Abstract
Radiation therapy has become one of the most important treatment modalities for human malignancy, but certain immediate and delayed side-effects on the normal surrounding tissues limit the amount of effective radiation that can be administered. After exposure of the abdominal region to ionizing radiation, nearly all patients experience transient symptoms of irradiation of the bowel. Acute-phase symptoms may persist for a short time, yet long-term complications can represent significant clinical conditions with high morbidity. Data from both experimental studies and clinical trials suggest the potential benefit for probiotics in radiation-induced enteritis and colitis. On the other hand, it is well evidenced that both useful and harmful effects of therapeutic applications of ionizing radiation upon living systems are ascribed to free-radical production. Therefore, the hypothesis that probiotics reinforce antioxidant defense systems of normal mucosal cells exposed to ionizing radiation may explain to an extent their beneficial action. The aim of this review is threefold: First, to make a short brief into the natural history of radiation injury to the intestinal tract. Second, to describe the primary interaction of ionizing radiation at the cellular level and demonstrate the participation of free radicals in the mechanisms of injury and, third, to try a more profound investigation into the antioxidant abilities of probiotics and prebiotics based on the available experimental and clinical data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, radiation therapy has formed a major part of the treatment regimen in various human malignancies, as well as being frequently applied in the palliative management of several other incurable ones. It is estimated that approximately 50–70% of all oncology patients are being treated with radiation therapy or a combination of chemotherapy and radiation therapy schedules [1, 2]. In order to eliminate most malignant tumors, ionizing radiation requires dose-fractionation regimens near the tolerance of the normal adjacent tissues. Despite recent technical advances and improvements in radiation therapy delivery procedures, normal tissue radiation toxicity remains an important drawback that limits the amount of effective ionizing radiation that can be administered [3]. Tissues containing rapid renewal cells like those of the bone marrow and the gastrointestinal mucosa demand fast cell proliferation and are therefore more susceptible to the toxic effects of ionizing radiation [4]. In this respect, radiation injury to the small and large intestine is among the most significant complications encountered in patients receiving ionizing radiation directed at the abdominal or pelvic cavity [5].
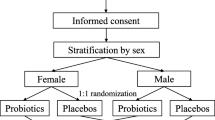
Ionizing radiation may affect normal tissues through direct cellular (e.g., clonogenic cell death, apoptotic cell death), direct functional (e.g., point mutations), and indirect injury processes [6]. However, most of the detrimental effects of ionizing radiation in biological systems occur mainly due to its indirect effects. Upon exposure to ionizing radiation, the dissipated energy interacts with intracellular water molecules causing decomposition, generating a burst of free radicals. These free radicals attack various intracellular biomolecules and bring about changes in their structure and function, thereby leading to lethal cellular injury [7]. Although the pathogenesis of radiation enteritis and colitis is not entirely clear, it was presumed to be an inflammatory process in which a large number of cell types, interacting molecular signals, including cytokines and growth factors, and various molecules on the endothelial cell surface participate. As a result, radiation enteritis is a complex interplay among a plethora of pathophysiological processes, including inflammation, epithelial regeneration, activation of the coagulation system, tissue remodeling, and collagen deposition [8, 9]. There is a generally accepted notion that both the useful effects of ionizing radiation upon malignant tumors and the harmful effects in normal tissues are largely mediated by the action of reactive oxygen species. Thus, an important challenge of modern radiation therapy is to develop pharmacological-dietary interventions capable of modifying the normal response of a biological system to ionizing radiation. Moreover, it has been observed that the protection of normal tissues may provide an increase in tumor control by allowing for an increase in the radiation dose [10, 11]. Various chemical compounds such as antioxidants and free-radical scavengers have been investigated as potential radioprotective agents. However, the inherent toxicity of these agents at the radioprotective doses warranted further search for safer and more effective radioprotectors [12, 13]. Accumulating evidence suggests that probiotics and prebiotics represent promising candidates for the prevention and control of several gastrointestinal disorders [14–20]. Recent experimental studies in animal models and clinical trials of patients with inflammatory bowel disease (IBD) have indicated that the oral administration of probiotics and prebiotics may effectively down-modulate the severity of intestinal inflammation [21–24]. Although there are still limited experimental data and clinical experience in human trials, these studies provide supporting evidence for the protective effects of probiotics in radiation induced intestinal injury [25–28]. While the mechanisms of radiation enteritis and probiotic/prebiotic actions continue to be under investigation, the hypothesis of underlying enhancement of cellular antioxidant defense should be thoroughly investigated.
Acute and Chronic Enteritis
According to the time of appearance, radiation enteropathy can be divided into two phases. Acute radiation enteritis (ARE) occurs either during or immediately following a course of radiation therapy. It is reported that approximately 80% of all patients undergoing abdominal-pelvic radiotherapy will manifest acute intestinal complications. Nausea, vomiting, abdominal pain, intermittent diarrhea that is often watery, and tenesmus are the most common symptoms of acute radiation enteritis [29, 30]. Diarrhea has been reported to result from a number of possible mechanisms, including bile salt malabsorption, bacterial overgrowth, and increased intestinal transit time. With diarrhea, the digestive and absorptive functions of the gastrointestinal (GI) tract are altered, resulting in malabsorption of protein, fat, lactose, bile salts, and vitamin B12 [31, 32]. Pathologically, the acute intestinal epithelium damage is described mainly as dilatation or destruction of crypt cell and decrease in villous height and number, ulceration, and severe mucosal and submucosal