Abstract
Background and aims
Inflammatory bowel disease is associated with intestinal oxidative stress. In the present study we test the preventative effect of Lactobacillus fermentum, a probiotic that produces per se glutathione, in the trinitrobenzenesulphonic acid (TNBS) model of rat colitis.
Methods
Colitis was induced in rats by intracolonic administration of 10 mg of TNBS dissolved in 0.25 ml of 50% ethanol. L. fermentum was administered orally (5×108 CFU suspended in 0.5 ml of skim milk) to a group of rats for 3 weeks, starting 2 weeks before colitis induction. Colonic damage was evaluated both histologically and biochemically, and the colonic luminal contents were used for bacterial studies as well as for short chain fatty acid (SCFA) production.
Results
L. fermentum treatment resulted in an amelioration of the inflammatory response in colitic rats as evidenced histologically and by a significant reduction of colonic MPO activity (P<0.05). The probiotic partially counteracted the colonic glutathione depletion induced by the inflammatory process. In addition, probiotic-treated colitic rats showed significant lower colonic tumour necrosis factor (TNF)α levels (P<0.01) and inducible nitric oxide synthase (iNOS) expression when compared to non-treated rats. Finally, the probiotic induced growth of Lactobacilli species and production of SCFA in colonic contents in comparison with control colitic rats.
Conclusion
Administration of the probiotic L. fermentum facilitates the recovery of the inflamed tissue in the TNBS model of rat colitis, an effect associated with increased levels of glutathione as well as with amelioration of the production of some of the mediators involved in the inflammatory response of the intestine, such as TNFα and NO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel disease (IBD) is a chronic disease of the digestive tract, and usually refers to two related conditions, ulcerative colitis and Crohn’s disease, which are characterised by chhronic and spontaneously relapsing inflammation. Although the aetiology of IBD remains unknown, there is increasing experimental evidence to support a role for luminal bacteria in the initiation and progression of these intestinal conditions, probably related to an imbalance in the intestinal microflora, relative predominance of aggressive bacteria and insufficient amount of protective species [1, 2]. This could justify the remission achieved in intestinal inflammation after treatment with antibiotics such as metronidazole or ciprofloxacin [3], or the fact that germ-free animals may fail to develop experimental intestinal inflammation [4]. A possible therapeutic approach in IBD therapy is the administration of probiotic microorganisms, defined as viable nutritional agents conferring benefits to the health of human host. In fact, it has been reported that administration of a mixture of Bifidobacterium and Lactobacillus [5] or of non-pathogenic viable Escherichia coli [6] prolongs remission in ulcerative colitis. Moreover, there are reports of successful induction and maintenance of remission of chronic pouchitis after oral bacteriotherapy [7, 8].
Different mechanisms have been proposed to participate in the therapeutic effects exerted by probiotic microorganisms. Firstly, these microorganisms could exert their action through a modulation of the intestinal bowel flora, which may result from competitive metabolic interactions with potential pathogens, production of anti-microbial peptides, or inhibition of epithelial adherence and translocation by pathogens [5, 9]; secondly, probiotics have been proposed to modulate the host defenses by influencing the intestinal immune system [10, 11]; and thirdly, these microorganisms have been reported to positively affect the intestinal barrier function [12, 13]. Moreover, an interesting approach in IBD treatment is the administration of probiotics capable of delivering in the intestinal lumen compounds that have been reported to exert beneficial effects in these intestinal conditions. Thus, the use of genetically modified Lactococcus lactis able to promote the delivery of either the anti-inflammatory cytokine mIL-10 [14] or trefoil factors [15] in the intestine cures or prevents experimental enterocolitis in mice. In addition, nitric oxide released by Lactobacillus farciminis improves experimental colitis in rats [16].
It is well reported that IBD is characterised by an unbalanced formation of reactive oxygen species and antioxidant micronutrients, and this may be important in the pathogenesis and/or perpetuation of the tissue injury in IBD [17, 18], which may provide a rationale for therapeutic modulation of these intestinal conditions with antioxidants. Thus, antioxidant therapy has been shown to be beneficial in experimental models of colitis [19–21], having been proposed that the beneficial effects exerted by 5-aminsalycilic derivates in human IBD are derived from their antioxidant properties [22]. In addition, glutathione, the major component of the endogenous nonprotein sulfhydryl pool, is an endogenous antioxidant that is essential in maintaining mucosal integrity; and some experimental data confirm this important role. Firstly, the inflammatory status in experimental colitis is associated with its depletion [17, 18]; secondly, when the sulfhydryl blocker iodoacetamide is administered intracolonically to rats, they develop colonic inflammation [23]; and thirdly, glutathione supplementation improves colonic damage in experimental colitis [24, 25]. Considering all of the above, a probiotic strain able to directly produce or promote the intestinal release of glutathione could have potential use in the treatment of IBD.
