Abstract
Ghrelin and leptin are the hormones that influence endocrine and exocrine functions of the pancreas and regulate feeding behaviors and energy metabolism. The aim of this study was to investigate the levels of ghrelin and leptin in pancreatitis of different severities and the relation of these hormones with blood glucose level and proinflammatory cytokines. The study was performed on 90 Wistar Albino rats. Three experimental groups composed of 30 rats were established: control group, 0.9% NaCl solution was injected intraperitoneally (i.p); acute edematous pancreatitis (AEP) group, 1 μg/100 g cerulein was injected i.p. five times, at 1-hr intervals; and acute necrotizing pancreatitis (ANP) group, 500 mg/100 g l-arginine was injected i.p. Ten animals in each group were sacrificed under anesthesia 12, 24 and 48 hr after the last injection. After blood withdrawal, the pancreas was totally excised. The levels of blood sugar, lipase, serum tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), ghrelin, and leptin were investigated and histopathologic examination was performed. Following pancreatitis induction, serum ghrelin levels increased at 24 hr and reached the peak level at 48 hr. Its level in the AEP group was higher than in the ANP group. Serum leptin levels in the AEP and ANP groups increased after 12 hr and stayed at high levels until 48 hr compared with the control group. Similarly to ghrelin and leptin, blood glucose levels increased in both pancreatitis groups, but the increase was more prominent in the ANP group, with levels >200 mg/ml at 48 hr. The levels of TNF-α and IL-1β in the AEP and ANP groups reached the peak level at 24 hr and then decreased to a level close to that of the control group at 48 hr. We conclude that serum leptin and ghrelin levels increase in the first 48 hr of AEP and ANP. As the serum ghrelin levels in ANP are higher than in AEP, it can be used as a marker to show the severity of pancreatitis. While TNF-α and IL-1β can be used as a prognostic factor in the first 24 hr, ghrelin and leptin can be used subsequently.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute pancreatitis (AP) is a severe disease with significant morbidity and mortality for which there is no specific treatment beyond supportive therapy. An amplified cytokine response plays an important pathophysiological role in the development of complications, especially in the progression of limited local pancreatic inflammation into a potentially dangerous systemic inflammatory reaction termed multiple organ dysfunction syndrome [1]. The spectrum of AP ranges from mild inflammation to severe necrotizing inflammation with systemic manifestations. Several scoring systems have been presented to determine the severity of pancreatic injury [2, 3]. The early detection of potentially severe AP is imperative because accurate and timely selection of those patients who will require intensive care may improve mortality. For this reason, cytokines, immune response markers, proenzymes, and enzyme complexes have been the subject of several studies for determining the severity of disease [4]. In this study, we aimed to find out the relation between the levels of ghrelin and leptin in edematous, necrotizing pancreatitis and the prognostic factors.
Ghrelin is a 28-amino acid polypeptide originally isolated from rat stomach [5] and it has been localized in endocrine X/A-like cells in the gastric mucosa [6] and ɛ-islet cells in the pancreas [7–9]. Ghrelin is considered to bind to the growth hormone secretagogue receptor (GHS-R) and then affects GH release, gastrointestinal function, feeding behavior, and energy metabolism [10–14]. In fetal pancreas, ghrelin is expressed in a prominent endocrine cell population [7, 9]. In adult pancreas, the number of ghrelin-immunreactive cells is reduced and these cells are localized at the periphery of human and rat pancreatic islets. Pancreatic exocrine secretion has been found to be inhibited by ghrelin in rat acinar cells [15]. Recent studies have indicated that ghrelin may have a direct action on ß cell function. However, both inhibitory [16, 17] and stimulatory [8, 18, 19] actions have been reported in vitro.
