Abstract
Liver cancer, one of the leading causes of all cancer related deaths, belongs to the most malignant cancer types. In fact, the secondary hepatic malignancies (liver metastases) are more common than the primary ones. Almost all solid malignancies can metastasise to the liver. It is well justified that the “treat and wait” approach in the overall management of the liver cancer is not up-to-date and so creation of complex individual patient profiles is needed. This review is specifically focused on the liver metastases originating from the colorectum, breast and prostate cancer. Innovative multilevel diagnostics may procure specific panels of validated biomarkers for predisposition, development and progression of metastatic disease. Creation of the patient specific “molecular portrait” is an essential part of the diagnostic strategy. Contextually, analysis of molecular and cellular patterns in blood samples as the minimally invasive diagnostic tool and construction of diagnostic windows based on individual patient profiling is highly recommended for patient cohorts predisposed to and affected by the liver metastatic disease. Summarised information on risk assessment, predictive and prognostic panels for diagnosis and treatments of the liver metastatic disease in colorectal, breast and prostate cancer is provided.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metastatic spread (metastatic disease (MD)) of primary tumours is the most important issue in cancer related mortality. MD is highly heterogeneous with respect to the tumour origin, molecular mechanisms, preference of distanced organs for metastatic spread, disease aggressiveness, therapy prognosis and individual outcomes [1]. Consequently, an individual patient phenotype might be decisive for more versus less pronounced predisposition to MD in cancer patients, disease progression, and, consequently chosen treatment approach. It is evident that patients with the triple-negative subtype of breast cancer (BC) have a higher predisposition to MD at a very early stage of the tumour initiation compared to the oestrogen/progesterone-receptor positive subtypes of BC who, if any, develop MD years or even decades later after the clinical BC onset [2]. Therefore, MD related mechanisms, diagnostics, effective prevention and therapy-targeting differ dramatically between individual tumour subtypes and patient phenotypes [3]. Further, MD frequently demonstrates organ-specific patterns of spread [4] that demands a development of MD-related predictive diagnostics and analysis of stratified MD patterns.
Liver cancer, one of the leading causes of all cancer related deaths, belongs to the most malignant cancer types. In fact, the secondary hepatic malignancies (liver metastases) are more common than the primary ones [5]. Numerous studies reveal that, after lymph nodes, the liver is the most common site of metastases from cancers arising in other (primary) sites [6]. Almost all solid malignancies, essentially the gastrointestinal cancers, breast cancers, lung cancers, genitourinary cancers, melanomas, sarcomas can metastasise to the liver. Thus, it is well justified that the “treat and wait” approach in the overall management of liver cancer is not up-to-date and so creation of complex individual patient profiles is needed [7, 8].
The corresponding incidence of hepatic metastasis of primary tumours is summarised in Fig. 1. Recently, a study carried out with altogether 3827 autopsies has detected 41 different primary cancer types with corresponding preferential metastatic sites. It concluded that the local and regional lymph nodes followed by the liver are the most frequent metastatic sites in all primary malignancies analysed in the study [6].
This review is specifically focused on (1) liver metastases originating from colorectal cancer (CRC) and BC—both carcinomas which metastasise to the liver more frequently than other primary tumours [6] and (2) liver metastasis originating from both breast and prostate cancer (PC), since both carcinomas are linked to and should be stratified by corresponding hormonal status of the patient [9]. Potential similarities in their metastatic spread to the liver are analysed in the article which might be of great interest for both diagnostic and treatment purposes. Consequently, the primary objective of the article is to interpret the currently existing data regarding the metastatic colonisation of the liver and potential specificity of the underlying mechanisms.
From primary tumours to circulating tumour cells (CTCs), micrometastases colonising the “fertile” environment and progressing metastatic disease
The cancer invasion-metastasis cascade includes multiple molecular pathways regulating “down-stream” intra- and extracellular events. The triggered cascade leads to the tumour expansion, detachment and circulation of tumour cells [10]. Circulating tumour cells (CTCs), in turn, preferably enter the “fertile” environment of distant organs such as that found in a damaged liver [11], colonise the “pre-metastatic niches” of the host with micrometastases [4] and then progress into advanced stages of the MD.
Development of liver metastases from all three cancer types (CRC, BC and PC) positively correlates with the density of CTCs in blood—an important prognostic factor [12]. Further investigations of this correlation may provide valuable data for a better patient stratification.
In order to examine the biological process of the metastatic progression to the liver, a xenograft metastasis model has been created and analysed in detail [13]. This model has shown that malignancies respond specifically to the host tumour’s environment facilitating metastatic progression [13]. In particular, breast malignancies react towards the “fertile” environment, thus expanding the outgrowth of microscopic secondary tumours [13–16]. Dormant tumour cells may persist in the latent phase for years before entering the active metastatic progression phase. Thereby, primary tumour cells retain the ability to influence the outgrowth of secondary tumours [13]. The progression from micrometastasis to an active MD (macrometastasis) depends on the biological characteristics of the tumour itself as well as on the synergies between the tumour and the host [17]. Consequently, only a minor portion—about 1 % or even less—of all CTCs are capable of developing a MD [18, 19].
A number of studies demonstrated a correlation between standardised histopathological biomarkers of BC and tumour cells disseminated in bone marrow (DTC), tumour cells circulating in peripheral blood CTC [20, 21] as well as circulating cell-free DNA [22]. Further, CTC level measured prior to the therapy initiation as well as at follow-up stages is an important predictor for both the progression-free and overall survival (OS) [23]. In particular, CTC levels of ≥5 cells per 7.5 ml blood in patients provide robust estimates for disease progression and survival that are more reliable than the conventional imaging approaches. Accumulated clinical data confirms a strong correlation between the pre-treatment CTC levels and the magnitude of metastatic spread at the stage of disease progression, especially for CTC levels ≥5/7.5 versus ≤5/7.5 ml of blood. Further, recent results of a prospective clinical trial confirmed the strong prognostic value of CTC in breast cancer MD. It suggests that the pre-treatment CTC levels may aid in stratifying breast cancer patients who are at risk of developing widespread visceral MD. Those patients, if identified early enough, may strongly benefit from preventive administration of aggressive anti-metastatic treatments [17, 24]. Investigations dedicated to predictive and prognostic value of individual CTC patterns with respect to a specific metastatic site may, further, lead to improved patient stratification and better adapted treatment strategies.
Castration resistant prostate cancer (PC) patients with greater than five CTC per 7.5 mL blood are known to suffer from a significantly shorter OS compared to the patients with ≤5 CTC [25]. Post-treatment CTC level is an independent predictor of the survival rates as CTC count was demonstrated to be superior to prostate specific antigen (PSA) in predicting survival [26]. Consequently, the role of CTC levels in prediction and prognosis of PC outcomes is increasing. In metastatic PC, CTC detection is an accurate minimally invasive approach for monitoring the disease progression. CTC patterns, as a specific biomarker, hold the potential to predict early metastasis [26]. CTC patterns in blood provide a platform for non-invasive inquiries into a tumour’s molecular behaviour enabling individualised, adaptive and more effective overall management of PC [26].
In case of colorectal liver metastasis, CTC levels are significantly higher in non-resectable (46 %) than in resectable cases (11.7 %) [27]. Patients with two or more CTC in the pattern, experience reduced time of relapse and disease progression; those CTC patterns are considered to be a strong predictor of the disease progression and mortality in patients with both resectable and non-resectable colorectal liver metastasis. Similarly to the prostate and breast cancer, CTC patterns in patients with colorectal liver metastasis are useful for more precise patient stratification and treatment prognosis [12].
In recent years, cell free nucleic acids (cfNAs, also known as CNAPS—circulating nucleic acids in plasma and serum) have been studied extensively, due to its evident association with cancer development and progression [28]. Yet, several mechanisms leading to the release of nucleic acids into the extracellular environment are not well understood. However, a biological function of cfNAs in tumour progression is evidence-based. Currently, there is no consensus on a gold standard for cfNAs analytical procedure. Future approaches targeting cfNAs in combination with characterisation of the disease/stage specific CTC patterns may lead to improved strategy for more optimal screening, diagnostics and treatment approaches in breast, prostate and colorectal cancer patients predisposed to MD [28].
