Abstract
Gastroesophageal reflux disease (GERD) is a common disease in infants and children. Prolonged (24-hr) pH monitoring in the esophagus for determination of increased acid exposure has, together with endoscopy, been the only routinely implemented method for GERD diagnosis. The recently introduced multiple intraluminal impedance (MII) provides additional information about the number of both acid and nonacid episodes of retrograde bolus movement in the esophagus. The aim of this study was to investigate the day-to-day reproducibility and the interobserver variability of 24-hr combined MII (number of nonacid and acidic reflux episodes) and pH in the esophagus in infants and children. Upper endoscopy followed by 2 × 24-hr consecutive combined MII and pH monitoring was performed in 33 infants and children referred to a tertiary center for evaluation of GERD. The study was performed in a hospital setting without dietary restrictions. Bland-Altman difference versus mean plots and calculation of the limits of agreement (LOA) were used for assessment of the reproducibility of the total number of acidic and nonacidic reflux episodes. LOA for the number of acidic reflux episodes on day 2 were 0.2–5.3 times the value obtained on day 1. For the total number of nonacidic reflux episodes, LOA were 0.04–8.6; for the total number of reflux episodes, 0.3–3.3. An abnormal reflux index on one or both recording days was found in 7 of 30 patients. In conclusion, considerable day-to-day variability was found for nonacidic reflux episodes. Less variability was found for acidic reflux episodes. This variability must be taken into consideration for the use of MII in the clinical evaluation of infants and children with GERD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the last decades 24-hr pH monitoring has been the gold standard for the evaluation of gastroesophageal reflux disease (GERD) in infants and children. The fraction of time at a pH < 4, the so-called reflux index (RI), may be calculated as the main parameter for acid exposure. Age-specific normal values have been compiled for the RI [1, 2]. However, prolonged pH monitoring as a diagnostic tool has several limitations in the evaluation of pediatric GERD [3]. The frequently fed infant poses a particular problem, as a number of nonacidic reflux episodes are produced due to the postprandial buffering of the gastric pH. Accordingly, the esophageal pH probe will be unable to register reflux episodes for a proportion of the monitoring time [4].
The development of multichannel intraluminal electrical impedance (MII) monitoring facilitates measurement of retrograde bolus movement in the esophagus independent of the pH [5–7]. Combination of the two techniques has been shown to give additional information compared to pH monitoring alone [8]. The distinction between acid and nonacid reflux episodes and the temporal association with symptoms [9] have been used in studies of the association between GERD and symptoms such as apnea [10] and cough [11]. Normal values for 24-hr combined pH/impedance monitoring have been published for adults [12, 13] but not for infants and children. The reproducibility of pH monitoring in infants and children has been investigated in several studies. We performed a study of 2 × 24-hr continuous esophageal pH in 30 infants and children and observed considerable intraindividual day-to-day variability, rendering pH monitoring a limited tool in interventional studies [14]. The study was performed in a clinical setting with no dietary or activity restrictions. A wireless probe in the esophagus has been developed [15], which may be of practical use in children. However, a recent study with the wireless pH probe showed similar performance as to reproducibility in children [16].
The reproducibility of pH/MII measurements has been investigated in 72 healthy adult subjects, with acceptable findings of 24-hr ambulatory impedance-pH, as assessed by Bland-Altma (BA) plots but without the calculation of limits of agreement (LOA) [6]. Furthermore, postprandial impedance and pH signals were solely recorded in 20 healthy volunteers during 90-min postprandial periods on 2 separate days. The reproducibility of MII was found to be comparable to the reproducibility of pH monitoring alone [17].
The detection of reflux by impedance can be done by semiautomatic software, but for a more precise interpretation, the traces must be investigated by hand. A recent study of 16,627 23-sec on-screen recording segments analyzed by three investigators showed a high level of inter- and intraobserver agreements in detection of the single reflux episode [18]. Studies of observer agreement of 24-hr pH/MII recordings have not been published.
The aim of the present study was to investigate the reproducibility of reflux parameter obtained by 2 times 24 hr consecutive pH/MII monitoring in children and infants with symptoms of GERD. In addition, the inter- and intraobserver variability of interpretation of combined pH/MII traces was investigated.
Methods
Subjects
Gastroesophageal reflux was studied by ambulatory 24-hr impedance/pH measurements in 33 infants and children (16 girls and 17 boys). All were referred with symptoms of GERD. The symptoms represented a wide range, from a 1-month-old infant with a history of apnea to a 14-year-old girl with abdominal pain and heartburn. Mean age was 4.7 years (range, 1 month to 14 years.) Three of the subjects were excluded from the study (one due to technical problems and two children who discontinued the probe and afterward their parents refused a replacement). Written informed consent was obtained from parents of all subjects. The protocol was approved by the regional ethics committee (Ref VF 20040226).
