Abstract
pH monitoring and multichannel intraluminal impedance (pH-MII) are two catheter-based methods for measuring reflux. pH monitoring has been the gold standard test for measuring acid reflux and forms the basis for many therapeutic trials. Its primary limitations are that (1) it only can measure acid reflux yet misses non-acid reflux, (2) it cannot differentiate swallowed contents from reflux contents, and (3) it cannot accurately measure refluxate height. pH-MII can overcome all of these limitations yet data is lacking on how pH-MII changes clinical outcome beyond a standard pH probe. Additionally, there are no normal pH-MII values in children other than preterm infants and the interpretation of the studies is still time consuming both of which currently limit the clinical utility of the test. pH-MII has, however, replaced pH monitoring in diagnostic and therapeutic reflux trials and undoubtedly the limitations of the technology will be overcome with additional future studies. This chapter discusses in detail the benefits and limitations of these technologies, as well as some other new methods of reflux monitoring.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Reflux Episode
- Reflux Event
- Multichannel Intraluminal Impedance
- Acid Suppression Therapy
- Pathologic Reflux
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Gastroesophageal reflux disease (GERD) is defined by the reflux of gastric contents into the esophagus resulting in well-defined symptoms and complications [1, 2]. In many cases, GERD can be diagnosed based on history alone; however, when patients present with atypical complaints or do not respond to medical therapy, objective testing may be necessary to assess the frequency and duration of acid reflux, or to document the association between gastroesophageal reflux (GER) and specific symptoms. Diagnostic techniques designed to discriminate between physiologic and pathologic reflux have been developed.
Esophageal pH monitoring, which employs a pH electrode to detect acid reflux in the distal esophagus, was first introduced in 1969 [3]. Over the years the advantages and limitations of traditional, catheter-based esophageal pH monitoring have become better understood, with a subsequent evolution to newer diagnostic techniques. Wireless methods to detect acidic contents in the esophagus have now become available (Bravo pH capsule) and pharyngeal probes have recently been introduced (Restech). Additionally, multichannel intraluminal impedance with pH (MII-pH) has been introduced as a novel method to measure acid and non-acid reflux. In the present chapter, we will discuss the technical details, clinical indications and applications of these diagnostic techniques for the dynamic detection of reflux episodes.
Catheter-Based Esophageal pH-Monitoring
Catheter-based esophageal pH monitoring is the most widely available and commonly used method to document abnormal acid exposure and correlate symptoms with acid reflux episodes. Testing quantifies the frequency and duration of acid reflux episodes, usually over an 18–24 h period. Most ambulatory catheter-based pH probes contain a small antimony electrode connected to a portable data logger that records intraesophageal pH, as well as events during the study, such as symptoms, meals, position changes, and activity. The methodology of esophageal pH monitoring has become relatively standardized with specific guidelines for use in children [4, 5].
Electrode Placement
Appropriate placement of the pH electrode relative to the lower esophageal sphincter (LES) is very important in order to gather accurate data. At higher distances above the LES, there is a linear decrease in acid exposure time, which decreases the sensitivity of the test. Adult protocols typically recommend that the pH electrode be positioned 5 cm above the superior margin of the LES in order to decrease the risk of slipping into the stomach during swallow-induced shortening of the esophagus [6]. Stationary esophageal manometry, usually performed as a separate procedure, is optimal for determination of LES location. In children however, this additional invasive procedure is not routinely performed. Strobel’s formula may be used to approximate the esophageal length for initial placement of the pH electrode above the LES [length from nares to LES (cm) = 5 + 0.252(height)] [7]. In the absence of manometry however, fluoroscopy should be used to confirm placement of the sensor at the level of the third vertebral body above the diaphragm, according to recommendations from the Working Group of the European Society of Pediatric Gastroenterology and Nutrition [5].
Recording Conditions
The optimal duration of monitoring should be at least 18 h, including a day and a night period [5]. Shorter studies have been proposed (30 min, 2 h, 8 h, and 12 h studies) but no study period has been found to be sufficiently sensitive or reproducible to replace the 24 h studies [8, 9]. Instructions for feeding and activity during the study should represent a balance between maintaining a degree of standardization and recreating a normal lifestyle with minimal restrictions. Although a strict standardized diet is generally not necessary, a minimum of three meals should be included. Meal periods are routinely excluded from the analysis because the pH probe cannot differentiate swallowed acidic contents from refluxate [10, 11]. Documentation of patient position and activity during the study should also be recorded since the effect of body position on different patterns of GER has been well reported; acid reflux is more common in the supine and right lateral positions than the prone or left lateral positions [4, 12]. Depending on the aim of the study, H2-blockers and proton-pump inhibitors should be stopped at least 3 or 7 days prior to the study, respectively. Adult data in healthy volunteers suggests that intragastric pH returns to baseline within 2–4 days after stopping acid suppression [13].
Definitions and Criteria
After the study is completed, data is downloaded from the data logger and analyzed with computer software. A reflux episode is usually defined as a drop in pH below 4 that lasts for more than 5 s [14]. The reflux index, which is the percentage of time of the entire duration of the investigation with pH <4 is generally considered the single most important variable in clinical practice for both adults and children [4, 6]. A pH of 4 is generally accepted as the optimum cutoff in both children and adults, based on early studies of correlating acid exposure with heartburn [15–17]. The threshold of pH < 4 also provides the best discrimination between subjects with proven reflux disease (the presence of esophagitis) and asymptomatic controls [6, 18, 19]. However, there is significant overlap between the reflux profiles of patients with and without symptoms and in patients with and without esophagitis because there are many possible criteria that define pathologic reflux, including the number of episodes greater than 5 min, the longest reflux episode, the percentage of time pH < 4, and the total number of reflux events. Several scores have been proposed, including the DeMeester score and the Boix-Ochoa score, but the current gold standard for reporting pH monitoring results is the reflux index, which is the percentage of time of the entire duration of the investigation with pH < 4 [4, 6].
