Abstract
Morin, a plant-derived flavonoid, has been reported to exhibit a wide range of pharmacological properties. In this study, we investigated the protective effect of morin on hepatic fibrosis induced by dimethylnitrosamine (DMN) in rats. Oral administration of morin remarkably prevented weight loss in the body and liver from DMN and inhibited the elevation of serum alanine transaminase (ALT), aspartate transaminase (AST), and total bilirubin levels. For the evaluation of hepatic fibrosis-related factors, we investigated expressions of collagen type I, transforming growth factor β1 (TGF-β1), and α-smooth muscle actin (α-SMA) in mRNA and protein levels. We observed that morin significantly reduced the expression of collagen type I, TGF-β1, and α-SMA on hepatic fibrosis induced by DMN. Taken together, this study demonstrated that morin showed hepatoprotective and antifibrogenic effects against DMN-induced hepatic injury. This suggests that morin may be useful in preventing the development of hepatic fibrosis and cirrhosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morin [2-(2,4-dihydroxyphenyl)-3,5,7-trihydroxy-4H-1-benzopyran-4-one] is a kind of flavonoid belonging to the group of flavonoids (Fig. 1) found in almonds (P. guajava L.) [1], mill (Prunus dulcis) [2], and other moraceas, which are used as dietary agents and also as herbal medicines [3]. It has been shown to act as a potent antioxidant [4, 5], xanthine oxidase inhibitor [6], cell proliferation inhibitor [7], apoptosis inducer [8], and modulator of lipoxygenase and cyclo-oxygenase activities in the arachidonic acid cascade [9]. It also acts as a chemopreventive agent against oral carcinogenesis in vitro and in vivo [10]. Furthermore, morin exhibits inhibition of tetradecanoylphorbo-13-acetate (TPA)-induced hepatocellular transformation [11].
Hepatic fibrosis is characterized by an excessive deposition of extracellular matrix (ECM) proteins and can ultimately lead to cirrhosis and organ failure [12]. The main causes of liver fibrosis include chronic viral hepatitis, alcohol abuse, autoimmune diseases, and hereditary metabolic disorders. The activation of hepatic stellate cells (HSCs) has been implicated in the pathogenesis of liver fibrosis [12, 13]. Activated HSCs are proliferative and fibrogenic, with accumulation of ECM, including α-smooth muscle actin (α-SMA) and collagen type I [14, 15]. Moreover, activated HSCs have been implicated in hepatic inflammation through their ability to secrete cytokines, including transforming growth factor-β1 (TGF-β1) in the course of liver fibrogenesis [12].
Dimethylnitrosamine (DMN) is a potent hepatotoxin, carcinogen, and mutagen. Exposure to repeated low-dose DMN causes subacute and chronic liver injury with varying degrees of necrosis, fibrosis, and nodular regeneration [16]. A DMN-induced fibrosis model is known to reproduce most of the features observed during human liver fibrosis [17]. This model also has various benefits, such as progressive and remarkable pathological alteration, a high fibrosis reproduction rate, and a low mortality rate in experimental animals [18].
The present study was designed to evaluate whether morin exerts a protective effect in rats with DMN-induced liver fibrosis. Here, we demonstrate, for the first time, that morin can show functional and morphological prevention by decreasing collagen type I, TGF-β1, and α-SMA in rats with DMN-induced liver fibrosis.
Material and Methods
Animals
Animal care and all experimental procedures were conducted in accordance with the Guide for Animal Experiments edited by the Korean Academy of Medical Sciences. Male Sprague-Dawley rats were obtained from ORIENT-BIO Laboratory Animal Research Center Co., Ltd. (Gyeonggi-do, Korea). Animals were kept on standard rat chow with free access to tap water, in a temperature- and humidity-controlled animal house under 12-h light–dark cycles. Eighteen rats, 170–180 g, were divided into three groups of six each (control, DMN, and morin groups). The DMN group was treated with intraperitoneal injections of DMN (diluted with saline) at a dose of 10 μl/kg of body weight three consecutive days per week for 4 weeks, as described previously [19]. The morin group was treated every other day for 4 weeks with morin suspended in a PEG400 mixture (N,N-dimethylacetamide to polyethylene glycol 400 to distilled water = 1:5:4) at a dose of 20 mg/kg by oral gavage before DMN treatment. The DMN group was treated with DMN as described above and equivalent volumes of the PEG400 mixture solution. The control group was treated with volumes of saline and PEG400 mixture solution equivalent to the treatment given to the morin group. At the end of the fourth week, all of the rats were sacrificed under ether anesthesia. Their livers were excised and weighed. Blood samples for biochemical analyses were obtained from the heart. The liver specimens were immediately fixed in 10% neutral buffered formalin for histochemical studies. The remaining liver tissue was homogenized using a glass Potter-Elvehjem homogenizer set for reverse-transcriptase polymerase chain reaction (RT-PCR) and Western blot study. The homogenate was freed from the cellular debris and nuclei by centrifugation at 700 g at 4°C for 10 min.