The aim of the present study was to test the preventative effects of a Lactobacillus fermentum strain in the trinitrobenzenesulphonic acid (TNBS) model of rat colitis, a well-established model of intestinal inflammation with some resemblance to human IBD [26]. The selection of this lactobacilli strain was based on its capacity to produce glutathione, an uncommon feature amongst lactobacilli strains. Special attention was paid to its effects after oral administration to colitic rats on the colonic glutathione levels and on the production of some of the mediators involved in the inflammatory response, such as tumour necrosis factor α (TNFα), leukotriene B4 (LTB4) and nitric oxide (NO). In addition, the correlation between the intestinal anti-inflammatory effect of L. fermentum and the modifications induced on colonic flora and on SCFA production in the luminal contents was also studied.
Materials and methods
This study was carried out in accordance with the ‘Guide for the Care and Use of Laboratory Animals’, as promulgated by the National Institute of Health, and was approved by the Animal Research and Ethic Committee of the University of Granada (Spain).
Reagents
All chemicals were obtained from Sigma (Madrid, Spain), unless otherwise stated. Glutathione reductase was provided by Boehringer Mannheim (Barcelona, Spain).
Glutathione production in bacteria
Puleva Biotech lactic acid bacterial collection was screened for Lactobacilli bacteria with the ability to produce glutathione. Cultures were grown in MRS medium at 37°C for 24 h and used to inoculate 50-ml Falcon tubes containing MRS medium. Cells were incubated for 24 h and 1-ml samples were taken to analyse glutathione content. Cells were washed with distilled water, suspended in 300 μl of TCA 7.5% (w/v) and disrupted by stirring. The mixture was centrifuged (at 10,500 g for 2 min) and 100 μl from the supernatant was transferred to a new tube containing 300 μl of MilliQ water. A portion (20 μl) from this solution was mixed with 340 μl of 0.6 M phosphate buffer (pH 7.8) and 340 μl of 1.25 mM Tris (carboxyethyl) phosphine HCl (TCEP) in 20 mM HCl. The sample was placed in the dark for 15 min, and then 800 μl of 12 mM ortho-pthalaldehyde in 50 mM sodium acetate was added and samples were placed at 4°C for 15 min. Samples were analysed by HPLC using a Spherisorb S3 ODS column at 0.8 ml/min in isocratic mode using 50 mM sodium acetate (pH 7.7)/acetonitrile (96:4) as mobile phase.
Preparation and administration of the probiotic
L. fermentum 5716, a human breast milk derived strain [27], was obtained from Puleva Biotech (Granada, Spain) and was normally growth in MRS media at 37°C under anaerobic conditions using the Anaerogen system (Oxoid, Basingstoke, UK). For probiotic treatment, bacteria was suspended in skim milk (109 CFU/ml) and stored at −80°C until usage.
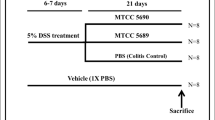
Experimental design
Female Wistar rats (180–200 g) were obtained from the Laboratory Animal Service of the University of Granada (Granada, Spain) and maintained under standard conditions. The rats were randomly assigned to three groups (n=10); two of them (non-colitic and control groups) received no probiotic treatment and the other (treated group) received the probiotic orally (5×108 CFU suspended in 0.5 ml of skim milk), daily for 3 weeks. Both non-colitic and control groups were given daily administration of the vehicle used to administer the probiotic (0.5 ml of skim milk). Two weeks after the treatment was started, the rats were fasted overnight and those from the control and treated groups were rendered colitic by the method originally described by Morris et al. [28]. Briefly, they were anaesthetised with halothane and given 10 mg of TNBS dissolved in 0.25 ml of 50% ethanol (v/v) by means of a Teflon cannula inserted 8 cm through the anus. Rats from the non-colitic group were administered intracolonically with 0.25 ml of phosphate-buffered saline instead of TNBS. All rats were killed with an overdose of halothane 1 week after induction of colitis.
Assessment of colonic damage
Body weight, water and food intake were recorded daily throughout the experiment. After the rats were sacrificed, the colon was removed aseptically and placed on an ice-cold plate, and longitudinally opened; then the luminal contents were collected for microbiological studies and for SCFA quantification (see below). Afterwards, the colonic segment was cleaned of fat and mesentery, blotted on filter paper; each specimen was weighed and its length measured under a constant load (2 g). The colon was scored for macroscopically visible damage on a 0–10 scale by two observers who were unaware of the treatment, according to the criteria described by Bell et al. [29] and Camuesco et al. [30], which take into account the extent as well as the severity of colonic damage. Representative whole gut specimens were taken from a region of the inflamed colon corresponding to the adjacent segment to the gross macroscopic damage and were fixed in 4% buffered formaldehyde. Cross-sections were selected and embedded in paraffin. Equivalent colonic segments were also obtained from the non-colitic group. Full-thickness sections of 5 μm were taken at different levels and stained with haematoxylin and eosin. The histological damage was evaluated on a 0–27 scale by two pathologist observers (A.N. and A.C.), who were blinded to the experimental groups, according to the criteria described previously [30]. The colon was subsequently divided into four segments for biochemical determinations. Two fragments were frozen at −80°C for myeloperoxidase (MPO) activity and inducible nitric oxide synthase (iNOS) expression, and another sample was weighed and frozen in 1 ml of 50 g/l trichloroacetic acid for total glutathione content determination. The remaining sample was immediately processed for the measurement of TNFα and leukotriene B4 (LTB4) levels. All biochemical measurements were performed in duplicate and completed within 1 week of sample collection.