Liver specific architecture and key players in creating “fertile” pre/metastatic microenvironment
The quality of interaction between CTC and microenvironment of the homing organ is a factor considered to be decisive for a metastatic spread in distanced organs [13]. From this perspective, the liver demonstrates some organ-specific properties predisposing it to CTC nesting and effective promotion of MD [4]. In the gastrointestinal cancers like CRC, which are drained by the enterohepatic circulation, the tumour cells reach the liver first. The liver provides opportunity to a number of tumour cells to arrest, extravasate and colonise the hepatic parenchyma [29]. Moreover, recent studies suggest that a significant percentage of CRC tumour cells are trapped in the liver [30]. Frequent metastatic spread of more distanced tumours such as breast and prostate cancer to the liver indicates that, indeed, circulation patterns (CTC, cfNAs) play an important role as discussed above. Further, multifaceted compatibilities of metastatic cells with the host stroma, organ-specific vascular architecture, cellular repertoire, typical set-up of angiogenic and growth factors, cytokines and metabolites play a crucial role, specifically in the liver metastasis [31]. The hepatic vascular endothelium is fenestrated and lacks an organised basement membrane that may particularly facilitate an effective nesting of invasive tumour cells [1]. Thereby, an elevated SRC proto-oncogene tyrosine kinase signalling protects the tumour cells from undergoing apoptosis within the new environment [4]. Additionally cancer cells release macrophage-migration inhibitory factor (MIF) which in turn triggers the TGFβ production that synergistically activates the stellate cells and recruitment of bone marrow derived cells [32]. These mechanisms collectively contribute to the invasiveness of secondary tumours and aggressive MD. Specific signalling on molecular level is typical for primary tumour cells leading to metastatic initiation and progression. Hence, the colon cancer cells secrete periostin which stimulates PI3 K/AKT signalling pathway in the colonised liver [4, 33]. Cancer cells interact with hepatocytes via claudin-2 stimulating metastatic activity [4]. The secretion of creatine kinase brain-type (CKB) by cancer cells contributes to metastatic outgrowth by generating phosphocreatine as a metabolite to regenerate ATP in cancer cells [34].
Major phases of the liver metastasis nesting and progression
The major phases of the liver metastasis nesting and progression include (i) the microvascular phase, that involves tumour cell arrest in the sinusoidal vessels and may lead to tumour cell death or extravasation, (ii) the extravascular phase/preangiogenic phase, during which the host stromal cells are recruited into avascular micrometastasis, (iii) the angiogenic phase, during which endothelial cells are recruited and the tumours become vascularised through interactions with microenvironment, and (iv) tumour growth phase which leads to clinically manifested metastases [35]. The unique vascular architecture of the liver allows primary and secondary tumours to acquire adequate nutrients and oxygen through various mechanisms linked to angiogenesis. Well known angiogenic/pro-angiogenic factors associated with the promotion and also inhibition of the liver metastases are as follows:
-
VEGF is associated with tumour progression and MD;
-
IL-8 has shown to contribute to human cancer progression through mitogenic, angiogenic and motogenic factors;
-
Integrins are transducers of extracellular matrix signals that influences endothelial cell survival;
-
PD-ECGF is involved in angiogenic and chemotactic activities;
-
TSP-1 and TSP-2 are known to inhibit angiogenesis.
These factors collectively may create the specific biomarker panel that is clinically useful for diagnostic and therapeutic purposes [36].
Metastatic spread from distant organs into the liver: heterogeneity and similarities
Currently, liver resection is the only potentially curative treatment for the liver MD [37]. For patients with the liver as the only metastatic site, surgical resection could provide survival rates of 27–39 % or higher, wherefrom, however, not more than 20 % patients may achieve long-term cure [38–41]. The major criteria for patients to undergo resection is the anticipation of attaining a negative margin (R0), whilst maintaining an adequate future liver remnant (FLR) with adequate vascular inflow, outflow and biliary drainage [42]. The factors specifically influencing the treatment approach are: safe resectability of metastatic lesions, FLR and concurrent liver pathologies diagnosed in the patient [43]. Despite careful consideration, about 58–78 % of the operated patients demonstrate recurrence after initial resection of liver metastases [44–47], and the follow-up complications such as liver and pelvic recurrence, are still frequent for the liver resection; the latter may develop hepatic recurrence as well. Patients with hepatic recurrence may undergo a repeated resection resulting in increased 3–5-year survival rates [42]. Although highly individual, an overall survival (OS) in patients with hepatic recurrence is associated with the number of metastatic sites rather than with the site of recurrence [43].
Inadequate FLR is a major contributor to liver failure; appearing as an early complication of post-hepatectomy [48]. An otherwise healthy liver tissue can tolerate reducing its volume all the way down to 20 % [43]. However, post-chemotherapeutic liver injury or cirrhosis requires sufficiently higher FLR of 30–40 % being particularly sensitive to the grade of the overall liver injury [49–51]. Comorbidities such as non-alcoholic steatohepatitis worsen the individual post-operative outcomes and increase morbidity rates [52–55], frequently related to hepatocellular insufficiency, especially in patients with BMI of more than 35 kg/m2 [56].
Gold standard of resectable liver metastasis from CRC is liver resection. There is no evidence of survival benefit of adjuvant chemotherapy after the liver resection.
Inoperability is usually due to large solitary tumours with insufficient liver remnants or due to an extensive bilobar disease [57]. For an inoperable liver MD, chemotherapeutic treatment is considered to be the first choice option [58]. While the general goal of chemotherapy is confined to prolong the OS, those patients who demonstrate a particularly good therapy-response may later be reconsidered to undergo a successful liver resection [59]. Additionally neo-adjuvant chemotherapy is applied prior to resection of the liver metastases, in order to improve post-operative individual outcomes and suppress metastatic recurrence [60]. In contrast, patients with inoperable liver metastases receiving systemic chemotherapy demonstrate 1-year, 3-year and 5-year OS rates by 83, 41 and 22 %, respectively [61]. The strategy of down staging the disease by chemotherapy [62–64] is referred to as conversion chemotherapy resulting in a 5-year survival in about 30 % of patients who undergo subsequent surgical resection [65]. New treatment modalities and innovative technologies are currently under development considering individualised patient profiles and treatments targeted to the affected molecular pathways of individual patients [66].
Liver metastatic spread specifically by colorectal cancer
Incidence and particularities
CRC is the third most common type of cancer but one of the leading causes of cancer-related deaths [67]. CRC occurs in both males and females, although it is more prevalent in males [68]. The reasons for this pattern are not completely understood yet. However, the cumulative effects of better awareness of CRC-screening in women and sex-specific exposure to endogenous and exogenous risk factors are suspected to play a role in this pattern. In contrast to CRC, prostate and breast cancer are two most common hormone-dependent cancers [69] as described later. Corresponding age of onset of all three primary tumours varies a lot. Therefore, CRC can occur both in young adult and aging populations, although more than 90 % of affected individuals are older than 50 years of age. The genetic predisposition is an important parameter to be considered for predictive diagnostics [67].
Liver resection is the only curative treatment for patients with colorectal metastases [43]. The liver is the most common site of metastases from CRC, which can be attributed to the following facts: (i) a short distance to the liver for outgrowing CRC invasive cells; (ii) the liver filters the venous drainage from the intra-abdominal viscera that is relevant for circulating tumour cells and cell-fee nucleic acids which, therefore, may enter the liver; (iii) due to its specific architecture, liver tissue consists of several types of cells providing a particularly “fertile” microenvironment for nesting of tumour cells [4]. As such, (i) is more specific for CRC liver metastasis, while (ii) and (iii) are common also for more distanced primary tumours such as breast and prostate cancer.