Biochemical Analyses of Serum
Serum alanine transaminase (ALT), aspartate transaminase (AST), total bilirubin (T. Bilirubin), and direct bilirubin (D. Bilirubin) levels were analyzed by the Green Gross Reference Lab (Seoul, Korea).
Liver Histopathology
For histopathological analysis, liver slices were cut, fixed in formaldehyde, and embedded in paraffin. Five-micron-thick sections were then stained with hematoxylin eosin (H&E) and Masson’s trichrome (MT) before observation under a light microscope. The degree of hepatic fibrosis was determined by the Knodell fibrosis score, which has four grades derived from the Metavir score; the area of fibrosis was measured by image analysis [20]. The histopathological fibrosis scores were as follows: 0, no fibrosis; I, perivenular and/or pericellular fibrosis; II, septal fibrosis; III, incomplete cirrhosis; and IV, complete cirrhosis [21]. Two expert pathologists blindly scored the tissue slices and evaluated degree of fibrosis according to a strict standard. The degree of fibrosis was expressed as the mean of eight fields in each slide. The degree of fibrosis by each pathologist was almost similar.
RNA Extraction and RT-PCR Analysis
Total RNA were extracted from frozen liver sample with Trizol reagent following the manufacturer’s protocol. An aliquot of total RNA was reverse transcribed and amplified using MMuLV reverse transcriptase and Taq DNA polymerase, respectively. Aliquots of the reverse transcription mixture were used for the amplification by polymerase chain reaction (PCR) of fragments specific to collagen type Ι, TGF-β 1 , and α-SMA. The expression levels of all the transcripts were normalized to that of the GAPDH mRNA in the same tissue. The primer pairs for collagen type Ι, TGF-β 1 , and α-SMA were designed using the Primer select program. The PCR products were electrophoresed on 1.5% agarose gel recorded by a KODAK imaging system, and the bands were quantitated using densitometry.
Western Blot Analysis
Liver protein (40 μg) was separated by sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) gel electrophoresis and transferred to a nitrocellulose membrane (Schleicher & Schuell, Middlesex, UK). The membrane was blocked with 5% skim milk in 10 mM Tris–HCl containing 150 mM NaCl and 0.5% Tween 20 (TBS-T). After washing with TBS-T, the membrane was then incubated with a primary antibody that recognizes collagen type Ι (1:1000), TGF-β1 (1:100), and α-SMA (1:500, Cell Signaling, Beverly, MA, USA). After washing with TBS-T, a horseradish peroxidase-conjugated secondary antibody (New England Biolabs, Beverly, MA, USA) was applied to the membrane and the blot was developed using an enhanced chemiluminescence detection kit (Amersham, Piscataway, NJ, USA).
Statistical Analyses
All of the values were expressed as the mean ± standard error (SE). Significant differences between the groups were statistically analyzed using Student’s t-test. The differences between multiple groups were evaluated by a one-way analysis of variances (ANOVA), followed by a nonparametric post hoc test (LSD). A P value of 0.05 or less was considered statistically significant.
Results
Body and Liver Weights
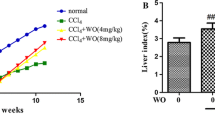
The effects of the morin on the body weight and liver weight of the rats are shown in Fig. 2. Treatment with DMN caused a significant decrease in both body weight and liver weight, compared with the control group. In the DMN group, body weight gain for 4 weeks was only 27% of the control, and oral administration of morin decreased this loss by 50%. Also, the final liver weight in the DMN group was 47% of that in the control group. However, liver weights in the morin group were 68% of that in the control group. This result showed that morin administration prevented this DMN-induced loss of liver weight. In addition, Fig. 2 implies that the administration of DMN to animals caused a significant (P < 0.05) decrease in relative liver weight, which is the average of liver weight at final body weight multiplied by 100. A significant increase in relative liver weight (P < 0.05) occurred with the cotreatment with morin. Relative liver weights in the morin group were 89% of that in the control group.
