Abstract
Preschool-age “hot” executive function capacity (i.e. reward-related effortful control) represents an early kind of self-regulation that is involved in social adjustment development as well as the development of subtypes of attention-deficit/hyperactivity disorder (ADHD). Early self-regulation development might be malleable by responsive parenting. We analyzed whether maternal responsiveness/sensitivity predicts reward-related control (RRC) development within the preschool period, and whether RRC mediates a negative link between maternal responsiveness and ADHD symptoms. A sample of 125 preschoolers and their families were seen at the ages of 4 and 5 years. Maternal responsiveness/sensitivity was assessed via home observations, RRC by neuropsychological tasks, and ADHD symptoms by a structured clinical parent interview. Maternal responsiveness/sensitivity predicted RRC development. The negative link between maternal responsiveness/sensitivity at 4 years and ADHD symptoms at 5 years was mediated by RRC performance at 5 years. Preschoolers showing ADHD symptoms combined with low RRC capacity in particular might benefit from responsive/sensitive parenting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent decades, broad evidence of a link between early emerging self-regulation capacity and social adjustment development across childhood and adolescence has been provided [1–3]. Temperamental self-regulation (also termed effortful control) has been defined as the capacity to voluntarily suppress a dominant cognitive, motor, motivational, or emotional response and to perform a subdominant one according to a rule or demand [3, 4]. The capacity largely overlaps with the executive function of inhibitory control (see [5, 6]) and has been thought to involve the executive (anterior) attention network [7].
Regarding executive functioning, recent neuropsychological and neuroimaging findings suggest differentiating between a “cool” and a “hot” executive control system [4, 8, 9]. Cool executive control refers to the capacity to suppress prepotent responses to abstract, cognitive, non-reward-related stimuli, while “hot” executive control refers to the suppression of responses to reward-related, motivational stimuli. Processing of cool and hot executive control tasks has been found to involve overlapping but also specific brain circuitry. Cool inhibitory control tasks involve a wide network of brain regions, including the anterior cingulate cortex, the inferior frontal gyrus, the dorsal lateral prefrontal cortex, the frontal eye field, the posterior parietal cortex, the striatum, and the cerebellum [7, 10]. Hot, reward-related tasks have been shown to involve the ventromedial orbitofrontal cortex/medial prefrontal cortex, the anterior cingulate, the ventral striatum and limbic brain structures [11, 12]. These networks and the associated performance in cool and hot executive control tasks have been found to mature far into late childhood and adolescence. Most critical developmental changes, however, have been shown to occur in the preschool period from 3 to 4 years onwards [13, 14].
Both characteristics, i.e. cognitive, cool inhibitory control and hot, reward-related control (RRC) have been thought to be involved in the pathogenesis of attention-deficit/hyperactivity disorder (ADHD). The characteristics have been regarded as basic deficits that indicate independent developmental pathways to the disorder. More specifically, the cool executive function pathway has been found to be characterized by compromised inhibitory control capacity [5, 15, 16], the motivational pathway by a low capacity to delay a gratification and the tendency to experience frustration while waiting (i.e. delay aversion), dysfunctional reward sensitivity [17], and an extreme approach tendency/exuberance [15, 18]. Accordingly, medium-sized correlations have been found between ADHD symptoms and performance in cool inhibitory control and hot RRC tasks (see the meta-analyses [19, 20]). The ADHD-related causal pathways have been thought to be based on genetic dispositions but may also involve aspects of an inadequate parent–child relationship [15, 16].
Indeed, recent research has provided some evidence for the malleability of early self-regulation development by environmental conditions. On the one hand, delay of gratification performance in preschoolers significantly improved after cognitive interventions comprising techniques like internal redirection of attention or altering the cognitive representation of the desired object [1, 21]. On the other hand, parenting behaviors that foster the use of internal language and cooperation with parents [22, 23] predicted the development of self-regulation/effortful control. More specifically, Lengua et al. [24] found that parental responsiveness, respect for autonomy and adequate limit setting in 3-year-olds predicted an increase in effortful control 6 months later. Kochanska et al. [23] showed that maternal responsiveness at the child’s age of 22 months predicted effortful control at 33 months. Chang et al. [25] found a positive association between maternal warmth/responsiveness and a latent effortful control variable in boys. These studies, however, used aggregate scores on cool and hot executive control tasks, leaving the question open whether developmental improvements in both domains are associated with parenting.