The incidence of CRC can be attributed to both familial and non-familial causes. About 30 % of CRC are familial (or hereditary) [67]. Sporadic CRC is much more frequent accounting for about 70 % of all cases [67]. It is noteworthy that a large patient cohort study, performed recently, demonstrated higher prevalence of synchronous liver MD in male compared to that of female: corresponding sex ratio is 2:1 by the age standardised incident rates. Further, the risk of developing synchronous MD decreases with progressing age [68]. Similarly, the frequency of metachronous MD is lower in females and patients aged over 75, decreasing with progressing age. Liver metastases are more frequent in primary colorectal tumours bigger than 3 cm in diameter compared to smaller ones [68]. The tumour progression stage at the time of diagnosis has been demonstrated to be the most important prognostic factor [68].
CRC specific biomarker panels with predictive and prognostic power for metastatic spread into the liver
Tumour metastasis to the liver involves an extensive tissue remodelling process which creates a “fertile” hepatic microenvironment for successful nesting of metastases enabling adhesion and extravasation of penetrating CRC cells [70–72]. The influx of metastatic tumour cells into the liver leads to a proinflammatory cytokine cascade rapidly activated by the host. Thereby, an induced Kupffer cell-mediated TNF-α production is followed by an increased expression of the vascular adhesion receptors E-selectin P-selectin, vascular cell adhesion molecule-1, and intercellular adhesion molecule-1 on sinusoidal endothelial cells. This highly selective inflammatory response to liver-invading tumour cells may influence the course of MD [71].
Microsatellite instability and epidermal growth factor (EGF) signalling pathway have been found to have prognostic and/or therapeutic value in MD of CRC [73]. Hence, the EGF signalling pathway targeting drugs are now available commercially for the treatment of stage IV metastatic CRC.
Recent studies reveal Musashi2 (MSI-2) to be highly expressed in CRC [74]. The Musashi (MSI), (with homologs MSI-1 and MSI-2, RNA-binding proteins family), acts as a post-translational repressor of target mRNA [75]. Overexpression of MSI-2 is associated with higher aggressiveness of invasion and spread of metastases including distant metastases to the liver [74]. The combination of both parameters, namely the over-expressed intratumoural MSI-2 and clinical TNM-staging (histological tumour grade (T), affected lymph nodes (N), metastases spread (M)) sufficiently increases the predictive power compared to this of individual parameters considered alone. Nanog, a transcription factor critical for the regulation of cell fate in the inner cell mass during embryonic development and pluripotency of embryonic stem cells, was found to be overexpressed in CRC and are related to histological tumour grade, lymph node metastasis, TNM-staging and liver metastasis [76]. Thus, the Nanog protein may be a potential biomarker for postoperative liver metastasis of CRC [77].
Clinical proteomics utilising urine samples has been developed as a highly sensitive diagnostic tool specifically for CRC metastasising to the liver [78]. To this end, two collagen-1-related peptides have been demonstrated as highly pathology-specific biomarker-candidates associated with tissue remodelling during metastatic invasion. Specific patterns of the epidermal growth factor receptor (EGFR) and prostaglandin-endoperoxide synthase 2 (PTGS2) with increased expression rates have been demonstrated as independent prognostic factors for poor prognosis in CRC patients with liver metastases after resection [79–81].
The miR-200 family of microRNA (miR-200a, miR-200b, miR-200c, miR-141, and miR-429) inhibits E-cadherin-suppressor targets (zinc finger E-box binding homeobox-1 and -2) which are important initiators of epithelial-mesenchymal transition (EMT) in CRC [82, 83]. Altered patterns of miR-200b, -200c, -141 and -429 are responsible for EMT-MET (mesenchymal-epithelial transition) switch in CRC metastasis [84]. The miR-200c/429 cluster is significantly overexpressed in patients with CRC liver metastasis compared to primary CRC that is regulated at the epigenetic level [85]. High serum concentrations of miR-200c are associated with poor prognosis, shorter overall survival being, therefore, an independent prognostic marker differentiating between CRC patients with and without liver MD [84]. Consequently, analysis of preoperative level of miR-200c in serum may be of clinical utility to identify CRC patients particularly predisposed to the tumour recurrence and active MD.
Liver metastatic spread specifically by breast cancer
Incidence and particularities
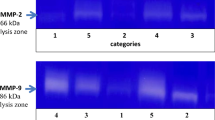
Breast cancer (BC) is recognised as a potential epidemic in the early twenty-first century [3] with around half-a-million deaths and about 1.7 million new cases annually [86]. Although BC mortality rates have slightly decreased over the last decades, the incidence rates continue to grow [87]. BC is highly heterogeneous in nature. About 10–15 % of patients develop an aggressive disease with distant metastases within 3 years of initial detection of the primary tumour—especially patients with triple-negative BC subtype [3]. Other BC subtypes (such as oestrogen/progesterone receptor positive BC) tend to develop distanced metastases several years or even some decades after BC treatment [2]. The long latency period between the tumour initiation and active MD denotes that BC is a systemic disease [13]. Consequently, BC patients are at risk of developing MD for their entire lifetime [3]. As recently documented, patients with hepatic BC metastases demonstrate highly specific profiles of matrix metalloproteinases as compared to other primary and secondary liver tumours [88]. Therefore, a more precise patient stratification and multilevel diagnostics is recommended for an advanced management of BC and MD in this patient cohort [3, 88].
Liver metastasis is found in about 25 % of patients with metastatic BC [89]. The most precise BC categorisation is based on corresponding molecular patterns as illustrated in Table 1 [90, 91]. Obese women were found to have 34 % higher risk of death from metastatic BC compared to patients with body mass index (BMI) within the standard range [92]. Further, clear indication has been recently provided demonstrating that underweight women (BMI < 20) are at sufficiently higher risk for BC mortality compared to the standard range BMI = 20–25 [93].
Poor prognosis in BC is linked to the visceral metastases development especially to the liver and lung. Liver resection in BC MD is shown to be beneficial for patients demonstrating a median survival of 38 months compared to 18 months in patients undergoing chemotherapy only [94]. An accurate grading of primary BC is a strong prognostic factor for metastases spread into the liver. Beneficial effects of chemo-adjuvant therapy specifically against liver metastases in BC are not well investigated yet.
BC specific biomarker panels with predictive and prognostic power for metastatic spread into the liver
Specific molecular biological characteristics of corresponding BC subtypes (hormone receptor status, morphology, etc.) are relevant for metastases latency i.e. early versus late occurrence of eventual MD. The typical example is oestrogen/progesterone receptor positive BC with 5 years and much longer metastatic latency compared to triple-negative BC with an early onset of more aggressive MD [95]. This subtype-specificity of BC MD consequently indicates substantial differences in corresponding biomarker-panels characteristic for individual subtypes.
Innovative multilevel diagnostics procuring specific panels of validated biomarkers for BC predisposition, development and progression into MD has been proposed [96]. Thereby, creation of a patient specific “molecular portrait” is an essential part of the overall diagnostic strategy. Contextually, analysis of the disease/stage specific molecular patterns in circulating leukocytes as the minimally invasive diagnostic tool followed by a construction of diagnostic windows based on individual patient profiling is highly recommended for BC patient cohort. To this end, the panel of functional groups of proteins involved in BC related molecular mechanisms has been published [96]. This approach has been, further, demonstrated as clinically useful [97].
Claudin-2 is overexpressed by BC cells preferentially in the liver metastatic spread as compared to all other sites [98] that indicates its high organ specificity. Claudin-2 is involved in cell adhesion and matrix remodelling in the liver metastases; it mediates cell–cell interactions between BC cells and hepatocytes leading to induction of c-Met (specific receptor of the tyrosine kinase) and stimulates metastatic progress in the liver [4].
WNT pathways regulate major events in cancer such as tumour initiation, cell migration/invasion, epithelial mesenchymal transition, angiogenesis, lymphangiogenesis, and impaired wound healing [99–101]. The effects on signalling and invasion of β-catenin-independent WNT signalling via the alternative WNT receptor ROR (ROR1/ROR2) have been contextually analysed. ROR1/ROR2 belongs to the receptor tyrosine kinases and is activated by the binding of WNT5a [102, 103]. WNT5a/b and ROR1/ROR2 are overexpressed while WNT/c-Jun is activated [104]. An activation of the kinase domain leads to Jun-N-terminal kinase (JNK) and subsequent c-Jun activation that might be prognostic for breast cancer MD. In contrast, expression patterns of PGR and ER analysed by taking biopsy lose any prognostic power for the liver metastasis after the resection. The proliferation index Ki67 is prognostic in both the primary tumour and liver metastasis. β-catenin-independent WNT score gains prognostic impact in the metastatic tissue of the liver, which may imply adaptation mechanisms triggered by tumour cells during metastatic progression and effective nesting within the host microenvironment [104].