Effect of morin on the body and liver weights of rats treated with DMN. DMN was given intraperitoneally at a dose of 10 µl/kg on three consecutive days a week for 4 weeks to each group. Morin was administrated orally at a dose of 20 mg/kg three times a week. Relative liver weight is the average of liver weight at final body weight multiplied by 100. Values are expressed as mean ± SE (n = 6). # P < 0.05 versus control and *P < 0.05 versus DMN, respectively. DMN, DMN alone-induced group; Morin, DMN with morin-treated group
Serum Parameters of Liver Function
The effects of morin on the serum parameters in the liver fibrosis model are shown in Table 1. ALT is a cytosolic enzyme, primarily present in the liver. An increase in plasma ALT indicates liver damage more specifically than AST. AST, which is a mitochondrial enzyme present in large quantities in the heart, liver, skeletal muscles, and kidneys, in part indicates liver injury. Activities of the serum ALT and AST were increased 6.6- and 4-fold in the DMN treatment group, as compared with the control, respectively. However, both the ALT and AST level increased by DMN treatment were significantly suppressed by cotreatment with morin. The level of serum bilirubins (T. Bilirubin and D. Bilirubin) were assessed as representative indexes of liver function. DMN caused 18- and 21-fold increase in T. Bilirubin and D. Bilirubin levels, respectively, compared with the control, whereas morin almost completely suppressed the increases in bilirubin levels induced by DMN.
Liver Histopathology
Liver fibrosis was evaluated by two histological methods: H&E and MT staining. The results from these two methods showed the same pattern. The control group showed normal architecture, whereas the DMN group exhibited extensive hemorrhagic necrosis and disruption of tissue architecture (Fig. 3A2). These alterations were remarkably reduced in the morin group (Fig. 3A3). Also, serial sections were stained with MT for collagen. In the control, collagen was observed only in the periportal area (Fig. 3B1). The DMN group showed increased collagen, and displayed bundles of collagen fibers surrounding the lobules, forming large fibrous septa (Fig. 3B2). The thickening of these collagen fiber bundles was markedly reduced in the morin group (Fig. 3B3). The histopathological fibrosis scores analysis confirmed that the liver fibrosis was significantly reduced by morin treatment, as compared with the DMN group (i.e., fibrosis score, 3.0 ± 0.8 versus 2.0 ± 0.0, P < 0.05, Table 2).
The mRNA Expression of Collagen Type I, TGF-β1, and α-SMA
The mRNA expression levels of collagen type I, TGF-β 1 , and α-SMA were amplified by RT-PCR (Fig. 4). After normalization against the corresponding GAPDH, values from densitometric analyses were expressed as the average ratios of collagen type I/GAPDH, TGF-β 1 /GAPDH, and α-SMA/GAPDH, respectively. As shown in Fig. 4, the mRNA expression level for collagen type I in the DMN group (0.91 ± 0.09) was higher than in the control group (0.29 ± 0.04). However, the mRNA expression level for collagen type I in the morin group (0.66 ± 0.07) was significantly lower than that of the DMN group (P < 0.05). Like for collagen type I, the mRNA expression level of TGF-β 1 in the morin group (0.61 ± 0.04) also showed a significant difference, compared with the DMN group (0.72 ± 0.03). In addition, the mRNA expression level of α-SMA in the morin group (0.82 ± 0.06) was significantly decreased, compared with the DMN group (1.01 ± 0.05, P < 0.05).