Procedure
A Sleuth multichannel intraluminal impedance ambulatory system (Sandhill Scientific, Inc., Highlands Ranch, CO, USA) was used for esophageal impedance and pH measurement. This system consists of a portable data logger and a catheter. The catheters used in this study contain one antimony pH electrode and six impedance channels. The principle of impedance measurements is based on the application of a low AC voltage across six ring sets. Resulting current changes indicate bolus movement episodes and the direction of movement present at each respective ring set. Three different probes were used: ZIN-S61C01E (height, <75 cm), ZPN-S61C01E (height, 75–150 cm), and ZAN-S61C01E (height, >150 cm). The probes had an external reference electrode which was placed on the chest of the subject. All probes were discharges after a single use. The data were sampled in a data logger at 50 Hz on a memory card and downloaded to a personal computer.
The studies were performed on an inpatient basis for both recording days. Proton pump inhibitor (PPI) treatment was discontinued at least 7 days before the procedure. All patients underwent upper endoscopy performed with Olympus GIF-N230 videoscopes (GIF-N230, GIFXP-240, and GIFX-160) under general anesthesia. During the procedure biopsies were obtained from the upper gastrointestinal tract. Esophagitis was classified according to the LA classification [10]. The lower esophageal sphincter (LES) was identified endoscopically and the distance to the mouth was measured. A combined pH/impedance probe was placed transnasally and the pH measuring channel was positioned 3 cm above the LES. During the 48-hr investigation the infants and children were encouraged to maintain a normal pattern of activity. No mealtime limitations were given; the duration of meals and sleeping periods were registered in a diary. The parents and subjects were instructed to use the event markers in case of specific predefined symptoms. The analysis was done by two investigators, both experienced in the analysis of pH/impedance tracings, with analysis of more than 100 recordings. Visual identification of individual reflux events was done, and the number of reflux (acidic or nonacidic) episodes registered. Finally, esophageal exposure to volume and acid was calculated.
The following parameters were measured for the assessment of esophageal motility.
-
Reflux index (RI): Defined as the fraction of recording time at a pH <4. The NASPGHAN 2001 criteria [2] were used for classification of the measurements into normal or pathologic.
-
All reflux: The total number of reflux episodes.
-
Acid reflux episode: Retrograde bolus movement detected by impedance accompanied by a fall in pH fall to <4.0.
-
Nonacid reflux episode: Retrograde bolus movement detected by impedance accompanied by a pH which remains >4.0.
Statistics
A difference-versus-mean plot, the so-called Bland-Altman (BA) plot [19], was used for analysis of the reproducibility of impedance and pH data obtained on the 2 recording days. The mean difference between the 2 recording days ± 1.96 SD was calculated as the LOA. Assessment of agreement among the investigators was done using BA plots, as the data were continuous. For testing differences between two groups the Wilcoxon two-sample rank-sum test was used. We used a P value of 0.05 as the level of significance.
Results
pH data
Data from 2 × 24-hr impedance/pH are presented in Table 1. Note that data are presented as median and percentile values, as they were not normally distributed. Median RI for all participants was 2.6% on the first recording day and 4.6% on the second; there was no significant difference between day 1 and day 2 (P = 0.15).
The reproducibility of the GERD diagnosis as based on the NASPGHAN criteria for RI was 77%. Seven subjects (23%) had discordant results on the 2 recording days; six of these subjects had a normal RI on day 1, and one showed the opposite phenomenon. The study group was divided into two: the group with an abnormal RI (14/30) on one or both recording days had median RI values of 10.3 (day 1) and 10.0 (day 2), respectively, and the group with a normal RI (16/30) on both recording days had RI values of 1.6 and 3.1 (Table 1), respectively.
Impedance data
The median number of all reflux episodes for all patients on the first and second recording days was 95 and 98, respectively. There was no significant difference between the 2 recording days in all reflux, acid reflux, or nonacid reflux (Table 1).
Comparison between the group with a normal RI (n = 16) and the group with an abnormal RI (n = 14), no significant differences were found on either of the recording days for the total number of reflux, acid reflux, and nonacid reflux episodes. The median all reflux percentage time detected by impedance time on the first recording day was 1.25%; the percentage time for nonacid reflux was 0.4%. These numbers are markedly lower than those found for the RI on that day.