inflammation [4, 33]. Regeneration is active between the fractions, and because of the rapid turnover of intestinal mucosa, the acute-phase symptoms persist for hours to several days and may quickly pass with conservative management within 2–3 weeks after the completion of treatment [34]. Although acute effects of ionizing radiation on the intestinal mucosa are commonly observed, severe late sequelae are not. Chronic radiation enteritis (CRE) may develop from 3 months to 6 years after exposure to ionizing radiation and has been reported to occur in 40% of patients undergoing abdominal or pelvic radiotherapy [35]. Patients who had prominent acute symptoms during radiotherapy may have a greater incidence of long-term complications [2]. Chronic intestinal complications of radiation therapy are usually manifestations of obliterative vasculitis, which can produce mucosal ulceration and bowel wall thickening or progressive interstitial fibrosis of the different bowel tissues. The former leads to bleeding, intestinal perforation, enteric fistulas, or local abscesses and the latter to stricture formations and partial or complete intestinal obstruction [36]. These long-term complications proved to be most difficult to manage and most morbid to the patient. The reported incidence of severe late chronic radiation enteritis varies between 5 and 15% of patients treated with radiation [37]. Although some patients will develop chronic radiation enteritis without predisposing causes, several factors might help to increase the frequency. The development of CRE is basically dose-dependent. After an irradiation dose of 45 Gy, clinical manifestations of CRE will be observed in up to 5% of patients. With 65 Gy, 50% of all patients will develop symptoms of CRE [38]. Patients who had had previous abdominal or pelvic surgical operations are of greater risk for the development of CRE, presumably because the normal small intestine motility is altered and loops fixed by adhesions in the fields of radiation will receive a disproportionately greater share [39]. Additional risk factors include concomitant cardiovascular disease, atherosclerosis, diabetes, concurrent chemotherapy, elderly age, thin body physique, female sex, and tobacco abuse [40]. Histopathological features include mucosal atrophy, atypical hyperplastic or cystic glands, intestinal wall fibrosis, vascular sclerosis (most prominent in small arteries and arterioles), and lymphatic dilatation. Intestinal dysmotility causing proximal bacterial overgrowth may contribute to diarrhea and malabsorption [41]. Malnutrition is also a common finding in patients with CRE, mainly due to malabsorptive diarrhea, pseudo-obstructive crises and poor oral tolerance (especially to high-fat and high-fiber foods). Significant hypocalcemia and hypoproteinemia may often accompany the malabsorptive state. Often total parenteral nutrition (TPN) is necessary to maintain an optimal nutritional state [42]. The prognosis of patients with radiation enteropathy is poor. Corrective surgery is associated with high postoperative morbidity and mortality. In the long term, the majority of patients have persistent or recurrent symptoms, and about 10% of patients with radiation enteropathy die as a direct result of the disease [43]. It has been pointed out above that the incidence of adverse chronic effects is proportional to the severity of the acute symptoms. Therefore, it is of great importance to protect the intestinal mucosa from the acute phase of radiation injury [44]. Some scientists have proposed the use of mechanical attempts to exclude the small bowel from the radiation field or the administration of various radioprotective agents such as amifostine, sucralfate, arginine, glutamine, keratinocyte growth factor (KGF), and other elemental diets [45–50].
Acute and Chronic Radiation Colitis
Although the colonic mucosal cell mitotic rate is significantly less rapid than that of the small intestine, the colon remains an extremely radiosensitive organ [51]. Furthermore, the anatomic location of the rectum at the back of the prostate, and the close proximity of the sigmoid colon to the cervix, the uterus, and the bladder, make exposure of the rectosigmoid to significant radiation dose unavoidable. Similarly to radiation enteritis, radiation colitis can occur at two times after radiation therapy. Acute radiation colitis (ARC) usually appears within hours to 6 weeks of radiation exposure. The most common symptoms include diarrhea, tenesmus, mucoid rectal discharge, and rectal bleeding if ulceration is present. In spite of the relatively high incidence of these symptoms, ARC is self-limiting, and heals without specific treatment after 2–6 months [52]. This acute phase is like ARE secondary to destruction of actively dividing cells within the colonic epithelium. Histologically, mucosa shows thickening with edematous lamina propria, patchy fibroblastic proliferation, and decreased mitotic rate. As the mucosa recovers from this insult, regenerative atypia can be seen [53]. The appearance of chronic radiation colitis (CRC) symptoms may be as early as 3 months after radiation therapy or delayed up to 2 years. In accordance to CRE, the severity of CRC syndrome seems to be related to the severity of the acute episode [54]. Chronic radiation colitis is established clinically as a constellation of symptoms, including diarrhea, tenesmus, mucoid rectal discharge, rectal bleeding, constipation, and less commonly low-grade obstruction or fistulous tract formation into adjacent organs [55]. Extensive complications such as strictures, abscesses, and fistula formation, often require surgical intervention at a frequency ranging from 2 to 17% [56]. Controversial clinical data have been reported concerning the best surgical management for CRE and CRC. Some surgeons advocated intestinal resection, while others proposed a more conservative management [57]. Bleeding may be minimal to chronic and severe, requiring blood transfusion. The incidence of rectal bleeding ranges between 1 and 20% [58]. Importantly, CRC is a precancerous lesion: Radiation-associated secondary rectal cancer originates mainly from the direct functional effects of ionizing radiation (such as point mutations) to the DNA and the following dysplasia and has a tendency to be diagnosed at an advanced stage and to bear a dismal prognosis [59]. In summary, ARE and ARC are common side-effects of abdominopelvic radiotherapy and usually transient with symptomatic management without interruption of radiation therapy treatments. However, the patients who develop these short-term acute manifestations are most likely to develop delayed-chronic complications. These chronic complications are life-threatening for the long-term cancer survivors and their management remains a major challenge for the clinicians.