Normal Ranges
Normative data are essential to guide interpretation of pH monitoring results and distinguish between physiologic versus pathologic reflux. Published pediatric data is rather limited, however, due to the difficulty in obtaining data from truly healthy and asymptomatic volunteers. In some studies, “normals” were obtained from children hospitalized for GER evaluations who turned out to be asymptomatic during the time of pH monitoring [20] or were found to have other causes for their gastrointestinal symptoms [21]. Overall, studies suggest that physiologic acid reflux is a common occurrence in infants during the first year of life, with decreased acid exposure found in older children and adults [20–24]. Based on the available data, the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) has established guidelines that define the upper limit of normal of the reflux index up to 12% in the first year of life and up to 6% thereafter [4].
Diagnostic Accuracy and Reproducibility
The estimated sensitivity of pH monitoring for predicting esophagitis in children is good, ranging from 83 to 100%, but the severity of reflux as measured by pH monitoring has not been found to necessarily correlate with the severity of symptoms [15, 25]. For children with non-erosive reflux disease (NERD), the clinical utility of pH monitoring has not been well studied. In adults, there is significant overlap between patients with NERD and normal patients; approximately 40% of adults with NERD had pathologic reflux but 60% did not, making the differentiation of normal patients from NERD patients difficult based on reflux burden alone [26, 27].
Reports on intrasubject reproducibility of esophageal pH results in children have had varied results. Vandenplas et al. studied infants and children over two consecutive 24-h periods; the correlation coefficients for the reflux index and number of reflux episodes between day 1 and day 2 were 0.95 and 0.98, respectively [28]. In contrast, the correlation coefficient for the reflux index reported by Mahajan and colleagues was only 0.62 between day 1 and day 2 [29]. In another study, 9 out of 30 children had discordant (normal versus abnormal) results between the two recording days, yielding an overall reproducibility of 70% [30]. Hampton et al found that there was discordance between day 1 and day 2 studies in 62% of infants. An additional study was done in the pediatric population comparing the amount of reflux in children who has pH monitoring with and without anesthesia; Hampton et al found that there was discordance between day 1 and day 2 studies in 62% of infants. An additional study was done in the pediatric population comparing the amount of reflux in children who has pH monitoring with and without anesthesia; McCallion et al found that the reproducibility of the percent time pH<4 was 85%. [31, 32]. Overall, there appears to be some degree of day-to-day variability among patients; whether these differences are clinically significant is debatable. When the clinical picture is unclear, consideration should be given for repeat testing.
The next question to ask is whether obtaining pH probe results translate into improvement in clinical outcome. Malfroot et al. found that 75% of patients with abnormal pH monitoring experienced symptomatic improvement in their pulmonary symptoms suggesting that it accurately measures pathologic reflux [33]. A randomized control trial of acid suppression in children with pathologic reflux by pH monitoring showed that between 69 and 74% of patients with pathologic reflux experience symptomatic improvement with acid suppression, suggesting that pH probe accurately predicts clinical response [34]. There is very limited data on the impact of this test on clinical outcome; the majority of data is on the correlation of esophagitis with clinical outcome and since there is a correlation between esophagitis and pH abnormalities, it may be reasonable to assume that there is a correlation between reflux burden and symptom improvement but there are few studies to support this directly.
Symptom Correlation
In addition to the quantification of reflux, 24-h esophageal pH monitoring also provides the opportunity to assess the temporal relationship between episodes of reflux and onset of symptoms. This may be especially helpful for patients with nonspecific or extraesophageal symptoms. Lam et al. found that using a two minute time window was best for correlation of chest pain with reflux, although the optimal time window for symptom–reflux association may vary depending on the particular symptom of interest [35].
Several statistical methods have been developed to better quantify the association of symptoms and reflux episodes but there is no conclusive data proving one index to be superior to the others. The symptom index (SI) is defined as the percentage of symptom episodes that are related to reflux, with a score of ≥50% suggesting a positive relationship between symptom and reflux [36, 37]. A second approach is the symptom sensitivity index (SSI), which divides the number of reflux episodes associated with symptoms by the total number of reflux episodes [38]. An arbitrary cutoff of 10% or higher is commonly used to indicate a significant association between symptoms and reflux episodes. The SI may overestimate the relationship between reflux and symptoms when there are a high number of reflux episodes, and the SSI is more likely to be positive when the number of symptom episodes is high. More recently, the symptom association probability (SAP) has been introduced. Using Fisher’s exact test, this method expresses the statistical likelihood that the patient’s symptoms are related to reflux [39]. By statistical convention, SAP ≥95% indicates that the probability that the observed association between reflux and the symptom occurred by chance is <5%.
While these indices are helpful for research, it is essential to determine if these indices predict symptom response to acid suppression. Taghavi et al. found that the SSI and the SAP predicted a response to acid suppression but this was an imperfect relationship. Although patients with a positive relationship between symptoms and reflux have been shown to more likely to respond to medical and surgical therapy, further prospective validation studies are needed [40, 41]. Unfortunately, all of these indices rely on the patient to accurately record symptoms immediately as they occur. Additionally, while these may suggest a temporal association, they do not always prove causality.
Pharyngeal pH Monitoring
Proving causality is even more difficult in the patient with extraesophageal manifestations of reflux (hoarseness, recurrent pneumonia, otitis media, and sinusitis) as there is an often unsatisfactory correlation between esophageal reflux and extraesophageal symptoms. As a result, the measurement of oropharyngeal acidification has been proposed as a more accurate indicator of proximal reflux than dual channel pH probes. The Restech Dx-pH probe (Respiratory Technology Corp., San Diego, CA) is a recently introduced, transnasal, oropharyngeal pH sensor. Besides being less invasive than traditional catheters, the antimony-based sensor is also designed to measure the pH of both liquid and aerosolized droplets in the posterior oropharynx. Investigators have recently proposed the use of less acidic pH thresholds or relative drops in pH to identify episodes of reflux in the posterior oropharynx, based on the hypothesis that the threshold of pH <4 may be too stringent and insensitive and that pH changes above 4 may be damaging to laryngeal tissue [42, 43].