Analysis of reproducibility
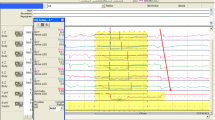
Reproducibility of the variables obtained by impedance/pH measurement was calculated for the 30 subjects who completed 2 × 24-hr consecutive pH/MII measurement. The reproducibility of the variables, the mean, and the difference from the mean were calculated and plotted in a difference-versus-mean plot (BA plot). Figure 1 shows all reflux episodes. As shown in Fig. 1 (plots 1A–4A), a cone-shaped distribution of the data typically appeared, illustrating that the difference was proportional to the mean. This effect was compensated by logarithmic transformation (plots 1B–4B), and the upper (mean + 2 SD) and lower (mean −2 SD) LOA were calculated by back transformation (Table 2). The reproducibility of all reflux episodes (Fig. 1, plots 1A and 1B) showed an upper LOA of 3.3 and a lower LOA of 0.3.
For acidic reflux (Fig. 1, plots 2A and 2B) the LOA was 0.2–5.3, and the corresponding value for nonacidic reflux episodes (Fig. 1, plots 3A and 3B) was 0.04–8.6. In conclusion, the best reproducibility was found for all reflux episodes and the worst was found for acid and nonacid reflux.
Inter- and intraobserver variability
The 30 2 × 24-hr combined impedance/pH recordings were analyzed by two observers, both experienced in analysis of impedance/pH tracings. Figure 2 shows a BA plot of the results of the first recording day for all reflux, acidic reflux, and nonacidic reflux for each of the investigators. The dots are scattered relatively closely, indicating a low variability between the two investigators. This is supported by the LOA of 0.5–1.5.
Endoscopy and histology
Esophagitis according to the LA classification [20] was observed in two patients. Five patients had superficial inflammation without mucosal breaks in the mucosa of the LES. Histological inflammation in the biopsies from the esophagus was found in six patients.
Discussion
The use of combined MII and pH is a new tool in the evaluation of pediatric GERD. MII/pH measurement may give new insight into the patophysiology of GERD, as MII/pH can directly establish the relationship between symptoms and retrograde bolus movement in the esophagus. The analyzed parameters include the number of retrograde movements and the length of time for the retrograde movements, Furthermore; the height of the reflux episode is conveniently measured by MII. The latter is potentially important in infants and children with respiratory symptoms, as the height may reflect the risk of respiratory complications of the reflux events.
For transition into clinical practice, the versatility of MII/pH depends on the performance characteristics of the methodology. In the present study we investigated 30 infants and children with combined MII and pH on 2 consecutive recording days. The day-to-day variability and the intraobserver variability in MII/pH recording were evaluated.
In a previous study of 2 × 24-hr consecutive pH monitoring [14], we found that the upper and lower LOA were 0.3 and 3.3. These findings were comparable to the LOA for RI obtained in the present study. The reproducibility of the GERD diagnosis based on the RI on each of the recording days was 77%. To our knowledge, no studies have evaluated the reproducibility of MII in infants and children. In the present evaluation of the impedance parameters, “all reflux” showed the best reproducibility, with LOA of 0.3–33. A greater span was found for nonacid and acid reflux episodes. The reproducibility for the total number of reflux episodes was significantly better than that found for RI. The higher variability of acidic and nonacidic reflux episodes may have several causes. The lower number by itself may influence the outcome. This study was done in a routine clinical setting. The infants and children all underwent upper endoscopy and placement of the probe under general anesthesia on day 1. We may assume that the reproducibility would have been better if the eating pattern on day 1 was repeated, however, this does not reflect the daily-life situation.
It is our opinion that MII tracing must be analyzed manually and that reading of the MII tracings requires experience. The agreement between the two investigators on number of acid, nonacid, and all reflux episodes was acceptable based on BA plots and the LOA. Low variability was found between the two experienced investigators.
The study group could be divided into two groups based on the RI cutoff values for normal or pathological reflux. The MII values showed no significant difference between the two groups with regard to the total number of all reflux, acid reflux, and nonacid reflux episodes. These findings correspond to a recently published paper stating that there was no difference in the mean number of acid or nonacid reflux episodes in patients with normal and abnormal pH probe studies [21]. This paper describes significantly more pH-only episodes in the group with an abnormal RI [11]. Our data support the conclusion that pH-metry should be included in pH/MII analysis.
Normal values for MII have been established in adults in both an American and a European study [12, 13], but these values are not suitable for diagnostic use in infants and children, as the meal and physical activity patterns are quite different. At present no normal values for infants and children exist. In the present study we found a 95th percentile value for all reflux of 88 on the first and 69 on the second recording day in the group with a normal RI. These are not to be regarded as normal values because the study subjects were all symptomatic and included both infants and children, but the values are comparable to the values found in both the American and the European study of normal adult values, e.g., 74 and 76 reflux episodes. Even though not a cutoff limit, together with a temporal relationship between a retrograde bolus and a symptom, this knowledge can strengthen the GERD diagnosis.