Leptin, which is a 16-kDa protein encoded by the obese gene, is an adipocyte-derived hormone that acts centrally in the hypothalamus to regulate body weight and peripheral energy expenditure [20]. The presence of leptin and expression of its receptors have been detected in other tissues like the stomach [21], liver [22], and pancreas [23]. Leptin receptors have been detected on pancreatic AR42J cells and their gene expression has been documented in pancretic acini, suggesting that this protein could take part in the regulation of pancreatic exocrine secretion [24]. On the other hand, the presence of leptin receptors on pancreatic ß cells suggests that leptin could be involved in the regulation of pancreatic endocrine function as well [25, 26].
Considering the information mentioned above, it is accepted that both ghrelin and leptin can influence endocrine and exocrine functions of the panceas. In AP, in which endocrine and exocrine functions of the pancreas are disturbed, the levels of these hormones can change and these changes can be used as a prognostic factor. The aim of this study was to investigate (a) the changes of these two hormones in the first 48 hr of pancreatitis in different severities, (b) the relationship between the changes of these hormones and blood glucose levels, and (c) the relation of proinflammatory cytokines (tumor necrosis factor [TNF]-α and interleukin [IL]-1β) with hormone levels.
Materials and methods
Animals and experimental design
The study was performed on male Wistar Albino rats weighting 240–280 g and was conducted following the experimental protocol approved by the Committee for Research and Animal Ethics of Gazi University. Animals were housed in cages at a normal room temperature under a 12-hr light-dark cycle. Food and water were available ad libitum. All rats were allowed at least 1 week of adaptation to the laboratory before the experimental procedure was begun. Rats were fasted for 16 hr before injections, while access to water was maintained until euthanasia. Rats were anesthetized with an intramuscular injection of 40 mg/kg ketamine (Ketalar; Parke Davis, Eczacıbasi, Istanbul, Turkey) and xylazine (Rompum; Bayer AG, Leverkusen, Germany).
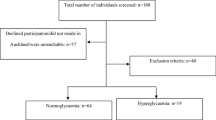
Three experimental groups were established: in the control group (n=30), animals were injected with a 0.9% NaCl solution intraperitoneally (i.p); in the acute edematous pancreatitis (AEP) group (n=30), AEP was induced by five intraperitoneal injections of cerulein at a dose of 1 μg/100 g/injection, at 1-hr intervals (Sigma-Aldrich Chemical, Steinheim, Germany); and in the acute necrotizing pancreatitis (ANP) group (n=30), ANP was induced by one i.p. injection of 500 mg/100 g l-arginine (Merck, Darmstat, Germany). Four milliliters of serum physiologic was injected subcutaneously in the flank region of all rats after the last i.p injection. All rats were permitted to take water and food after the experiment. Food intake was ceased 2 hr before sacrifice. Ten animals in each group were sacrificed under anesthesia 12, 24, and 48 hr after the last injection. A midline incision was made and blood samples were taken at the abdominal aorta. After blood withdrawal, the pancreas was carefully dissected out from its attachment to the stomach and was totally excised. All rats were killed by hemorrhage. Blood samples were kept at −80°C for biochemical analyses, which were run in duplicate.
Blood sugar and lipase assay
Serum blood sugar and lipase were determined using a Beckman Coulter LX-20 System analyzer (Beckman, Fullerton, CA, USA) and Beckman kits, according to the supplier’s specification.
Serum tumor necrosis factor-α and interleukin-1β assay
To determine the levels of TNF-α and IL-1β, a commercial solid phase sandwich enzyme-linked immunosorbent assay (ELISA) from Biosource International (Camarillo, CA, USA) was used. TNF-α and IL-1-β levels were determined from a standard curve for recombinant TNF-α and IL-1β, and concentrations are expressed as picograms per milliliter. The ELISA detection limit for TNF-α and IL-1β was 3 pg/ml.
Serum ghrelin and leptin assay
Ghrelin concentration in the serum was determined using a commercially available ELISA kit from Phoenix Pharmaceuticals (Belmont, CA, USA). Serum leptin concentrations were determined using a commercially available kit from Linco Research (USA). Serum ghrelin and leptin concentrations are expressed as nanograms per milliliter.