The mRNA levels of collagen type I, transforming growth factor-β 1 (TGF-β 1 ), and α-smooth muscle actin (α-SMA) after treatment of morin by reverse-transcriptase polymerase chain reaction (RT-PCR). (a) Total RNA was prepared and RT-PCR was performed. The PCR products were separated on a 1.5% agarose gel and stained with ethidium bromide. (b) Quantification of collagen type I, TGF-β 1 , and α-SMA mRNA expression was performed by densitometric analysis. Values are expressed as mean ± SE of collagen type I/GAPDH, TGF-β 1 /GAPDH, and α-SMA/GAPDH for at least six separate experiments. * P < 0.05 versus DMN. Con, control; DMN, DMN alone-induced group; Morin, DMN with morin-treated group
The Protein Expression of Collagen Type I, TGF-β1, and α-SMA
We next assessed the effects of morin on the protein expression levels of collagen type I, TGF-β1, and α-SMA in the DMN-induced liver fibrosis rats. The levels of collagen type I, TGF-β1, and α-SMA protein were determined by Western blot analysis. As shown in Fig. 5, values from densitometric analysis after normalization against the corresponding β-actin were expressed as the average ratios of collagen type I/β-actin, TGF-β1/β-actin, and α-SMA/β-actin, respectively. As shown in Fig. 5, the protein expression level of collagen type I in the DMN group (0.73 ± 0.02) was higher than in the control group (0.04 ± 0.01), whereas the expression of collagen type I in the morin group (0.31 ± 0.06) was significantly decreased, compared with the DMN group (P < 0.05). Also, the expression level of TGF-β1 in the morin group (0.50 ± 0.02) was decreased statistically, compared with the DMN group (0.92 ± 0.05, P < 0.05). Like the results for mRNA expression, the protein expression of α-SMA in the morin group (0.66 ± 0.05) was significantly lower than that of the DMN group (0.88 ± 0.04, P < 0.05).
The expressions of collagen type I, transforming growth factor-β1 (TGF-β1), and α-smooth muscle actin (α-SMA) after treatment of morin by Western blot. (a) Liver protein (40 μg) was separated by SDS-PAGE, transferred to a nitrocellulose membrane, and blotted with anti-collagen type I, anti-TGF-β1, anti-α-SMA, or β-actin antibody. (b) Quantifications of collagen type I, TGF-β1, and α-SMA expressions were performed by densitometry analysis. Values are expressed as mean ± SE of collagen type I/β-actin, TGF-β1/β-actin, and α-SMA/β-actin for at least six separate experiments. * P < 0.05 versus DMN. Con, control; DMN, DMN alone-induced group; Morin, DMN with morin-treated group
Discussion
Hepatic fibrosis represents a common response to chronic liver injury from various origins. It is accompanied by hepatocellular necrosis and inflammation. DMN treatment causes liver fibrosis/cirrhosis, leading to shrunken livers, alteration of the hepatic architecture, and biological change [22, 23]. In the present study, a DMN-induced liver fibrosis model was successfully established, as evaluated by fibrosis score measurements, histological observations, and serum biochemical markers. Also, we found that morin exerted protective effects on DMN-induced hepatic fibrosis in rats. The results showed that the fibrosis scores of the livers from rats treated with morin were significantly reduced in comparison with those of the DMN-treated rats that were not given morin. In addition, in relation to histological changes, morin reduced the extensive disruption of tissue architecture and collagen fibers induced by DMN. It is known that serum biochemical markers, such as ALT, AST, and bilirubins, are representatives of liver function: their increased levels are indicators of liver damage. Here, it was exhibited that the levels of ALT, AST, and bilirubins were remarkably decreased by morin in rats with DMN-induced liver fibrosis. These results indicate that morin improves DMN-induced liver fibrosis in rats.
Hepatic fibrosis is usually initiated by hepatocyte damage, leading to the recruitment of inflammatory cells and platelets and the subsequent release of cytokines, such as TGF-β1 [24]. These factors probably affect the inflammatory and repairing phase of liver fibrosis by activating HSC [25, 26]. HSC, a principal cellular source of ECM during chronic liver injury, undergoes a transition into myofibroblast-like cells expressing α-SMA. Activated HSC is associated with cell proliferation and the accumulation of ECM, including collagen type I and α-SMA. In fact, the initiation stage is followed by the perpetuation stage, in which increased α-SMA and collagen type I are amplified by enhanced growth factor expression, such as TGF-β1. TGF-β1 is one of the major fibroblast growth factors [27] and plays a role as a crucial cytokine during HSC activation and the formation of liver fibrosis. Overexpression of TGF-β1 is involved in a number of disease processes in the liver [28]. Therefore, to determine the effect of morin, we additionally investigated the expression of fibrosis related molecules, including collagen type I, TGF-β1, and α-SMA in rats with DMN-induced fibrosis. Our study showed that morin reduced the expression of collagen type I, one of the main components of the ECM accumulation in liver fibrosis, and decreased the expression of TGF-β1, corresponding to a reduction of α-SMA expression. These results indicate a pivotal role of morin in reducing fibrogenesis progression.