MPO activity was measured according to the technique described by Krawisz et al. [31]; the results were expressed as MPO units per gram of wet tissue; 1 unit of MPO activity was defined as that degrading 1 μmol hydrogen peroxide/min at 25°C. Total glutathione content was quantified with the recycling assay described by Anderson [32], and the results were expressed as nmol/g wet tissue. Colonic samples for TNFα and LTB4 determinations were immediately weighed, minced on an ice-cold plate and suspended in a tube with 10 mM sodium phosphate buffer (pH 7.4) (1:5 w/v). The tubes were placed in a shaking water bath (37°C) for 20 min and centrifuged at 9,000 g for 30 s at 4°C; the supernatants were frozen at −80°C until assay. TNFα was quantified by enzyme-linked immunoabsorbent assay (Amersham Pharmacia Biotech, Buckinghamshire, UK) and the results were expressed as pg/g wet tissue. LTB4 was determined by enzyme immunoassay (Amersham Pharmacia Biotech) and the results expressed as ng/g wet tissue. iNOS expression was analysed by Western blotting as previously described [20], and control of protein loading and transfer was conducted by detection of the β-actin levels.
Microbiological studies
Luminal content samples were homogenised in peptone physiological saline (100 mg faeces/ml). Tenfold serial dilutions were made in the same medium and aliquots of 0.1 ml of the appropriate dilution were spread onto the following agar media: MRS agar for lactobacilli, MRS agar supplemented with 0.5 mg/l dicloxacillin, 1 g/l LiCl and 0.5 g/l l-cysteine hydrochloride for Bifidobacterium; reinforced clostridial containing 20 μg/ml de polymyxin for Clostridium. All media were obtained from Oxoid (Basingstoke, UK), whereas antibiotics and other supplements were obtained from Sigma (St. Louis, MO). Culture plates were incubated in absence of oxygen at 37°C for 24–48 h. Similarly, 1 ml of suitable dilution was spread onto specific Count Plates Petrifilm (3M, St. Paul, MN) for coliforms, for total aerobes and for Enterobacteriaceae. Plates were incubated at 37°C for 24 h. After the incubation, the specific colonies grown on the selective culture media were counted and the number of viable microorganism per gram faecal (CFU/g) was calculated. The mean and standard error per group were calculated from the log values of the CFU/g.
SCFA quantification in colonic contents
To quantify the SCFA concentration in the colonic luminal contents, samples were homogenised with 150 mM NaHCO3 (pH 7.8) (1:5, wt/v) in an argon atmosphere. Samples were incubated for 24 h at 37°C and stored at −80°C until the extraction. To extract the SCFAs, 50 μl of the internal standard 2-methylvaleric acid (100 mM), 10 μl of sulphuric acid and 0.3 ml of ethyl acetate were added to 1 ml of the homogenate and then centrifuged at 10,000 g for 5 min at 4°C. The supernatants were dehydrated with sodium sulphate anhydrous and centrifuged 10,000 g for 5 min at 4°C. Later, 0.5 ml of the sample was splitless inoculated into a gas chromatograph (Varian CP-3800) equipped with an ID (CPWAX 52CB 60 m×0.25 mm), and connected to a FID detector (Varian, Lake Forest, CA). Helium was used as the carrier and the make-up gas, with a flow rate of 1.5 ml/min. Injection temperature was 250°C. Acetate, propionate and butyrate concentrations were automatically calculated from the areas of peaks using the Star Chromatography WorkStation program (version 5.5), which was on-line connected to the FID detector.
Statistics
All results are expressed as the mean±SEM. Differences between means were tested for statistical significance using a one-way analysis of variance (ANOVA) and post-hoc least significance tests. Non-parametric data (score) are expressed as the median (range) and were analysed using the Mann–Whitney U-test. Differences between proportions were analysed with the chi-square test. All statistical analyses were carried out with the Statgraphics 5.0 software package (STSC, Maryland), with statistical significance set at P<0.05.
Results
Intestinal anti-inflammatory activity of L. fermentum administration in rats with TNBS-induced colitis
More than 50 strains of lactic acid bacteria belonging to Puleva Biotech’s collection were screened for their ability to produce glutathione. The results confirmed that the ability to produce glutathione is not a common feature in the lactobacilli group, although it has been reported in other prokaryotic microorganism [33, 34]. In fact, the production of glutathione was detectable in the strain L. fermentum 5716, which, in addition to its ability to produce glutathione (1.4±0.3 mM in culture media), was also able to generate the antioxidant dipeptide γ-Glu-Cys (2.3±0.2 mM in culture media) (Fig. 1). For this reason, we decided to use this strain to test its ability to prevent the inflammatory response in the in vivo assay of experimental colitis.
