Abstract
The clinical significance of circulating follistatin (FLST), an inhibitor of the multifunctional cytokine activin A (Act A), was investigated in patients with prostate cancer (PCa). The serum concentrations of this molecule were determined by an enzyme-linked immunosorbent assay (ELISA) in PCa patients with (M+) or without (M0) bone metastases, in patients with benign prostate hyperplasia (BPH) and in healthy subjects (HS). The effectiveness of FLST in detecting PCa patients with skeletal metastases was determined by the receiver operating characteristic (ROC) curve analysis. Serum FLST was significantly higher in PCa patients than in BPH patients (P = 0.001) or HS (P = 0.011). Conversely, in BPH patients, FLST levels resulted lower than in HS (P = 0.025). In cancer patients the serum concentrations of FLST significantly correlated with the presence of bone metastases (P = 0.0005) or increased PSA levels (P = 0.04). Interestingly, significant differences in the ratio between FLST and Act A serum concentrations (FLST/Act A) were observed between HS and BPH patients (P = 0.001) or PCa patients (P = 0.0005). Finally, ROC curve analysis, highlighted a sound diagnostic performance of FLST in detecting M+ patients (P = 0.0001). However, the diagnostic effectiveness of FLST did not result significantly superior to that of Act A or PSA. These findings suggest that FLST may be regarded as a potential, molecular target in the treatment of metastatic bone disease while its clinical role as soluble marker in the clinical management of PCa patients with bone metastases needs to be better defined.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Activin A (Act A) is a multifunctional cytokine of the transforming growth factor-beta (TGF-β) superfamily of growth factors [1]. This molecule appears to be implicated in the regulation of a broad range of important biological processes including cell proliferation, differentiation, apoptosis, immune response, wound healing, embryogenesis, endocrine functions, tissue metabolism and homeostasis [1–3]. The biological activity of activin A is modulated by several endogenous inhibitors including follistatin (FLST), a cystein rich glycosylated polypeptide chain of 31–39 kDa that binds Act A with high affinity (850–500 pM) [1, 3, 4]. Interestingly, growing evidence suggests that the activin–follistatin system (Act/FLST) may have a regulatory function in controlling several physiological and pathological processes [3, 5, 6]. In particular, recent findings indicate that these molecules appear to have a role in the regulation of bone turnover in normal and pathological conditions. To confirm this, several experimental studies provide evidence that the Act/FLST system modulates osteoclast activity, osteoblast formation, cartilage maturation and endochondral bone formation [6–13] and that the balance between these molecules is deregulated in several disorders associated with increased bone degradation [6, 9, 14, 15]. These observations might suggest the possible involvement of FLST, in particular, in the pathogenesis of bone metastasis, a pathological process which is known to be associated with marked disturbances of bone turnover [16]. This hypothesis is corroborated by many observations showing that tumors which preferentially metastasize to the bone including prostate cancer present altered expression levels of FLST [3, 17–26]. Furthermore, the possible correlation between the diffusion of malignant cells into the bone and alteration in the Act A/FLST balance in patients with prostate cancer is further indirectly supported by certain recent studies of ours which demonstrate that the circulating levels of Act A are markedly elevated in these patients and that this phenomenon correlates with the presence and number of skeletal metastases [27]. On the basis of these findings we have undertaken further investigation in order to assess the clinical significance of circulating FLST in PCa patients with bone metastasis and its relationship with Act A.
Patients and methods
These studies were carried out on serum samples, collected between 2004 and 2006, from 35 patients with prostate cancer, 20 patients with histologically proven benign prostatic hyperplasia (BPH) (median age 61.9, range 55–74) and 21 registered male healthy blood donors (HS) who served as control group. The prostate cancer group (PCa) comprised 15 patients with confined disease (M0) and 20 patients with clinically documented bone metastases and no apparent extraskeletal involvement (M+) [27]. The main characteristics of cancer patients are reported in Table 1.
