Abstract
Glucagon-like peptide-2 (GLP-2) is an enteroendocrine hormone which is uniquely trophic for the intestine; a physiological role in regulating nutrient absorptive capacity is becoming apparent. GLP-2, independent of enteral feeding, stimulates a classical pattern of intestinal adaptation in terminal ileum following resection. Herein we investigate the effects of GLP-2 on the jejunal remant using a rat model of short bowel syndrome (SBS). Juvenile 250- to 275-g SD rats underwent 80% distal small bowel resection, leaving 20 cm of proximal jejunum and venous catheterization. Animals were maintained with total parenteral nutrition (TPN) or TPN+10 μg/kg/hr GLP-2 (n=8 per group). After 7 days, intestinal permeability was assessed by urinary recovery of gavaged carbohydrate probes. Animals were euthanized, and the intestines taken for analysis of morphology, crypt cell proliferation, apoptosis, and expression of SGLT-1 and GLUT-5 transport proteins. GLP-2 treatment reduced intestinal permeability and increased in vivo glucose absorption, small intestinal weight, surface area, villus height, crypt depth, and microvillus height. Intestinal mucosal DNA and protein content per unit length of the small bowel were increased (P < 0.05 for all comparisons). However, in contrast to previous studies examining GLP-2’s effects on remnant ileum, the jejunal crypt apoptotic index was increased in GLP-2-treated animals, with no increase in SGLT-1 or GLUT 5 expression. These results show that exogenous GLP-2 treatment of animals with jejunal remnant reduces intestinal permeability, increases glucose absorption, and stimulates morphological features of intestinal adaptation including increased micovillus height and surface area. However, the pattern of changes seen is different from that in remnant ileum. This suggests that GLP-2’s effects are specific to different regions of the bowel. Nonetheless, remnant jejunum is responsive to GLP-2 in the absence of enteral nutrition. Further studies are warranted to establish the mechanisms of action and therapeutic potential of GLP-2 in modulating nutrient absorptive capacity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The intestine possesses a remarkable ability to increase its functional capacity in response to changes in nutrient availability or to intrinisic variations in function of the intestine itself such as occurs with disease or following resection. This phenomenon is known as intestinal adaptation [1–3]. Following surgical resection, if the residual bowel is not able to compensate, malabsorption ensues, resulting in so-called short bowel syndrome (SBS). An appreciation of the role of glucagon-like peptide 2 (GLP-2) as part of the physiological regulation of nutrient absorptive capacity is emerging. GLP-2 is a 33-amino acid member of the PACAP (pituitary adenylate cyclase activating peptide) glucagon superfamily [4], which has been shown to be trophic to the entire gastrointestinal (GI) tract [5, 6]. GLP-2 is produced in the distal ileum and proximal colon by intestinal L-cells [7–9]. In response to ingestion of nutrients, L-cells release GLP-1, PYY, and GLP-2; these “hindgut” hormones appear to signal nutrient availability or excess to the animal and initiate a coordinated metabolic and functional response [10, 11]. The release of these hormones from the L-cell is signaled via both vagally mediated pathways (in turn stimulated by nutrients in the proximal gut) and direct stimulation (nutrients in distal bowel); long-chain fatty acids appear to be the most potent stimuli [8, 10, 12, 13]. GLP-2 has been shown to affect gastric and small intestinal motility, epithelial permeability, crypt cell proliferation, and nutrient absorption [8, 14, 15]. At the cellular level GLP-2 activates a specific G-protein-coupled receptor [16], which has been localized to the enteric neuronal system [16–18]. The precise pathways involved are unclear; there are conflicting data suggesting that GLP-2 may act on intestinal epithelial cells directly or via intermediate enteroendocrine cell activation [19–22]. It is clear that administration of exogenous GLP-2 to intact animals results in hypertrophy throughout the GI tract, with increases in villus height, crypt depth, protein content, and bowel weight [5, 6, 10]. GLP-2 has also been shown to increase the activity of specific sugar transport proteins (SGLT-1 and glut-2), intestinal blood flow, and glucose uptake [23, 24].
We have recently shown that following proximal intestinal resection the remnant ileum produces increased levels of GLP-2 and that postprandial GLP-2 levels are inversely correlated with the nutrient absorptive capacity of the residual bowel [13]. We have also demonstrated that GLP-2 alone, independent of enteral feeds, will stimulate the classical features of adaptation with remnant ileum [25]. However, the specific features of GLP-2 stimulation of remnant jejunum after massive intestinal resection have not been studied. This is particularly important given the frequency and severity of this situation clinically [2]. Extensive experience suggests that following massive resection remnant ileum is much more able to adapt and up-regulate nutrient absorptive capacity than jejunum [2, 26]. It is unclear whether these differences are due to a differential regional sensitivity to signals stimulating adaptation or alterations in the physiologic signals themselves with different remnant sections of intestine. After distal ileal resection, it is likely that the production of GLP-2, even with significant nutrient malabsorption, will be reduced [27]. This may be particularly important in human infants; we have shown that this population does not appear to be able to produce GLP-2 by colonic stimulation [28]. This may be species or age specific; in rodent studies with juvenile adult animals we have shown that remnant jejunum and colon produce elevated levels of GLP-2 after resection, as do adult human patients with similar anatomy [27, 29].