In summary, the present study demonstrated that morin exhibited hepatoprotective and antifibrotic effects by decreasing collagen type I, TGF-β1, and α-SMA. Thus, we suggest that morin may be potentially useful in preventing the development of hepatic fibrosis.
References
Wijeratne SS, Abou-Zaid MM, Shahidi F (2006) Antioxidant polyphenols in almond and its coproducts. J Agric Food Chem 54:312–318. doi:10.1021/jf051692j
Aggarwal BB, Shishodia S (2006) Molecular targets of dietary agents for prevention and therapy of cancer. Biochem Pharmacol 71:1397–1421. doi:10.1016/j.bcp.2006.02.009
Xie MX, Long M, Liu Y, Qin C, Wang YD (2006) Characterization of the interaction between human serum albumin and morin. Biochim Biophys Acta 1760:1184–1191
Wu TW, Zeng LH, Wu J, Fung KP (1993) Morin hydrate is a plant-derived and antioxidant-based hepatoprotector. Life Sci 53:PL213–PL218. doi:10.1016/0024-3205(93)90266-6
Wu TW, Zeng LH, Wu J, Fung KP (1994) Morin: a wood pigment that protects three types of human cells in the cardiovascular system against oxyradical damage. Biochem Pharmacol 47:1099–1103. doi:10.1016/0006-2952(94)90424-3
Yu Z, Fong WP, CH Cheng (2006) The dual actions of morin (3, 5, 7, 2′, 4′-pentahydroxyflavone) as a hypouricemic agent. Uricosuric effect and xanthine oxidase inhibitory activity. J Pharmacol Exp Ther 316:169–175. doi:10.1124/jpet.105.092684
Kuo HM, Chang LS, Lin YL, Lu HF, Yang JS, Lee JH et al (2007) Morin inhibits the growth of human leukemia hl-60 cells via cell cycle arrest and induction of apoptosis through mitochondria dependent pathway. Anticancer Res 27:395–405
Manna SK, Aggarwal RS, Sethi G, Aggarwal BB, Ramesh GT (2007) Morin (3, 5, 7, 2′, 4′-pentahydroxyflavone) abolishes nuclear factor-kappab activation induced by various carcinogens and inflammatory stimuli, leading to suppression of nuclear factor-kappab-regulated gene expression and up-regulation of apoptosis. Clin Cancer Res 13:2290–2297. doi:10.1158/1078-0432.CCR-06-2394
Laughton MJ, Evans PJ, Moroney MA, Hoult JR, Halliwell B (1991) Inhibition of mammalian 5-lipoxygenase and cyclo-oxygenase by flavonoids and phenolic dietary additives. Relationship to antioxidant activity and to iron ion-reducing ability. Biochem Pharmacol 42:1673–1681. doi:10.1016/0006-2952(91)90501-U
Kawabata K, Tanaka T, Honjo S, Kakumoto M, Hara A, Makita H et al (1999) Chemopreventive effect of dietary flavonoid morin on chemically induced rat tongue carcinogenesis. Int J Cancer 83:381–386. doi:10.1002/(SICI)1097-0215(19991029)83:3<381::AID-IJC14>3.0.CO;2-X
Hsiang CY, Wu SL, Ho TY (2005) Morin inhibits 12-o-tetradecanoylphorbol-13-acetate-induced hepatocellular transformation via activator protein 1 signaling pathway and cell cycle progression. Biochem Pharmacol 69:1603–1611. doi:10.1016/j.bcp.2005.03.008
Friedman SL (2003) Liver fibrosis—from bench to bedside. J Hepatol 38(Suppl 1):S38–S53. doi:10.1016/S0168-8278(02)00429-4
Bataller R, Brenner DA (2005) Liver fibrosis. J Clin Invest 115:209–218
Pinzani M, Marra F (2001) Cytokine receptors and signaling in hepatic stellate cells. Semin Liver Dis 21:397–416. doi:10.1055/s-2001-17554
Lotersztajn S, Julien B, Teixeira-Clerc F, Grenard P, Mallat A (2005) Hepatic fibrosis: molecular mechanisms and drug targets. Annu Rev Pharmacol Toxicol 45:605–628. doi:10.1146/annurev.pharmtox.45.120403.095906