Liver metastases spread specifically by prostate cancer
Incidence and particularities
A number of studies reveal the occurrence of prostate cancer (PC) in 30 % of the men above 50 years of age [105]. Although only 9 % of them develop clinical disease, PC remains the second leading cause of cancer deaths in men in Europe and USA [105, 106], due to PC MD. In particular, PC stage IV is characterised by metastases beyond the seminal vesicles and spread to distant organs [107]. Although bones are the most frequent metastatic site for PC, an autopsy study of 1589 patients reported 25 % of all cases demonstrating the liver metastases, seen most frequently for primary tumours over 8 cm in diameter [105]. PC is more common in males with a strong family history of the disease indicating the role of a genetic component. Further, smokers, black males, and patients consuming a diet high in animal fat or in chromium are at increased risk for PC. Additionally, PC is more aggressive in black males as they are found with a higher tumour grade at the time of diagnosis [108, 109].
PC specific biomarker panels with predictive and prognostic power for metastatic spread into the liver
Serum cytokines have been shown to mediate systemic immunosuppression in men with PC and visceral metastases [110]. IL-6 is the most extensively investigated player directly secreted from prostate tumour cells as well as from macrophages and other cells within the tumour microenvironment [111]. One of the major functions of IL-6 is to steer the adaptive immune response away from a tumouricidal T-helper response and towards an immune response associated with chronic inflammation and tumour growth promotion [111, 112]. Tumour necrosis factor alpha (TNFA) is another systemic pro-inflammatory cytokine associated with a kind of chronic inflammation that promotes tumour growth [113]. The third cytokine potentially involved in the association between visceral metastases and poor responsiveness of PC patients to immunotherapy is IL-8 (a pleotropic cytokine produced by several cell types), which has a well-documented role in neutrophil recruitment. Moreover, binding of IL-8 to specific receptors of endothelial cells has been associated with angiogenesis [114, 115].
Androgen-Deprivation Therapy (ADT) is generally recommended as the initial treatment for metastatic PC. For advanced PC (with a higher volume), ADT is combined with chemotherapy [107]. In the PC group with visceral metastases receiving prednisone alone, the overall survival (OS) is reported to be 8.3 months. Thereby, the liver metastases were associated with particularly poor outcomes and OS recorded by 6.7 months in patients who received abiraterone acetate (AA) over prednisone [116]. Analyses show that second-line hormonal therapy is a reasonable option for men with Castration Resistant Prostate Cancer (CRPC) and visceral metastases. In addition, PC metastasising to the liver is reported as being more lethal than PC metastasising to the bone [110]. Further, docetaxel treatment of PC appears to provide clinical benefits to the patients both with and without visceral MD increasing the OS by 2–3 months.
Immunohistochemical studies analysing the role of antiapoptotic pathways in the pathophysiology of PC show that soft tissue metastases are more likely to express nuclear survivin than the bone metastases [110]. Soft-tissue lesions derived from the liver and lymph nodes express an angiogenic patterns different from that of bone metastases, with a significant relative overexpression of the proangiogenic factor angiopoietin-2. On a systemic level, serum cytokine panels are found to possess a prognostic power being evidently associated with the liver MD progression [110].
If given enough time, most patients with MD may become resistant to androgen ablation. The median survival in patients with PSA level >4 ng/mL was found to be 13 months [117]. In a study on higher serum concentrations of C-reactive protein, it has been found that inflammation may have a crucial role in advancing the PC [118]. Thereby, C-reactive protein is a readily measurable biomarker with a potential to enhance the power of corresponding prognostic models that should be, further, validated in a prospective clinical trial [118].
Conclusions
Multilevel diagnostics may procure specific panels of validated biomarkers for predisposition, development and progression of MD. Highly innovative approaches consider a variety of suboptimal health conditions creating “fertile” microenvironment and pre-metastatic niches which may effectively support MD systemically [3, 119, 120]. Creation of the patient specific “molecular portrait” is an essential part of the improved diagnostic strategy. Contextually, analysis of molecular and cellular pathology/stage specific patterns in blood samples as the minimally invasive diagnostic tool and construction of diagnostic windows based on individual patient profiling is highly recommended for patient cohorts predisposed to and affected by the liver MD. Summarised information relevant for risk assessment, predictive and prognostic biomarker panels specific for the liver MD in colorectal, breast and prostate cancers is provided in Table 2.
References
Chambers AF, Groom AC, MacDonald IC (2002) Metastasis: dissemination and growth of cancer cells in metastatic sites. Nat Rev Cancer 2:563–572. doi:10.1038/nrc865
Zhang XH-F, Giuliano M, Trivedi MV, Schiff R, Osborne CK (2013) Metastasis dormancy in estrogen receptor-positive breast cancer. Clin Cancer Res 19:6389–6397. doi:10.1158/1078-0432.CCR-13-0838
Golubnitschaja O, Debald M, Yeghiazaryan K, Kuhn W, Pešta M, Costigliola V, Grech G (2016) Breast cancer epidemic in the early 21st century: evaluation of risk factors, cumulative questionnaires and recommendations for preventive measures. Tumor Biol. doi:10.1007/s13277-016-5168-x
Obenauf AC, Massagué J (2015) Surviving at a distance: organ-specific metastasis. Trends Cancer 1:76–91. doi:10.1016/j.trecan.2015.07.009
Ananthakrishnan A, Gogineni V, Saeian K (2006) Epidemiology of primary and secondary liver cancers. Semin Interv Radiol 23:47–63. doi:10.1055/s-2006-939841
Disibio G, French SW (2008) Metastatic patterns of cancers: results from a large autopsy study. Arch Pathol Lab Med 132:931–939. doi:10.1043/1543-2165(2008)132[931:MPOCRF]2.0.CO;2
Abraham J-A, Golubnitschaja O (2016) Time for paradigm change in management of hepatocellular carcinoma: is personalised approach in horizon? Pers Med. doi:10.2217/pme-2016-0013
Abraham J-A, Yeghiazaryan K, Golubnitschaja O (2016) Selective internal radiation therapy in treatment of hepatocellular carcinoma: new concepts of personalisation. Pers Med 13(4):347–360. doi:10.2217/pme-2016-0014
K-M Rau H-YK (2005) The mechanisms and managements of hormone-therapy resistance in breast and prostate cancers. Endocr Relat Cancer 12:511–532. doi:10.1677/erc.1.01026