The present study was undertaken to determine if exogenous GLP-2 alone will induce adaptation in remnant jejunum following massive intestinal resection. We defined adaptation primarily as an increase in intestinal villus height and crypt depth, resulting in an increase in intestinal mucosal surface area and nutrient absorptive capacity. We also examined gross intestinal morphology (wet weight, protein, and DNA content), cellular kinetics (crypt cell proliferation [CCP], crypt cell apoptosis), and transporter expression (SGLT-1, Glut-5). We show that remnant jejunum does show adaptation in response to exogenous GLP-2 without enteral feeding, but the pattern of response is distinct from that seen in remnant ileum under similar experimental conditions.
Materials and methods
Animal care and maintenance
These studies were conducted following the guidelines of the Canadian Council for Animal Care, with approval of the Animal Care Committee at the University of Calgary. Juvenile male Sprague Dawley (SD) rats (Charles River, Montreal, PQ, Canada) weighing 260–280 g were housed in metabolic caging and acclimatized for 7 days prior to experiments. Animals were maintained under controlled standard lab parameters of controlled temperature and humidity and 12-hr light/dark cycles. Animals were maintained on a liquid diet (Ensure Plus; Abbott Laboratories, Saint-Laurent, PQ, Canada), 50 ml daily, for 2 days prior to surgery.
Using our previously described methods [25, 29], animals underwent an 80% distal small intestinal resection, leaving 20 cm of proximal jejunum anastomosed to the ascending colon. All procedures were done following an overnight fast using halothane anesthetic and aseptic technique. Animals received preoperative and postoperative cefazolin throughout the study (50 mg/kg/day; Novapharm, Toronto, ON, Canada). Procedures were done with the aid of an operating microscope (NM 114; J. K. Hoppl, New York, USA). Bowel anastomosis was completed with interrupted sutures of 6-0 silk (Davis-Geck, Peterborough, ON, Canada) and the abdomen was closed with a 4-0 absorbable suture. We have found that the surgical stress and weight loss of doing a resection and catheter insertion in 1 day are excessive. Thus animals were allowed to recover for 24 hr, then reanesthetized, and a Silastic catheter, 1.6 mm in outer diameter (Bentec Medical Inc., Woodland, CA, USA), was inserted into the right jugular vein, tunneled out of the back, and attached to a standard free swivel device (Harvard Labs, Boston, MA, USA).
Total parenteral nutrition (TPN) was delivered by a multichannel syringe pump (Pump 22 infusion pump; Harvard Apparatus Canada). Animals were randomly assigned to the TPN only or the TPN+GLP2 group (n=8 each). In order to prevent hyperglycemia, the concentration of glucose was increased over 3 days. For the first day all animals were maintained with 60 ml/day low-concentration TPN (4% amino acids, 10% dextrose and electrolyte) solution. On the second day all animals were maintained with 60 ml/day of half-strength TPN. Then from the third day to the end of the experiment (day 8) all animals received 60 ml/day TPN (50 ml Travasol, 5% amino acids with 25% dextrose and added 57 mM NaCl, 20 mM KCl, 7.2 mM CACl2, 3.2 mM MgSO4, 15 mM KPO4; Baxter Labs, Toronto, ON) and multivitamins 1000 (5 ml/L; Sabex Inc., Toronto, ON) mixed with 10 ml 20% Intralipid (Kabi Pharmacia, Montreal, PQ, Canada). Thus the total daily intake was 300 cal/kg body weight. GLP-2 animals received human GLP-21–33 (recombinant; NPS Pharmaceuticals, Toronto, ON, Canada) mixed with their daily volume of TPN, at a total dose of 10 μg/kg/hr. GLP-2 dosage was based on our previous studies, aiming for a target level of 6 ng/ml, or approximately twice the normal postprandial peak with massive proximal resection and remnant ileum [25, 29]. All animals were reviewed daily for well-being, ensuring normal grooming and activity. The animals were reweighed on day 7 and the final day of the experimental period, day 8.
Intestinal glucose absorption/permeability
Intestinal absorption of 3-O-methylglucose (3-O-MG), mannitol (Man), and lactulose (Lac) was used as a marker of intestinal transport capacity and permeability. 3-O-MG is actively transported by the SGLT-1 contransporter, while Man and Lac are absorbed passively through transcellular pathways (Man) and intracellular gaps in the tight junctions (Lac) [30, 31]. Rats were preconditioned to handling by daily sham gavage during the acclimatization period. On day 7, the animals were gavaged with a 2-ml solution containing 60 mg 3-O-MG, 40 mg Man, and 60 mg Lac (352 mOsm/L). Urine was collected over the next 20 hr, the volume was recorded, and samples were frozen for analysis. We have previously shown that sugars in the urine in this system are stable during the collection period (<3% loss [31]). The samples were batch analyzed for the presence of the carbohydrate probes by high-performance liquid chromatography (HPLC). In brief, the urine was filtered through a 0.4-μm filter, diluted, deionized, and then injected onto a Dionex MA-1 ion exchange column (Dionex Corp., Sunnyvale, CA, USA). The sugars were eluted with NaOH at a flow rate of 0.4 ml/min at concentrations ranging from 400 to 600 μm/L, and the peaks detected using pulse and amperometric detection on a Dionex HPLC and quantitated as peak areas. Calibration was performed daily with authenticated samples. The data are reported as absorbance, reflecting the percentage of the gavaged amount recovered in the urine.