Radiation Induced Oxidative Damage to Normal Tissues
Ionizing radiation exerts its therapeutic benefit by affecting directly or indirectly the synthesis of the DNA chain in cells undergoing mitosis, particularly by the generation of oxygen-free radicals. Because neoplastic cells are generally undifferentiated and stem-cell-like, they reproduce rapidly, and have a diminished ability to repair sub-lethal damage compared to differentiated cells [60]. However, intestinal mucosa also has a relatively high mitotic rate, which makes it vulnerable to ionizing radiation directed to the abdominal and pelvic cavity [61]. Upon exposure to ionizing radiation, the dissipated energy interacts with intracellular water causing decomposition of H2O molecules, and generation of hydrogen radicals (H·) and hydroxyl radicals (HO·) [62]. These in turn recombine to produce a variety of other free radicals. Hydroxyl radicals (OH·) are highly reactive and consequently short-lived. Hydrogen radical (H·) has been suggested to yield superoxide radical (O ·−2 ) in the presence of oxygen [63]. Previous attempts to prevent free-radical production had been directed to reduce local blood flow and tissue oxygen tension [64]. Superoxide radical (O ·−2 ) is not particularly reactive by itself, but can further interact with water and produce hydroperoxyl radical (HO ·2 ), which is much more reactive, and hydrogen peroxide (H2O2) [65]. The nitric oxide (NO) molecule is another free radical exhibiting a variety of beneficial effects in the gut [66]. However, sustained levels of NO production, as observed in inflammatory conditions, may result in direct tissue toxicity. Particularly in radiation enteritis, increased NO synthesis has been observed, derived from the inducible isoform of NO synthase (iNOS). This result suggests that the NO pathway contributes to the inflammatory response of radiation enteritis [67, 68]. Recent evidence indicates that most of the toxicity attributed to NO is rather due to peroxynitrite. The formation of peroxynitrite (ONOO−) has been ascribed to the diffusion-controlled reaction between nitric oxide free radical (NO·) and superoxide radical (O ·−2 ). The resultant pairing of these two free radicals forms peroxynitrite anion (ONOO−), a molecule that itself is not a free radical, but is a powerful oxidant [69]. Reactive oxygen species (ROS) act together with reactive nitrogen species (RNS) to damage cells, causing a situation known as oxidative/nitrosative stress. Therefore, these two species are often collectively referred to as ROS/RNS [70]. Excessive ROS/RNS production is a harmful process which can lead by several ways to significant cellular damage. They may trigger chemical chain reactions with all major cellular macromolecules such as DNA, proteins, and membrane lipids. DNA is affected with a variety of lesions including oxidized bases, abasic sites, stand brakes, as well as DNA–DNA and DNA–protein cross-links [71]. Oxidative damage to proteins is characterized by formation of carbonyl groups (e.g., meta-tyrosine and ortho-tyrosine formation from phenylalanine), and is a highly damaging event [72]. Particularly, hydroxyl radical (OH·) depolymerizes hyaluronic acid, degrades collagen, inactivates essential enzymes and transport proteins via sulfhydryl oxidation, and also nicks nucleic acids. In addition, RNS may induce nitration of tyrosine residues of proteins [73]. Lipid peroxidation is the oxidative degradation of membrane lipids. Polyunsaturated fatty acids, when exposed to ROS and particularly to hydroxyl radical (OH·), can be oxidized to lipid hydroperoxides that decompose to yield hydrocarbons and reactive aldehydes, such as malondialdehyde (MDA) and 4-hydroxynoneal in the presence of metals [74]. This lipid peroxidation can cause severe impairment of membrane function through changes in membrane permeability and fluidity, and membrane protein oxidation, ultimately leading to cell lysis [75]. These reactions, caused by overwhelming oxidative stress, may lead to either lethal cellular injuries or may result in the initiation of apoptosis [76]. Moreover, it must be noted that radiolysis of water molecules is not the only reason for ROS production. Ionizing radiation can affect interactions between different cellular systems. An early inflammatory response appears just a few hours after irradiation, and is characterized by leukocyte infiltration into the irradiated organs.
The development of an inflammatory response is a finely regulated process that involves sequential leukocyte-endothelial cell interactions. An increase in oxygen radical production in the vascular wall has been documented as early as 2 h after irradiation with a more intense oxidant stress observed at 6 h, this second burst being produced mainly by infiltrating inflammatory cells [77]. Radiation-induced fibroatrophic process (RIF) constitutes a late, local, and unavoidable sequela to high-dose radiotherapy, related to the development of CRE and CRC. Evidence suggests involvement of reactive oxygen species (ROS), and fibroblasts, mediated by TGF-β1 [78]. Since ROS/RNS are highly reactive and thus have a too brief half-life, the approach most often employed in the study of oxidative stress is assessing the presence and quantity of the oxidative biomarkers of lipids (e.g., malondialdehyde), antioxidant biomarkers (e.g., glutathione, catalase), nitrosive biomarkers (e.g., 3-nitrotyrosine), and inflammatory biomarkers (e.g., myeloperoxidase/neutrophils) [79].
Probiotics, Prebiotics, and Synbiotics
Probiotics are defined as living microorganisms in food and dietary supplements which, upon ingestion, beneficially affect the host by selectively stimulating the growth and/or activity of one or limited number of bacteria in the colon [80]. Prebiotics are defined as non-digestible dietary carbohydrates, e.g. lactulose, lactosucrose, fructo-and galacto-oligosaccharides, inulin, which upon consumption, stimulate the growth and metabolism of endogenous protective bacteria. Beneficial effects of prebiotics are also associated with the generation of short-chain fatty acids (SCFA) due to fermentation by colonic bacteria [81]. SCFA may effectively protect intestinal structure against radiation-induced damage by improving mucosal integrity [82]. Synbiotics are defined as mixtures of probiotics and prebiotics that beneficially affect host intestinal health with their reinforced synergistic action [83]. Most of the interactions between probiotic bacteria and inflamed intestinal mucosa have been best highlighted in animal models of inflammatory bowel disease. These interactions may also hold true for the intestinal epithelial response to radiation induced injury. In fact, the two inflammatory processes correspond regarding the pathological progress and clinical outcome. Both IBD and radiation enteritis are characterized by the involvement of reactive oxygen species in the pathogenesis of intestinal inflammation [84]. Moreover, certain mucosal cytokines are activated in a similar way in both diseases. Indeed the mucosal levels of interleukins IL-1β, IL-2, IL-6, and IL-8 are significantly higher, while the tumor necrosis factor-alpha (TNF-α) level is also significantly elevated both in patients with IBD and radiation colitis [85]. In support of this, similar systemic and topical drugs are clinically used to alleviate the manifestations of inflammatory bowel disease and radiation colitis. Therefore, probiotics and prebiotics may also act in a similar way.
The Role of Probiotics and Prebiotics in Intestinal Antioxidant Defense Mechanisms
Against oxidative stress, aerobic cells like those of intestinal mucosa are equipped with a complex antioxidant defense system which includes enzymatic and non-enzymatic components having synergistic and interdependent effects on each other. The inherent antioxidant enzymatic network includes proteins, such as superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GSH-Px), glutathione reductase (GR), and glutathione-s-transferase (GST), while non-enzymatic antioxidant defense consists of low-molecular-weight antioxidant molecules acting mainly as free-radical scavengers, such as glutathione (GSH), α-tocopherol (vitamin E), ascorbic acid (vitamin C) and melatonin [86, 87]. Under normal conditions, this antioxidant defense system protects the cells from oxidative damage, but under excessive oxidant-generating conditions may become insufficient. Ionizing radiation is a well-recognized factor to cause downregulation of the antioxidant defense mechanisms in the intestinal mucosa [88]. It has been observed to decrease the activities of SOD, GSH-Px, and CAT, and reduce the intracellular concentration of GSH. A possible explanation for this phenomenon may be due to their increased utilization by the enhanced ROS production [89]. As mentioned above, superoxide dismutase (SOD) is an enzymatic antioxidant. The physiological importance of SOD is the disproportionation of superoxide anion (O2−) to oxygen (O2) and hydrogen peroxide (H2O2). Superoxide dismutase SOD is considered as the first line of defense against oxygen-derived free radicals [90]. Recent experimental data indicate that treatment with SOD significantly reduces peroxidation reactions in the inflamed colon and affords significant amelioration of colonic inflammatory changes in a rat model of trinitrobenzene sulphonic acid (TNBS) colitis [91]. In addition, treatment with SOD decreases oxidative stress and adhesion molecule upregulation in response to abdominal irradiation in mice. This observation is associated with an attenuation of the radiation-induced intestinal inflammatory response [92]. Despite these promising results, the therapeutic application of SOD is limited, mainly due to its short circulatory half-life of only 5–10 min, which restricts its bioavailability. In order to resolve this problem, efforts have been made to find suitable vehicles for SOD. Probiotic species capable of local delivery of SOD open a novel approach in bowel diseases characterized from ROS production. In a relevant study, genetically engineered species of Lactobacillus plantarum and Lactococcus lactis capable of producing and releasing SOD were found to exhibit antiinflammatory effects in the TNBS colitis model, and offer clear-cut advantages over continuous infusion of bovine SOD [93]. Another experimental study demonstrated that Lactobacillus gasseri producing manganese SOD had significant anti-inflammatory activity reducing the severity of colitis in IL-10-deficient mice [94]. Microbiological laboratory findings from two studies indicated that two strains of Lactobacillus fermentum, named E-3 and E-18, and Streptococcus thermophilus showed significant antioxidative activity due to production of SOD [95, 96].
