis C. Liver Int. 2009;29:748–753.
Di Bisceglie AM, Shiffman ML, Everson GT, Lindsay KL, Everhart JE, Wright EC. Prolonged therapy of advanced chronic hepatitis C with low-dose peginterferon. N Engl J Med. 2008;359:2429–2441.
Ishak K, Baptista A, Bianchi L, Callea F, De Groote J, Gudat F. Histological grading and staging of chronic hepatitis. J Hepatol. 1995;22:696–699.
Everhart JE, Wright EC, Goodman ZD, Dienstag JL, Hoefs JC, Kleiner DE. Prognostic value of Ishak fibrosis stage: Findings from the hepatitis C antiviral long-term treatment against cirrhosis trial. Hepatology. 2010;51:585–594.
Cholongitas E, Vibhakorn S, Lodato F, Burroughs AK. Angiotensin II antagonists in patients with recurrent hepatitis C virus infection after liver transplantation. Liver Int. 2010;30:334–335.
Acknowledgments
This study was supported by the National Institute of Diabetes & Digestive & Kidney Diseases (contract numbers are listed below). Additional support was provided by the National Institute of Allergy and Infectious Diseases (NIAID), the National Cancer Institute, the National Center for Minority Health and Health Disparities and by General Clinical Research Center and Clinical and Translational Science Center grants from the National Center for Research Resources, National Institutes of Health (grant numbers are listed below). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health. Additional funding to conduct this study was supplied by Hoffmann-La Roche, Inc., through a Cooperative Research and Development Agreement (CRADA) with the National Institutes of Health. In addition to the authors of this manuscript, the following individuals were instrumental in the planning, conduct and/or care of patients enrolled in this study at each of the participating institutions as follows: University of Massachusetts Medical Center, Worcester, MA: (Contract N01-DK-9-2326) Gyongyi Szabo, MD, Barbara F. Banner, MD, Maureen Cormier, RN, Donna Giansiracusa, RN. University of Connecticut Health Center, Farmington, CT: (Grant M01RR-06192) Herbert L. Bonkovsky, MD, Gloria Borders, RN, Michelle Kelley, RN, ANP. Saint Louis University School of Medicine, St Louis, MO: (Contract N01-DK-9-2324) Adrian M. Di Bisceglie, MD, Bruce Bacon, MD, Brent Neuschwander-Tetri, MD, Elizabeth M. Brunt, MD, Debra King, RN. Massachusetts General Hospital, Boston, MA: (Contract N01-DK-9-2319, Grant M01RR-01066; Grant 1 UL1 RR025758-01, Harvard Clinical and Translational Science Center) Andrea E. Reid, MD, Atul K. Bhan, MD, Wallis A. Molchen, David P. Lundmark. University of Colorado Denver, School of Medicine, Aurora, CO: (Contract N01-DK-9-2327, Grant M01RR-00051, Grant 1 UL1 RR 025780-01), Gregory T. Everson, MD, Thomas Trouillot, MD, Marcelo Kugelmas, MD, S. Russell Nash, MD, Jennifer DeSanto, RN, Carol McKinley, RN. University of California—Irvine, Irvine, CA: (Contract N01-DK-9-2320, Grant M01RR-00827) Timothy R. Morgan, MD, John C. Hoefs, MD, John R. Craig, MD, M. Mazen Jamal, MD, MPH, Muhammad Sheikh, MD, Choon Park, RN. University of Texas Southwestern Medical Center, Dallas, TX: (Contract N01-DK-9-2321, Grant M01RR-00633, Grant 1 UL1 RR024982-01, North and Central Texas Clinical and Translational Science Initiative) William M. Lee, MD, Thomas E. Rogers, MD, Peter F. Malet, MD, Janel Shelton, Nicole Crowder, LVN, Rivka Elbein, RN, BSN, Nancy Liston, MPH. University of Southern California, Los Angeles, CA: (Contract N01-DK-9-2325, Grant M01RR-00043) Karen L. Lindsay, MD, MMM, Sugantha Govindarajan, MD, Carol B. Jones, RN, Susan L. Milstein, RN. University of Michigan Medical Center, Ann Arbor, MI: (Contract N01-DK-9-2323, Grant M01RR-00042, Grant 1 UL1 RR024986, Michigan Center for Clinical and Health Research) Anna S. Lok, MD, Robert J. Fontana, MD, Joel K. Greenson, MD, Pamela A. Richtmyer, LPN, CCRC, R. Tess Bonham, BS. Virginia Commonwealth University Health System, Richmond, VA: (Contract N01-DK-9-2322, Grant M01RR-00065) Mitchell L. Shiffman, MD, Richard K. Sterling, MD, MSc, Melissa J. Contos, MD, A. Scott Mills, MD, Charlotte Hofmann, RN, Paula Smith, RN. Liver Diseases Branch, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, MD: Marc G. Ghany, MD, T. Jake Liang, MD, David Kleiner, MD, PhD, Yoon Park, RN, Elenita Rivera, RN, Vanessa Haynes-Williams, RN. National Institute of Diabetes and Digestive and Kidney Diseases, Division of Digestive Diseases and Nutrition, Bethesda, MD: James E. Everhart, MD, Leonard B. Seeff, MD, Patricia R. Robuck, PhD, Jay H. Hoofnagle, MD, Elizabeth C. Wright, PhD. University of Washington, Seattle, WA: (Contract N01-DK-9-2318) Chihiro Morishima, MD, David R. Gretch, MD, PhD, Minjun Chung Apodaca, BS, ASCP, Rohit Shankar, BC, ASCP, Natalia Antonov, M. Ed. New England Research Institutes, Watertown, MA: (Contract N01-DK-9-2328) Kristin K. Snow, MSc, ScD, Anne M. Stoddard, ScD, Teresa M. Curto, MSW, MPH. Armed Forces Institute of Pathology, Washington, DC: Zachary D. Goodman, MD, PhD. Data and Safety Monitoring Board Members: (Chair) Gary L. Davis, MD, Guadalupe Garcia-Tsao, MD, Michael Kutner, PhD, Stanley M. Lemon, MD, Robert P. Perrillo, MD.
Conflict of interest
Financial relationships of the authors with Hoffmann-La Roche, Inc., are as follows: R. T. Chung receives research support. Authors with no financial relationships related to this project are: B. K. Abu Dayyeh, M. Yang, and J. L. Dienstag.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study is conducted for the HALT-C Trial Group.
This is publication #58 of the HALT-C Trial.
Rights and permissions
About this article
Cite this article
Abu Dayyeh, B.K., Yang, M., Dienstag, J.L. et al. The Effects of Angiotensin Blocking Agents on the Progression of Liver Fibrosis in the HALT-C Trial Cohort. Dig Dis Sci 56, 564–568 (2011). https://doi.org/10.1007/s10620-010-1507-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-010-1507-8