Intestinal morphology and histology
On the morning of day 8, animals were injected with 50 mg/kg 5-bromo-2′-deoxyuridine (BrdU; Sigma-Aldrich Co., St. Louis, MO, USA) ip, 1 hr prior to sacrifice. At sacrifice, animals were first anesthetized with an intravenous injection of ketamine (10 mg/kg), and the TPN/GLP-2 infusion was stopped. Within 2 min, blood was drawn by cardiac puncture for GLP-2 determinations. Animals were then euthanized with an overdose of sodium pentobarbital (50 mg/kg iv; Huntington Labs, Toronto, ON, Canada) and tissues were harvested.
Morphology: gross and microscopic
Gross intestinal morphology was assessed using standardized methods [25]. Briefly, the remnant bowel was resected from the pylorus to the rectum, the mesentery was removed, and using a standardized tension (10-g weight), bowel length was measured from the duodenojejunal (DJ) junction to the anastomotic site along the antimesenteric border and, for the colon, from the anastomotic site to the rectum. The intestinal circumference was measured midway between the ligament of Treitz and the anastomotic site, and colonic circumference was measured at the middle colic artery. The bowel was then quickly opened along the antimesenteric border and rinsed in cold saline. The intestinal remnants were weighed and samples for morphologic analysis were harvested 4 cm above the anastomosis and fixed in 10% formalin. The adjacent aboral 4 cm of small bowel and a portion of the ascending colon were frozen for protein analysis. Paraffin sections were cut at 6-μm thickness and then stained with hematoxylin and eosin. An observer blinded to the origin of the intestinal tissue assessed morphology. For each slide, measurements of villus height, villus width, crypt depth, and number of villi/100 μm were recorded for a minimum of 10 well-oriented villus/crypt units using an ocular micrometer [32]. The serosal and villus surface area was used to estimate the total intestinal surface area using previously described methods [33].
At the time of tissue harvesting for conventional microscopy, in four animals from each group, a 5-mm rim of jejunal tissue was harvested for electron microscopy, using previously described methods [34, 35]. In brief, the tissue was opened, pinned, and fixed in 5% glutaraldehyde/phosphate buffer. Tissues were postfixed in 1% OsO4 for 2 hr, dehydrated in graded alcohols, treated with propylene oxide, and then embedded in Spurr’s low-viscosity medium (J. B. EM Services, Dorval, PQ, Canada). Ultrathin sections were obtained and double stained with uranyl acetate in 50% ethanol and 0.4% lead citrate. Micrographs were obtained from the midvillus region of the sections, as selected by a low-magnification view of the complete villus. Duplicate measurements from each micrograph were obtained by an observer blinded as to study conditions, and jejunal midvillus brush border area was calculated as previously described [34].
Crypt cell proliferation/apoptotic rates
Crypt cell proliferation and apoptotic rates were quantified using BrdU as a label of actively dividing cells within the crypt and caspase-3 staining as an indicator of apoptosis [25, 36]. BrdU staining was done using our previously validated methods, which have been shown by other authors to correlate well with epithelial cell turnover in the rat [37, 38]. In brief, deparaffinized sections were denatured with 1 M HCl for 1 hr at 60°C and then blocked for 2 hr with phosphate-buffered saline (PBS [mM]: 130 NaCl, 2.7 KCl, 8.1 NaHPO4, 1.5 KH2 PO4, pH 7.3) blocking solution containing 10% normal goat serum and 1% bovine serum albumin (BSA). The jejunal tissue was then incubated in a 1:200 dilution of monoclonal mouse BrdU primary antibody (Sigma) in the same blocking solution at 4°C overnight. Crypt cells incorporating BrdU were detected by immunofluorescence with a Cy3-conjugated anti-mouse IgG secondary (Jackson Immunoresearch Labs, West Grove, PA, USA). Ten consecutive well-oriented crypts per slide were reviewed by an observer blinded as to tissue source and reported as the number of BrdU-staining cells per crypt.