Catalase is another major enzymatic antioxidant that catalyzes the decomposition of hydrogen peroxide into water and oxygen. Although lactic acid bacteria are generally catalase-negative, an experimental study of dimethylhydrazine-induced colon carcinogenesis in mice revealed a catalase-producing Lactobacillus lactis strain able to prevent tumor appearance [97]. Similar expectations about beneficial effects of specific probiotic strains may also hold true for the case of radiation-induced oxidative stress in the intestine.
Apart from engineering recombinant probiotic strains capable of producing antioxidative enzymes, the development of probiotics with secretory properties of non-enzymatic antioxidant molecules with free-radical scavenging activity is also of great interest. One of the most important intracellular non-enzymatic antioxidant molecules is glutathione (GSH). Glutathione is a tripeptide that contains a sulfhydryl group (–SH) and is highly efficient in detoxifying ROS and peroxides. In the oxidative chain reaction, GSH is converted to its oxidized form glutathione disulfide (GSSG). One of the most essential functions of GSH is to act as hydroxyl radical (OH·) scavenger since the hydroxyl radical cannot be eliminated by an enzymatic reaction [98]. In addition, the antioxidant selenoprotein glutathione peroxidase (GSH-Px) catalyzes the reaction of GSH with lipidic (LOOH) or nonlipidic (ROOH) hydro peroxides as well as hydrogen peroxide (H2O2) to CSSG and their corresponding alcohols LOH, ROH, and H2O, respectively. Glutathione disulfide (CSSG) is then reduced back to GSH by the antioxidant enzyme glutathione reductase (GR). Consequently, at sufficiently high radiation doses, GSH becomes depleted, leaving highly reactive ROS to react with critical cellular biomolecules and cause tissue damage. Hence, the concentration of intracellular GSH is the key determinant of the extent of radiation-induced intestinal injury.
Both clinical and experimental evidence confirm the important role of GSH in the maintenance of intestinal mucosal integrity. Firstly, the inflammatory status in patients suffering from ulcerative colitis and Crohn’s colitis is associated with its depletion [99]. Secondly, glutathione supplementation improved colonic damage, restored glutathione levels, and decreased spectacularly lipid peroxidation in a rat model of TNBS colitis [100]. However, oral administration of GSH-even in very large doses (3 g)—is difficult to increase its systematic availability in order to reach circulating beneficial levels [101]. On the other hand, various thiol antioxidants and GSH precursors such as cysteine, N-acetylcysteine, N-acetylcysteine amide (NACA), and cysteamine have been shown to protect rodents against the harmful effects of radiation. Their application, however, has been limited by their toxic side-effects [13, 102].
Another interesting aspect is the relation between GSH concentration and fibrosis mediated by transforming growth factor-beta TGF-β. TGF-β is the most potent and ubiquitous profibrogenic cytokine, and its expression is increased in almost all the fibrotic diseases and in experimental fibrosis models [103]. An experimental study indicated increased expression of TGF-β in radiation enteropathy and concluded that this observation was related to the chronicity of radiation enteropathy [104]. Moreover, TGF-β increases ROS production and decreases the concentration of GSH. Recent findings address the potential mechanism whereby oxidative stress mediates fibrogenesis induced by TGF-β and the potential therapeutic value of GSH and its precursors in fibrotic diseases [105].
Considering all of the above, probiotic strains able to directly produce or promote the intestinal release of glutathione could have potential therapeutic value. A laboratory study investigated GSH concentrations in probiotics belonging to the genera Bifidobacterium and Lactococcus [106]. Furthermore, in another animal study, oral administration of the probiotic strain Lactobacillus fermentum, a microorganism that has been demonstrated in vitro to produce GSH and its precursor the dipeptide γ-Glu-Cys facilitates the recovery of the inflamed tissue in the TNBS model of rat colitis, an effect associated with an increase in the production of some mediators involved in the inflammatory response of the intestine [107]. In addition, two recent experimental studies demonstrated that multispecies probiotics {Lactobacillus acidophilus (W70), L. casei (W56), L. salivarius (W24), Lactococcus lactis (W58), Bifidobacterium bifidum (W23), and B. lactis (W52)} enhanced de novo synthesis of GSH and increased GSH content locally in the pancreas as well as systemically after pretreatment in a well-established model of severe acute pancreatitis. These observations were associated with reduced activation of inflammation and acinar cell injury, and concluded that probiotic pre-treatment diminished acute pancreatitis-induced intestinal barrier dysfunction and prevented oxidative stress via mechanisms mainly involving mucosal GSH biosynthesis [108, 109]. To the best of our knowledge, there is no experimental study that has investigated the relationship between radiation enteritis and colitis and glutathione or probiotics capable for local delivery of GSH.