Histological examination
Samples of pancreatic tissue excised from the body portion for morphological examination were fixed in 10% formalin, then embedded in paraffin, and sections were stained with hemotoxylin and eosin. The slides were examined by two experienced pathologists without knowledge of the chemicals given. Histological grading of edema was done using a scale raging from 0 to 3 (0 = no edema, 1 = interlobular edema, 2= interlobular and moderate intralobular edema, 3 = interlobular edema and severe intralobular edema). Leukocytic infiltration was also graded from 0 to 3 (0 = absent, 1 = scarce perivascular infiltration, 2 = moderate perivascular and scarce diffuse infiltration, 3 = abundant diffuse infiltration). Grading of vacuolization was based on the appropriate percentage of acinar cells involved: 0 = absent, 1 = less than 25%, 2 = 25–50%, and 3 = more than 50% of acinar cells [27].
Statistical analysis
Results are expressed as the mean ±SE. Comparisons within groups were made using the Mann-Whitney U test. One-way ANOVA and Scheffe’s post hoc test were carried out for multiple comparisons. P< 0.05 was considered statistically significant. Statistics were analyzed using the SPSS program, version 11.5.
Results
During the experiment two rats in the ANP group died. New rats replaced these two.
Histopathologic examination
Edema, inflammation, vacuolization, and necrosis in the ANP group at 12, 24, and 48 hr were significantly higher than in the control group (P< 0.001). Also, edema at 12 and 24 hr (P=0.01) and necrosis at 48 hr (P< 0.05) were higher in the ANP group compared to the AEP group. All parameters except necrosis in the AEP group were higher than in the control group. Edema, vacuolization, and necrosis at 48 hr were more significant than at 12 hr in the AEP group (P< 0.05). In the ANP group, all histologic parameters except necrosis were higher at 48 hr than at 12 hr (P< 0.05).
Serum lipase levels
Serum lipase levels at 12, 24, and 48 hr in both the AEP and the ANP groups were significantly higher than in the control group (P< 0.001). Lipase at 24 and 48 hr in the ANP group was higher than in the AEP group (P=0.006 and P< 0.001, respectively) (Table 1).
Blood sugar levels
Serum glucose levels at 12, 24, and 48 hr in the ANP group were higher than in the control group (P< 0.001). The blood glucose level in the ANP group at 48 hr was >200 ml/dl. Although the blood glucose level in the AEP group was higher than in the control group, the difference was not statistically significant (P > 0.05). Blood glucose levels of the ANP and AEP groups showed no significant difference (P > 0.05; Table 1).
Serum ghrelin levels at 24 and 48 hr in both the AEP and the ANP groups were significantly higher than in the control group. At 48 hr the serum ghrelin level in the ANP group was significantly higher than in the AEP group. a P=0.003 vs. the control group; b P=0.023 vs. the control group; c P<0.001 vs. the control group; d P=0.07 vs. the AEP group; e P=0.001 vs. 12 hr in the ANP group; f P=0.001 vs. 24 hr in the ANP group; g P=0.014 vs. the control group; i P< 0.001 vs. 12 hr in the AEP group
Serum TNF-α levels
Serum TNF-α levels measured in both the AEP and the ANP groups at 12 and 24 hr were significantly higher than in the control group (P=0.001 and P< 0.001, respectively). Serum TNF-α levels at 12 and 24 hr in the ANP group were significantly higher than in the AEP group (P=0.013 and P=0.001). On the other hand TNF-(levels at 48 hr in the AEP and ANP groups were decreased close to those in the control group (Table 1).
Serum IL-1β levels
Serum IL-1β level in the ANP group at 12 and 24 hr was significantly higher than in the controls (P=0.001 and P< 0.001, respectively) and the AEP group (P=0.038 and P=0.049, respectively). Also, IL-1β levels at 12 and 24 hr in the AEP group were higher than in the control group (P=0.028 and P=0.04, respectively). Serum IL-1β levels in the ANP and the AEP groups reached the peak level at 24 hr but decreased to the control-group level at 48 hr (Table 1).