L. fermentum 5716 administration for 2 weeks failed to induce any symptoms of diarrhoea or effect in the weight evolution (data not shown). However, once colitis was induced, the probiotic-treated rats showed an overall lower impact of TNBS-induced colonic damage compared to the TNBS control group. The anti-inflammatory effect was evidenced macroscopically by a significantly lower colonic damage score than that of control rats (P<0.05), with a significant reduction of the extent of colonic necrosis and/or inflammation (Table 1). This anti-inflammatory effect was also associated with a significant reduction of the colonic weight/length ratio between both colitic groups, an index of colonic oedema that is increased significantly as a consequence of the inflammatory process (Table 1). The histological studies confirmed the intestinal anti-inflammatory effect exerted by L. fermentum (Fig. 2). Histological assessment of colonic samples from the TNBS control group revealed severe transmural disruption of the normal architecture of the colon, extensive ulceration and inflammation involving all the intestinal layers of the colon, giving a score value of 21.6±2.3 (mean±SEM). Colonic samples were characterised by severe oedema, interstitial microhaemorrhages and diffuse leucocyte infiltration, mainly composed of neutrophils in the mucosa layer and, to a lesser extent, lymphocytes in the submucosa. Most of the rats showed epithelial ulceration of the mucosa affecting over 75% of the surface. The inflammatory process was associated with crypt hyperplasia and dilation, and moderate to severe goblet cell depletion. However, histological analysis of the colonic specimens from rats treated with the probiotic revealed a more pronounced recovery of the intestinal architecture than controls, with a score of 9.4±1.9 (mean±SEM) (P<0.01 vs TNBS control group). Thus, most of the samples (nine of ten) showed almost complete restoration of the epithelial cell layer, in contrast to the extensive ulceration observed in non-treated animals; in fact, the zones with ulceration were surrounded by tissue in process of re-epithelisation. Moreover, the transmural involvement of the lesions was reduced. The goblet cell depletion was less severe and thus they appeared replenished with their mucin content, and no dilated crypts were observed. The improvement in colonic histology was accompanied by a reduction in the inflammatory infiltrate, which was slight to moderate with a patchy distribution, although neutrophils were the predominant cell type.
Histological sections of colonic mucosa from colitic rats 1 week after TNBS instillation stained with haematoxylin and eosin. a Non-colitic group showing the normal histology of the rat colon (original magnification ×20). b TNBS control group showing complete destruction of the mucosa, which has been substituted by inflammatory granulation tissue. There is evident edema and intense diffuse transmural inflammatory infiltrate (original magnification ×100). c L. fermentum-treated group showing amelioration in the inflammatory process and ‘restoration’ of the mucosal tissue with the presence of mucin-replenished goblet cells (original magnification ×100)
The lower leucocyte infiltration was also assessed biochemically by the reduction of colonic MPO activity, a marker of neutrophil infiltration that was enhanced in the TNBS control group (Table 2). In addition, probiotic-treated colitic rats showed a significant increase of colonic glutathione content, which is depleted in colitic rats as a consequence of the colonic oxidative stress induced by the inflammatory process, as previously reported in this model of experimental colitis [35] (Table 2). Finally, the colonic inflammation induced by TNBS was characterised by increased levels of colonic TNFα and LTB4 (Table 2) as well as by a greater colonic iNOS expression (Fig. 3) in comparison with non-colitic animals. Treatment of colitic rats with L. fermentum resulted in a significant reduction of colonic TNFα levels (Table 2), but no significant modification of colonic LTB4 levels was obtained between both colitic groups (Table 2). Finally, a lower colonic iNOS expression was also observed in colitic animals that received the bacteria suspension when compared to TNBS control animals (Fig. 3).
Effects of L. fermentum administration on colonic bacterial profile
TNBS colitis resulted in a significant reduction of faecal lactobacilli count in comparison with normal rats (P=0.003). Probiotic-treated colitic rats showed significantly higher counts of Lactobacilli species in colonic contents in comparison with control colitic rats (P=0.039), without showing statistical differences with non-colitic control group (Fig. 4). No statistical differences were observed in Bifidobacteria counts amongst three groups (P>0.1; Fig. 4) or in the amount of other faecal potential pathogenic bacteria such as entherobacteria or coliforms (data not shown).
Effects of L. fermentum administration on SCFA production
When the colonic contents from TNBS control rats were incubated for 24 h, a reduction of the levels of SCFA was observed compared to non-colitic rats (P<0.01, Table 3), similar to that described previously in this model of experimental colitis [36]. However, the intestinal contents obtained from the colitic treated rats showed greater acetate, butyrate and propionate production than those from TNBS control rats without probiotic treatment (P<0.01, Table 3).
Discussion
IBD is characterised by the abnormal production of free radicals with resultant oxidant-induced tissue injury and reduced antioxidant defenses [17, 18]. For this reason, antioxidant therapy can constitute an interesting approach in the downregulation of this inflammatory condition. In fact, the beneficial effects exerted by the 5-aminosalicylic derivatives in the treatment of IBD have been partially attributed to their antioxidant and free radical scavenger properties [22]. Moreover, several antioxidant compounds, such as flavonoids or vitamin E, have been reported to exert anti-inflammatory activity in experimental models of rat colitis [19–21], which was associated with restoration of glutathione colonic mucosal levels. Glutathione is a sulfhydryl-derived compound that actively participates in the antioxidant mechanisms of the intestinal mucosa, preserving it from oxidant-induced tissue damage. Different studies have reported diminished glutathione content in these intestinal conditions, both in humans [37] and in experimental models of rat colitis [19–21], and that glutathione supplementation results in beneficial effects in experimental colitis [24, 25]. All these facts prompted us to evaluate the intestinal anti-inflammatory effect of the probiotic L. fermentum, a microorganism that has been demonstrated in vitro to produce antioxidant compounds, such as glutathione and its precursor the dipeptide γ-Glu-Cys, in the TNBS model of rat colitis.