Morgan-Parkes JH (1995) Metastases: mechanisms, pathways, and cascades. Am J Roentgenol 164:1075–1082. doi:10.2214/ajr.164.5.7717206
Sullivan WJ, Christofk HR (2015) The metabolic milieu of metastases. Cell 160:363–364. doi:10.1016/j.cell.2015.01.023
Miller MC, Doyle GV, Terstappen LWMM, Miller MC, Doyle GV, Terstappen LWMM (2010) Significance of circulating tumor cells detected by the cell search system in patients with metastatic breast colorectal and prostate cancer. J Oncol 2010:e617421. doi:10.1155/2010/617421
Redig AJ, McAllister SS (2013) Breast cancer as a systemic disease: a view of metastasis. J Intern Med 274:113–126. doi:10.1111/joim.12084
Elkabets M, Gifford AM, Scheel C, Nilsson B, Reinhardt F, Bray M-A, Carpenter AE, Jirström K, Magnusson K, Ebert BL, Pontén F, Weinberg RA, McAllister SS (2011) Human tumors instigate granulin-expressing hematopoietic cells that promote malignancy by activating stromal fibroblasts in mice. J Clin Invest 121:784–799. doi:10.1172/JCI43757
Kuznetsov HS, Marsh T, Markens BA, Castaño Z, Greene-Colozzi A, Hay SA, Brown VE, Richardson AL, Signoretti S, Battinelli EM, McAllister SS (2012) Identification of luminal breast cancers that establish a tumor-supportive macroenvironment defined by proangiogenic platelets and bone marrow-derived cells. Cancer Discov 2:1150–1165. doi:10.1158/2159-8290.CD-12-0216
McAllister SS, Gifford AM, Greiner AL, Kelleher SP, Saelzler MP, Ince TA, Reinhardt F, Harris LN, Hylander BL, Repasky EA, Weinberg RA (2008) Systemic endocrine instigation of indolent tumor growth requires osteopontin. Cell 133:994–1005. doi:10.1016/j.cell.2008.04.045
Bidard F-C, Peeters DJ, Fehm T, Nolé F, Gisbert-Criado R, Mavroudis D, Grisanti S, Generali D, Garcia-Saenz JA, Stebbing J, Caldas C, Gazzaniga P, Manso L, Zamarchi R, de Lascoiti AF, De Mattos-Arruda L, Ignatiadis M, Lebofsky R, van Laere SJ, Meier-Stiegen F, Sandri M-T, Vidal-Martinez J, Politaki E, Consoli F, Bottini A, Diaz-Rubio E, Krell J, Dawson S-J, Raimondi C, Rutten A, Janni W, Munzone E, Carañana V, Agelaki S, Almici C, Dirix L, Solomayer E-F, Zorzino L, Johannes H, Reis-Filho JS, Pantel K, Pierga J-Y, Michiels S (2014) Clinical validity of circulating tumour cells in patients with metastatic breast cancer: a pooled analysis of individual patient data. Lancet Oncol 15:406–414. doi:10.1016/S1470-2045(14)70069-5
Hoon DSB, Kitago M, Kim J, Mori T, Piris A, Szyfelbein K, Mihm MC, Nathanson SD, Padera TP, Chambers AF, Vantyghem SA, MacDonald IC, Shivers SC, Alsarraj M, Reintgen DS, Passlick B, Sienel W, Pantel K (2006) Molecular mechanisms of metastasis. Cancer Metastasis Rev 25:203–220. doi:10.1007/s10555-006-8500-x
Hüsemann Y, Geigl JB, Schubert F, Musiani P, Meyer M, Burghart E, Forni G, Eils R, Fehm T, Riethmüller G, Klein CA (2008) Systemic spread is an early step in breast cancer. Cancer Cell 13:58–68. doi:10.1016/j.ccr.2007.12.003
Diel IJ, Kaufmann M, Costa SD, Holle R, von Minckwitz G, Solomayer EF, Kaul S, Bastert G (1996) Micrometastatic breast cancer cells in bone marrow at primary surgery: prognostic value in comparison with nodal status. J Natl Cancer Inst 88:1652–1658
Solomayer EF, Diel IJ, Krempien B, Meyberg GC, Gollan C, Krainick U, Wallwiener D, Bastert G (1998) Results of iliac crest biopsies taken from 1465 patients with primary breast cancer. J Cancer Res Clin Oncol 124:44–48
Leary RJ, Sausen M, Kinde I, Papadopoulos N, Carpten JD, Craig D, O’Shaughnessy J, Kinzler KW, Parmigiani G, Vogelstein B, Diaz LA, Velculescu VE (2012) Detection of chromosomal alterations in the circulation of cancer patients with whole-genome sequencing. Sci Transl Med 4:162ra154. doi:10.1126/scitranslmed.3004742
Giuliano M, Giordano A, Jackson S, De Giorgi U, Mego M, Cohen EN, Gao H, Anfossi S, Handy BC, Ueno NT, Alvarez RH, De Placido S, Valero V, Hortobagyi GN, Reuben JM, Cristofanilli M (2014) Circulating tumor cells as early predictors of metastatic spread in breast cancer patients with limited metastatic dissemination. Breast Cancer Res 16:440. doi:10.1186/s13058-014-0440-8
Smerage JB, Barlow WE, Hortobagyi GN, Winer EP, Leyland-Jones B, Srkalovic G, Tejwani S, Schott AF, O’Rourke MA, Lew DL, Doyle GV, Gralow JR, Livingston RB, Hayes DF (2014) Circulating tumor cells and response to chemotherapy in metastatic breast cancer: SWOG S0500. J Clin Oncol 32:3483–3489. doi:10.1200/JCO.2014.56.2561
de Bono JS, Scher HI, Montgomery RB, Parker C, Miller MC, Tissing H, Doyle GV, Terstappen LWWM, Pienta KJ, Raghavan D (2008) Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin Cancer Res 14:6302–6309. doi:10.1158/1078-0432.CCR-08-0872
Hu B, Rochefort H, Goldkorn A (2013) Circulating tumor cells in prostate cancer. Cancers 5:1676–1690. doi:10.3390/cancers5041676
Seeberg LT, Waage A, Brunborg C, Hugenschmidt H, Renolen A, Stav I, Bjørnbeth BA, Brudvik KW, Borgen EF, Naume B, Wiedswang G (2015) Circulating tumor cells in patients with colorectal liver metastasis predict impaired survival. Ann Surg 261:164–171. doi:10.1097/SLA.0000000000000580
Fleischhacker M, Schmidt B (2015) Extracellular Nucleic Acids and Cancer. In: Circulating nucleic acids in early diagnosis, prognosis and treatment monitoring (Ed: Gahan PB), Book-Series: Advances in predictive, preventive and personalised medicine (Ed.: Golubnitschaja O), Springer, Dordrecht, V.5, ISBN 978-94-017-9167-0
Gupta GP, Minn AJ, Kang Y, Siegel PM, Serganova I, Cordón-Cardo C, Olshen AB, Gerald WL, Massagué J (2005) Identifying site-specific metastasis genes and functions. Cold Spring Harb Symp Quant Biol 70:149–158. doi:10.1101/sqb.2005.70.018
Denève E, Riethdorf S, Ramos J, Nocca D, Coffy A, Daurès J-P, Maudelonde T, Fabre J-M, Pantel K, Alix-Panabières C (2013) Capture of viable circulating tumor cells in the liver of colorectal cancer patients. Clin Chem 59:1384–1392. doi:10.1373/clinchem.2013.202846
Singh AD, Bergman L, Seregard S (2005) Uveal melanoma: epidemiologic aspects. Ophthalmol Clin 18:75–84. doi:10.1016/j.ohc.2004.07.002
Costa-Silva B, Aiello NM, Ocean AJ, Singh S, Zhang H, Thakur BK, Becker A, Hoshino A, Mark MT, Molina H, Xiang J, Zhang T, Theilen T-M, García-Santos G, Williams C, Ararso Y, Huang Y, Rodrigues G, Shen T-L, Labori KJ, Lothe IMB, Kure EH, Hernandez J, Doussot A, Ebbesen SH, Grandgenett PM, Hollingsworth MA, Jain M, Mallya K, Batra SK, Jarnagin WR, Schwartz RE, Matei I, Peinado H, Stanger BZ, Bromberg J, Lyden D (2015) Pancreatic cancer exosomes initiate pre-metastatic niche formation in the liver. Nat Cell Biol 17:816–826. doi:10.1038/ncb3169
Bao S, Ouyang G, Bai X, Huang Z, Ma C, Liu M, Shao R, Anderson RM, Rich JN, Wang X-F (2004) Periostin potently promotes metastatic growth of colon cancer by augmenting cell survival via the Akt/PKB pathway. Cancer Cell 5:329–339. doi:10.1016/S1535-6108(04)00081-9