Serum ghrelin levels
There was no significant difference among the three groups in serum ghrelin levels at 12 hr (P > 0.05). Although serum ghrelin levels in the ANP and the AEP groups at 24 hr were significantly higher than in the control group (P = 0.003), no differences were seen between them (P > 0.05). Serum ghrelin levels in the ANP group at 24 and 48 hr were higher than the level at 12 hr (P< 0.05 and P< 0.001, respectively). Serum ghrelin level at 48 hr in the ANP group was higher than in the control and the AEP group. Considering that the histopathologic findings of pancreatitis last longer than 48 hr, serum ghrelin levels increased more and continued to increase significantly after 24 hr (Fig. 1).
Serum leptin levels
Serum leptin levels at 24 and 48 hr in both the AEP (P=0.027 and P< 0.001, respectively) and the ANP (P=0.027 and P< 0.001, respectively) groups were significantly higher than in the control group. At 12 hr, serum leptin levels in the ANP group were significantly higher than in the control group (P< 0.001). There was no significant difference in serum leptin levels at 48 hr in either the AEP or the ANP group. In the AEP group the serum leptin level at 48 hr was higher than the level at 12 hr, but in the ANP group there was no difference between the 48- and the 12-hr level (P > 0.05). Serum leptin levels showed an increasing line after 12 hr compared to the control group (Fig. 2).
Serum leptin levels at 24 and 48 hr in both the AEP and the ANP groups were significantly higher than in the control group. At 12 hr the serum leptin level in the ANP group was significantly higher than in the control group. a P< 0.001 vs. the control group; b P=0.027 vs. the AEP group; c P=0.022 vs. the control group; d P<0.001 vs. the control group; e P< 0.05 vs. 12 and 24 hr in the AEP group
Discussion
In this study, we investigated the serum levels of ghrelin and leptin in experimental models of AP of differing severities. This is an original study, being the first to determine the serum ghrelin levels in AP. Serum ghrelin levels started to increase 24 hr after i.p administration of l-arginine and cerulein and reached the peak level at 48 hr. Serum ghrelin levels in the ANP group were higher than those in the AEP group. Similarly, serum leptin levels in both pancreatitis groups started to increase after 12 hr and stayed at a higher level compared to the control group. Parallel to the increase in serum ghrelin and leptin levels at 48 hr, blood glucose levels in both pancreatitis groups increased in the same period; but the blood glucose level increased to >200 mg/ml in the ANP group, which is a worse prognostic factor [3]. In recent studies, several cytokines such TNF-α, which was investigated as a prognostic factor [4], and IL-1β, which has an important role in the pathophysiology of AP [1, 4], has been studied several times before. In our study, it was seen that following i.p administration of cerulein and l-arginine, IL-1β and TNF-α levels reached peak levels at 24 hr and decreased to the control-group level at 24 hr.
The biological effects of leptin are exerted via specific leptin receptors which have been detected in gastric mucosa, small intestine, and liver, as well as in pancreatic β cells and pancreatic acini and afferent nerves [21–23]. A recent study showed that leptin receptors have been detected on pancreatic AR42J cells and their gene expression has been documented in pancreatic acini, suggesting that this protein could take part in the regulation of pancreatic exocrine secretion [24]. Based on the information that leptin has a regulatory effect on endocrine and exocrine functions of the pancreas, levels of leptin in AP have been the subject of several studies. Yavuz et al. [27] showed that 24 hr and 7 days after the induction of edematous pancreatitis with i.p cerulein, serum leptin levels were higher than in the control group, but there was no difference between the levels on day 1 and day 7. Similarly Konturek et al. [28] showed high serum leptin levels in patients with AP compared with the control group. In our study serum leptin levels increased after 12 hr in the ANP group and after 24 hr in the AEP group and reached the peak level at 48 hr in both groups compared with the control group.