The results obtained in the present study reveal the efficacy of L. fermentum in this experimental model of colitis, thus incorporating a new microorganism to the probiotics that have been reported to attenuate the development of colonic injury in experimental and human IBD [38]. This beneficial effect was histologically evidenced with a significant reduction of the extent and severity of inflamed tissue achieved after probiotic treatment in comparison with non-treated colitic rats. The anti-inflammatory effect was also stated biochemically, since its administration to colitic rats resulted in a significant inhibition of colonic MPO activity, a marker of neutrophil infiltration previously described to be upregulated in experimental colitis [31], and widely used to detect and follow intestinal inflammatory processes. In consequence, a reduction of the activity of this enzyme can be interpreted as a manifestation of the anti-inflammatory activity of a given compound [39]. The ability of the probiotic to reduce granulocyte infiltration was confirmed histologically since the level of leucocyte infiltrate in the colonic mucosa was lower in treated colitic animals than in the corresponding TNBS control groups. This may account for the beneficial effect showed by this probiotic because margination and extravasation of circulating granulocytes contributes markedly to the colonic injury in this model of IBD [40]. These results are in agreement with other studies that describe the attenuation exerted by several probiotics in leucocyte–endothelial cell adhesion in this experimental model of rat colitis [16]. The inhibitory effect on leucocyte infiltration may be the consequence of the preventative effect exerted by the probiotic against the free radical derived oxidative injury that takes place after TNBS instillation in the colonic tissue [25, 41], since the intestinal anti-inflammatory effect was associated with a restoration of the colonic glutathione levels in comparison with non-treated colitic rats. The production of γ-Glu-Cys, precursor of glutathione, by this Lactobacilli strain may play a key role, since it has been described to be more efficiently uptaken than glutathione in the intestine. Although γ-Glu-Cys can be also substrate for other enzymes, like gamma-glutamylcyclotransferase, glutathione synthesis is increased in animal cells because of its higher affinity for the enzyme glutathione synthetase [42]. The free radical scavenger properties attributed to both compounds, γ-Glu-Cys and glutathione, produced by this probiotic seem to be crucial in its anti-inflammatory effect. In fact, it has been proposed that free radical generation in the inflamed tissue constitutes an early signal that promotes the infiltration of neutrophils into colonic tissue, which in turn produce a large amount of free radicals that actively participate in the perpetuation of the inflammatory response [43]. For this reason, the rapid neutralisation of these reactive oxygen species would result in the inhibition of neutrophil infiltration, as observed in the present study. The inhibitory effect of the probiotic on the production and/or release of others mediators with chemotactic properties, like LTB4, can be ruled out because the probiotic treatment was not associated with a significant modification of the colonic levels of this eicosanoid in comparison with non-treated colitic rats.
Moreover, this inhibitory effect on neutrophil infiltration attributed to the probiotic may also justify the inhibition of the synthesis and/or release of NO, another mediator that participates in the inflammatory process, since probiotic treatment of colitic rats was associated with a reduction in colonic iNOS expression. During the last decade, it has become increasingly clear that chronic colonic inflammation, both in human IBD and in experimental colitis, is associated with enhanced NO production, mainly via iNOS activity [44–46]. The simultaneous overproduction of NO and reactive oxygen metabolites, like superoxide anion, can yield the highly toxic radical peroxynitrite in the inflamed intestine [17]. Since neutrophils have been also considered as an important source of NO [47, 48], the effect exerted by L. fermentum in decreasing the neutrophil infiltration may in turn contribute to preserve colonic mucosa from peroxynitrite insult.
The present study also reveals that probiotic treatment promotes the downregulation of TNFα, a pro-inflammatory mediator that has been proposed to play a key role in colonic inflammation [49]; in fact, different drugs capable of interfering with the activity of this mediator are being developed for IBD therapy [50]. The ability of probiotic bacteria to downregulate TNFα production has been reported previously for other lactobacilli strains such as L. casei and of L. bulgaricus when they were cultured with inflamed mucosa from patients with Crohn’s disease [51]. This effect was attributed to the existence of a cross-talk between bacteria and mucosal cells, being able to downregulate the degree of activation of intestinal immune cells [51]. The results obtained in the present study show that, in the case of L. fermentum, this relationship between bacteria and mucosal cells may be driven by SCFA, mainly butyrate. In fact, when colonic contents were incubated for 24 h, SCFA production was increased in probiotic-treated colitic rats in comparison with the corresponding control rats without probiotic treatment. Thus, the inhibitory effect of probiotic administration on cytokine production may be related to the ability of SCFA to interfere with transcription factors. Nuclear factor-kappa B (NF-κB) is a transcription factor that, in combination with others, plays a central role in regulating the expression of genes encoding numerous cytokines in immune and inflammatory responses [52]. Thus, it has been previously reported that butyrate decreases TNFα production by intestinal biopsies and by isolated lamina propria mononuclear cells via inhibition of NF-κB activation and IκBα degradation [53]. The inhibitory effect of butyrate on NF-κB activation in HT-29 cells, probably derived from its ability to inhibit deacetylases, has also been reported [54]. However, the amelioration of the colonic oxidative stress observed after probiotic treatment to colitic rats may also account for its effect on cytokine production, since NF-κB is a redox-sensitive transcription factor activated by oxidant stress in the inflamed intestinal mucosa [55].