The clinical validity of these alternative criteria, however, is not yet established. A previous study which employed pharyngeal pH monitoring found that 92% of pharyngeal pH decreases of 1–2 pH units and 66% of pH <4 events were artifactual or independent of esophageal acidification [44]. Moreover, recent studies which combined the Restech oropharyngeal pH probe with concurrent esophageal pH monitoring in adults have also found inconsistencies between oropharyngeal and distal esophageal pH data, with higher numbers of non-correlating oropharyngeal pH events during sleep and supine periods [45, 46].
Chiou et al., who used the Restech probe in children, found that a high proportion of oropharyngeal pH events did not correlate with distal reflux by pH-MII, especially with the use of alternative pH criteria and during supine periods [47]. One reason for this finding may be that decreased salivary flow during sleep leads to drying of the oropharyngeal pH electrode and subsequently false readings. This phenomenon was initially described by Wiener et al. as “pharyngeal pseudo-reflux” in reference to artifacts with a gradual descent to pH <4 without a corresponding fall in esophageal pH [48]. The utility of pharyngeal monitoring is still questionable and additional studies are underway to validate its use.
Wireless pH Monitoring
One of the main limitations to all of the catheter-based tests is that patient discomfort can be significant, such that their typical eating and activity patterns are altered to the point that the study may not be representative of a “typical” day for the patient. To overcome this limitation, a wireless method has recently been devised. The Bravo pH system (Medtronic, Shoreview, MN) consists of an antimony electrode contained within a small capsule which is pinned to the mucosal wall of the distal esophagus during an upper GI endoscopy and transmits pH data wirelessly to a portable receiver using radiotelemetry. The capsule can remain in place for up to 4 or more days but typically is in place for at least 2 days allowing for extended recording. In adults, the capsule is placed 6 cm above the squamocolumnar junction, with placement confirmation by endoscopy [49]. There are currently no specific guidelines for placement in children. Adult series have reported significant chest discomfort, early detachment of the capsule, perforation, and the need for endoscopic removal of the capsule but because of the small case series in pediatrics, the extent of Bravo complications in children is still largely unknown [49–51].
In published studies of children older than 4 years old, pH monitoring with the Bravo capsule was better tolerated than the transnasal catheter in terms of appetite, activity, and satisfaction, with no significant complications other than mild chest discomfort [52–54]. Because of the prolonged recording, using this technique there is additional opportunity for the correlation of symptoms with reflux, particularly symptoms that do not typically occur on a daily basis.
Only one study to date has compared the Bravo capsule side-by-side with a simultaneous transnasal pH catheter in children. Croffie and colleagues found no significant difference in the reflux index obtained by the two devices on day 1; on day 2, however, the median reflux index recorded by the Bravo capsule was significantly higher compared to day 1 of both the capsule and catheter [54]. The clinical significance of this is unclear, with only one patient having discordant (abnormal versus normal) results between the 2 days of recording.
Several pediatric studies have compared the pH results between day 1 and day 2 of the Bravo studies. In a study of Bravo in 23 children, Gunnarsdottir et al. found no statistically significant differences in the reflux profiles between the first 24 h and the entire 48-h recording but 7 children received a different classification (normal versus abnormal) between day 1 and 2 [55]. In a series of 145 Bravo studies in children, there were significantly more long duration events and a higher percentage of time that the pH was less than 4 in the upright position on day 1 compared to day 2 [52]. Currently, there is no consensus on whether the interpretation of the results should rely on the first or the second day or average of the days; outcome studies are needed to make this determination.
Currently, Bravo is a reasonable alternative for patients that cannot tolerate a catheter-based system, but the need for anesthesia for placement (and the resultant associated costs) combined with the need to stop acid suppression therapy may limit its utility in becoming the gold standard reflux tool [51, 56].
Proximal Esophageal pH Monitoring
Proximal esophageal pH monitoring is designed to assess the proximal extent of acid reflux and its relationship with oropharyngeal and respiratory symptoms. Studies employing dual-probe pH monitoring of both the distal and proximal esophagus have provided mixed results in terms of sensitivity and specificity for extra-esophageal manifestations of reflux, intra-subject reproducibility and prediction of response to therapy [57, 58]. Additionally, there is poor correlation between the acidification in the proximal sensor with the acidification in the distal esophagus raising the question of whether the proximal acidification has any significance in the absence of distal acidification. In pediatrics, because there are a limited number of catheter sizes and a wide range of esophageal lengths, it is difficult to ensure that the proximal sensor is uniformly in the same location without compromising distal sensor location. Furthermore, it is unclear which pH level produces damage to bronchial, laryngeal and pharyngeal tissue and while the literature is based on a pH cut-off of 4, non-acid reflux with pH 4–7 may also play a clinically significant role in aerodigestive diseases [59, 60]. At the current time however, the clinical advantage of proximal esophageal pH monitoring in children is not yet clearly proven and more studies are needed to validate their use.
Multichannel Intraluminal Impedance (pH-MII)
MII-pH uses sensors distributed throughout the esophagus to measure resistance to flow rather than pH changes alone. The advantages of pH-MII are the following: (1) the sensors are able to determine the directionality of flow so that reflux events can be distinguished from swallows; (2) multiple sensors throughout the esophagus allows for accurate determination of refluxate height; (3) the sensors, which do not rely on pH, are able to detect non-acid reflux which is common in the pediatric population, in the acid suppressed patient and in the postprandial period [61–63]; and (4) because liquid and gas have different impedances, the sensors can differentiate the composition of the refluxed material.
Traditionally, there are seven impedance sensors placed in series which generate six impedance waves, one for each pair of adjacent sensors (Fig. 12.1). Sensors are distributed throughout the esophagus at different spacing depending on the size of the catheter that is used (infant for ages 0–2, pediatric for ages 2–10 and adult for children older than 10). Since the impedance sensors cannot differentiate between acid versus non-acid material, a distal pH sensor has been added to the catheter allowing the clinician to determine whether the flow across the catheter is acidic, weakly acidic, or non-acidic, depending on the pH value.