In conclusion, simultaneous MII and pH monitoring is conveniently done in children and infants. MII/pH proved to be technically reliable, as using the catheters only once resulted in malfunction in only 1 of 33 patients. The lack of normal values and the high day-to-day variability of MII/pH observed in the present study limit the usefulness of the number of reflux episodes as a marker for GERD as well as for interventional studies. The strength of this new investigational tool is its ability to establish a temporal association between specific clinical events and the detection of a retrograde bolus movement in the esophagus.
References
Vandenplas Y, Goyvaerts H, Helven R, Sacre L (1991) Gastroesophageal reflux, as measured by 24-hour pH monitoring, in 509 healthy infants screened for risk of sudden infant death syndrome. Pediatrics 88:834–840
Rudolph CD, Mazur LJ, Liptak GS, et al. (2001) Guidelines for evaluation and treatment of gastroesophageal reflux in infants and children: recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr 32(Suppl 2):S1–S31
Wenzl TG, Moroder C, Trachterna M, et al. (2002) Esophageal pH monitoring and impedance measurement: a comparison of two diagnostic tests for gastroesophageal reflux. J Pediatr Gastroenterol Nutr 34:519–523
Mitchell DJ, McClure BG, Tubman TR (2001) Simultaneous monitoring of gastric and oesophageal pH reveals limitations of conventional oesophageal pH monitoring in milk fed infants. Arch Dis Child 84:273–276
Skopnik H, Silny J, Heiber O, Schulz J, Rau G, Heimann G (1996) Gastroesophageal reflux in infants: evaluation of a new intraluminal impedance technique. J Pediatr Gastroenterol Nutr 23:591–598
Sifrim D, Silny J, Holloway RH, Janssens JJ (1999) Patterns of gas and liquid reflux during transient lower oesophageal sphincter relaxation: a study using intraluminal electrical impedance. Gut 44:47–54
Castell DO, Vela M (2001) Combined multichannel intraluminal impedance and pH-metry: an evolving technique to measure type and proximal extent of gastroesophageal reflux. Am J Med 111(Suppl 8A):157S–159S
Sifrim D, Holloway R, Silny J, et al. (2001) Acid, nonacid, and gas reflux in patients with gastroesophageal reflux disease during ambulatory 24-hour pH-impedance recordings. Gastroenterology 120:1588–1598
Sifrim D, Castell D, Dent J, Kahrilas PJ (2004) Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut 53:1024–1031
Wenzl TG, Schenke S, Peschgens T, Silny J, Heimann G, Skopnik H (2001) Association of apnea and nonacid gastroesophageal reflux in infants: Investigations with the intraluminal impedance technique. Pediatr Pulmonol 31:144–149
Sifrim D, Dupont L, Blondeau K, Zhang X, Tack J, Janssens J (2005) Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut 54:449–454
Zerbib F, des Varannes SB, Roman S, et al. (2005) Normal values and day-to-day variability of 24-h ambulatory oesophageal impedance/pH monitoring in a Belgian-French cohort of healthy subjects. Aliment Pharmacol Ther 22:1011–1021
Shay S, Tutuian R, Sifrim D, et al. (2004) Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol 99:1037–1043
Nielsen RG, Kruse-Andersen S, Husby S (2003) Low reproducibility of 2×24-hour continuous esophageal pH monitoring in infants and children: a limiting factor for interventional studies. Dig Dis Sci 48:1495–1502
Pandolfino JE, Richter JE, Ours T, Guardino JM, Chapman J, Kahrilas PJ (2003) Ambulatory esophageal pH monitoring using a wireless system. Am J Gastroenterol 98:740–749
Hochman JA, Favaloro-Sabatier J (2005) Tolerance and reliability of wireless pH monitoring in children. J Pediatr Gastroenterol Nutr 41:411–415
Bredenoord AJ, Weusten BL, Timmer R, Smout AJ (2005) Reproducibility of multichannel intraluminal electrical impedance monitoring of gastroesophageal reflux. Am J Gastroenterol 100:265–269
Peter CS, Sprodowski N, Ahlborn V, et al. (2004) Inter- and intraobserver agreement for gastroesophageal reflux detection in infants using multiple intraluminal impedance. Biol Neonate 85:11–14
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Lundell LR, Dent J, Bennett JR, et al. (1999) Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 45:172–180
Rosen R, Lord C, Nurko S (2006) The sensitivity of multichannel intraluminal impedance and the pH probe in the evaluation of gastroesophageal reflux in children. Clin Gastroenterol Hepatol 4:167–172
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dalby, K., Nielsen, R.G., Markoew, S. et al. Reproducibility of 24-Hour Combined Multiple Intraluminal Impedance (MII) and pH Measurements in Infants and Children. Evaluation of a Diagnostic Procedure for Gastroesophageal Reflux Disease. Dig Dis Sci 52, 2159–2165 (2007). https://doi.org/10.1007/s10620-006-9731-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-006-9731-y