Determination of follistatin serum concentrations
Peripheral venous blood specimen from PCa patients or BPH patients were collected before starting any clinical treatment. The blood was drawn into polycarbonate tubes, allowed to clot at room temperature and then centrifuged at 3,500 rpm for 15 min (Hereus Omnifuge 2.0 RS, Hereus Sepatech). Serum aliquots were stored at −80°C until assays were performed. Total FLST serum concentrations (i.e., FS288, FS300 and FS315 isoforms) was determined by a commercially available two-step sandwich enzyme-linked immunosorbent assay (ELISA) kit (R&D System, Minneapolis USA) in accordance with the manufacturer’s instructions. The reported detection limit was 29 pg/ml (range 10–83 pg/ml). According to the manufacturer, FLST does not cross-react with recombinant human activin A, activin B and activin AB.
Serum activin A and prostate specific antigen (PSA) determinations
Activin A and PSA serum concentrations were previously determined in PCA patients, BPH patients and in HS as described [27]. The reported detection limits were <78 pg/ml for activin A and <0.009 ng/ml for PSA respectively.
Statistical analysis
The D’Agostino–Pearson test was used to assess the normal distribution of the data. Therefore, statistical analysis was performed, where required, by the non parametric Mann–Whitney U test, the Kruskall–Wallis test, the Spearman rank correlation test or the parametric Student t test for independent samples. The diagnostic effectiveness of follistatin, activin A or PSA, alone or in combinations, in discriminating between M0 and M+ patients was determined by the receiver operating characteristic (ROC) curve analysis [28]. The significance of the difference between the areas under the ROC curves (AUCs) was assessed in accordance with Hanley and McNeil [29]. Data analysis was performed by using the Medcalc version 7.4.4 statistical software package (MEDCALC Mariakerke, Belgium). P values < 0.05 were considered statistically significant.
Results
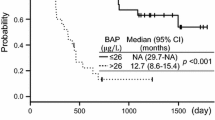
FLST serum levels were higher in PCa patients (mean 2.56 ± 1.5 ng/ml) than in BPH patients (mean 1.5 ± 0.72 ng/ml) or HS (mean 1.70 ± 0.45 ng/ml) or (Fig. 1). Conversely, BPH patients had FLST serum concentrations that were significantly lower than those measured in HS (P = 0.025) (Fig. 1). Interestingly, the ratio between the serum concentrations FLST and Act A (FLST/Act A ratio) was significantly higher in the HS group (mean 5.5 ± 3.3) than in M0 (mean 2.9 ± 1.4) or M+ (2.7 ± 1.2) or BPH patients (mean 2.1 ± 0.9), while no significant difference in this parameter was shown between M0 and M+ patients or between BPH and M0 or M+ patients (Fig. 2). In PCa patients, FLST levels were more elevated in M+ patients (median 2.7 ng/ml) as compared to M0 patients (median 1.75 ng/ml) (Table 1). Moreover, in cancer patients a positive correlation was observed between FLST and Act A or PSA serum concentrations (r = 0.59, P = 0.0013 and r = 0.56, P = 0.024, by the Spearman rank correlation test respectively) while no correlation was shown between serum FLST and Gleason score or extracapsular involvement or lymph node status (Table 1). Lastly, ROC curve generated to assess the effectiveness of FLST in discriminating between M+ and M0 patients showed, in this respect, a good diagnostic performance for this molecule (Fig. 3). However, the AUC of FLST did not significantly differ from that of Act A or PSA (Fig. 3; Table 2). The combination of FLST with Act A or PSA, did not substantially resulted in an improved diagnostic accuracy as compared to that of each single molecule (Fig. 3; Table 2).