Other important molecules produced by some probiotics, which may be potentially useful for oxidative stress reduction in the intestine, are the exopolysaccharides (EPSs). Exopolysaccharides constitute long-chain polysaccharides consisting of branched, repeating units of sugars or sugar derivatives, such as galactose, glucose, and rhamnose, that probiotic bacteria release into the surrounding environment to protect themselves under starvation conditions and also at extreme pH and temperature. Various health benefits have been attributed to EPSs. Recently, a biotechnology study reported the time course of the extracellular biosynthesis of an EPS by the probiotic bacterium Bacillus coagulans RK-02 and proved that this EPS exhibited significant in vitro antioxidant and free-radical scavenging activities when compared to standard antioxidants such as vitamin C and vitamin E [110]. Another experimental study compared the efficacy of the high-EPS producing probiotic Lactobacillus delbrueckii subsp. Bulgaricus B3 strain with the low-EPS producing probiotic Lactobacillus delbrueckii subsp. Bulgaricus A13 strain in a rat model of acetic acid colitis. Both strains attenuated the severity of experimental colitis, but the oxidative biomarker MPO was lower in the high-EPS producing group. These results concluded that exopolysaccharide-producing probiotics significantly improved experimental colitis, which may be mediated by EPS in a dose-dependent manner [111].
Probiotics apart from producing substances with antioxidant and free-radical scavenging activities also exhibit to a degree, metal chelating activities. Metal ions may correlate with the pathogenesis of various chronic diseases such as coronary heart disease, carcinogenesis, and arthritis, mainly by promoting free-radical production. It was mentioned earlier that transition metal ions can initiate lipid peroxidation and start a chain reaction by means of decomposition of hydroperoxides (ROOH) to peroxyl (ROO·) and alkyoxyl (RO·) radicals. Among many ions playing catalytic roles in free-radical chain reactions, iron and cooper ions are highly reactive. The chelating ability of 19 lactic acid bacteria toward Cu2+ and Fe2+ ions was investigated in a study, which indicated that probiotics exhibit, to an extent, metal chelating activity. However, Streptococcus thermophilus 821 and Bifidobacterium longum 15708 demonstrated the highest Fe2+ and Cu2+ chelating ability, respectively [112]. According to another laboratory study, the antioxidant activity of probiotic Lactobacillus plantarum KCTC 3099 was compared with Lactobacillus rhamnosus GG. In order to define the antioxidative mechanism, superoxide dismutase (SOD) and metal ion chelating activities were determined. The result demonstrated little SOD activity for Lactobacillus plantarum KCTC 3099, but a higher level of chelating activity for both Fe2+ and Cu2+ metal ions [113].
Probiotic bacteria exhibit antioxidant activities in all major ways. They may reinforce the inherent cellular antioxidant defense by secreting enzymes like SOD. They also release and promote the production of the major non-enzymatic antioxidant and free-radical scavenger GSH. Moreover, they promote the production of certain antioxidant biomolecules, such as the EPSs, and, finally, they exhibit metal chelating activities. All these data suggest that probiotics may have a potential therapeutic role in ROS-characterized gastrointestinal disorders. However, there is a need for further investigation both in animal models and human trials in order to confirm the idea that individual probiotic bacteria strains may concretely affect beneficially the pathogenesis and the natural history of radiation-induced enteritis and colitis.
Conclusions
The goal of radiation treatment is to deliver precisely measured doses of ionizing radiation to a defined tumor volume with the minimum acceptable injurious effects to the surrounding healthy tissues. However, radiation injury to the intestine will remain a major obstacle to the treatment of abdominal and pelvic malignancies with radiotherapy and continues to adversely impact the quality of life of long-term cancer survivors. Since radiotherapy is now used with increased frequency for solid organ neoplasms of the abdomen and pelvis, the incidence of radiation enteritis and colitis is likely to increase in the future. It is generally accepted that radiation therapy exerts its beneficial effects in the eradication of neoplastic cells through irretrievable cellular injuries due to free-radical production. The same mechanism has been proposed for the alterations observed in the normal adjacent tissues. Quite recently, experimental studies in animal models have pointed out to some degree the protective effects of probiotics in radiation-induced intestinal injury. Human clinical studies have long noted the benefits of probiotic bacteria in the symptomatic management of radiation enteropathy. In the light of these findings, probiotics may play a key role in the enhancement of host intestinal antioxidant defense systems. Additionally, these studies demonstrated excellent safety of probiotics and lack of serious side-effects, even in the setting of intestinal inflammation. As a result, probiotic bacteria with the ability to secrete extracellularly antioxidant compounds or to promote intracellular enforcement of antioxidant systems are close enough to fulfill the criteria of the ideal intestinal radioprotector. Through genetic engineering, it is now possible not only to strengthen the effects of existing strains but also to create completely new probiotics able to directly produce or promote the intestinal release of specific agents. Now it is more obvious than before that in order to create efficient strategies for modification of intestinal radiation responses, it is required to strengthen collaborative research between several medical disciplines and pharmaceutical and biotechnology scientists.
References
Ballas LK, Elkin EB, Schrag D, Minsky BD, Bach PB. Radiation therapy facilities in the United States. Int J Radiat Oncol Biol Phys. 2006;66:1204–1211.
Wang J, Boerma M, Fu Q, Hauer-Jensen M. Significance of endothelial dysfunction in the pathogenesis of early and delayed radiation enteropathy. World J Gastroenterol. 2007;13:3047–3055.
Vozenin-Brotons MC. Tissue toxicity induced by ionizing radiation to the normal intestine: understanding the pathophysiological mechanisms to improve the medical management. World J Gastroenterol. 2007;13:3031–3032.
Berthrong M. Pathologic changes secondary to radiation. World J Surg. 1986;10:155–170.
Bismar MM, Sinicrope FA. Radiation enteritis. Curr Gastroenterol Rep. 2002;4:361–365.
Stone HB, Coleman CN, Anscher MS, McBride WH. Effects of radiation on normal tissue: consequences and mechanisms. Lancet Oncol. 2003;4:529–536.
Akpolat M, Kanter M, Uzal MC. Protective effects of curcumin against gamma radiation-induced ileal mucosal damage. Arch Toxicol. 2009;83:609–617.
Denham JW, Hauser-Jensen M. The radiotherapeutic injury-a complex ‘wound’. Radiother Oncol. 2002;63:129–145.
Zhao W, Robbins ME. Inflammation and chronic oxidative stress in radiation-induced late normal tissue injury: therapeutic implications. Curr Med Chem. 2009;16:130–143.
Weiss JF, Landauer MR. Radioprotection by antioxidants. Ann NY Acad Sci. 2000;899:44–60.
Weiss JF. Pharmacologic approaches to protection against radiation-induced lethality and other damage. Environ Health Perspect. 1997;105:1473–1478.
Nair CKK, Parida DK, Nomura T. Radioprotectors in radiotherapy. J Radiat Res. 2001;42:21–37.
Wu W, Abraham L, Ogony J, Matthews R, Goldstein G, Ercal N. Effects of N-acetylcysteine amide (NACA), a thiol antioxidant on radiation-induced cytotoxicity in Chinese hamster ovary cells. Life Sci. 2008;82:1122–1130.