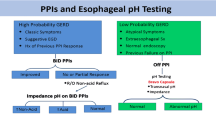
The pH-MII catheter is inserted through the nose and the catheter is positioned so the distal pH sensor is at the third vertebral body above the diaphragmatic angle (Fig. 12.2) [5]. Studies are performed for 24 h and, as with pH studies, meals are conventionally excluded from analyses. Typically, when performing pH studies, acid suppression medications are stopped a minimum of 48 h prior to testing because the pH probe cannot detect non-acid reflux, which is prevalent in the acid suppressed patient [64]. Since the pH-MII catheter can detect acid and non-acid reflux, the studies can be performed off or on acid suppression therapy, although adult studies suggest that symptom correlation may be improved if medications are stopped prior to pH-MII testing [65].
Definitions
A liquid episode is defined as a drop in impedance to 50% of the baseline value or below, with a subsequent recovery back to 50% of the baseline value. This drop in impedance needs to be visualized in at least the distal two channels to be considered “reflux.” Gas reflux is defined as simultaneous increases in impedance to greater than 8,000 Ω in two or more channels. Mixed reflux has components of both liquid and gas. There are three types of reflux episodes that can be detected: (1) acid reflux events detected by both the impedance and the pH-sensor, (2) non-acid reflux events, which are detected only by the impedance sensors, and (3) pH-only events, which are detected only by the pH sensor, without any impedance changes. In some studies, non-acid reflux is further subdivided into weakly acidic reflux (pH 4–7) and alkaline reflux (pH > 7). The importance of pH-only events is still questionable and the current theory is that pH only episodes represent very distal reflux that does not meet criteria for an impedance detected event (i.e., the reflux does not reach the required three impedance sensors).
Interpretation
The interpretation of impedance tracings is time-consuming and in most research laboratories is still done by hand even though there is commercially available analysis software. Roman et al. studied the concordance of the automated software (Sandhill Scientific) to detect reflux events compared to a manual scoring of the events. Agreement between visual and automated analysis was good (Kendall’s coefficient W > 0.750, P < 0.01) for all parameters. They also analyzed symptom detection, and concluded that despite good agreement with manual analysis, automatic analysis overestimated the number of non-acid reflux events [66]. Manual analysis remains the gold standard to detect an association between symptoms and non-acid reflux events [66]. Hemmink et al. determined the sensitivity of the automated software (Medical Measurement Systems) and found that sensitivity of the software was 73 ± 4%. Additionally, the automated software incorrectly determined a symptom association 16–20% of the time, depending on the symptom index used [67]. There are selected populations where the impedance software is particularly inaccurate; manual interpretation is critical in the presence of esophagitis or if there is a motility disorder, such as achalasia or esophageal atresia, all of which lower impedance baselines. The low impedance baseline results in significant underestimations of the amount of reflux present.
Sensitivity
Impedance sensors have been shown to accurately detect boluses in the esophagus down to 0.1 ml using fluoroscopy [68, 69]. The difficulty in determining the sensitivity of pH-MII is which gold standard technique should be used as the basis for comparison; the pediatric studies have used reflux detected by any device (pH-MII and pH probe) as the gold standard. Rosen et al. found that the sensitivity of pH-MII was 76 ± 13% compared to the pH probe whose sensitivity was 80 ± 18%. When patients taking acid suppression were studied, the sensitivity of the pH probe dropped to 47 ± 36% whereas the sensitivity of pH-MII in medicated patients was 80 ± 21% [70]. Francavilla et al. found that the sensitivity of pH-MII was 86 ± 12%, that this sensitivity was higher in infants compared to children as infants have more non-acid reflux events, and that impedance resulted in a higher symptom index, symptom sensitivity index, and symptom association probability than the pH probe [71]. Wenzl et al. found that in untreated infants, the sensitivity of pH-MII to detect acid reflux events was 54% compared to the pH probe [72]. Failure of pH-MII to report reflux events detected by pH probe primarily occurs when (1) there is a persistent drop in pH less than 4 even after the bolus had been cleared by impedance, (2) the pH hovers around 4 with multiple drops to less than 4, or (3) pH drops are associated with swallows.
Reproducibility
Dalby et al. performed 48 h impedance studies in 30 children to determine the degree of variability between the first and second day of recording [73]. The authors found that the reproducibility for the total number of reflux events in each patient between different days was better than the reproducibility for the number of acid or non-acid events individually. On a population basis, there was no significant difference between the median total number, acid or non-acid events between day 1 and day 2 [73]. Results from adult studies support this pediatric study. Aanen et al., in a study of 21 adults, found that the number of acid, weakly acidic, and total events was similar between the 2 days with a Kendall’s W value ranging from 0.9 to 0.92, where a value of 1 indicates perfect concordance. Additionally, the reproducibility of symptom indices using the SAP, SI and SSI was 0.9, 0.73, and 0.86 respectively [74]. Similarly Zerbib et al. found, in 27 adults, that there was good reproducibility for the number, acidity and composition of reflux events (Kendall’s W-values = 0.72–0.85) [75].
Normal Values
One of the current limitations to pH-MII monitoring is the lack of normal pediatric values to differentiate physiologic from pathologic reflux. Adult normal values have been published. Shay et al. conducted a multicenter study of 60 healthy volunteers and found that the upper limit of normal for total, acid, weakly acid, and non-acid reflux were 73, 55, 26, and 1, respectively [76]. Zerbib et al. found similar numbers in normal adults with the upper limit of normal for healthy adults for total, acid, weakly acid, and non-acid reflux were 75, 50, 33, and 15, respectively [75].
Normal preterm infant values differ significantly from adults; the upper limit for total number of reflux events was 100 of which up to 52% can be acid and up to 98% can be non-acid [61]; the study, however, was performed with nasogastric tubes in place which can stent open the Lower Esophageal Sphincter and increase the number of reflux events by more than 50%, suggesting that these values may be artificially high [77]. In contrast, in a small study of older children (n = 10, patients with normal pH recording and normal esophageal biopsies and no gastrointestinal symptoms), the 95th percentile for total events was 69, a value very similar to adult data [78]. Obviously, larger studies are needed to confirm the range of normal values in children. Because normal cut-off values are not available in pediatrics, the main role of impedance is to correlate symptoms with reflux events.
