Abstract
The treatment options for palliating malignant gastroduodenal obstruction include open gastrojejunostomy (OGJ), laparoscopic gastrojejunostomy (LGJ), and endoscopic stenting (ES). The aim of this study was to compare the clinical outcomes and costs among ES, OGJ, and LGJ in patients who present with gastroduodenal obstruction from advanced upper gastrointestinal tract cancer. We designed a model for patients with malignant gastroduodenal obstruction. We analyzed success rates, complication rates and costs of the three treatment modalities: ES, OGJ, and LGJ. Baseline outcomes and costs were based on published reports. Success was defined as no major procedure-related and long-term complications over a 1-month period. Failure of therapy was defined as recurrent symptoms or death due to a procedural complication. Sensitivity analyses and cost-effectiveness analyses for the various strategies were performed. ES resulted in the lowest mortality rate and the lowest cost of the three treatment options analyzed. Mortality in the OGJ group was 2.1 times that in the ES cohort and 1.8 times that in the LGJ cohort. Sensitivity analyses confirmed ES as the dominant strategy. In conclusion, ES is the preferred treatment for palliation of duodenal obstruction due to advanced upper gastrointestinal tract cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Malignant gastroduodenal obstruction is a late complication from local extension of carcinoma of the pancreas, stomach, or duodenum, occurring in up to 20% of patients [1–3]. As a result, patients develop nausea, vomiting, weight loss, and anorexia, leading to a markedly impaired quality of life [4]. For these reasons an adequate palliative procedure is essential in improving the quality of life for patients with unresectable cancer. Adequate palliative options have to effectively relieve the symptoms of obstruction, result in acceptable morbidity and mortality and be cost-effective. The treatment option that offers all these benefits remains controversial.
Options for the treatment of gastroduodenal obstruction include surgical bypass procedures (open or laparoscopic) and endoscopic palliation by insertion of a self-expanding metallic stents (SEMS). Either treatment option has an initial success rate of >90% [5–8]. For several decades the only option available for palliation was via an open gastrojejunostomy (OGJ) [9, 10]. With the introduction of laparoscopic techniques, laparoscopic gastrojejunostomy (LGJ) was adopted as the palliative procedure of choice at many institutions. OGJ is associated with higher morbidity and mortality than LGJ (Table 1) and may be associated with improved quality of life [6, 7, 11, 12]. Although surgical methods have higher rates of early mortality and morbidity than endoscopic methods, they are much more durable and require less re-intervention compared to nonsurgical methods such as endoscopic stenting (ES). ES is initially more cost-effective and is associated with lower morbidity and mortality as well as providing the advantage of being performed in an outpatient setting. ES has not been compared to surgical procedures in randomized controlled trials to determine the best approach for palliation [13, 14]. The aim of our study was to use decision analysis to simulate a trial comparing OGJ, LGJ, and ES to compare clinical outcomes, complications, and cost-effectiveness over a 1-month period in patients with malignant duodenal obstruction.
Methods
Decision analysis
Medical decision analysis is a method to determine the optimal treatment strategy for a given clinical scenario. This requires construction of a decision tree, which is a precise representation of the various treatment options being compared and the major consequences of these options. If the probability of the outcomes can be estimated, then the treatment modality that optimizes the outcome can be determined.
Literature review
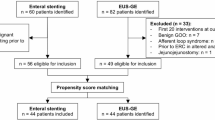
A MEDLINE search examining the English-language literature was performed using the following terms: pancreatic neoplasm, duodenal neoplasm, gastric neoplasm, gastroduodenal obstruction, open gastrojejunostomy, laparoscopic gastrojejunostomy, self-expanding metal stents, cost, morbidity, and mortality. Published articles were reviewed and examined for morbidity and mortality in peer-reviewed journals of surgery and gastroenterology. Only studies that had nine or more patients and outcome data that could be extracted were used. Updated series took precedence over older studies from the same institution. There was some difference in the studies with regard to design, patient number, patient population, and experience of the participating surgeon and/or gastroenterologist. A total of 33 studies were evaluated. Weighted means for each parameter were calculated from the usable trials and applied to our decision tree. All probabilities for clinical inputs in the model, as well as the range tested in the sensitivity analysis, are summarized in Table 1.