AP is associated with induction of a systemic inflammatory response, which is responsible for its morbidity and mortality [1–3]. With increasing neutrophil migration to the pancreas, a variety of inflammatory cytokines is realized, including IL-1, IL-6, IL-8, platelet activating factors, and TNF-α.There is considerable evidence that pro-inflammatory cytokines (TNF-α and IL-1β) play a central role in AP and may mediate the systemic complications of AP [1, 2]. Pro-inflammatory cytokine production correlates with disease severity [1, 2]. Konturek et al. [28] showed that leptin given in the experimental model of AP has a modulating effect on inflammation by increasing the levels of TNF-α and the anti-inflammatory cytokine IL-4. And also, Warzecha et al. [29] showed a decline in IL-1β level following the administration of leptin in experimental ischemic AP. Dembinski et al. [30] demonstrated that pancreatic treatment with ghrelin diminished pro-inflammatory IL-1β release. Leptin and ghrelin generated in the pancreas during AP could act by reducing the increments of proinflammatory cytokines, such as TNF-α and IL-1β. In our study TNF-α and IL-1β levels increased 24 hr after the induction of pancreatitis in both pancreatitis groups, especially in the ANP group, and decreased to the level of the control group at 48 hr. As the serum leptin and ghrelin levels at 24 and 48 hr were significantly higher than in the control group, they are probably responsible for the decrease in pro-inflammatory cytokine levels. Especially, this effect may be more prominent in the AEP group because of the higher ghrelin levels compared with the ANP group.
As a result, serum leptin and ghrelin levels are increasing at 48 hr of experimental AP. Serum ghrelin levels can be used in follow-up of the severity of pancreatitis. Endogenous leptin and ghrelin may be responsible for the hyperglycemia and the moderation of pro-inflammatory cytokines in AP. While TNF-α and IL-1β are valuable as prognostic factors in the first 24 hr, the levels of ghrelin and leptin can be used for this purpose in later periods. The long-term effects of these two polypeptides on AP can be determined by more studies.
References
Weber CK, Adler G (2003) Acute pancreatitis. Curr Opin Gastroenterol 19:447–450
Imrie CW, Whyte AS (1975) A prospective study of acute pancreatitis. Br J Surg 62:490–494
Ranson JHC (1982) Etiological and prognosis in human acute pancreatitis: a review. Am J Gastroenterol 77:633–638
Triester SL, Kowdley KV (2002) Prognostic factors in acute pancreatitis. J Clin Gastroenterol 34:167–176
Kojima M, Hosoda H, Date Y, et al. (1999) Ghrelin is a growth-hormone releasing acylated peptide from stomach. Nature 402:656–660
Ariyasu H, Takaya K, Tagami T, et al. (2001) Stomach is major source of circulating ghrelin, and feeding state determines plasma ghrelin-like immunoreactivity levels in humans. J Clin Endocrinol Metab 86:4753–4758
Prado CL, Pugh-Bernard AE, Elghazi L, et al. (2004) Ghrelin cells replace insulin-producing beta cells in two mouse models of pancreas development. Proc Natl Acad Sci USA 101:2924–2929
Wierup N, Yang S, McEvilly RJ, et al. (2004) Ghrelin is expressed in a novel endocrine cell type in developing rat islets and inhibits insulin secretion from INS-1 (832/13) cells. J Histochem Cytochem 52:301–310
Wierup N, Sundler F (2005) Ultrastructure of islet ghrelin cells in the human fetus. Cell Tissue Res 319:423–428
Dornonville de la Cour C, Bjorkqvist M, et al. (2001) A-like cells in the rat stomach contains ghrelin and do not operate under gastrin control. Regul Pept 99:141–150