Receiver operating characteristic (ROC) curve for follistatin to detect PCa patients with bone metastases. Detailed results of the ROC analysis are given in Table 2
Discussion
Growing evidence suggests that the FLST/Act A system may be implicated in the pathogenesis of metastatic bone disease. This hypothesis is corroborated by several experimental observations which show that the balance between these molecules results deregulated in several pathological conditions associated with an altered bone turnover and in tumors which preferentially metastasize to the bone including prostate cancer [9–15, 17–26, 30–32]. In line with these observations, our data show that the serum levels of FLST are significantly increased in patients with prostate cancer and that the ratio between the serum concentrations of FLST and Act A (FLTS/Act A ratio) in these patients significantly differs from that measured in HS. Moreover, our studies highlight a positive correlation between circulating levels of FLST and the presence of bone metastasis or increased PSA levels. These findings further confirm and add to previous observations by Sardana et al. [26] showing a significant difference in FLST serum concentrations between subjects with or without prostate cancer. Our data are also consistent with those immunohistochemical and molecular biology studies which highlight a positive correlation between altered expression level of FLST in prostate cancer and a more aggressive behaviour of this tumor [22–26, 31–33]. Although these observations reinforce the hypothesis of a possible involvement of FLST in PCa progression, the mechanisms by which this molecule may facilitate, in particular, bone metastasis formation in PCa patients remain to be unravelled. In this regard, some in vitro studies suggest that FLST may foster bone metastasis formation in prostate cancer by modulating the activity of the bone morphogenic protein-7 (BMP-7), a member of the TGF-β family which is critical in the formation of osteoblastic lesions associated with prostate cancer metastases [34–37]. In addition, recent in vitro evidence suggests that FLST may indirectly facilitate bone metastasis formation by inhibiting activin type II receptor (ActRII) mediated signalling pathway [38]. This phenomenon appears to lead to the up-regulation of ADAM-15, a disintegrin which facilitate cell detachment by cleaving integrin molecules and whose overexpression appears to be strongly correlated with prostatic metastasis [39]. Intriguingly, this mechanism has been described as peculiar to prostate cancer and neuroblastoma [38]. Furthermore, experimental evidence suggests that this molecule may also facilitate the diffusion of malignant cells into the bone via the angiogenic route, through the activation of mechanisms which are independent from its Act A or BMPs inhibiting activity. In particular, some of these studies show that, FLST may interact with angiogenin, a 14-kDa protein which exerts its pro angiogenic functions by activating endothelial and smooth muscle cells and which promotes migration, invasion, proliferation and formation of tubular structure [40–43]. Additionally, it has been suggested that FLST, in concert with vascular endothelial growth factor (VEGF), may foster the formation of new blood vessels by stimulating the production of matrix-metalloproteinase-2 (MMP-2), a proteolytic enzyme which has been implicated in tumor angiogenesis and bone metastasis formation in prostate cancer [44–46]. On the other hand, conflicting results have been generated from experimental in vivo studies regarding the promoting activity of FLST on tumor angiogenesis. In fact, Krneta et al. [47] recently showed that FLST may act as a potent angiogenesis stimulator in SCID mice transplanted with R30C human mammary tumor cells. Conversely, Ogino et al. [48] reported that, in NK cell-depleted SCID mice, FLST gene transfection resulted in the suppression of the experimental multiple organ metastases via inhibition of angiogenesis by small cell lung cancer (SCLC) cells. The discrepancies in these results are currently, in part, explained through the use of different animal tumor models and through the different role of the Act A-FLST system in the progression of different tumor types [47–51]. Therefore, further studies are needed to better assess the pro-angiogenetic effects of FLST on human tumors. Finally, ROC curves generated to asses the clinical value of circulating FLST as a gauge of bone metastasis in PCa patients, showed a good diagnostic performance of FLST in this respect. These data are consistent with recent findings from proteomic analysis studies which actually consider FLST as one of the novel candidate biomarkers of certain solid tumors including prostate cancer [25, 26, 49, 52, 53]. However, in our series of patients, the diagnostic performance of FLST did not result significantly superior to that of Act A or PSA. Although these data cast doubt on the specific role of serum FLST as a diagnostic gauge of bone metastasis in PCa patients, they indicate that this molecule may be of potential clinical interest as a circulating biomarker for the therapeutic management and follow-up of these patients when undergoing antimetastatic treatments. In conclusion, in line with other previous observations [47, 54], the present study suggests that, FLST may contribute to foster bone metastasis formation in PCa patients. In this scenario, FLST may be regarded as a new, potential molecular target in the treatment of metastatic bone disease while further investigations with a wider number of subjects is needed to better define the clinical role of this molecule as a biomarker that might be useful in the management of these patients.