Decision analytic model
Using a decision analysis software program, DATA 3.5 (TreeAge Software Inc., Williamstown, MA), we evaluated clinical outcomes, failure rates, testing characteristics, complication rates, and costs in patients with malignant gastroduodenal obstruction from advanced upper GI cancer over a 1-month period in three treatment groups: group A, ES; group B, OGJ; and group C, LGJ.
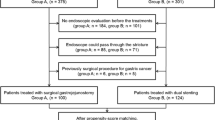
For each of the groups, the analysis started with a cohort of 100 hypothetical patients with malignant gastroduodenal obstruction. Patients were divided into a subset of those who had immediate complications following the procedure and those who had no procedural complications. In those patients who had immediate procedural complications, the mortality and morbidity of stent placement or surgery were modeled based on published rates in the literature. Those patients that did not die due to a procedure-related complication and had no procedural complications were then assessed for long-term major complications and mortality within a 1-month period. ES long-term complications included stent occlusion with recurrence of duodenal obstruction. Major complications for surgical bypass included in our model included abdominal abscess formation, efferent limb obstruction, deep vein thrombosis/pulmonary embolism, and marginal ulcers. The cost-effectiveness was also determined in each of the arms. An example of the decision tree model is shown in Fig. 1.
Cost-effectiveness
For the cost-effectiveness of OGJ, LGJ, and ES to be adequately determined, the average cost at the national level must be established. These estimates were obtained from the Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project (HCUPnet) national online database for 2002, the most recent year for which data are available [15]. This database provides an aggregate of national statistics on average hospital costs for certain medical conditions, ES and surgical complications, grouped according to the ICD-9-CM (The International Classification of Diseases, Ninth Revision, Clinical Modification) code.
Appraisal of clinical outcomes
The decision tree was used to evaluate the preferred treatment strategy, failure rates, complication rates, and costs for three treatment groups: the ES, OGJ, and LGJ groups. Short-term mortality and morbidity were assessed. Success was defined as no major procedure-related complication and no long-term complications over a 1-month period after the procedure. Failure of therapy was defined as either recurrent symptoms or death attributed to a procedural complication. We also performed cost-effectiveness analyses for the different treatment modalities.
Sensitivity analysis
The performance characteristics for ES, OGJ, and LGJ were varied to determine the threshold complication rates that would alter treatment strategies using one-way and multiple-way sensitivity analyses so as detect its effect on the ultimate results.
Since it is not realistic to rely on one value for probabilities, as there is marked variability in outcomes in the literature, sensitivity analysis must be performed in such a way that changing the morbidity and mortality rate alters the favored decision strategy. Such alteration tests the robustness of the model. If manipulation of the model does alter the strategy, the model is considered to be sensitive to changes in the probability of that particular test. In the final analysis, sensitivity analysis helps determine the most optimal treatment modality for patients with malignant gastroduodenal obstruction.
One-way sensitivity analyses were done by varying single-variable baseline probabilities over a credible range and then interpreting their effect on final outcomes. For each scenario, one-way sensitivity analysis was performed, plotting success of therapy against surgical complications, to determine the optimal strategy to follow (ES versus OGJ versus LGJ). Three-way sensitivity analysis of recurrent procedural complications in ES, OGJ, and LGJ was then performed to further validate the strength of the decision model.
Results
Decision analysis
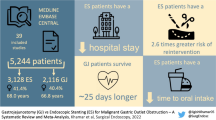
ES was the dominant and most cost-effective strategy in the treatment of a malignant duodenal obstruction. The ES strategy resulted in the highest rate of success (72%), i.e., least amount of major procedure-related and long-term complications, and the lowest mortality rate (2.1%). ES was also the most cost-effective of all strategies over a 1-month follow-up ($8213). This strategy therefore had the highest success rate, had the fewest negative outcomes for patients in terms of mortality, and was found to be the most cost-effective.
In comparison, the OGJ group had the lowest success rate (63%) and the highest mortality (4.5%) over a 1-month follow-up. Mortality in the OGJ group was 2.1 times that in the ES cohort and 1.8 times that in the LGJ cohort. OGJ was also found to be the most expensive treatment strategy, with an incremental cost of $12,191.