Loo JM, Scherl A, Nguyen A, Man FY, Weinberg E, Zeng Z, Saltz L, Paty PB, Tavazoie SF (2015) Extracellular metabolic energetics can promote cancer progression. Cell 160:393–406. doi:10.1016/j.cell.2014.12.018
Vidal-Vanaclocha F (2011) The Tumor Microenvironment at Different Stages of Hepatic Metastasis. In: Brodt P (ed) Liver Metastasis Biol. Clin. Manag. Springer Netherlands, pp 43–87
Takeda A, Stoeltzing O, Ahmad SA, Reinmuth N, Liu W, Parikh A, Fan F, Akagi M, Ellis LM (2002) Role of angiogenesis in the development and growth of liver metastasis. Ann Surg Oncol 9:610–616
Bramhall SR, Gur U, Coldham C, Gunson BK, Mayer AD, McMaster P, Candinas D, Buckels JAC, Mirza DF (2003) Liver resection for colorectal metastases. Ann R Coll Surg Engl 85:334–339. doi:10.1308/003588403769162468
Abbas S, Lam V, Hollands M (2011) Ten-year survival after liver resection for colorectal metastases: systematic review and meta-analysis. ISRN Oncol 2011:763245. doi:10.5402/2011/763245
Choti MA, Sitzmann JV, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD, Lillemoe KD, Yeo CJ, Cameron JL (2002) Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg 235:759–766
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230:309–318
Nordlinger B, Van Cutsem E, Rougier P, Köhne C-H, Ychou M, Sobrero A, Adam R, Arvidsson D, Carrato A, Georgoulias V, Giuliante F, Glimelius B, Golling M, Gruenberger T, Tabernero J, Wasan H, Poston G, European Colorectal Metastases Treatment Group (2007) Does chemotherapy prior to liver resection increase the potential for cure in patients with metastatic colorectal cancer? A report from the European colorectal metastases treatment group. Eur J Cancer Oxf Engl 1990 43:2037–2045. doi:10.1016/j.ejca.2007.07.017
van Dam RM, Lodewick TM, van den Broek MAJ, de Jong MC, Greve JW, Jansen RLH, Bemelmans MHA, Neumann UP, Olde Damink SWM, Dejong CHC (2014) Outcomes of extended versus limited indications for patients undergoing a liver resection for colorectal cancer liver metastases. HPB 16:550–559. doi:10.1111/hpb.12181
Mattar RE, Al-alem F, Simoneau E, Hassanain M (2016) Preoperative selection of patients with colorectal cancer liver metastasis for hepatic resection. World J Gastroenterol 22:567–581. doi:10.3748/wjg.v22.i2.567
Nakamura S, Suzuki S, Konno H (1999) Resection of hepatic metastases of colorectal carcinoma: 20 years’ experience. J Hepatobiliary Pancreat Surg 6:16–22
Suzuki S, Sakaguchi T, Yokoi Y, Kurachi K, Okamoto K, Okumura T, Tsuchiya Y, Nakamura T, Konno H, Baba S, Nakamura S (2001) Impact of repeat hepatectomy on recurrent colorectal liver metastases. Surgery 129:421–428. doi:10.1067/msy.2001.112486
Malafosse R, Penna C, Sa Cunha A, Nordlinger B (2001) Surgical management of hepatic metastases from colorectal malignancies. Ann Oncol Off J Eur Soc Med Oncol ESMO 12:887–894
Assumpcao L, Choti MA, Gleisner A et al (2008) Patterns of recurrence following liver resection for colorectal metastases: effect of primary rectal tumor site. Arch Surg 143:743–749. doi:10.1001/archsurg.143.8.743
Mullen JT, Ribero D, Reddy SK, Donadon M, Zorzi D, Gautam S, Abdalla EK, Curley SA, Capussotti L, Clary BM, Vauthey J-N (2007) Hepatic insufficiency and mortality in 1059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg 204:854–862. doi:10.1016/j.jamcollsurg.2006.12.032
Abdalla EK, Denys A, Chevalier P, Nemr RA, Vauthey J-N (2004) Total and segmental liver volume variations: implications for liver surgery. Surgery 135:404–410. doi:10.1016/j.surg.2003.08.024
Abdalla EK, Hicks ME, Vauthey JN (2001) Portal vein embolization: rationale, technique and future prospects. Br J Surg 88:165–175. doi:10.1046/j.1365-2168.2001.01658.x
Vauthey J-N, Pawlik TM, Abdalla EK, Arens JF, Nemr RA, Wei SH, Kennamer DL, Ellis LM, Curley SA (2004) Is extended hepatectomy for hepatobiliary malignancy justified? Ann Surg 239:722–732. doi:10.1097/01.sla.0000124385.83887.d5
Behrns KE, Tsiotos GG, DeSouza NF, Krishna MK, Ludwig J, Nagorney DM (1998) Hepatic steatosis as a potential risk factor for major hepatic resection. J Gastrointest Surg Off J Soc Surg Aliment Tract 2:292–298
Neal CP, Mann CD, Pointen E, McGregor A, Garcea G, Metcalfe MS, Berry DP, Dennison AR (2012) Influence of hepatic parenchymal histology on outcome following right hepatic trisectionectomy. J Gastrointest Surg Off J Soc Surg Aliment Tract 16:2064–2073. doi:10.1007/s11605-012-2008-1
Reddy SK, Marsh JW, Varley PR, Mock BK, Chopra KB, Geller DA, Tsung A (2012) Underlying steatohepatitis, but not simple hepatic steatosis, increases morbidity after liver resection: a case-control study. Hepatol Baltim Md 56:2221–2230. doi:10.1002/hep.25935
Vauthey J-N, Pawlik TM, Ribero D, Wu T-T, Zorzi D, Hoff PM, Xiong HQ, Eng C, Lauwers GY, Mino-Kenudson M, Risio M, Muratore A, Capussotti L, Curley SA, Abdalla EK (2006) Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol Off J Am Soc Clin Oncol 24:2065–2072. doi:10.1200/JCO.2005.05.3074
Fernandez FG, Ritter J, Goodwin JW, Linehan DC, Hawkins WG, Strasberg SM (2005) Effect of steatohepatitis associated with irinotecan or oxaliplatin pretreatment on resectability of hepatic colorectal metastases. J Am Coll Surg 200:845–853. doi:10.1016/j.jamcollsurg.2005.01.024
Zakaria S, Donohue JH, Que FG, Farnell MB, Schleck CD, Ilstrup DM, Nagorney DM (2007) Hepatic resection for colorectal metastases. Ann Surg 246:183–191. doi:10.1097/SLA.0b013e3180603039
Leonard GD, Brenner B, Kemeny NE (2005) Neoadjuvant chemotherapy before liver resection for patients with unresectable liver metastases from colorectal carcinoma. J Clin Oncol Off J Am Soc Clin Oncol 23:2038–2048. doi:10.1200/JCO.2005.00.349
Lehmann K, Rickenbacher A, Weber A, Pestalozzi BC, Clavien P-A (2012) Chemotherapy before liver resection of colorectal metastases: friend or foe? Ann Surg 255:237–247. doi:10.1097/SLA.0b013e3182356236
Pessaux P, Chenard M-P, Bachellier P, Jaeck D (2010) Consequences of chemotherapy on resection of colorectal liver metastases. J Visc Surg 147:e193–e201. doi:10.1016/j.jviscsurg.2010.06.004
Wang C-C, Li J (2012) An update on chemotherapy of colorectal liver metastases. World J Gastroenterol WJG 18:25–33. doi:10.3748/wjg.v18.i1.25
Alberts SR, Horvath WL, Sternfeld WC, Goldberg RM, Mahoney MR, Dakhil SR, Levitt R, Rowland K, Nair S, Sargent DJ, Donohue JH (2005) Oxaliplatin, fluorouracil, and leucovorin for patients with unresectable liver-only metastases from colorectal cancer: a north central cancer treatment group phase II study. J Clin Oncol Off J Am Soc Clin Oncol 23:9243–9249. doi:10.1200/JCO.2005.07.740
Bismuth H, Adam R, Lévi F, Farabos C, Waechter F, Castaing D, Majno P, Engerran L (1996) Resection of nonresectable liver metastases from colorectal cancer after neoadjuvant chemotherapy. Ann Surg 224:509–522