The rate of apoptosis in the crypts was quantified by immunohistochemical staining for intracellular activated caspase-3, using previously validated methods [25, 39]. Activated caspase-3 is the first step of the common final common pathway of apoptosis; staining is detectable before evidence of nuclear changes or TUNEL staining [39]. In previous studies, we have found that villus staining is variable, so this was not done in the present study [25]. In brief, 6-μm paraffin sections were deparaffinized and blocked with 3% hydrogen peroxide for 30 min to reduce endogenous peroxidase activity. Following a 1-hr incubation in blocking buffer (2% BSA, 0.2% milk, 2% normal goat serum, 0.8% Triton X-100 in PBS), the slides were treated overnight at 4°C with either a 1:500 dilution of anti-active caspase-3 antibody (BD PharMingen, Canada) or a 2% BSA/PBS blocking buffer (control). After several washings, the slides were incubated with a 1:25 dilution of horseradish peroxidase-conjugated anti-rabbit IgG for 2 hr at room temperature. Diaminobenzidine (DAB; Vector kit; Vector Laboratories, USA) was added to visualize activated caspase-3. Slides were counterstained with Mayer’s hematoxylin and analyzed. Counts are reported as caspase-3 positive-staining cells per crypt.
Intestinal transporter quantification
In order to assess treatment effects on the expression of intestinal transporter proteins, tissue levels of SGLT 1 and GLUT-5 were quantified using Western blot analysis. In brief, previously snap-frozen samples of jejunum mucosa were thawed, then homogenized in 2.5 mM EDTA, and aliquots were placed in Laemmli’s sample buffer (Sigma Chemical Co.). The protein concentration was determined by Lowry assay [40]. Protein samples were separated by sodium dodecyl sulfate (SDS)–polyacrylamide gel electrophoresis and electrotransferred onto PVDF transfer membranes (Amersham Pharmacia Biotech, Buckinghamshire, England). The resulting blots were blocked with 5% nonfat dry milk in PBS containing 0.05% Tween 20 and then incubated for 24 hr at 4°C with 1:5000 anti-SGLT-1 antibody or 1:2500 anti-GLUT-5 (both from Chemicon, USA). The membranes were then washed and incubated with HRP:anti-rabbit IgG at 1:3000 (Amersham) for 2 hr at room temperature, and positivity was detected by enhanced chemiluminescence with ECL western blotting detection reagents (Amersham) on X-OMAT AR film (Eastman Kodak Co., Rochester, NY, USA). Band density (OD/mm2) was determined using a calibrated imaging densitometer (GS-710; BioRad) and Quantity One software (BioRad).
Serum GLP-2 quantification
Blood draws were completed in the morning on the day of sacrifice. The blood was drawn into heparinized syringes, transferred into chilled EDTA tubes, and centrifuged (in <10 min from the original draw) at 2500g×10 min at 4°C. The serum was collected and placed into cryovials containing 1 mM phenylmethylsulfonyl fluoride (PMSF; in 90% ethanol), quickly frozen on dry ice, and stored at −70°C until analysis. Using our previously described methods , total GLP-2 levels (GLP 1 to 33 and 3 to 33) were measured using an ELISA based on a polyclonal antibody (ALE0303; NPS Pharmaceuticals, Mississauga, ON) specific for GLP-2 1-33 and 3-33 [13]. This assay measures both the active (1-33) and the inactive (3-33) forms of GLP-2, however, the aggregate level is highly correlated with the level of active GLP-2, as determined by 1-33 GLP-2 specific radioimmunoassay [13].
Statistical methods
All data are expressed as means±SE. Comparisons between groups were done using Student’s t test with P < 0.05.
Results
GLP-2 supplementation of TPN induced significant adaptive changes within the remnant jejunum (Table 1). Both groups gained weight over the 8-day study period; there were no significant differences between the groups. Animal well-being (grooming, activity) was also similar for both groups; all animals completed the study. GLP-2 treatment induced a significant increase in small bowel weight both in absolute terms and as a percentage of total body weight. However, the weight of the colon was not affected, nor were there changes in kidney or liver weights between the groups (data not shown). As expected, in the TPN+GLP-2 animals, total GLP-2 levels were significantly increased versus those in the animals given TPN alone (11.4±3.4 vs 0.2±0.1 ng/ml; P < 0.002).
Intestinal glucose absorption/permeability
GLP-2 treatment resulted in a significant increase in 3-O-MG absorption and permeability to Lac, and the Lac/Man ratio was decreased in the TPN+GLP-2 groups (P < 0.05; Table 2). Further, the ratio of 3-O-MG absorption (active transport) to Man (passive uptake) was significantly increased in the TPN+GLP-2 animals (Table 2).
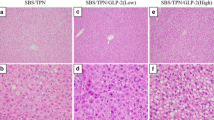
Morphology: gross and microscopic
GLP-2 treatment did not result in a significant change in jejunal length or width. However, the microscopic indexes of villus height and crypt depth were increased, as was the calculated total mucosal surface area (P < 0.05; Table 3a and Fig. 1a).
(A) Jejunal morphology. Microscopic sections stained with hematoxylin and eosin. Treatment groups: TPN and TPN+GLP-2 jejunum. TPN+GLP-2 rats showed a significant increase in villus height, crypt depth, and mucosal surface area (see also Table 3a). (B) Jejunal microvilli. Electron microscopy sections representative of TPN and TPN+GLP-2 jejunum. TPN+GLP-2-maintained rats had a significant increase in microvillus height, density, and surface area (see also Table 4b). Representative photos. (Original magnifications: A, ×20,000; B, ×10.)