Symptom Association
Given the lack of normative data to determine normal pH-MII in children, the most important use of the technique has been to study the temporal association between symptoms and reflux. There is significant debate in the adult literature about the optimal way to correlate reflux with symptoms but the literature is clear that pH-MII is superior to pH monitoring alone when evaluating symptom correlation [59, 65, 79, 80]. The rates of symptom index (SI), symptom sensitivity index (SSI), and the symptom association probability (SAP) positivity have been studied using MII-pH. In adults, Aanen et al. found that the SAP and the SSI were the most reproducible indices in patients who had two impedance studies separated by a minimum of 1 week [74]. Similarly, Brendenoord et al. found that the SAP was the most frequently positive index followed by the SI and then the SSI. They also found that the addition of pH-MII over a standard pH probe increased the number of patients with a positive SI and SAP but did not increase the number of patients with a positive SSI [79].
In pediatrics, Rosen et al. studied 28 children taking acid suppression therapy for intractable respiratory symptoms; in these patients, more patients had a positive SI for respiratory symptoms using MII-pH than pH probe alone but there was no difference in the number of patients with a positive SSI when MII-pH was used compared to a standard pH probe [59]. In contrast, Thilmany et al. found that the rate of positivity for the SI was higher for acid reflux episodes whereas the rate of positivity of SSI was higher for non-acid reflux episodes suggesting that the value of pH-MII may differ depending on what symptom index is used [81]. Loots et al. studied 50 children undergoing pH-MII testing and found that uniformly pH-MII resulted in a higher symptom association, regardless of the index used, compared to pH probe and that the SAP was the most frequently positive symptom index [82].
One of the limitations of symptom indices is that they only represent a significant temporal relationship rather than a true cause and effect relationship. The normal cut off values, therefore, represent statistical definitions and are not linked to clinical outcomes; the normal values of 50% for the SI, 10% for the SSI and 95% for the SAP were not generated by investigating clinical outcomes. Rosen et al. looked at the value of the SI and the SSI in predicting fundoplication outcome. They found that neither a positive SI nor an SSI predicted fundoplication results and, using ROC curves, there was no clear cut off value for either index predicting outcome [83]. These data suggest that a temporal association alone does not prove causality which is the key limitation to all of the symptom indices. A second limitation of the symptom indices is the time lag between when a symptom occurs and when the patient actually records the symptom. In a study by Sifrim et al., there was an average delay of 28 s between the time when a patient coughed and when they actually recorded a cough on the symptom log [84]. Furthermore, patients only recorded, on average, 38% of coughs on the log [84]. To address this limitation, impedance sensors can be paired with pressure sensors which measures esophageal pressure spikes occurring when a patient coughs. Coughs appear as simultaneous high pressure spikes in the esophagus and this allows for precise correlation between reflux and cough without the possibility for recording error. Because the placement of two catheters can be uncomfortable, new technologies are on the horizon to measure cough-reflux associations less invasively.
Proximal Reflux
One of the advantages of MII-pH is that the multiple sensors can detect full column reflux which is extremely important when determining the impact of reflux on the airways. Rosen et al. found that, in children with severe respiratory symptoms, full column reflux is more highly associated with respiratory symptoms than distal reflux [59]. The importance of full column reflux in the generation of symptoms is further supported by Jadcherla et al. who found that acid reflux events reaching the proximal esophagus were four times more likely to be associated with symptoms that distal events [85]. The next step is to determine whether full column reflux predicts clinical outcome. Rosen et al. found that full column reflux events, rather than total reflux burden, predicted a positive surgical outcome after fundoplication [86]. In other studies, the relationship between full column reflux and symptoms is less clear. Condino et al. found that, in asthmatic children, proximal reflux was not a predictor of symptom generation [80]. Because extraesophageal symptoms represent the consequences of a heterogeneous grouping of diseases, it is often difficult to determine a definitive relationship between full column events and symptoms, but it is becoming increasingly clear that full column reflux may be an important component of a pH-MII report.
Impedance and Clinical Outcome
The role of impedance in improving clinical outcomes is uncertain at this time. Several adult studies have shown that pH-MII may predict a clinical response to therapy [87, 88]. There is only a single pediatric study which investigated the role of how pH-MII testing changed clinical outcome. For each pH-MII done for clinical reasons, Rosen et al. gave the results of the pH portion of the test and asked the referring gastroenterologist how the pH results changed management. The MII portion of the test was then given to the ordering clinician who was again asked how this result changed clinical management. Out of 50 impedances ordered by 23 attendings, the MII portion of the test changed the clinical management of the patient 22% of the time. Whether this change in management results in patient improvement is unknown.
The Future for MII
Currently, evidence indicates that pH-MII has replaced the gold standard pH-only monitoring for the evaluation of reflux in a research setting. It also seems to be the new gold standard for the evaluation of patients with persistent symptoms in the postprandial period and for patients with persistent symptoms despite acid suppression therapy. The utility of the technology is limited by the time-consuming nature of the study interpretation and a paucity of evidence to prove that it improves clinical outcomes over a standard pH monitoring.
References
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–20.
Sherman PM, Hassall E, Fagundes-Neto U, et al. A global, evidence-based consensus on the definition of gastroesophageal reflux disease in the pediatric population. Am J Gastroenterol. 2009;104:1278–95.
Spencer J. Prolonged pH recording in the study of gastro-oesophageal reflux. Br J Surg. 1969;56:912–4.
Rudolph C, Mazur L, Liptak G, et al. Guidlines for evaluation and treatment of gastroesophageal reflux in infants and children: recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr. 2001;32:S1–31.
Vandenplas Y, Belli D, Boige N. A standardized protocol for the methodology of esophageal pH monitoring and interpretation of the data for the diagnosis of gastro-esophageal reflux. J Pediatr Gastroenterol Nutr. 1992;14:467–71.
Hirano I, Richter J. ACG practice guidelines: esophageal reflux testing. Am J Gastroenterol. 2007;102:668–85.