Khatri VP, Chee KG, Petrelli NJ (2007) Modern multimodality approach to hepatic colorectal metastases: solutions and controversies. Surg Oncol 16:71–83. doi:10.1016/j.suronc.2007.05.001
Adam R, Delvart V, Pascal G, Valeanu A, Castaing D, Azoulay D, Giacchetti S, Paule B, Kunstlinger F, Ghémard O, Levi F, Bismuth H (2004) Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy. Ann Surg 240:644–658. doi:10.1097/01.sla.0000141198.92114.f6
Golubnitschaja O, Cebioglu M, Yeghiazaryan K, Pieper CC, Schild HH (2014) “Molecular signature” in blood of liver cancer diagnosed patients as a criterion for optimal therapy modalities. EPMA J 5:A38. doi:10.1186/1878-5085-5-S1-A38
De Rosa M, Pace U, Rega D, Costabile V, Duraturo F, Izzo P, Delrio P (2015) Genetics, diagnosis and management of colorectal cancer (review). Oncol Rep 34:1087–1096. doi:10.3892/or.2015.4108
Manfredi S, Lepage C, Hatem C, Coatmeur O, Faivre J, Bouvier A-M (2006) Epidemiology and Management of Liver Metastases From Colorectal Cancer. Ann Surg 244:254–259. doi:10.1097/01.sla.0000217629.94941.cf
Risbridger GP, Davis ID, Birrell SN, Tilley WD (2010) Breast and prostate cancer: more similar than different. Nat Rev Cancer 10:205–212. doi:10.1038/nrc2795
Auguste P, Fallavollita L, Wang N, Burnier J, Bikfalvi A, Brodt P (2007) The host inflammatory response promotes liver metastasis by increasing tumor cell arrest and extravasation. Am J Pathol 170:1781–1792. doi:10.2353/ajpath.2007.060886
Khatib A-M, Auguste P, Fallavollita L, Wang N, Samani A, Kontogiannea M, Meterissian S, Brodt P (2005) Characterization of the host proinflammatory response to tumor cells during the initial stages of liver metastasis. Am J Pathol 167:749–759. doi:10.1016/S0002-9440(10)62048-2
Gout S, Huot J (2008) Role of cancer microenvironment in metastasis: focus on colon cancer. Cancer Microenviron 1:69–83. doi:10.1007/s12307-008-0007-2
Yim K-L (2011) Microsatellite instability in metastatic colorectal cancer: a review of pathology, response to chemotherapy and clinical outcome. Med Oncol 29:1796–1801. doi:10.1007/s12032-011-0050-6
Zong Z, Zhou T, Rao L, Jiang Z, Li Y, Hou Z, Yang B, Han F, Chen S (2016) Musashi2 as a novel predictive biomarker for liver metastasis and poor prognosis in colorectal cancer. Cancer Med. doi:10.1002/cam4.624
Ito T, Kwon HY, Zimdahl B, Congdon KL, Blum J, Lento WE, Zhao C, Lagoo A, Gerrard G, Foroni L, Goldman J, Goh H, Kim S-H, Kim D-W, Chuah C, Oehler VG, Radich JP, Jordan CT, Reya T (2010) Regulation of myeloid leukaemia by the cell-fate determinant Musashi. Nature 466:765–768. doi:10.1038/nature09171
Watanabe M, Ohnishi Y, Inoue H, Wato M, Tanaka A, Kakudo K, Nozaki M (2014) NANOG expression correlates with differentiation, metastasis and resistance to preoperative adjuvant therapy in oral squamous cell carcinoma. Oncol Lett 7:35–40. doi:10.3892/ol.2013.1690
Xu F, Dai C, Zhang R, Zhao Y, Peng S, Jia C (2012) Nanog: A Potential Biomarker for Liver Metastasis of Colorectal Cancer. Dig Dis Sci 57:2340–2346. doi:10.1007/s10620-012-2182-8
Bröker MEE, Lalmahomed ZS, Roest HP, van Huizen NA, Dekker LJM, Calame W, Verhoef C, IJzermans JNM, Luider TM (2013) Collagen peptides in urine: a new promising biomarker for the detection of colorectal liver metastases. PLoS One 8:e70918. doi:10.1371/journal.pone.0070918
Colussi D, Brandi G, Bazzoli F, Ricciardiello L (2013) Molecular pathways involved in colorectal cancer: implications for disease behavior and prevention. Int J Mol Sci 14:16365–16385. doi:10.3390/ijms140816365
Karnes WE, Shattuck-Brandt R, Burgart LJ, DuBois RN, Tester DJ, Cunningham JM, Kim CY, McDonnell SK, Schaid DJ, Thibodeau SN (1998) Reduced COX-2 protein in colorectal cancer with defective mismatch repair. Cancer Res 58:5473–5477
Ogino S, Brahmandam M, Kawasaki T, Kirkner GJ, Loda M, Fuchs CS (2006) Combined analysis of COX-2 and p53 expressions reveals synergistic inverse correlations with microsatellite instability and CpG Island methylator phenotype in colorectal cancer. Neoplasia 8:458–464
Burk U, Schubert J, Wellner U, Schmalhofer O, Vincan E, Spaderna S, Brabletz T (2008) A reciprocal repression between ZEB1 and members of the miR-200 family promotes EMT and invasion in cancer cells. EMBO Rep 9:582–589. doi:10.1038/embor.2008.74
Wellner U, Schubert J, Burk UC, Schmalhofer O, Zhu F, Sonntag A, Waldvogel B, Vannier C, Darling D, zur Hausen A, Brunton VG, Morton J, Sansom O, Schüler J, Stemmler MP, Herzberger C, Hopt U, Keck T, Brabletz S, Brabletz T (2009) The EMT-activator ZEB1 promotes tumorigenicity by repressing stemness-inhibiting microRNAs. Nat Cell Biol 11:1487–1495. doi:10.1038/ncb1998
Toiyama Y, Hur K, Tanaka K, Inoue Y, Kusunoki M, Boland CR, Goel A (2014) Serum miR-200c is a novel prognostic and metastasis-predictive biomarker in patients with colorectal cancer. Ann Surg 259:735–743. doi:10.1097/SLA.0b013e3182a6909d
Hur K, Toiyama Y, Takahashi M, Balaguer F, Nagasaka T, Koike J, Hemmi H, Koi M, Boland CR, Goel A (2013) MicroRNA-200c modulates epithelial-to-mesenchymal transition (EMT) in human colorectal cancer metastasis. Gut 62:1315–1326. doi:10.1136/gutjnl-2011-301846
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108. doi:10.3322/caac.21262
Ekwueme DU, Guy GP, Rim SH, White A, Hall IJ, Fairley TL, Dean HD (2014) Health and economic impact of breast cancer mortality in young women, 1970–2008. Am J Prev Med 46:71–79. doi:10.1016/j.amepre.2013.08.016
Golubnitschaja O, Yeghiazaryan K, Stricker H, Trog D, Schild HH, Berliner L (2016) Patients with hepatic breast cancer metastases demonstrate highly specific profiles of matrix metalloproteinases MMP-2 and MMP-9 after SIRT treatment as compared to other primary and secondary liver tumours. BMC Cancer 16(1):357. doi:10.1186/s12885-016-2382-2
Tampellini M, Berruti A, Gerbino A, Buniva T, Torta M, Gorzegno G, Faggiuolo R, Cannone R, Farris A, Destefanis M, Moro G, Deltetto F, Dogliotti L (1997) Relationship between CA 15-3 serum levels and disease extent in predicting overall survival of breast cancer patients with newly diagnosed metastatic disease. Br J Cancer 75:698–702
Makki J (2015) Diversity of breast carcinoma: histological subtypes and clinical relevance. Clin Med Insights Pathol 8:23–31. doi:10.4137/CPath.S31563
Weigelt B, Peterse JL, van’t Veer LJ (2005) Breast cancer metastasis: markers and models. Nat Rev Cancer 5:591–602. doi:10.1038/nrc1670
Osman MA, Hennessy BT (2015) Obesity correlation with metastases development and response to first-line metastatic chemotherapy in breast cancer. Clin Med Insights Oncol 9:105–112. doi:10.4137/CMO.S32812
Chan DSM, Vieira AR, Aune D, Bandera EV, Greenwood DC, McTiernan A, Navarro Rosenblatt D, Thune I, Vieira R, Norat T (2014) Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol Off J Eur Soc Med Oncol ESMO 25:1901–1914. doi:10.1093/annonc/mdu042