Abbreviations
- Act A:
-
Activin A
- ActRII:
-
Activin type II receptor
- AUC:
-
Area under the curve
- BMP-7:
-
Bone morphogenic protein-7
- BPH:
-
Benign prostate hyperplasia
- FLST:
-
Follistatin
- FLST/Act A ratio:
-
Follistatin/Activin A ratio
- ELISA:
-
Enzyme linked immunosorbent assay
- HS:
-
Healthy subjects
- MMP-2:
-
Matrix-metalloproteinase-2
- M0:
-
Patients with confined disease
- M+:
-
Patients with bone metastases
- PCa:
-
Prostate cancer
- PSA:
-
Prostate specific antigen
- ROC curve:
-
Receiver operating characteristic curve
- SCLC:
-
Small cell lung cancer
- TGF-β:
-
Transforming growth factor-beta
- VEGF:
-
Vascular endothelial growth factor
References
Welt C, Sidis Y, Keutmann H, Schneyer A (2002) Activins, inhibins, and follistatins: from endocrinology to signaling. A paradigm for the new millennium. Exp Biol Med 227:724–752
Chen YG, Wang Q, Lin SL et al (2006) Activin signaling and its role in regulation of cell proliferation, apoptosis, and carcinogenesis. Exp Biol Med 231:534–544
Risbridger GP, Schmitt JF, Robertson DM (2001) Activins and inhibins in endocrine and other tumors. Endocr Rev 22(6):836–858
Phillips DJ, de Kretser DM (1998) Follistatin: a multifunctional regulatory protein. Front Neuroendocrinol 19(4):287–322
Aoki F, Kojima I (2007) Therapeutic potential of follistatin to promote tissue regeneration and prevent tissue fibrosis. Endocr J 54(6):849–854
Werner S, Alzheimer C (2006) Roles of activin in tissue repair, fibrosis and inflammatory disease. Cytokine Growth Factor Rev 17(3):157–171
Inoue S, Nomura S, Hosoi T, Ouchi Y, Orimo H, Muramatsu M (1994) Localization of follistatin, an activin-binding protein, in bone tissues. Calcif Tissue Int 55(5):395–397
Funaba M, Ogawa K, Murata T et al (1996) Follistatin and activin in bone: expression and localization during endochondral bone development. Endocrinology 137(10):4250–4259
Eiken M, Swagemakers S, Koedeman M et al (2007) The activin A-follistatin system: potent regulator of human extracellular matrix mineralization. Faseb J 21(11):2949–2960
Tardif G, Pelletier JP, Boileau C, Martel-Pelletier J (2009) The BMP antagonists follistatin and gremlin in normal and early osteoarthritic cartilage: an immunohistochemical study. Osteoarthr Cartil 17(2):263–270
Murase Y, Okahashi N, Koseki T et al (2001) Possible involvement of protein kinases and Smad2 signaling pathways on osteoclast differentiation enhanced by activin A. J Cell Physiol 188(2):236–242
Gaddy-Kurten D, Coker JK, Abe E et al (2002) Inhibin suppresses and activin stimulates osteoblastogenesis and osteoclastogenesis in murine bone marrow cultures. Endocrinology 143(1):74–83
Kawabata N, Kamiya N, Suzuki N et al (2007) Changes in extracellular activin A: follistatin ratio during differentiation of a mesenchymal progenitor cell line ROB.C26 into osteoblasts and adipocytes. Life Sci 81:8–18
Hayashi K, Yamaguchi T, Yano S et al (2009) BMP/Wnt antagonists are upregulated by dexamethasone in osteoblasts and reversed by alendronate and PTH: potential therapeutic targets for glucocorticoid-induced osteoporosis. Biochem Biophys Res Commun 379(2):261–266
Borawski J, Naumnik B, Myśliwiec M (2004) Activin A/follistatin system: another link to heparin-induced osteoporosis? Clin Appl Thromb Hemost 10(2):191–192
Mundy GR (2002) Metastasis to bone: causes, consequences and therapeutic opportunities. Nat Rev Cancer 2:584–593
Kakiuchi S, Daigo Y, Tsunoda T et al (2003) Genome-wide analysis of organ-preferential metastasis of human small cell lung cancer in mice. Mol Cancer Res 1(7):485–499