Sazawal S, Hiremath G, Dhingra U, Malik P, Deb S, Black RE. Efficacy of probiotics in prevention of acute diarrhoea: a meta-analysis of masked, randomized, placebo-controlled trials. Lancet Infect Dis. 2006;6:374–382.
Johnson-Henry KC, Mitchell DJ, Avitzur Y, Galindo-Mata E, Jones NL, Sherman PM. Probiotics reduce bacterial colonization, gastric inflammation in H. pylori-infected mice. Dig Dis Sci. 2004;49:1095–1102.
Kukkonen K, Savilahti E, Haahtela T, et al. Probiotics and prebiotic galacto-oligosaccharides in the prevention of allergic diseases: a randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol. 2007;119:192–198.
Madsen KL. The use of probiotics in gastrointestinal disease. Can J Gastroenterol. 2001;15:817–822.
Fotiadis CI, Stoidis CN, Spyropoulos BG, Zografos ED. Role of probiotics, prebiotics and synbiotics in chemoprevention for colorectal cancer. World J Gastroenterol. 2008;14:6453–6457.
Wollowski I, Rechkemmer G, Pool-Zobel BL. Protective role of probiotics and prebiotics in colon cancer. Am J Clin Nutr. 2001;73:451S–455S.
Barbara G, Stanghellini V, Cremon C, et al. Probiotics and irritable bowel syndrome: rationale and clinical evidence for their use. J Clin Gastroenterol. 2008;42:S214–S217.
Ewaschuk JB, Dieleman LA. Probiotics and prebiotics in chronic inflammatory bowel diseases. World J Gastroenterol. 2006;12:5941–5950.
Peran L, Sierra S, Comalada M, et al. A comparative study of the preventative effects exerted by two probiotics, Lactobacillus reuteri and Lactobacillus fermentum, in the trinitrobenzenesulfonic acid model of rat colitis. Br J Nutr. 2007;97:96–103.
Peran L, Camuesco D, Comalada M, et al. Preventative effects of a probiotic, Lactobacillus salivarius ssp. salivarius, in the TNBS model of rat colitis. World J Gastroenterol. 2005;11:5185–5192.
Guarner F, Malagelada JR. Role of bacteria in experimental colitis. Best Pract Res Clin Gastroenterol. 2003;17:793–804.
Seal M, Naito Y, Barreto R, Lorenzetti A, Safran P, Marotta F. Experimental radiotherapy-induced enteritis: a probiotic interventional study. J Dig Dis. 2007;8:143–147.
Demirer S, Aydintug S, Aslim B, et al. Effects of probiotics on radiation-induced intestinal injury in rats. Nutrition. 2006;22:179–186.
Delia P, Sansotta G, Donato V, et al. Use of probiotics for prevention of radiation-induced diarrhea. World J Gastroenterol. 2007;13:912–915.
Ciorba MA, Stenson WF. Probiotic therapy in radiation-induced intestinal injury and repair. Ann NY Acad Sci. 2009;1165:190–194.
Smith DH, DeCosse JJ. Radiation damage to the small intestine. World J Surg. 1986;10:189–194.
Andreyev J. Gastrointestinal symptoms after pelvic radiotherapy: a new understanding to improve management of symptomatic patients. Lancet Oncol. 2007;8:1007–1017.
Cengiz M, Akbulut S, Atahan IL, Grigsby PW. Acute phase response during radiotherapy. Int J Radiat Oncol Biol Phys. 2001;46:1093–1096.
Westergaard H. Bile acid malabsorption. Curr Treat Options Gastroenterol. 2007;10:28–33.
Erbil Y, Oztezcan S, Giriş M, et al. The effect of glutamine on radiation-induced organ damage. Life Sci. 2005;78:376–382.
Cho LC, Antoine JE. Radiation injury to the gastrointestinal tract. In: Feldman M, Friedman LS, Sleisenger MH, eds. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease. 8th ed. Philadelphia: WB Saunders; 2006:813–826.
Turina M, Mulhall AM, Mahid SS, Yashar C, Galandiuk S. Frequency and surgical management of chronic complications related to pelvic radiation. Arch Surg. 2008;143:46–52.
Galland RB, Spencer J. Natural history and surgical management of radiation enteritis. Br J Surg. 1987;74:742–747.
Abayomi J, Kirwan J, Hackett A. The prevalence of chronic radiation enteritis following radiotherapy for cervical or endometrial cancer and its impact on quality of life. Eur J Oncol Nurs. 2009;13:262–267.
Regimbeau JM, Panis Y, Gouzi JL, Fagniez PL. Operative and long-term results after surgery for chronic radiation enteritis. Am J Surg. 2001;182:237–242.
Hauser-Jensen M, Wang J, Denham JW. Bowel injury: current and evolving management strategies. Semin Radiat Oncol. 2003;13:357–371.
Cox JD, Byhardt RW, Wilson JF, Haas JS, Komaki R, Olson LE. Complications of radiation therapy and factors in their prevention. World J Surg. 1986;10:171–188.
Rubio CA, Jalnas M. Dose-time-dependent histological changes following irradiation of the small intestine of rats. Dig Dis Sci. 1996;41:392–401.
Gavazzi C, Bhoori S, Lovullo S, Cozzi G, Mariani L. Role of home parenteral nutrition in chronic radiation enteritis. Am J Gastroenterol. 2006;101:374–379.
Muttillo IA, Elias D, Bolognese A, et al. Surgical treatment of severe late radiation injury to the bowel: a retrospective analysis of 83 cases. Hepatogastroenterology. 2002;49:1023–1026.
Dörr W, Hendry JH. Consequential late effects in normal tissues. Radiother Oncol. 2001;61:223–231.
Matsuu-Matsuyama M, Shichijo K, Okaichi K, et al. Sucralfate protects intestinal epithelial cells from radiation-induced apoptosis in rats. J Radiat Res (Tokyo). 2006;47:1–8.
Hwang JM, Chan DC, Chang TM, et al. Effects of oral arginine and glutamine on radiation-induced injury in the rat. J Surg Res. 2003;109:149–154.
Ersin S, Tuncyurek P, Esassolak M, et al. The prophylactic and therapeutic effects of glutamine- and arginine-enriched diets on radiation-induced enteritis in rats. J Surg Res. 2000;89:121–125.
Waddell BE, Rodriguez-Bigas MA, Lee RJ, Weber TK, Petrelli NJ. Prevention of chronic radiation enteritis. J Am Coll Surg. 1999;189:611–624.