However, the participation of the modification in the immune response in the intestinal anti-inflammatory effect exerted by this probiotic does not exclude mechanisms proposed by other probiotics, mainly a role in prevention in the imbalance in the intestinal microflora, given the relative predominance of aggressive bacteria and insufficient amount of protective species that has been reported to occur in these intestinal conditions [1, 2]. Previous studies have suggested that in TNBS-induced colitis, specific strains from colonic microflora invades the colonic wall after disruption of the epithelium and the presence of bacteria within the wall contributes to the transmural inflammation [56]. In fact, the present study reveals that the colonic damage induced by TNBS was associated with a significant reduction of lactobacilli count in the colonic lumen, which was counteracted after probiotic treatment without showing statistical differences with non-colitic rats.
In conclusion, administration of the probiotic L. fermentum 5716 facilitates the recovery of the inflamed tissue in the TNBS model of rat colitis, an effect associated with amelioration of the production of some of the mediators involved in the inflammatory response of the intestine, including TNFα and NO. This beneficial effect could be ascribed to its ability to prevent oxidative stress that occurs in this inflammatory condition, through the increased production of glutathione, which might attenuate the exacerbated immune response evoked by the colonic instillation of the hapten TNBS in the rats.
References
Fiocchi C (1998) Inflammatory bowel disease: aetiology and pathogenesis. Gastroenterology 115:182–205
Shanahan F (2000) Probiotics and inflammatory bowel disease: is there a scientific rationale? Inflamm Bowel Dis 6:107–115
Chung PY, Peppercorn MA (1999) Antibiotics in inflammatory bowel disease. Drugs Today 35:89–103
Taurog JD, Richardson JA, Croft JT, Simmons WA, Zhou M, Fernandez-Sueiro JL, Balish E, Hammer RE (1994) The germ-free state prevents development of gut and joint inflammatory disease in HLA-B27 transgenic rats. J Exp Med 180:2359–2364
Venturi A, Gionchetti P, Rizzello F, Johansson R, Zucconi E, Brigidi P, Matteuzzi D, Campieri M (1999) Impact on the composition of the faecal flora by a new probiotic preparation: preliminary data on maintenance treatment of patients with ulcerative colitis. Aliment Pharmacol Ther 13:1103–1108
Rembacken BJ, Snelling AM, Hawkey PM, Chalmers DM, Axon AT (1999) Non-pathogenic Escherichia coli versus mesalazine for the treatment of ulcerative colitis: a randomised trial. Lancet 354:635–639
Gionchetti P, Rizzello F, Helwig U, Venturi A, Lammers KM, Brigidi P, Vitali B, Poggioli G, Miglioli M, Campieri M (2003) Prophylaxis of pouchitis onset with probiotic therapy: a double-blind, placebo-controlled trial. Gastroenterology 124:1202–1209
Gionchetti P, Rizzello F, Venturi A, Brigidi P, Matteuzzi D, Bazzocchi G, Poggioli G, Miglioli M, Campieri M (2000) Oral bacteriotherapy as maintenance treatment in patients with chronic pouchitis: a double-blind, placebo-controlled trial. Gastroenterology 119:305–309
Tannock GW, Munro K, Harmsen HJ, Welling GW, Smart J, Gopal PK (2000) Analysis of the fecal microflora of human subjects consuming a probiotic product containing Lactobacillus rhamnosus DR20. Appl Environ Microbiol 66:2578–2588
Ulisse S, Gionchetti P, D’Alo S, Russo FP, Pesce I, Ricci G, Rizzello F, Helwig U et al (2001) Expression of cytokines, inducible nitric oxide synthase, and matrix metalloproteinases in pouchitis: effects of probiotic treatment. Am J Gastroenterol 96:2691–2699
Schultz M, Linde HJ, Lehn N, Zimmermann K, Grossmann J, Falk W, Scholmerich J (2003) Immunomodulatory consequences of oral administration of Lactobacillus rhamnosus strain GG in healthy volunteers. J Dairy Res 70:165–173
Madsen K, Cornish A, Soper P, McKaigney C, Jijon H, Yachimec C, Doyle J, Jewell L, De Simone C (2001) Probiotic bacteria enhance murine and human intestinal epithelial barrier function. Gastroenterology 121:580–591
Otte JM, Podolsky DK (2004) Functional modulation of enterocytes by gram-positive and gram-negative microorganisms. Am J Physiol 286:G613–G626
Steidler L, Hans W, Schotte L, Neirynck S, Obermeier F, Falk W, Fiers W, Remaut E (2000) Treatment of murine colitis by Lactococcus lactis secreting interleukin-10. Science 289:1352–1355