In addition, examination of the ultrastructural morphology showed a GLP-2-associated increase in microvillus height and density, with an overall increase in microvillus surface area per unit of villus mucosal surface (P < 0.05; Table 4b and Fig. 1b).
Crypt cell proliferation/apoptotic rates
TPN+GLP-2 therapy resulted in a significant increase in crypt cell proliferation rates (CCPRs) (P < 0.05; Fig. 2). GLP-2 therapy was also associated with an increase in caspase-3 positive-staining cells within the jejunal remnant crypt cell compartment (P < 0.02; Fig. 3).
(A) BrdU immunoreactivity in the crypt region of the jejunum. Sections show BrdU staining of TPN-only or TPN+GLP-2 animals. Crypt cells incorporating BrdU were stained with monoclonal BrdU primary antibody and visualized with Cy3 anti-mouse IgG. Arrows indicate typical staining; all staining indicates BrdU-positive nuclei. (Secondary magnification, ×40.) (B) Crypt cell proliferation changes as assessed by BrdU immunoreactivity. There was a significant increase in the TPN+GLP-2-treated group (* P < 0.05 vs. TPN alone). Mean±SE BrdU immunoreactive cells per crypt.
(A) Activated caspase-3 immunoreactivity in crypt region of jejunal mucosa. Representative active caspase-3 staining (arrows) in the jejunum of the TPN and TPN+GLP-2 groups. Note the increase in caspase-3-immunopositive cells in TPN+GLP2 compared to TPN-only tissue. As described under Materials and Methods, antiactivated caspase-3 antibody was visualized with horseradish peroxidase-conjugated anti-rabbit IgG. Slides were counterstained with Mayer’s hematoxylin. (B) Activated caspase-3 immunoreactivity. Counts are reported as activated caspase-3 positive-staining cells per crypt (mean±SE; * P < 0.002 vs TPN alone). GLP-2 treatment was associated with a significant increase in the number of activated caspase-3-positive cells per crypt.
Nutrient transporter expression
There were no differences in SGLT-1 or GLUT-5 protein expression between the TPN-maintained animals and the GLP-2+TPN animals (Figs. 4 and 5).
Discussion
Intestinal adaptation has classically been studied by examining the postresectional changes occurring in spontaneously feeding animals. The results of the present study show that in animals supported entirely with parenteral nutrition, exogenous GLP-2 induces a specific pattern of adaptive changes in remnant jejunum. Overall the pattern is similar to that described in our previous study of GLP-2-induced adaptation in remnant ileum; however, there were some significant differences. There appears to be change in the rate of breakdown of exogenous GLP-2 with remnant jejunum vs ileum. In previous studies of animals with an ileal remnant model, using an identical infusion protocol, GLP-2 levels were 6.0±1.2 ng/ml, whereas in the present study levels were nearly doubled, at 11.4±3.4 ng/ml [25]. This suggests that in different regions of the intestine there may be intrinsic or resection-induced variations in dipeptidyl peptidase IV (DPP-IV) activity, the primary breakdown pathway of GLP-2 [41]. It is very unlikely that the increase in GLP-2 levels noted was due to any increase in native production since the TPN-alone animals had negligible GLP-2 levels. Further studies are suggested to examine the relationship between resection and GLP-2 metabolism.
Importantly GLP-2 was shown to induce an increase in crypt cell proliferation and an increase in villus height and crypt depth in remnant jejunum. Overall, there was a significant increase in small intestinal weight, protein, and DNA content (Table 1). The effects were similar to those seen in the ileal remnant using a similar rodent model [25], and parallel aspects of the effects in jejunum seen in a porcine model, supported by TPN [42] and studies done in rats maintained on enteral nutrition [43]. Comparisons with these studies suggest that there may be a dose relationship between GLP-2 and crypt cell proliferation. In studies using a neonatal pig model, using a lower and intermittent dose of GLP-2, no increase in CCPR was noted; however, in studies using a higher intermittent dose, or continuous infusion as in the present study, a definite increase in crypt cell proliferation rate was noted [42, 43]. It is interesting to note that in our studies in spontaneously adapting, enterally fed animals, both basal and meal-stimulated levels of GLP-2 were elevated to the range of 7–9 ng/ml (using the same assay as in the present study). CCPR was best correlated with peak postprandial levels [13]. Further study is required to determine if the variations in the described effects of GLP-2 on CCPR are due to species differences or variations in the dosing level and/or pattern.