Ben-Josef E, Han S, Tobi M, et al. Intrarectal application of amifostine for the prevention of radiation-induced rectal injury. Semin Riadiat Oncol. 2002;12:81–85.
Giriş M, Erbil Y, Oztezcan S, et al. The effect of heme oxygenase-1 induction by glutamine on radiation-induced intestinal damage: the effect of heme oxygenase-1 on radiation enteritis. Am J Surg. 2006;191:503–509.
Diestel CF, Marques RG, Lopes-Paulo F, et al. Role of l-glutamine and glycine supplementation on irradiated colonic wall. Int J Colorectal Dis. 2007;22:1523–1529.
Johnston MJ, Robertson GM, Frizelle FA. Management of late complications of pelvic radiation in the rectum and anus: a review. Dis Colon Rectum. 2003;46:247–259.
Hovdenak N, Fajardo LF, Hauser-Jensen M. Acute radiation proctitis: a sequential clinicopathologic study during pelvic radiotherapy. Int J Radiat Oncol Biol Phys. 2000;48:1111–1117.
Wang CJ, Leung SW, Chen HC, et al. The correlation of acute toxicity and late rectal injury in radiotherapy for cervical carcinoma: evidence suggestive of consequential late effect (CQLE). Int J Radiat Oncol Biol Phys. 1998;40:85–91.
Babb RR. Radiation proctitis: a review. Am J Gastroenterol. 1996;91:1309–1311.
Kountouras J, Zavos C. Recent advances in the management of radiation colitis. World J Gastroenterol. 2008;14:7289–7301.
Tagkalidis PP, Tjandra JJ. Chronic radiation proctitis. ANZ J Surg. 2001;71:230–237.
Williams HR, Vlavianos P, Blake P, Dearnaley DP, Tait D, Andreyev HJ. The significance of rectal bleeding after pelvic radiotherapy. Aliment Pharmacol Ther. 2005;21:1085–1090.
Tamai O, Nozato E, Miyazato H, et al. Radiation-associated rectal cancer: report of four cases. Dig Surg. 1999;16:238–243.
Gillette EL, Gillette SM. Principles of radiation therapy. Semin Vet Med Surg (Small Anim). 1995;10:129–134.
Thomson A, Hemphill D, Jeejeebhoy KN. Oxidative stress and antioxidants in intestinal disease. Dig Dis. 1998;16:152–158.
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39:44–84.
Abou-Seif MA, El-Naggar MM, El-Far M, Ramadan M, Salah N. Amelioration of radiation-induced oxidative stress and biochemical alteration by SOD model compounds in pre-treated gamma-irradiated rats. Clin Chim Acta. 2003;337:23–33.
Empey LR, Papp JD, Jewell LD, Fedorak RN. Mucosal protective effects of vitamin E and misoprostol during acute radiation-induced enteritis in rats. Dig Dis Sci. 1992;37:205–214.
De Grey AD. HO2*: the forgotten radical. DNA Cell Biol. 2002;21:251–257.
Sobko T, Reinders C, Norin E, Midtvedt T, Gustafsson LE, Lundberg JO. Gastrointestinal nitric oxide generation in germ-free and conventional rats. Am J Physiol Gastrointest Liver Physiol. 2004;287:G993–G997.
Freeman SL, MacNaughton WK. Ionizing radiation induces iNOS-mediated epithelial dysfunction in the absence of an inflammatory response. Am J Physiol Gastrointest Liver Physiol. 2000;278:G243–G250.
Erbil Y, Dibekoglu C, Turkoglu U, et al. Nitric oxide and radiation enteritis. Eur J Surg. 1998;164:863–868.
Pacher P, Beckman JS, Liaudet L. Nitric oxide and peroxynitrite in health and disease. Physiol Rev. 2007;87:315–324.
Kilciksiz S, Demirel C, Erdal N, et al. The effect of N-acetylcysteine on biomarkers for radiation-induced oxidative damage in a rat model. Acta Med Okayama. 2008;62:403–409.
Barker S, Weinfeld M, Zheng J, Li L, Murray D. Identification of mammalian proteins cross-linked to DNA by ionizing radiation. J Biol Chem. 2005;280:33826–33838.
Stadtman ER. Protein oxidation and aging. Science. 1992;257:1220–1224.
Taysi S, Koc M, Büyükokuroğlu ME, Altinkaynak K, Sahin YN. Melatonin reduces lipid peroxidation and nitric oxide during irradiation-induced oxidative injury in the rat liver. J Pineal Res. 2003;34:173–177.
Valko M, Morris H, Cronin MT. Metals, toxicity and oxidative stress. Curr Med Chem. 2005;12:1161–1208.
Marnett LJ. Oxy radicals, lipid peroxidation and DNA damage. Toxicology. 2002;181–182:219–222.
Matés JM, Sánchez-Jiménez FM. Role of reactive oxygen species in apoptosis: implications for cancer therapy. Int J Biochem Cell Biol. 2000;32:157–170.
Molla M, Panes J. Radiation-induced intestinal inflammation. World J Gastroenterol. 2007;13:3043–3046.
Robbins ME, Zhao W. Chronic oxidative stress and radiation-induced late normal tissue injury: a review. Int J Radiat Biol. 2004;80:251–259.
Hwang ES, Kim GH. Biomarkers for oxidative stress status of DNA, lipids, and proteins in vitro and in vivo cancer research. Toxicology. 2007;229:1–10.
Kligler B, Cohrssen A. Probiotics. Am Fam Physician. 2008;78:1073–1078.
Lomax AR, Calder PC. Prebiotics, immune function, infection and inflammation: a review of the evidence. Br J Nutr. 2009;101:633–658.
Kapkac M, Erikoglu M, Tuncyurek P, et al. Fiber enriched diets and radiation induced injury of the gut. Nutr Res. 2003;23:77–83.
De Vrese M, Schrezenmeir J. Probiotics, prebiotics, and synbiotics. Adv Biochem Eng Biotechnol. 2008;111:1–66.
Otamiri T, Sjödahl R. Oxygen radicals: their role in selected gastrointestinal disorders. Dig Dis. 1991;9:133–141.
Indaram AV, Visvalingam V, Locke M, Bank S. Mucosal cytokine production in radiation-induced proctosigmoiditis compared with inflammatory bowel disease. Am J Gastroenterol. 2000;95:1221–1225.