Vandenbroucke K, Hans W, Van Huysse J, Neirynck S, Demetter P, Remaut E, Rottiers P, Steidler L (2004) Active delivery of trefoil factors by genetically modified Lactococcus lactis prevents and heals acute colitis in mice. Gastroenterology 127:502–513
Lamine F, Fioramonti J, Bueno L, Nepveu F, Cauquil E, Lobysheva I, Eutamene H, Theodorou V (2004) Nitric oxide released by Lactobacillus farciminis improves TNBS-induced colitis in rats. Scand J Gastroenterol 39:37–45
Pavlick KP, Laroux FS, Fuseler J, Wolf RE, Gray L, Hoffman J, Grisham MB (2002) Role of reactive metabolites of oxygen and nitrogen in inflammatory bowel disease. Free Radic Biol Med 33:311–322
Buffinton GD, Doe WF (1995) Depleted mucosal antioxidant defences in inflammatory bowel disease. Free Radic Biol Med 19:911–918
Galvez J, Coelho G, Crespo ME, Cruz T, Rodriguez-Cabezas ME, Concha A, Gonzalez M, Zarzuelo A (2001) Intestinal anti-inflammatory activity of morin on chronic experimental colitis in the rat. Aliment Pharmacol Ther 15:2027–2039
Camuesco D, Comalada M, Rodriguez-Cabezas ME, Nieto A, Lorente MD, Concha A, Zarzuelo A, Galvez J (2004) The intestinal anti-inflammatory effect of quercitrin is associated with an inhibition in iNOS expression. Br J Pharmacol, DOI 10.1038/sj.bjp.0705941
Gonzalez R, Sanchez de Medina F, Galvez J, Rodriguez-Cabezas ME, Duarte J, Zarzuelo A (2001) Dietary vitamin E supplementation protects the rat large intestine from experimental inflammation. Int J Vitam Nutr Res 71:243–250
Travis SPL, Jewel DP (1994) Salicylates for ulcerative colitis—their mode of action. Pharmacol Ther 63:135–161
Rachmilewitz D, Karmeli F, Okon E (1995) Sulfhydryl blocker-induced rat colonic inflammation is ameliorated by inhibition of nitric oxide synthase. Gastroenterology 109:98–106
Loguercio C, D’Argenio G, Delle Cave M, Cosenza V, Della Valle N, Mazzacca G, Del Vecchio Blanco C (2003) Glutathione supplementation improves oxidative damage in experimental colitis. Dig Liver Dis 35:635–641
Ardite E, Sans M, Panes J, Romero FJ, Pique JM, Fernandez-Checa JC (2000) Replenishment of glutathione levels improves mucosal function in experimental colitis. Lab Invest 80:735–744
Jurjus AR, Khoury NN, Reimund JM (2004) Animal models of inflammatory bowel disease. J Pharmacol Toxicol Methods 50:81–92
Martin R, Langa S, Reviriego C, Jiminez E, Marin ML, Xaus J, Fernandez L, Rodriguez JM (2003) Human milk is a source of lactic acid bacteria for the infant gut. J Pediatr 143:754–758
Morris GP, Beck PL, Herridge W, Depew W, Szewczuk MR, Wallace JL (1989) Hapten induced model of chronic inflammation and ulceration in rat colon. Gastroenterology 96:795–803
Bell CJ, Gall DG, Wallace JL (1995) Disruption of colonic electrolyte transport in experimental colitis. Am J Physiol 268:G622–G630
Camuesco D, Peran L, Comalada M, Nieto A, Di Stasi LC, Rodriguez-Cabezas ME, Concha A, Zarzuelo A, Galvez J (2005) Preventative effects of lactulose in the trinitrobenzenesulphonic acid model of rat colitis. Inflamm Bowel Dis 11:265–271
Krawisz JE, Sharon P, Stenson WF (1984) Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity. Assessment of inflammation in rat and hamster models. Gastroenterology 87:1344–1350
Anderson ME (1985) Determination of glutathione and glutathione disulfide in biological samples. Methods Enzymol 113:548–555
Newton GL, Arnold K, Price MS, Sherrill C, Delcardayre SB, Aharanowitz Y, Cohen G, Davies J et al (1996) Distribution of thiols in microorganisms: mycothiol is a mayor thiol in most Actinomycetes. J Bacteriol 178:1990–1995
Fahey RC, Brown WC, Adams WB, Worsham MB (1978) Occurrence of glutathione in bacteria. J Bacteriol 133:1126–1129
Galvez J, Garrido M, Rodriguez-Cabezas ME, Ramis I, Sanchez de Medina F, Merlos M, Zarzuelo A (2003) The intestinal anti-inflammatory activity of UR-12746S on reactivated experimental colitis is mediated through downregulation of cytokine production. Inflamm Bowel Dis 9:363–371
Rodriguez-Cabezas ME, Galvez J, Lorente MD, Concha A, Camuesco D, Azzouz S, Osuna A, Redondo L, Zarzuelo A (2002) Dietary fiber down-regulates colonic tumor necrosis factor alpha and nitric oxide production in trinitrobenzenesulfonic acid-induced colitic rats. J Nutr 132:3263–3271