The LGJ strategy resulted in a success rate of 69%. The overall mortality was 2.5% and the incremental cost was $10,340. In comparison to the ES group, LGJ was less successful in relieving duodenal obstruction, with a higher overall mortality.
Overall, the OGJ and LGJ had similar clinical and economic outcomes. However, the ES maximized relief of duodenal obstruction and minimized the negative outcomes of overall mortality. The OGJ and LGJ strategies are inferior due to lower success rates, higher costs, and higher mortality. The success of each strategy is summarized in Fig. 2.
One-way sensitivity analysis was performed by altering the ES complication rates over a wide range to evaluate if this would alter our results. This revealed unchanged results when failure rates of the ES were less than 30%. When failure rates of ES were higher than 30%, LGJ became preferred over ES and OGJ for the treatment of malignant obstruction (Fig. 3). Sensitivity analysis revealed that final results remained consistent within a wide range of complications for ES, requiring the ES complications rate to be unrealistically high (over 30%) for the conclusions to be affected. The plot of this graft is procedural success, which, again, is a composite of both procedure-related and long-term (i.e., 1-month) complications. Thus, the one-way sensitivity analysis performed for the sensitivity of the three strategies showed unchanged results.
Results of one-way sensitivity analysis comparing ES to LGJ and OGJ. This graph illustrates that ES was the dominant strategy for the treatment of malignant gastroduodenal obstruction unless the immediate procedural complication rate exceeded 30%. Above this complication rate, LGJ became the therapy of choice
Similarly, a three-way sensitivity analysis was performed by altering the complication rates for ES, LGJ, and OGJ, which again showed ES to be the superior strategy for the palliation of malignant gastrodudoneal obstruction (Fig. 4).
The results of the decision analysis model are summarized in Table 2.
Discussion
This decision analysis demonstrates that placement of endoscopic stents achieves excellent palliation for gastroduodenal obstruction, with an overall 1-month success rate of 72%. This strategy was superior to both OGJ and LGJ.
Unfortunately, up to 80% of patients with upper GI cancers present with metastatic disease at the time of diagnosis [16]. In these cases, the management of cancers is related to amelioration of symptoms from tumor invasion to the biliary tree, duodenum, and splanchnic nerves [17]. Effective palliative includes relief of symptoms from pain and gastric outlet and bowel obstruction. For the subgroup of patients who present with gastric or duodenal outlet obstruction, their quality of life is severely impaired from nausea, vomiting, and inability to obtain adequate nutrition. Prior to laparoscopic and endoscopic techniques, OGJ was the palliative option for the management of duodenal outlet obstruction. However, OGJ carry considerable morbidity and mortality. The introduction of LGJ resulted in a decrease in complications and mortality compared to the OGJ. LGJ is also associated with a decrease in length of hospital stay [18–21]. The laparoscopic approach is, however, more technically demanding and requires expertise in laparoscopic suturing. It remains unclear which strategy would result in a better outcome and cost when comparing surgical approaches to endoscopic techniques.
We constructed a decision analysis model to mimic the clinical scenario of three therapeutic options for a patient presenting with malignant gastroduodenal obstruction. Patients were stratified into three treatment groups and the model was used to determine the optimal management strategy. Our results demonstrated that ES with SEMS was the preferred treatment for palliation of duodenal obstruction. Compared to surgical procedures, ES has a higher success rate, fewer complications, and a lower cost.
The efficacy and safety of ES with SEMS for palliation of malignant duodenal obstruction have been examined previously [22–26]. These studies showed that SEMS were associated with shorter hospitalization and lower costs compared to surgical approaches, had better patency, and had lower less morbidity and mortality than surgical gastrojejunostomy for palliation [19, 21, 27, 28]. SEMS resulted in a significant reduction in the time to starting oral intake and length of hospital stay after the procedure. Patients who underwent either OGJ or LGJ had significantly more postoperative complications (P=0.016) than did those who underwent stenting (Table 2).
Although endoscopic duodenal SEMS are increasingly used with high initial success in relieving obstruction and a lower morbidity and hospital stay compared to surgery [13, 28–30], large studies with long-term results are unavailable. One of the pitfalls of SEMS is tumor in growth and stent migration, which leads to recurrent duodenal obstruction in up to 25% of endoscopically palliated cases [31].