An unexpected finding of the present study was a significant increase in apoptosis within the crypt compartment in the remnant jejunum of GLP-2-treated animals. In our previous studies we saw a nonsignificant increase in apoptotic rates in remnant ileum stimulated with exogenous GLP-2, while other authors have suggested a GLP-2-induced decrease in apoptosis [25, 42]. These results are similar to the variation in the described effects of resection on apoptosis. For example, in studies using an enterally fed mouse model of SBS [36, 44–46], the adapting remnant ileum shows a consistent increase in apoptosis, which has been related to EGF receptor signaling and bax expression. Conversely, in studies using mice, TPN-maintained pigs, or GLP-2-transfected cell models, and varyious methods of assaying apoptosis, GLP-2 has been suggested to decrease apoptosis [42, 46–48]. The results of the present study suggest that continual GLP-2 stimulation results in an increase in crypt compartment apoptotic rates in the jejunum. The reason for this is not intuitive but could be related to changes in crypt cell “selection” for absorptive function of the enterocyte [3, 17, 37]. In this paradigm, activation of the crypts results in increased production of all intestinal cell lines, with subsequent selection for apoptosis of nonabsorptive phenotypes (e.g., enteroendocrine, mucus producing cells) during the maturation phase through the crypts [17, 49]. The variations in the described effects of GLP-2 on apoptosis seen in other reports may relate to differential GLP-2 effects at different sites of the intestine, varying doses, species differences, or variations in testing methodology. The results of the present study suggest that GLP-2 in vivo induces an increase in crypt compartment apoptosis, which is similar to that described in spontaneously adapting, enterally fed animals following resection; this important point requires further direct study.
We did not see an effect of GLP-2 on the active or passive glucose transporter SGLT-1 or GLUT-5, respectively. This contrasts both with our previous results and other authors’ findings with higher doses of GLP-2 in the jejunum [25, 43]. It may be relevant that in the present study mucosal sampling was done consistently in the morning, which would correspond to the lower expression phase of the diurnal variation of SGLT-1 protein expression [43]. However, the improvement in vivo of 3-O-MG absorption was consistent with observations from our previous work [25]. Furthermore, expression of the uptake of 3-O-MG to the uptake of Man as a ratio, which was also significantly increased in the GLP-2-treated animals (Table 2), shows that this is due to an increase in active transport, and not to nonspecific absorption through an increased surface area. Taken together, these findings suggest that GLP-2 treatment of residual jejunum increases nutrient absorptive capacity by increasing the mucosal surface area available for nutrient transport, rather than increasing the density of transporters per unit surface area, which parallels the findings of typical nutrient-induced intestinal adaptation [2, 3, 26]. In ileum, GLP-2 may be able to increase both surface area and SGLT-1 transporter expression [25].
An additional unique observation of the present studies was the effect of GLP-2 on jejunal microvillus architecture. The increases in microvillus height and density are features of increased nutrient absorptive capacity [34]. Moreover, they may be some of the mechanisms of the previously described GLP-2-induced increases in SGLT-1 function [23, 25, 52]. The parallels with EGF-induced increases in brush border surface area are striking [34] and suggest that the GLP-2 and EGF effector pathways may overlap [53].
Importantly, the observed decrease in permeability with GLP-2 may also be clinically relevant. In human patients with SBS, systemic sepsis from enteric organisms can be a difficult problem; GLP-2 may be useful in preventing bacterial translocation in these patients, reducing the tendency for enteric-induced infection in SBS patients [2, 50, 51].
These findings highlight the region-specific effects of GLP-2 as a trophic peptide. Our results suggest that GLP-2 results in a consistent increase in crypt cell proliferation throughout the intestine, but a differential effect on apoptosis. This may in turn alter enterocyte maturation and so alter the transport capability of the mature villus. This is likely relevant both in adaptation following resection or disease states and in the normal regulation of nutrient absorptive capacity in response to variations in nutrient availability for free-living animals. Clearly, there are significant and biologically important effects of GLP-2 on intestinal function and whole-animal physiology that strongly support further research.