Strobel C, Byrne W, Ament M, Euler A. Correlation of esophageal lengths in children with height: application to the Tuttle test without prior esophageal manometry. J Pediatr. 1979;94:81–4.
Jolley SG, Tunell WP, Carson JA, Smith EI, Grunow J. The accuracy of abbreviated esophageal pH monitoring in children. J Pediatr Surg. 1984;19:848–54.
Tolia V, Kauffman RE. Comparison of evaluation of gastroesophageal reflux in infants using different feedings during intraesophageal pH monitoring. J Pediatr Gastroenterol Nutr. 1990;10:426–9.
Wo JM, Castell DO. Exclusion of meal periods from ambulatory 24-hour pH monitoring may improve diagnosis of esophageal acid reflux. Dig Dis Sci. 1994;39:1601–7.
Ter RB, Johnston BT, Castell DO. Exclusion of the meal period improves the clinical reliability of esophageal pH monitoring. J Clin Gastroenterol. 1997;25:314–6.
Tobin JM, McCloud P, Cameron DJ. Posture and gastro-oesophageal reflux: a case for left lateral positioning. Arch Dis Child. 1997;76:254–8.
Bell N, Karol MD, Sachs G, Greski-Rose P, Jennings DE, Hunt RH. Duration of effect of lansoprazole on gastric pH and acid secretion in normal male volunteers. Aliment Pharmacol Ther. 2001;15:105–13.
van Wijk MP, Benninga MA, Omari TI. Role of the multichannel intraluminal impedance technique in infants and children. J Pediatr Gastroenterol Nutr. 2009;48:2–12.
Cucchiara S, Staiano A, Gobio Casali L, Boccieri A, Paone F. Value of the 24 hour intraoesophageal pH monitoring in children. Gut. 1990;31:129–33.
Vandenplas Y, Franckx-Goossens A, Pipeleers-Marichal M, Derde M, Sacre-Smits L. Area under pH 4: advantages of a new parameter in the interpretation of esophageal pH monitoring data in infants. J Pediatr Gastroenterol Nutr. 1989;9:34–9.
Wenner J, Johansson J, Johnsson F, Oberg S. Optimal thresholds and discriminatory power of 48-h wireless esophageal pH monitoring in the diagnosisof GERD. Am J Gastroenterol. 2007;102:1862–9.
Steiner SJ, Gupta SK, Croffie JM, Fitzgerald JF. Correlation between number of eosinophils and reflux index on same day esophageal biopsy and 24 hour esophageal pH monitoring. Am J Gastroenterol. 2004;99:801–5.
Black D, Haggitt R, Orenstein S, Whitington P. Esophagitis in infants. Morphologic histological diagnosis and correlation with measures of gastroesophageal reflux. Gastroenterology. 1990;98:1408–14.
Boix-Ochoa J, Lafuenta J, Gil-Vernet J. Twenty-four hour esophageal pH monitoring in gastroesophageal reflux. J Pediatr Surg. 1980;15:74–8.
Cucchiara S, Santamaria F, Minella R, et al. Simultaneous prolonged recordings of proximal and distal intraesophageal pH in children with gastroesophageal reflux disease and respiratory symptoms. Am J Gastroenterol. 1995;90:1791–6.
Euler A, Byrne W. Twenty-four-hour esophageal intraluminal pH probe testing: a comparative analysis. Gastroenterology. 1981;80:957–61.
Sondheimer J. Continuous monitoring of distal esophageal pH: a diagnostic test for gastroesophageal reflux in infants. J Pediatr. 1980;96:804–7.
Vandenplas Y, Goyvaerts H, Helven R, et al. Gastroesophageal reflux, as assessed by 24-hour pH monitoring, in 509 healthy infants screened for SIDS-risk. Pediatrics. 1991;88:834–40.
Salvatore S, Hauser B, Vandemaele K, Novario R, Vandenplas Y. Gastroesophageal reflux disease in infants: how much is predictable with questionnaires, pH-metry, endoscopy and histology? J Pediatr Gastroenterol Nutr. 2005;40:210–5.
Savarino E, Zentilin P, Tutuian R, et al. The role of nonacid reflux in NERD: lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol. 2008;103:2685–93.
Bredenoord AJ, Hemmink GJ, Smout AJ. Relationship between gastro-oesophageal reflux pattern and severity of mucosal damage. Neurogastroenterol Motil. 2009;21:807–12.
Vandenplas Y, Helven R, Goyvaerts H, et al. Reproducibility of continuous 24 hour oesophageal pH monitoring in infants and children. Gut. 1990;31:374–7.
Mahajan L, Wyllie RLO, et al. Reproducibility of 24-hour intraesophageal pH monitoring in pediatric patients. Pediatrics. 1998;101:260–3.
Nielsen R, Kruse-Andersen S, Husby S. Low reproducibility of 2 × 24-hour continuous esophageal pH monitoring in infants and children: a limiting factor for interventional studies. Dig Dis Sci. 2003;48:1495–502.
Hampton F, MacFadyen U, Simpson H. Reproducibility of 24 hour oeosophageal pH studies in infants. Arch Dis Child. 1990;65:1249–54.
McCallion WA, Gallagher TM, Boston VE, Potts SR. Effect of general anaesthesia on prolonged intraoesophageal pH monitoring. Arch Dis Child. 1995;73:235–8.
Malfroot A, Vandenplas Y, Verlinden M, Piepsz A, Dab I. Gastroesophageal reflux and unexplained chronic respiratory disease in infants and children. Pediatr Pulmonol. 1987;3:208–13.
Gunasekaran T, Gupta S, Gremse D, et al. Lansoprazole in adolescents with gastroesophageal reflux disease: pharmacokinetics, pharmacodynamics, symptom relief efficacy, and tolerability. J Pediatr Gastroenterol Nutr. 2002;35 Suppl 4:S327–35.
Lam H, Breumelhof R, Roelofs J, Van Berge Henegouwen G, Smout A. What is the optimal time window in a symptom analysis of 24-hour esophageal pressure and pH data? Dig Dis Sci. 1994;39:402–9.