Mutlu-Türkoğlu U, Erbil Y, Oztezcan S, Olgaç V, Toker G, Uysal M. The effect of selenium and/or vitamin E treatments on radiation-induced intestinal injury in rats. Life Sci. 2000;66:1905–1913.
Grisham MB, MacDermott RP, Deitch EA. Oxidant defense mechanisms in the human colon. Inflammation. 1990;14:669–680.
Haton C, François A, Vandamme M, Wysocki J, Griffiths NM, Benderitter M. Imbalance of the antioxidant network of mouse small intestinal mucosa after radiation exposure. Radiat Res. 2007;167:445–453.
Adaramoye O, Ogungbenro B, Anyaegbu O, Fafunso M. Protective effects of extracts of Vernonia amygdalina, Hibiscus sabdariffa and vitamin C against radiation-induced liver damage in rats. J Radiat Res (Tokyo). 2008;49:123–131.
Koc M, Taysi S, Buyukokuroglu ME, Bakan N. Melatonin protects rat liver against irradiation-induced oxidative injury. J Radiat Res (Tokyo). 2003;44:211–215.
Seguí J, Gironella M, Sans M, et al. Superoxide dismutase ameliorates TNBS-induced colitis by reducing oxidative stress, adhesion molecule expression, and leukocyte recruitment into the inflamed intestine. J Leukoc Biol. 2004;76:537–544.
Mollà M, Gironella M, Salas A, et al. Protective effect of superoxide dismutase in radiation-induced intestinal inflammation. Int J Radiat Oncol Biol Phys. 2005;61:1159–1166.
Han W, Mercenier A, Ait-Belgnaoui A, et al. Improvement of an experimental colitis in rats by lactic acid bacteria producing superoxide dismutase. Inflamm Bowel Dis. 2006;12:1044–1052.
Carroll IM, Andrus JM, Bruno-Bárcena JM, Klaenhammer TR, Hassan HM, Threadgill DS. Anti-inflammatory properties of Lactobacillus gasseri expressing manganese superoxide dismutase using the interleukin 10-deficient mouse model of colitis. Am J Physiol Gastrointest Liver Physiol. 2007;293:G729–G738.
Kullisaar T, Zilmer M, Mikelsaar M, et al. Two antioxidative lactobacilli strains as promising probiotics. Int J Food Microbiol. 2002;72:215–224.
Chang SK, Hassan HM. Characterization of superoxide dismutase in Streptococcus thermophilus. Appl Environ Microbiol. 1997;63:3732–3735.
de LeBlanc A, LeBlanc JG, Perdigón G, et al. Oral administration of a catalase-producing Lactococcus lactis can prevent a chemically induced colon cancer in mice. J Med Microbiol. 2008;57:100–105.
Pompella A, Visvikis A, Paolicchi A, De Tata V, Casini AF. The changing faces of glutathione, a cellular protagonist. Biochem Pharmacol. 2003;66:1499–1503.
Buffinton GD, Doe WF. Depleted mucosal antioxidant defenses in inflammatory bowel disease. Free Radic Biol Med. 1995;19:911–918.
Loguercio C, D’Argenio G, Delle Cave M, et al. Glutathione supplementation improves oxidative damage in experimental colitis. Dig Liver Dis. 2003;35:635–641.
Witschi A, Reddy S, Stofer B, Lauterburg BH. The systemic availability of oral glutathione. Eur J Clin Pharmacol. 1992;43:667–669.
Mansour HH, Hafez HF, Fahmy NM, Hanafi N. Protective effect of N-acetylcysteine against radiation induced DNA damage and hepatic toxicity in rats. Biochem Pharmacol. 2008;75:773–780.
Verrecchia F, Mauviel A. Transforming growth factor-beta and fibrosis. World J Gastroenterol. 2007;13:3056–3062.
Richter KK, Langberg CW, Sung CC, Hauer-Jensen M. Association of transforming growth factor beta (TGF-beta) immunoreactivity with specific histopathologic lesions in subacute and chronic experimental radiation enteropathy. Radiother Oncol. 1996;39:243–251.
Lui RM, Pravia KA. Oxidative stress and glutathione in TGF-beta-mediated fibrogenesis. Free Radic Biol Med. 2010;48:1–15.
Musenga A, Mandrioli R, Bonifazi P, Kenndler E, Pompei A, Raggi MA. Sensitive and selective determination of glutathione in probiotic bacteria by capillary electrophoresis-laser induced fluorescence. Anal Bioanal Chem. 2007;387:917–924.
Peran L, Camuesco D, Comalada M, et al. Lactobacillus fermentum, a probiotic capable to release glutathione, prevents colonic inflammation in the TNBS model of rat colitis. Int J Colorectal Dis. 2006;21:737–746.
Lutgendorff F, Trulsson LM, van Minnen LP, et al. Probiotics enhance pancreatic glutathione biosynthesis and reduce oxidative stress in experimental acute pancreatitis. Am J Physiol Gastrointest Liver Physiol. 2008;295:G1111–G1121.
Lutgendorff F, Nijmeijer RM, Sandström PA, et al. Probiotics prevent intestinal barrier dysfunction in acute pancreatitis in rats via induction of ileal mucosal glutathione biosynthesis. PLoS One. 2009;4:e4512.
Kodali VP, Sen R. Antioxidant and free radical scavenging activities of an exopolysaccharide from a probiotic bacterium. Biotechnol J. 2008;3:245–251.
Sengül N, Aslím B, Uçar G, et al. Effects of exopolysaccharide-producing probiotic strains on experimental colitis in rats. Dis Colon Rectum. 2006;49:250–258.
Lin MY, Yen CL. Antioxidative ability of lactic acid bacteria. J Agric Food Chem. 1999;47:1460–1466.
Lee J, Hwang KT, Heo MS, Lee JH, Park KY. Resistance of Lactobacillus plantarum KCTC 3099 from Kimchi to oxidative stress. J Med Food. 2005;8:299–304.
Acknowledgments
The authors state that there was no extra-institutional funding. Supported by the National and Kapodιstrian University of Athens, Athens, Greece.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
BGS, EPM, CNS, and CF have made contributions to conception and design. BGS and EPM contributed to the analysis and interpretation of data and wrote the manuscript. All authors read and approved the final manuscript. All authors contributed equally to the final draft of the manuscript. CF has given the final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spyropoulos, B.G., Misiakos, E.P., Fotiadis, C. et al. Antioxidant Properties of Probiotics and Their Protective Effects in the Pathogenesis of Radiation-Induced Enteritis and Colitis. Dig Dis Sci 56, 285–294 (2011). https://doi.org/10.1007/s10620-010-1307-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-010-1307-1