References
Dowling RBC (1967) Structural and functional changes following small intestinal resection in the rat. Clin Sci 32:139–143
Sigalet DL (2001) Short bowel syndrome in infants and children: an overview. Semin Pediatr Surg 10(2):49–55
Williamson RC (1978) Intestinal adaptation I and II. N Engl J Med 298:1393–1450
Mayo KE, Miller LJ, Bataille D, et al. (2003) International Union of Pharmacology. XXXV. The glucagon receptor family. Pharmacol Rev 55(1):167–194
Brubaker PL, Izzo A, Hill M, Drucker DJ (1997) Intestinal function in mice with small bowel growth induced by glucagon-like peptide-2. Am J Physiol 272(6, Pt 1):E1050–E1058
Drucker DJ, Erlich P, Asa SL, Brubaker PL (1996) Induction of intestinal epithelial proliferation by glucagon-like peptide 2. Proc Natl Acad Sci USA 93(15):7911–7916
Orskov C, Holst JJ, Knuhtsen S, Baldissera FG, Poulsen SS, Nielsen OV (1986) Glucagon-like peptides GLP-1 and GLP-2, predicted products of the glucagon gene, are secreted separately from pig small intestine but not pancreas. Endocrinology 119(4):1467–1475
Roberge JN, Brubaker PL (1991) Secretion of proglucagon-derived peptides in response to intestinal luminal nutrients. Endocrinology 128(6):3169–3174
Rocca AS, Brubaker PL (1999) Role of the vagus nerve in mediating proximal nutrient-induced glucagon-like peptide-1 secretion. Endocrinology 140(4):1687–1694
Drucker DJ (2002) Biological actions and therapeutic potential of the glucagon-like peptides. Gastroenterology 122(2):531–544
Sigalet DL (2001) ALX-0600 (NPS Allelix Corp). Curr Opin Invest Drugs 2(4):505–509
Brubaker PL, Schloos J, Drucker DJ (1998) Regulation of glucagon-like peptide-1 synthesis and secretion in the GLUTag enteroendocrine cell line. Endocrinology 139(10):4108–4114
Martin GR, Wallace LE, Hartmann B, et al. (2005) Nutrient-stimulated GLP-2 release and crypt cell proliferation in experimental short bowel syndrome. Am J Physiol Gastrointest Liver Physiol 288(3):G431–G438
Bozkurt A, Naslund E, Holst JJ, Hellstrom PM (2002) GLP-1 and GLP-2 act in concert to inhibit fasted, but not fed, small bowel motility in the rat. Regul Pept 107(1–3):129–135
Ljungmann K, Hartmann B, Kissmeyer-Nielsen P, Flyvbjerg A, Holst JJ, Laurberg S (2001) Time-dependent intestinal adaptation and GLP-2 alterations after small bowel resection in rats. Am J Physiol Gastrointest Liver Physiol 281(3):G779–G785
Munroe DG, Gupta AK, Kooshesh F, et al. (1999) Prototypic G protein-coupled receptor for the intestinotrophic factor glucagon-like peptide 2. Proc Natl Acad Sci USA 96(4):1569–1573
Bjerknes M, Cheng H (2001) Modulation of specific intestinal epithelial progenitors by enteric neurons. Proc Natl Acad Sci USA 98:12497–12502
Wallace LE, Martin G, Swain MG, Sharkey KA, Sigalet DL (2004) Acute GLP-2 treatment induces effects in both peripheral and central nervous systems. Can J Gastroenterol 18:A120
Ramsanahie A, Duxbury MS, Grikscheit TC, et al. (2003) Effect of GLP-2 on mucosal morphology and SGLT1 expression in tissue-engineered neointestine. Am J Physiol Gastrointest Liver Physiol 285(6):G1345–G1352
Rocha FG, Shen KR, Jasleen J, et al. (2004) Glucagon-like peptide-2: divergent signaling pathways. J Surg Res 121(1):5–12
Walsh NA, Yusta B, DaCambra MP, Anini Y, Drucker DJ, Brubaker PL (2003) Glucagon-like peptide-2 receptor activation in the rat intestinal mucosa. Endocrinology 144(10):4385–4392
Yusta B, Huang L, Munroe D, et al. (2000) Enteroendocrine localization of GLP-2 receptor expression in humans and rodents. Gastroenterology 119(3):744–755
Cheeseman CI (1997) Upregulation of SGLT-1 transport activity in rat jejunum induced by GLP-2 infusion in vivo. Am J Physiol 273(6, Pt 2):R1965–R1971
Guan X, Stoll B, Lu X, et al. (2003) GLP-2-mediated up-regulation of intestinal blood flow and glucose uptake is nitric oxide-dependent in TPN-fed piglets. Gastroenterology 125(1):136–147
Martin GR, Wallace LE, Sigalet DL (2004) Glucagon-like peptide-2 induces intestinal adaptation in parenterally fed rats with short bowel syndrome. Am J Physiol Gastrointest Liver Physiol 286(6):G964–G972
O’Brien DP, Nelson LA, Huang FS, Warner BW (2001) Intestinal adaptation: structure, function, and regulation. Semin Pediatr Surg 10(2):56–64
Jeppesen PB, Hartmann B, Hansen BS, Thulesen J, Holst JJ, Mortensen PB (1999) Impaired meal stimulated glucagon-like peptide 2 response in ileal resected short bowel patients with intestinal failure. Gut 45(4):559–563
Sigalet DL, Martin G, Meddings J, Hartman B, Holst JJ (2004) GLP-2 levels in infants with intestinal dysfunction. Pediatr Res 56(3):371–376
Topstad D, Martin G, Sigalet D (2001) Systemic GLP-2 levels do not limit adaptation after distal intestinal resection. J Pediatr Surg 36(5):750–754
Meddings JB, Gibbons I (1998) Discrimination of site-specific alterations in gastrointestinal permeability in the rat. Gastroenterology 114(1):83–92