Ward B, Wu W, Richter J, et al. Ambulatory 24-hour esophageal pH monitoring. Technology searching for a clinical application. J Clin Gastroenterol. 1986;8:59–67.
Singh S, Richter JE, Bradley LA, Haile JM. The symptom index. Differential usefulness in suspected acid-related complaints of heartburn and chest pain. Dig Dis Sci. 1993;38:1402–8.
Breumelhof R, Smout A. The symptom sensitivity index: a valuable additional parameter in 24-hour esophageal pH monitoring. Am J Gastroenterol. 1991;86:160–4.
Weusten B, Roelofs J, Akkermans L, Van Berge Henegouwen G, Smout A. symptom-association probability: an improved method for symptom analysis of 24-hour esophageal pH data. Gastroenterology. 1994;107:1741–5.
Taghavi S, Ghasedi M, Saberi-Firoozi M, et al. Symptom association probability and symptom sensitivity index: preferable but still suboptimal predictors of response to high dose omeprazole. Gut. 2005;54:1067–71.
Diaz S, Aymerich R, Clouse RE. The symptom association probability (SAP) is superior to the symptom index (SI) for attributing symptoms to gastroesophageal reflux: validation using outcome from laparoscopic antireflux surgery (LARS). Gastroenterology. 2002;122:A75.
Wiener GJ, Tsukashima R, Kelly C, et al. Oropharyngeal pH monitoring for the detection of liquid and aerosolized supraesophageal gastric reflux. J Voice. 2009;23:498–504.
Ayazi S, Lipham JC, Hagen JA, et al. A new technique for measurement of pharyngeal pH: normal values and discriminating pH threshold. J Gastrointest Surg. 2009;13:1422–9.
Williams R, Ali G, Wallace K. Esophagopharyngeal acid regurgitation: dual pH monitoring criteria for its detection and insights into mechanisms. Gastroenterology. 1999;117:1051–61.
Golub JS, Johns III MM, Lim JH, DelGaudio JM, Klein AM. Comparison of an oropharyngeal pH probe and a standard dual pH probe for diagnosis of laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. 2009;118:1–5.
Chheda NN, Seybt MW, Schade RR, Postma GN. Normal values for pharyngeal pH monitoring. Ann Otol Rhinol Laryngol. 2009;118:166–71.
Chiou E, Rosen R, Nurko S. Correlation of changes in oropharyngeal pH with gastroesophageal reflux events in children. J Pediatr Gastroenterol Nutr. 2009;49:E36.
Wiener G, Koufman J, Wu W, et al. Chronic hoarseness secondary to gastroesophageal reflux disease: documentation with 24-h ambulatory pH monitoring. Am J Gastroenterol. 1989;84:1503–8.
Pandolfino JE, Richter JE, Ours T, Guardino JM, Chapman J, Kahrilas PJ. Ambulatory esophageal pH monitoring using a wireless system. Am J Gastroenterol. 2003;98:740–9.
Lacy B, Edwards S, Paquette L, Weiss J, Kelley M, Ornvold K. Tolerability and clinical utility of the Bravo pH capsule in children. J Clin Gastroenterol. 2009;43(6):514–9.
Fajardo NR, Wise JL, Locke GR, Murray JA, Talley NJ. Esophageal perforation after placement of wireless Bravo pH probe. Gastrointest Endosc. 2006;63:184–5.
Souza AL, Morley-Fletcher A, Nurko S, Rodriguez L. BRAVO wireless pH in children: is there an effect of anesthesia? Gastroenterology. 2009;136:A-510.
Gunnarsdottir A, Stenstrom P, Arnbjornsson E. Wireless esophageal pH monitoring in children. J Laparoendosc Adv Surg Tech. 2008;18:443–7.
Croffie J, Fitzgerald J, Molleson J, et al. Accuracy and tolerability of the Braco catheter-free pH capsule in patients between the ages of 4 and 18 years. J Pediatr Gastroenterol Nutr. 2007;45:559–63.
Gunnarsdottir A, Stenstrom P, Arnbjornsson E. 48-hour wireless oesophageal pH-monitoring in children: are two days better than one? Eur J Pediatr Surg. 2007;17:378–81.
Pandolfino J, Kahrilas P. Prolonged pH monitoring: Bravo capsule. Gastrointest Endosc Clin North Am. 2005;15:307–18.
Toila V, Vandenplas Y. Systematic review: the extra-oesophageal symptoms of gastro-oesophageal reflux disease in children. Aliment Phamacol Ther. 2009;29:258–72.
Vaezi MF, Richter JE, Stasney CR, et al. Treatment of chronic posterior laryngitis with esomeprazole. Laryngoscope. 2006;116:254–60.
Rosen R, Nurko S. The importance of multichannel intraluminal impedance in the evaluation of children with persistent respiratory symptoms. Am J Gastroenterol. 2004;99:2452–8.
Patterson N, Mainie I, Rafferty G, et al. Nonacid reflux episodes reaching the pharynx are important factors associated with cough. J Clin Gastroenterol. 2009;43:414–9.
Lopez-Alonso M, Moya MJ, Cabo JA, et al. Twenty-four-hour esophageal impedance-pH monitoring in healthy preterm neonates: rate and characteristics of acid, weakly acidic, and weakly alkaline gastroesophageal reflux. Pediatrics. 2006;118:e299–308.
Mitchell DJ, McClure BG, Tubman TR. Simultaneous monitoring of gastric and oesophageal pH reveals limitations of conventional oesophageal pH monitoring in milk fed infants. Arch Dis Child. 2001;84:273–6.
Sifrim D, Holloway R, Silny J, Tack J, Lerut A, Janssens J. Composition of the postprandial refluxate in patients with gastroesophageal reflux disease. Am J Gastroenterol. 2001;96:647–55.
Vela MF, Camacho-Lobato L, Srinivasan R, Tutuian R, Katz PO, Castell DO. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology. 2001;120:1599–606.
Hemmink GJ, Bredenoord AJ, Weusten BL, Monkelbaan JF, Timmer R, Smout AJ. Esophageal pH-impedance monitoring in patients with therapy-resistant reflux symptoms: ‘on’ or ‘off’ proton pump inhibitor? Am J Gastroenterol. 2008;103:2446–53.