Toshinai K, Mondal MS, Nakazato M, Date Y, et al. (2001) Upregulation of ghrelin expression in the stomach upon fasting, insulin–induced hypoglycemia, and leptin administration. Biochem Biophys Res Commun 281:1220–1225
Lee HM, Wang G, Englander EW, et al. (2002) Ghrelin, a new gastrointestinal endocrine peptide that stimulates insulin secretion:enteric distribution, ontogeny, influence of endocrine and dietary manipulations. Endocrinology 143:185–190
Shiiya T, Nakazato M, Mizuta M, et al. (2002) Plasma ghrelin levels in lean and obese humans and the effect of glucose on ghrelin secretion. J Clin Endocrinol Metab 87:240–244
Wierup N, Swensson H, Mulder H, Sundler F (2002) The ghrelin cell:a novel developmentally regulated islet cell in the human pancreas. Regul Pept 107:63–69
Zhang W, Chen M, Chen X, et al. (2001) Inhibition of pancreatic protein secretion by ghrelin in the rat. J Physiol 537:231–236
Dezaki K, Hosoda H, Kakei M, et al. (2004) Endogenous ghrelin in pancreatic islets restricts insulin release by attenuating Ca2+ signaling in beta-cells: implication in the glycemic control in rodents. Diabetes 53:3142–3151
Date Y, Nakazato M, Hashiguchi S, et al. (2002) Ghrelin is present in pancreatic alpha-cells of humans and rats and stimulates insulin secretion. Diabetes 51:124–129
Adeghate E, Ponery AS (2002) Ghrelin stimulates insulin secretion from the pancreas of normal and diabetic rats. J Neuroendocrinol 14:555–560
Date Y, Nakazato M, Hashiguchi S, et al. (2002) Ghrelin is present in pancreatic alpha cells of humans and rats and stimulates insulin secretion. Diabetes 51:124–129
Zhang Y, Proenca R, Maffei M, et al. (1994) Positional cloning of the mouse obese gene and its human homologue. Nature 372:425–432
Bado A, Levasseur S, Attoub S, et al. (1998) The stomach is a source of leptin. Nature 394:790–793
Lin J, Barb CR, Matteri RL, et al. (2000) Long form leptin receptor mRNA expression in the brain, pituitary, and other tissues in the pig. Domest Anim Endocrinol 19:53–61
Konturek PC, Konturek SJ, Brzozowski T, et al. (2001) Role of leptin in the stomach and the pancreas. J Physiol Paris 95:345–354
Harris DM, Flaningan CL, Go FL, Wu SV (1999) Regulation of cholecystokinin-mediated amylase secretion by leptin in rat pancreatic acinar tumor cell line AR42J. Pancreas 19:224–230
Kiefer TJ, Heller RS, Habener JF (1996) Leptin receptors expressed on pancreatic beta-cells. Biochem Biophys Res Commun 224:522–527
Ahren BO, Havel PJ (1999) Leptin inhibits insulin secretion induced by cellular cAMP in a pancreatic B cell line (INS-1 cells). Am J Physiol 277:959–966
Yavuz N, Unal E, Memisoglu K, et al. (2004) Plasma leptin levels in rats with pancreatitis. Tohoku J Exp Med 204:243–248
Konturek PC, Jaworek J, Maniatoglou A, et al. (2002) Leptin modulates the inflammatory response in acute pancreatitis. Digestion 65:149–160
Warzecha Z, Dembinski A, Ceranowicz P, et al. (2002) Influence of leptin administration on the course of acute ischemic pancreatitis. J Physiol Pharmacol 53:775–790
Dembinski A, Warzecha Z, Ceranowicz P, et al. (2003) Ghrelin attenuates the development of acute pancreatitis in rat. J Physiol Pharmacol 54:561–573
Acknowledgments
The authors thank The Scientific and Technical Research Council of Turkey (TUBITAK; project no. 105S010- SBAG-HD-14) for supporting this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kerem, M., Bedirli, A., Pasaoglu, H. et al. Role of Ghrelin and Leptin in Predicting the Severity of Acute Pancreatitis. Dig Dis Sci 52, 950–955 (2007). https://doi.org/10.1007/s10620-006-9150-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-006-9150-0