Miralles-Barrachina O, Savoye G, Belmonte-Zalar L, Hochain P, Ducrotte P, Hecketsweiler B, Lerebours E, Dechelotte P (1999) Low levels of glutathione in endoscopic biopsies of patients with Crohn’s colitis: the role of malnutrition. Clin Nutr 18:313–317
Schultz M, Sartor RB (2000) Probiotics and inflammatory bowel diseases. Am J Gastroenterol 95:S19–S21
Veljaca M, Lesch CA, Pllana R, Sanchez B, Chan K, Guglietta A (1995) BPC-15 reduces trinitrobenzene sulfonic-induced colonic damage in rats. J Pharmacol Exp Ther 272:417–422
Ajuebor MN, Zagorski J, Kunkel SL, Strieter RM, Hogaboam CM (2004) Contrasting roles for CXCR2 during experimental colitis. Exp Mol Pathol 76:1–8
Grisham MB, Olkmer C, Tso P, Yamada T (1991) Metabolism of trinitrobenzene sulfonic acid by rat colon produces reactive oxygen species. Gastroenterology 101:540–547
Wu G, Fang YZ, Yang S, Lupton JR, Turner ND (2004) Glutathione metabolism and its implications for health. J Nutr 134:489–492
Guo X, Wang WP, Ko JK, Cho CH (1999) Involvement of neutrophils and free radicals in the potentiating effects of passive cigarette smoking on inflammatory bowel disease in rats. Gastroenterology 117:884–892
Rachmilewitz D, Karmeli F, Okon E, Bursztyn M (1995) Experimental colitis is ameliorated by inhibition of nitric oxide synthase activity. Gut 37:247–255
Hogaboam CM, Jacobson K, Collins SM Blennerhassett MG (1995) The selective beneficial effects of nitric oxide inhibition in experimental colitis. Am J Physiol 268:G673–G684
Kimura H, Miura S, Shigematsu T, Ohkubo N, Tsuzuki Y, Kurose I, Higuchi H, Akiba Y et al (1997) Increased nitric oxide production and inducible nitric oxide synthase activity in colonic mucosa of patients with active ulcerative colitis and Crohn’s disease. Dig Dis Sci 42:1047–1054
Ikeda I, Kasajima T, Ishiyama S, Shimojo T, Takeo Y, Nishikawa T, Kameoka S, Hiroe M, Mitsunaga A (1997) Distribution of inducible nitric oxide synthase in ulcerative colitis. Am J Gastroenterol 92:1339–1341
McCafferty DM, Miampamba M, Sihota E, Sharkey KA, Kubes P (1999) Role of inducible nitric oxide synthase in trinitrobenzene sulphonic acid induced colitis in mice. Gut 45:864–873
Van Deventer SJH (1997) Tumor necrosis factor and Crohn’s disease. Gut 40:443–448
Rutgeerts P, Van Assche G, Vermeire S (2004) Optimizing anti-TNF treatment in inflammatory bowel disease. Gastroenterology 126:1593–1610
Borruel N, Carol M, Casellas F, Antolin M, de Lara F, Espin E, Naval J, Guarner F, Malagelada JR (2002) Increased mucosal tumour necrosis factor alpha production in Crohn’s disease can be downregulated ex vivo by probiotic bacteria. Gut 51:659–664
Schottelius AJ, Baldwin AS Jr (1999) A role for transcription factor NF-kappa B in intestinal inflammation. Int J Colorectal Dis 14:18–28
Segain JP, Raingeard de la Bletiere D, Bourreille A, Leray V, Gervois N, Rosales C, Ferrier L, Bonnet C et al (2000) Butyrate inhibits inflammatory responses through NFκB inhibition: implications for Crohn’s disease. Gut 47:397–403
Inan MS, Rasoulpour RJ, Yin L, Hubbard AK, Rosenberg DW, Giardina C (2000) The luminal short-chain fatty acid butyrate modulates NF-κB activity in a human colonic epithelial cell line. Gastroenterology 118:724–734
Rogler G, Brand K, Vogl D, Page S, Hofmeister R, Andus T, Knuechel R, Baeuerle PA et al (1998) Nuclear factor kappaB is activated in macrophages and epithelial cells of inflamed intestinal mucosa. Gastroenterology 115:357–369
Garcia-Lafuente A, Antolin M, Guarner F, Crespo E, Salas A, Forcada P, Laguarda M, Gavalda J et al (1997) Incrimination of anaerobic bacteria in the induction of experimental colitis. Am J Physiol 272:G10–G15
Acknowledgements
This study was supported by the Spanish Ministry of Science and Technology (SAF2002-02592) and by Instituto de Salud ‘Carlos III’ (PI021732), with funds from the European Union, and by Junta de Andalucia (CTS 164). Mònica Comalada is a recipient of Juan de la Cierva Program from Spanish Ministry of Science and Technology. Laura Perán is a recipient from Puleva Foundation (Spain).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Peran, L., Camuesco, D., Comalada, M. et al. Lactobacillus fermentum, a probiotic capable to release glutathione, prevents colonic inflammation in the TNBS model of rat colitis. Int J Colorectal Dis 21, 737–746 (2006). https://doi.org/10.1007/s00384-005-0773-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-005-0773-y