Yamazaki H, Inui Y, Yun CH, Guengerich FP, Shimada T (1992) Cytochrome p450 2e1 and 2a6 enzymes as major catalysts for metabolic activation of n-nitrosodialkylamines and tobacco-related nitrosamines in human liver microsomes. Carcinogenesis 13:1789–1794. doi:10.1093/carcin/13.10.1789
Bertelli AA, Giovannini L, Stradi R, Bertelli A, Tillement JP (1996) Plasma, urine and tissue levels of trans- and cis-resveratrol (3, 4′, 5-trihydroxystilbene) after short-term or prolonged administration of red wine to rats. Int J Tissue React 18:67–71
Lee MH, Yoon S, Moon JO (2004) The flavonoid naringenin inhibits dimethylnitrosamine-induced liver damage in rats. Biol Pharm Bull 27:72–76. doi:10.1248/bpb.27.72
Ala-Kokko L, Pihlajaniemi T, Myers JC, Kivirikko KI, Savolainen ER (1987) Gene expression of type i, iii and iv collagens in hepatic fibrosis induced by dimethylnitrosamine in the rat. Biochem J 244:75–79
Pilette C, Rousselet MC, Bedossa P, Chappard D, Oberti F, Rifflet H et al (1998) Histopathological evaluation of liver fibrosis: quantitative image analysis vs semi-quantitative scores. Comparison with serum markers. J Hepatol 28:439–446. doi:10.1016/S0168-8278(98)80318-8
Aleynik SI, Leo MA, Ma X, Aleynik MK, Lieber CS (1997) Polyenylphosphatidylcholine prevents carbon tetrachloride-induced lipid peroxidation while it attenuates liver fibrosis. J Hepatol 27:554–561. doi:10.1016/S0168-8278(97)80361-3
Savolainen ER, Brocks D, Ala-Kokko L, Kivirikko KI (1988) Serum concentrations of the n-terminal propeptide of type iii procollagen and two type iv collagen fragments and gene expression of the respective collagen types in liver in rats with dimethylnitrosamine-induced hepatic fibrosis. Biochem J 249:753–757
Jenkins SA, Grandison A, Baxter JN, Day DW, Taylor I, Shields R (1985) A dimethylnitrosamine-induced model of cirrhosis and portal hypertension in the rat. J Hepatol 1:489–499. doi:10.1016/S0168-8278(85)80747-9
Bauer M, Schuppan D (2001) TGFbeta1 in liver fibrosis Time to change paradigms? FEBS Lett 502:1–3. doi:10.1016/S0014-5793(01)02655-2
Giannelli G, Antonaci S (2005) Immunological and molecular aspects of liver fibrosis in chronic hepatitis C virus infection. Histol Histopathol 20:939–944
Wells RG (2005) The role of matrix stiffness in hepatic stellate cell activation and liver fibrosis. J Clin Gastroenterol 39:S158–S161. doi:10.1097/01.mcg.0000155516.02468.0f
Schnabl B, Kweon YO, Frederick JP, Wang XF, Rippe RA, Brenner DA (2001) The role of smad3 in mediating mouse hepatic stellate cell activation. Hepatology 34:89–100. doi:10.1053/jhep.2001.25349
Gressner AM, Weiskirchen R, Breitkopf K, Dooley S (2002) Roles of TGF-beta in hepatic fibrosis. Front Biosci 7:d793–d807. doi:10.2741/gressner
Acknowledgment
This work was supported by an Inha University Research Grant.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Hee-Seung Lee and Kyung Hee Jung have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Lee, HS., Jung, K.H., Park, IS. et al. Protective Effect of Morin on Dimethylnitrosamine-Induced Hepatic Fibrosis in Rats. Dig Dis Sci 54, 782–788 (2009). https://doi.org/10.1007/s10620-008-0404-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-008-0404-x