Because there are no RCTs comparing the modality of choice for palliation between surgical intervention and endoscopic management, we elected to use sensitivity analysis to determine the best strategy for palliation in this unfortunate group of patients. Our decision analysis showed that ES is a more cost-effective alternative than LGJ and OGJ for relief of malignant gastroduodenal obstruction over a 1-month period. ES was more cost-effective than surgical bypass and was associated with fewer complications. Although ES has a higher 1-month complication rate than surgical bypass, resulting from SEMS obstruction, this problem is typically managed by re-placement of an endostent. Replacement of stents does not add significant morbidity and mortality. Our analysis showed that even with the need to replace stents, the cost of ES is lower than that of surgical approaches. This finding is consistent with previous studies [32, 33]. However, it is important to note that in both studies cited, there were no differences in morbidity or mortality in patients who underwent ES versus surgical therapy.
Our decision modeling is subject to several limitations. The influences of factors such as patient preferences, which may impact the choice of clinical approach, are difficult to assess. The model has a level of uncertainty when examining the clinical assumptions. Like all decision models, the limitations may affect the validity and generalizability of our findings. Therefore, sensitivity analysis allows us to address this uncertainty by giving a range of values to inputs prone to uncertainty. We made a number of simplifying assumptions so as to create a working decision model that may not capture many of the subtleties that occur in clinical practice.
The results of this study allow us to establish the cost-effectiveness and overall success of ES compared to surgical modalities. Surgical bypass should be performed when there is no staff available with clinical expertise to place ES, when ES cannot be arranged, or when ES fails to relieve duodenal obstruction. Surgical bypass may also be an option for recurrent obstruction after ES. If there is significant obstruction of the second portion of the duodenum, then ES may possibly prevent future access to the common bile duct for palliation of obstructive jaundice. In this case, LGJ may be the best surgical option. If an attempt to place ES fails, LGJ should be the second modality of choice.
In conclusion, ES with SEMS is safe, is cost-effective, and results in more rapid recovery as well as less hospitalization compared to the surgical approaches for palliation of malignant gastroduodenal obstruction. ES should therefore be the first therapeutic approach for patients with gastroduodenal obstruction.
References
Lillemoe KD, Cameron JL, Hardacre JM, et al. (1999) Is prophylactic gastrojejunostomy indicated for unresectable periampullary cancer? A prospective randomized trial. Ann Surg 230:322–328
van Heek NT, van Geenen RC, Busch OR, et al. (2002) Palliative treatment in “peri”-pancreatic carcinoma: stenting or surgical therapy? Acta Gastroenterol Belg 65:171–175
Kulke MH (2002) Metastatic pancreatic cancer. Curr Treat Options Oncol 3:449–457
Khullar SK, DiSario JA (1996) Gastric outlet obstruction. Gastrointest Endosc Clin North Am 6:585–603
Adler DG, Baron TH (2002) Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol 97:72–78
Alam TA, Baines M, Parker MC (2003) The management of gastric outlet obstruction secondary to inoperable cancer. Surg Endosc 17:320–323
Bozzetti F, Bonfanti G, Audisio RA, et al. (1987) Prognosis of patients after palliative surgical procedures for carcinoma of the stomach. Surg Gynecol Obstet 164:151–154
Kazanjian KK, Reber HA, Hines OJ (2004) Laparoscopic gastrojejunostomy for gastric outlet obstruction in pancreatic cancer. Am Surg 70:910–913
Sarr MG, Cameron JL (1982) Surgical management of unresectable carcinoma of the pancreas. Surgery 91:123–133
Di Fronzo LA, Cymerman J, Egrari S, et al. (1999) Unresectable pancreatic carcinoma: correlating length of survival with choice of palliative bypass. Am Surg 65:955–958