Kang Y, Siegel PM, Shu W et al (2003) A multigenic program mediating breast cancer metastasis to bone. Cancer Cell 3(6):537–549
Razanajaona D, Joguet S, Ay AS et al (2007) Silencing of FLRG, an antagonist of activin, inhibits human breast tumor cell growth. Cancer Res 67(15):7223–7229
Bloise E, Couto HL, Massai L et al (2009) Differential expression of follistatin and FLRG in human breast proliferative disorders. BMC Cancer 9:320. doi:10.1186/1471-2407-9-320
Thomas TZ, Chapman SM, Hong W et al (1998) Inhibins, activins, and follistatins: expression of mRNAs and cellular localization in tissues from men with benign prostatic hyperplasia. Prostate 34(1):34–43
McPherson SJ, Mellor SL, Wang H et al (1999) Expression of activin A and follistatin core proteins by human prostate tumor cell lines. Endocrinology 140(11):5303–5309
Wang Q, Tabatabaei S, Planz B et al (1999) Identification of an activin–follistatin growth modulatory system in the human prostate: secretion and biological activity in primary cultures of prostatic epithelial cells. J Urol 161(4):1378–1384
Risbridger GP, Mellor SL, McPherson SJ, Schmitt JF (2001) The contribution of inhibins and activins to malignant prostate disease. Mol Cell Endocrinol 180(1–2):149–155
Härkönen P, Törn S, Kurkela R et al (2003) Sex hormone metabolism in prostate cancer cells during transition to an androgen-independent state. J Clin Endocrinol Metab 88(2):705–712
Sardana G, Jung K, Stephan C, Diamandis EP (2008) Proteomic analysis of conditioned media from the PC3, LNCaP, and 22Rv1 prostate cancer cell lines: discovery and validation of candidate prostate cancer biomarkers. J Proteome Res 7(8):3329–3338
Leto G, Incorvaia L, Badalamenti G et al (2006) Activin A circulating levels in patients with bone metastasis from breast or prostate cancer. Clin Exp Metastasis 23(2):117–122
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148:839–884
van Schaik RH, Wierikx CD, Timmerman MA et al (2000) Variations in activin receptor, inhibin/activin subunit and follistatin mRNAs in human prostate tumour tissues. Br J Cancer 82:112–117
Chen Q, Watson JT, Marengo SR et al (2006) Gene expression in the LNCaP human prostate cancer progression model: progression associated expression in vitro corresponds to expression changes associated with prostate cancer progression in vivo. Cancer Lett 244(2):274–288
Vaarala MH, Porvari K, Kyllönen A, Vihko P (2000) Differentially expressed genes in two LNCaP prostate cancer cell lines reflecting changes during prostate cancer progression. Lab Investig 80(8):1259–1266
Fujii Y, Kawakami S, Okada Y et al (2000) Regulation of prostate-specific antigen by activin A in prostate cancer LNCaP cells. Am J Physiol Endocrinol Metab 286(6):E927–E931
Masuda H, Fukabori Y, Nakano K et al (2003) Increased expression of bone morphogenetic protein-7 in bone metastatic prostate cancer. Prostate 54(4):268–274
Buijs JT, Rentsch CA, van der Horst G et al (2007) BMP7, a putative regulator of epithelial homeostasis in the human prostate, is a potent inhibitor of prostate cancer bone metastasis in vivo. Am J Pathol 171(3):1047–1057
Ye L, Lewis-Russell JM, Kynaston H, Jiang WG (2007) Endogenous bone morphogenetic protein-7 controls the motility of prostate cancer cells through regulation of bone morphogenetic protein antagonists. J Urol 178(3):1086–1091