Roman S, des Bruley Varannes S, Pouderoux P, et al. Ambulatory 24-h oesophageal impedance-pH recordings: reliability of automatic analysis for gastro-oesophageal reflux assessment. Neurogastroenterol Motil. 2006;18:978–86.
Hemmink GJ, Bredenoord AJ, Aanen MC, Weusten BL, Timmer R, Smout AJ. Computer analysis of 24-h esophageal impedance signals. Scand J Gastroenterol. 2011;46(3):271–6.
Imam H, Shay S, Ali A, Baker M. Bolus transit patterns in healthy subjects: a study using simultaneous impedance monitoring, videoesophagram, and esophageal manometry. Am J Physiol Gastrointest Liver Physiol. 2005;288:G1000–6.
Peter CS, Wiechers C, Bohnhorst B, Silny J, Poets CF. Detection of small bolus volumes using multiple intraluminal impedance in preterm infants. J Pediatr Gastroenterol Nutr. 2003;36:381–4.
Rosen R, Lord C, Nurko S. The sensitivity of multi-channel intraluminal impedance (MII) compared to pH probe in the detection of gastroesophgeal reflux in children. Clin Gastroenterol Hepatol. 2006;4:167–72.
Francavilla R, Magista AM, Bucci N, et al. Comparison of esophageal pH and multichannel intraluminal impedance testing in pediatric patients with suspected gastroesophageal reflux. J Pediatr Gastroenterol Nutr. 2010;50:154–60.
Wenzl TG, Moroder C, Trachterna M, et al. Esophageal pH monitoring and impedance measurement: a comparison of two diagnostic tests for gastroesophageal reflux. J Pediatr Gastroenterol Nutr. 2002;34:519–23.
Dalby K, Nielsen RG, Markoew S, Kruse-Andersen S, Husby S. Reproducibility of 24-hour combined multiple intraluminal impedance (MII) and pH measurements in infants and children. Evaluation of a diagnostic procedure for gastroesophageal reflux disease. Dig Dis Sci. 2007;52:2159–65.
Aanen MC, Bredenoord AJ, Numans ME, Samson M, Smout AJ. Reproducibility of symptom association analysis in ambulatory reflux monitoring. Am J Gastroenterol. 2008;103:2200–8.
Zerbib F, des Varannes SB, et al. Normal values and day-to-day variability of 24-h ambulatory oesophageal impedance-pH monitoring in a Belgian-French cohort of healthy subjects. Aliment Pharmacol Ther. 2005;22:1011–21.
Shay S, Tutuian R, Sifrim D, et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol. 2004;99:1037–43.
Peter CS, Wiechers C, Bohnhorst B, Silny J, Poets CF. Influence of nasogastric tubes on gastroesophageal reflux in preterm infants: a multiple intraluminal impedance study. J Pediatr. 2002;141:277–9.
Rosen R, Furuta G, Fritz J, Donovan K, Nurko S. Role of acid and nonacid reflux in children with eosinophilic esophagitis compared with patients with gastroesophageal reflux and control patients. J Pediatr Gastroenterol Nutr. 2008;46:520–3.
Bredenoord AJ, Weusten BL, Timmer R, Conchillo JM, Smout AJ. Addition of esophageal impedance monitoring to pH monitoring increases the yield of symptom association analysis in patients off PPI therapy. Am J Gastroenterol. 2006;101:453–9.
Condino AA, Sondheimer J, Pan Z, Gralla J, Perry D, O’Connor JA. Evaluation of gastroesophageal reflux in pediatric patients with asthma using impedance-pH monitoring. J Pediatr. 2006;149:216–9.
Thilmany C, Beck-Ripp J, Griese M. Acid and non-acid gastro-esophageal refluxes in children with chronic pulmonary diseases. Respir Med. 2007;101:969–76.
Loots CM, Benninga MA, Davidson GP, Omari TI. Addition of pH-impedance monitoring to standard pH monitoring increases the yield of symptom association analysis in infants and children with gastroesophageal reflux. J Pediatr. 2009;154:248–52.
Rosen R, Levine P, Lewis J, Mitchell P, Nurko S. Reflux events detected by pH-MII do not determine fundoplication outcome. J Ped Gastroenterol Nutrit 2010 Mar;50(3):251–5.
Sifrim D, Dupont L, Blondeau K, Zhang X, Tack J, Janssens J. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54:449–54.
Jadcherla SR, Gupta A, Fernandez S, et al. Spatiotemporal characteristics of acid refluxate and relationship to symptoms in premature and term infants with chronic lung disease. Am J Gastroenterol. 2008;103:720–8.
Rosen R, Levine P, Lewis J, Mitchell P, Nurko S. Reflux events detected by pH-MII do not determine fundoplication outcome. J Pediatr Gastroenterol Nutr. 2010;50:251–5.
Mainie I, Tutuian R, Agrawal A, Adams D, Castell DO. Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication. Br J Surg. 2006;93:1483–7.
Becker V, Bajbouj M, Waller K, Schmid RM, Meining A. Clinical trial: persistent gastro-oesophageal reflux symptoms despite standard therapy with proton pump inhibitors—a follow-up study of intraluminal-impedance guided therapy. Aliment Pharmacol Ther. 2007;26:1355–60.
Acknowledgment
This work was supported in part by NIH NIDDK073713 (R.R.).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Rosen, R., Chiou, E. (2013). Esophageal pH and Impedance Monitoring. In: Faure, C., Di Lorenzo, C., Thapar, N. (eds) Pediatric Neurogastroenterology. Clinical Gastroenterology. Humana Press, Totowa, NJ. https://doi.org/10.1007/978-1-60761-709-9_12
Download citation
DOI: https://doi.org/10.1007/978-1-60761-709-9_12
Published:
Publisher Name: Humana Press, Totowa, NJ
Print ISBN: 978-1-60761-708-2
Online ISBN: 978-1-60761-709-9
eBook Packages: MedicineMedicine (R0)