Lawrence W Jr, McNeer G (1958) The effectiveness of surgery for palliation of incurable gastric cancer. Cancer 11:28–32
Choi YB (2002) Laparoscopic gatrojejunostomy for palliation of gastric outlet obstruction in unresectable gastric cancer. Surg Endosc 16:1620–1626
Wong YT, Brams DM, Munson L, et al. (2002) Gastric outlet obstruction secondary to pancreatic cancer: surgical vs endoscopic palliation. Surg Endosc 16:310–312
Yim HB, Jacobson BC, Saltzman JR, et al. (2001) Clinical outcome of the use of enteral stents for palliation of patients with malignant upper GI obstruction. Gastrointest Endosc 53:329–332
Steiner C, Elixhauser A, Schnaier J (2002) The healthcare cost and utilization project: an overview. Eff Clin Pract 5:143–151
Yeo TP, Hruban RH, Leach SD, et al. (2002) Pancreatic cancer. Curr Probl Cancer 26:176–275
Singh SM, Longmire WP Jr, Reber HA (1990) Surgical palliation for pancreatic cancer. The UCLA experience. Ann Surg 212:132–139
Bergamaschi R, Marvik R, Thoresen JE, et al. (1998) Open versus laparoscopic gastrojejunostomy for palliation in advanced pancreatic cancer. Surg Laparosc Endosc 8:92–96
Mittal A, Windsor J, Woodfield J, et al. (2004) Matched study of three methods for palliation of malignant pyloroduodenal obstruction. Br J Surg 91:205–209
Ghanem AM, Hamade AM, Sheen AJ, et al. (2006) Laparoscopic gastric and biliary bypass: a single-center cohort prospective study. J Laparoendosc Adv Surg Tech A 16:21–26
Mehta S, Hindmarsh A, Cheong E, et al. (2006) Prospective randomized trial of laparoscopic gastrojejunostomy versus duodenal stenting for malignant gastric outflow obstruction. Surg Endosc 20:239–242
Topazian M, Ring E, Grendell J (1992) Palliation of obstructing gastric cancer with steel mesh, self-expanding endoprostheses. Gastrointest Endosc 38:58–60
Feretis C, Benakis P, Dimopoulos C, et al. (1996) Palliation of malignant gastric outlet obstruction with self-expanding metal stents. Endoscopy 28:225–228
Holt AP, Patel M, Ahmed MM (2004) Palliation of patients with malignant gastroduodenal obstruction with self-expanding metallic stents: the treatment of choice? Gastrointest Endosc 60:1010–1017
Lindsay JO, Andreyev HJ, Vlavianos P, et al. (2004) Self-expanding metal stents for the palliation of malignant gastroduodenal obstruction in patients unsuitable for surgical bypass. Aliment Pharmacol Ther 19:901–905
Johnsson E, Thune A, Liedman B (2004) Palliation of malignant gastroduodenal obstruction with open surgical bypass or endoscopic stenting: clinical outcome and health economic evaluation. World J Surg 28:812–817
Del PM, Ballare M, Montino F, et al. (2005) Endoscopy or surgery for malignant GI outlet obstruction? Gastrointest Endosc 61:421–426
Maosheng D, Ohtsuka T, Ohuchida J, et al. (2001) Surgical bypass versus metallic stent for unresectable pancreatic cancer. J Hepatobil Pancreat Surg 8:367–373
Bethge N, Breitkreutz C, Vakil N (1998) Metal stents for the palliation of inoperable upper gastrointestinal stenoses. Am J Gastroenterol 93:643–645
Espinel J, Sanz O, Vivas S, et al. (2006) Malignant gastrointestinal obstruction: endoscopic stenting versus surgical palliation. Surg Endosc 20(7):1083–1087
Ely CA, Arregui ME (2003) The use of enteral stents in colonic and gastric outlet obstruction. Surg Endosc 17:89–94
Brandabur JJ, Kozarek RA, Ball TJ, et al. (1988) Nonoperative versus operative treatment of obstructive jaundice in pancreatic cancer: cost and survival analysis. Am J Gastroenterol 83:1132–1139
Raikar GV, Melin MM, Ress A, et al. (1996) Cost-effective analysis of surgical palliation versus endoscopic stenting in the management of unresectable pancreatic cancer. Ann Surg Oncol 3:470–475
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper was completed without any support or sponsorship.
Rights and permissions
About this article
Cite this article
Siddiqui, A., Spechler, S.J. & Huerta, S. Surgical Bypass Versus Endoscopic Stenting for Malignant Gastroduodenal Obstruction: A Decision Analysis. Dig Dis Sci 52, 276–281 (2007). https://doi.org/10.1007/s10620-006-9536-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-006-9536-z