Weinrich M, Weiß Christel, Schuld J, Rau BM (2014) Liver resections of isolated liver metastasis in breast cancer: results and possible prognostic factors. HPB Surg 2014:e893829. doi:10.1155/2014/893829
Girotra S, Yeghiazaryan K, Golubnitschaja O (2016) Potential biomarker panels in overall breast cancer management: advancements by multi-level diagnostics. Pers Med. doi:10.2217/pme-2016-0020
Golubnitschaja O, Yeghiazaryan K, Costigliola V, Trog D, Braun M, Debald M, Kuhn W, Schild HH (2013) Risk assessment, disease prevention and personalised treatments in breast cancer: is clinically qualified integrative approach in the horizon? EPMA J 4:6. doi:10.1186/1878-5085-4-6
Debald M, Yeghiazaryan K, Cebioglu M, Kuhn W, Schild HH, Golubnitschaja O (2013) “Suspect molecular signature” in blood as the indicator of undiagnosed breast cancer, cancer risk and targeted prevention. EPMA J 4:22. doi:10.1186/1878-5085-4-22
Kimbung S, Kovács A, Bendahl P-O, Malmström P, Fernö M, Hatschek T, Hedenfalk I (2014) Claudin-2 is an independent negative prognostic factor in breast cancer and specifically predicts early liver recurrences. Mol Oncol 8:119–128. doi:10.1016/j.molonc.2013.10.002
Clevers H, Loh KM, Nusse R (2014) Stem cell signaling. An integral program for tissue renewal and regeneration: wnt signaling and stem cell control. Science 346:1248012. doi:10.1126/science.1248012
Nusse R (2012) Wnt signaling. Cold Spring Harb Perspect Biol. doi:10.1101/cshperspect.a011163
Reya T, Clevers H (2005) Wnt signalling in stem cells and cancer. Nature 434:843–850. doi:10.1038/nature03319
Henry C, Quadir A, Hawkins NJ, Jary E, Llamosas E, Kumar D, Daniels B, Ward RL, Ford CE (2015) Expression of the novel Wnt receptor ROR2 is increased in breast cancer and may regulate both β-catenin dependent and independent Wnt signalling. J Cancer Res Clin Oncol 141:243–254. doi:10.1007/s00432-014-1824-y
Zhang S, Chen L, Cui B, Chuang H-Y, Yu J, Wang-Rodriguez J, Tang L, Chen G, Basak GW, Kipps TJ (2012) ROR1 is expressed in human breast cancer and associated with enhanced tumor-cell growth. PLoS One 7:e31127. doi:10.1371/journal.pone.0031127
Bleckmann A, Conradi L-C, Menck K, Schmick NA, Schubert A, Rietkötter E, Arackal J, Middel P, Schambony A, Liersch T, Homayounfar K, Beißbarth T, Klemm F, Binder C, Pukrop T (2016) β-catenin-independent WNT signaling and Ki67 in contrast to the estrogen receptor status are prognostic and associated with poor prognosis in breast cancer liver metastases. Clin Exp Metastasis. doi:10.1007/s10585-016-9780-3
Bubendorf L, Schöpfer A, Wagner U, Sauter G, Moch H, Willi N, Gasser TC, Mihatsch MJ (2000) Metastatic patterns of prostate cancer: an autopsy study of 1589 patients. Hum Pathol 31:578–583
Pouessel D, Gallet B, Bibeau F, Avancès C, Iborra F, Sénesse P, Culine S (2007) Liver metastases in prostate carcinoma: clinical characteristics and outcome. BJU Int 99:807–811. doi:10.1111/j.1464-410X.2006.06663.x
Treatment for advanced prostate cancer. http://www.uptodate.com/contents/treatment-for-advanced-prostate-cancer-beyond-the-basics. Accessed 18 Mar 2016
Fowler JE, Sanders J, Bigler SA, Rigdon J, Kilambi NK, Land SA (2000) Percent free prostate specific antigen and cancer detection in black and white men with total prostate specific antigen 2.5–9.9 ng./ml. J Urol 163:1467–1470
Moul JW, Douglas TH, McCarthy WF, McLeod DG (1996) Black race is an adverse prognostic factor for prostate cancer recurrence following radical prostatectomy in an equal access health care setting. J Urol 155:1667–1673
Drake CG (2014) Visceral metastases and prostate cancer treatment: “die hard”, “tough neighborhoods”, or “evil humors”? Oncol (Williston Park NY) 28:974–980
Weaver CT, Harrington LE, Mangan PR, Gavrieli M, Murphy KM (2006) Th17: an effector CD4 T cell lineage with regulatory T cell ties. Immunity 24:677–688. doi:10.1016/j.immuni.2006.06.002
Azevedo A, Cunha V, Teixeira AL, Medeiros R (2011) IL-6/IL-6R as a potential key signaling pathway in prostate cancer development. World J Clin Oncol 2:384–396. doi:10.5306/wjco.v2.i12.384
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454:436–444. doi:10.1038/nature07205
Yoshimura T, Matsushima K, Tanaka S, Robinson EA, Appella E, Oppenheim JJ, Leonard EJ (1987) Purification of a human monocyte-derived neutrophil chemotactic factor that has peptide sequence similarity to other host defense cytokines. Proc Natl Acad Sci USA 84:9233–9237
Huang S, Mills L, Mian B, Tellez C, McCarty M, Yang X-D, Gudas JM, Bar-Eli M (2002) Fully humanized neutralizing antibodies to interleukin-8 (ABX-IL8) inhibit angiogenesis, tumor growth, and metastasis of human melanoma. Am J Pathol 161:125–134
Goodman OB, Flaig TW, Molina A, Mulders PFA, Fizazi K, Suttmann H, Li J, Kheoh T, de Bono JS, Scher HI (2014) Exploratory analysis of the visceral disease subgroup in a phase III study of abiraterone acetate in metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis 17:34–39. doi:10.1038/pcan.2013.41
Hussain M, Tangen CM, Higano C, Schelhammer PF, Faulkner J, Crawford ED, Wilding G, Akdas A, Small EJ, Donnelly B, MacVicar G, Raghavan D (2006) Absolute prostate-specific antigen value after androgen deprivation is a strong independent predictor of survival in new metastatic prostate cancer: data from Southwest oncology group trial 9346 (INT-0162). J Clin Oncol 24:3984–3990. doi:10.1200/JCO.2006.06.4246
Renee C, Prins BLR (2010) C-reactive protein as an adverse prognostic marker for men with castration-resistant prostate cancer (CRPC): confirmatory results. Urol Oncol 30:33–37. doi:10.1016/j.urolonc.2009.11.012
Cox TR, Rumney RMH, Schoof EM, Perryman L, Høye AM, Agrawal A, Bird D, Latif NA, Forrest H, Evans HR, Huggins ID, Lang G, Linding R, Gartland A, Erler JT (2015) The hypoxic cancer secretome induces pre-metastatic bone lesions through lysyl oxidase. Nature 522(7554):106–110. doi:10.1038/nature14492
Golubnitschaja O, Debald M, Kuhn W, Yeghiazaryan K, Bubnov RV, Goncharenko VM, Lushchyk U, Grech G, Konieczka K (2016) Flammer syndrome and potential formation of pre-metastatic niches: a multi-centred study on phenotyping, patient stratification, prediction and potential prevention of aggressive breast cancer and metastatic disease. EPMA J 7(Suppl 1):A25
Acknowledgments
Krishna Chander Sridhar has been awarded by the European Association for Predictive, Preventive and Personalised Medicine (EPMA) for the best presentation to the topic at the Workshop of Young Professionals, EPMA World Congress 2015, Bonn, Germany. More information is provided here www.epmanet.eu.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Golubnitschaja, O., Sridhar, K.C. Liver metastatic disease: new concepts and biomarker panels to improve individual outcomes. Clin Exp Metastasis 33, 743–755 (2016). https://doi.org/10.1007/s10585-016-9816-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-016-9816-8