Feeley BT, Gamradt SC, Hsu WK et al (2005) Influence of BMPs on the formation of osteoblastic lesions in metastatic prostate cancer. J Bone Miner Res 20(12):2189–2199
Simon DP, Vadakkadath Meethal S, Wilson AC et al (2009) Activin receptor signaling regulates prostatic epithelial cell adhesion and viability. Neoplasia 11(4):365–376
Najy AJ, Day KC, Day ML (2008) ADAM15 supports prostate cancer metastasis by modulating tumor cell-endothelial cell interaction. Cancer Res 68(4):1092–1099
Riordan JF (2001) Angiogenin. Methods Enzymol 341:263–267
Gao X, Hu H, Zhu J, Xu Z (2007) Identification and characterization of follistatin as a novel angiogenin-binding protein. FEBS Lett 581(28):5505–5510
Yoshioka N, Wang L, Kishimoto K et al (2006) A therapeutic target for prostate cancer based on angiogenin-stimulated angiogenesis and cancer cell proliferation. Proc Natl Acad Sci USA 103(39):14519–14524
Tsuji T, Sun Y, Kishimoto K et al (2005) Angiogenin is translocated to the nucleus of HeLa cells and is involved in ribosomal RNA transcription and cell proliferation. Cancer Res 65(4):1352–1360
Oh IS, Kim GH (2004) Vascular endothelial growth factor upregulates follistatin in human umbilical vein endothelial cells. Biotechnol Bioprocess Eng 9:201–206
Björklund M, Koivunen E (2005) Gelatinase-mediated migration and invasion of cancer cells. Biochim Biophys Acta 1755(1):37–69
Littlepage LE, Sternlicht MD, Rougier N et al (2010) Matrix metalloproteinases contribute distinct roles in neuroendocrine prostate carcinogenesis, metastasis, and angiogenesis progression. Cancer Res 70:2224–2234
Krneta J, Kroll J, Alves F et al (2008) Dissociation of angiogenesis and tumorigenesis in follistatin- and activin-expressing tumors. Cancer Res 66:5686–5695
Ogino H, Yano S, Kakiuchi S et al (2008) Follistatin suppresses the production of experimental multiple-organ metastasis by small cell lung cancer cells in natural killer cell-depleted SCID mice. Clin Cancer Res 14:660–667
Seder CW, Hartojo W, Lin L et al (2009) Upregulated INHBA expression may promote cell proliferation and is associated with poor survival in lung adenocarcinoma. Neoplasia 11(4):388–396
Chlenski A, Liu S, Baker LJ et al (2004) Neuroblastoma angiogenesis is inhibited with a folded synthetic molecule corresponding to the epidermal growth factor-like module of the follistatin domain of SPARC. Cancer Res 64(20):7420–7425
Stove C, Vanrobaeys F, Devreese B et al (2004) Melanoma cells secrete follistatin, an antagonist of activin-mediated growth inhibition. Oncogene 23(31):5330–5339
Planque C, Kulasingan V, Smith CR et al (2009) Identification of five candidate lung cancer biomarkers by proteomic analysis of conditioned media of four lung cancer cell lines. Mol Cell Proteomics 8(12):2746–2758
Goo YA, Liu AY, Ryu S et al (2009) Identification of secreted glycoproteins of human prostate and bladder stromal cells by comparative quantitative proteomics. Prostate 69(1):49–61
van der Poel HG, Hanrahan C, Zhong H, Simons JW (2003) Rapamycin induces Smad activity in prostate cancer cell lines. Urol Res 30:380–386
Acknowledgments
This study was supported by funds from Ministry of Education, University and Research (MIUR) (Fondi Ateneo ex quota 60%).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tumminello, F.M., Badalamenti, G., Fulfaro, F. et al. Serum follistatin in patients with prostate cancer metastatic to the bone. Clin Exp Metastasis 27, 549–555 (2010). https://doi.org/10.1007/s10585-010-9344-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-010-9344-x