Martin GR, Meddings JB, Sigalet DL (2003) 3-O Methylglucose absorption in vivo correlates with nutrient absorption and intestinal surface area in experimental short bowel syndrome. J Parenter Enteral Nutr 27(1):65–70
Menge H, Hopert R, Alexopoulos T, Riecken EO (1982) Three-dimensional structure and cell kinetics at different sites of rat intestinal remnants during the early adaptive response to resection. Res Exp Med (Berl) 181(2):77–94
Sigalet DL, Martin GR, Poole A (2000) Differential sugar absorption as a marker for adaptation in short bowel syndrome. J Pediatr Surg 35(5):661–664
Chung BM, Wong JK, Hardin JA, Gall DG (1999) Role of actin in EGF-induced alterations in enterocyte SGLT1 expression. Am J Physiol 276(2, Pt 1):G463–G469
Buret A, Gall DG, Olson ME (1991) Growth, activities of enzymes in the small intestine, and ultrastructure of microvillus border in gerbils infected with Giardia duodenalis. Parasitol Res 77(2):109–114
Cohn SM, Lieberman MW (1984) The use of antibodies to 5-bromo-2’-deoxyuridine for the isolation of DNA sequences containing excision-repair sites. J Biol Chem 259(20):12456–12462
Potten CS, Loeffler M (1990) Stem cells: attributes, cycles, spirals, pitfalls and uncertainties. Lessons for and from the crypt. Development 110(4):1001–1020
Musckhelishvili L, Latendresse JR, Kodell RL, Henderson EB (2003) Evaluation of cell proliferation in rat tissues with BrdU, PCNA, Ki-67(MIB-5) immunohistochemistry and in situ hybridization for histone mRNA. J Histochem Cytochem 51(12):1681–1688
Marshman E, Ottewell PD, Potten CS, Watson AJM (2001) Caspase activation during spontaneous and radiation–induced apoptosis in the murine intestine. J Pathol 195:285–292
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193(1):265–275
Dunphy JL, Justice FA, Taylor RG Fuller PJ (1999) mRNA levels of dipeptidyl peptidase IV decrease during intestinal adaptation. J Surg Res 87:130–133
Burrin DG, Stoll B, Jiang R, et al. (2000) GLP-2 stimulates intestinal growth in premature TPN-fed pigs by suppressing proteolysis and apoptosis. Am J Physiol Gastrointest Liver Physiol 279(6):G1249–G1256
Ramsanahie AP, Berger UV, Zinner MJ, Whang EE, Rhoads DB, Ashley SW (2004) Effect of glucagon-like peptide-2 (GLP-2) on diurnal SGLT1 expression. Dig Dis Sci 49(11–12):1731–1737
Jarboe MD, Juno RJ, Bernal NP, et al. (2004) Bax deficiency rescues resection-induced enterocyte apoptosis in mice with perturbed EGF receptor function. Surgery 136(2):121–126
Knott AW, O’Brien DP, Juno RJ, et al. (2003) Enterocyte apoptosis after enterectomy in mice is activated independent of the extrinsic death receptor pathway. Am J Physiol Gastrointest Liver Physiol 285(2):G404–G413
Dahly EM, Guo Z, Ney DM (2002) Alterations in enterocyte proliferation and apoptosis accompany TPN-induced mucosal hypoplasia and IGF-I-induced hyperplasia in rats. J Nutr 132(7):2010–2014
Tsai CH, Hill M, Asa SL, Brubaker PL, Drucker DJ (1997) Intestinal growth-promoting properties of glucagon-like peptide-2 in mice. Am J Physiol 273:E77–E84
Yusta B, Boushey RP, Drucker DJ (2000) The glucagon-like peptide-2 receptor mediates direct inhibition of cellular apoptosis via a cAMP-dependent protein kinase-independent pathway. J Biol Chem 275(45):35345–35352
Marshman E, Booth C, Potten CS (2002) The intestinal epithelial stem cell. BioEssays 24:91–98
Kouris GJ, Liu Q, Rossi H, et al. (2001) The effect of glucagon-like peptide 2 on intstinal permeability and bacterial translocation in acute necrotizing pancreatitis. Am J Surg 181:571–575
Sigalet DL, Martin G, Meddings J (2004) 3-O Methylglucose absorption in vivo correlates with nutrient aborption and intestinal surface area in experimental short bowel syndrome. JPEN J Parenter Enteral Nutr 28:158–162
Scott RB, Kirk D, MacNaughton WK, Meddings JB (1998) GLP-2 augments the adaptive response to massive intestinal resection in rat. Am J Physiol 275(5, Pt 1):G911–G921
Dahly EM, Gillinham MB, Guo Z, et al. (2003) Role of luminal nutrients and endogenous GLP-2 in intestinal adaptation to mid-small bowel resection. Am J Physiol Gastrointest Liver Physiol 284:G670–G682
Acknowledgments
This study was supported by funding from the Alberta Children’s Hospital Research Foundation. We thank NPS Pharmaceuticals for provision of GLP-2 and performance of assays and Lidia Demchyshyn for support. Thanks are also due to Gail Wright-Wilson for secretarial support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sigalet, D.L., Bawazir, O., Martin, G.R. et al. Glucagon-like Peptide-2 Induces a Specific Pattern of Adaptation in Remnant Jejunum. Dig Dis Sci 51, 1557–1566 (2006). https://doi.org/10.1007/s10620-006-9077-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-006-9077-5