Several longitudinal studies analyzed the role of sensitive, responsive parenting as a predictor of exclusively cool executive function development in preschoolers (i.e. performance in cool inhibitory control and working memory tasks). The obtained associations were usually positive (see [22, 26–29]). Moreover, because cool executive functioning and RRC have been supposed to be involved in the development of ADHD symptoms, a mediation effect between parenting and ADHD symptoms by cool executive functions and RRC appears likely. However, such mediation effects have also been analyzed exclusively for the cool domain. Here, Sulik et al. [29] found that the link between sensitive parenting and externalizing symptoms in children between 36 and 90 months was mediated by cool executive functions of the child (i.e. working memory, inhibitory control, shifting). Olson et al. [28], however, were unable to confirm such a mediation model. In their study, parenting and a cool executive function score independently predicted later externalizing symptoms of the child. To the best of our knowledge, a corresponding model comprising ADHD symptoms and RRC capacity in particular has not yet been examined, and only two studies have investigated the association between parenting and RRC performance: In preschoolers from low-income families, Li-Grining [30] found that delay of gratification performance (measured by the Snack Delay and the Gift-Wrap task of the effortful control battery by Kochanska) at age 4 was associated with a composite score comprising concurrent and preceding child-mother connectedness. By contrast, Bernier et al. [26] found no association between parenting behaviors such as maternal responsiveness, autonomy support/mind-mindedness and delay of gratification (measured by the Gift Wrap task) development between 18 and 26 months.
Taken together, RRC capacity has been regarded as an essential component of social adjustment development and as a vulnerability marker for one of the heterogeneous ADHD-related etiological pathways. RRC development might be fostered by responsive, sensitive parenting and might mediate the link between parenting and ADHD symptoms. These associations have been thought to be specifically pronounced in the preschool period because of a heightened sensitivity of the developing RRC-related brain circuitry to environmental influences [31, 32]. However, empirical research on these issues is sparse and the few existing studies show conflicting results. In the present study, we therefore aim to analyze whether maternal responsiveness/sensitivity predicts preschool RRC development and whether RRC might work as a mediator between the parenting behavior and ADHD symptoms. It was hypothesized that (1) maternal responsiveness assessed at age 4 predicts RRC development between the ages of 4 and 5, and (2) RRC mediates a negative link between maternal responsiveness at age 4 and ADHD symptoms at age 5.
Method
Participants
The sample consisted of 125 4-year-old children (71 boys; 57%) and their primary caregivers. At childcare facilities in Marburg and surrounding villages (mid-Western Germany), parents of 4-year-old children received an information letter and were asked to fill in a screening questionnaire on ADHD symptoms (ADHD rating scale by Döpfner, Görtz-Dorten, and Lehmkuhl [33], description see below). Preschoolers showing elevated ADHD symptoms were oversampled (i.e. 65 children, 52% of the sample, exceeded the 70th percentile of the screening questionnaire). Exclusion criteria were: IQ < 80, motor disabilities, sensory handicaps, chronic diseases involving brain functions, any continuous pharmacological treatment, and insufficient German language skills of parents or child. Sample characteristics are shown in Table 1.
Assessments were conducted at two time points: at age 4 (M = 54; SD = 3; range: 48–59 months) and 12 months later, at age 5 (M = 67; SD = 3; range: 60–74 months). Of the original sample, five parent–child pairs (4%) did not take part in the second assessment wave, leaving 120 participants (96%) for the longitudinal analyses. Parents gave their written informed consent to participate in the study, and received an expense allowance of 50 Euros at each wave. The study was approved by the Ethics Committee of the Faculty of Medicine, University of Marburg.
Procedure
At each assessment wave, a home visit, a “playroom” session, and a telephone interview with the mother were conducted. Observations of mother–child interaction and an intelligence test with the child were conducted during the home visits, RRC tasks were conducted in a quiet room at the childcare facilities, and the clinical interview on the child’s ADHD symptoms was carried out by telephone. The examiners who conducted the home visits and scored maternal responsiveness during the interaction episodes were blind to the RRC and to the ADHD symptom scores of the child.
Variables
Maternal Responsiveness/Sensitivity at Age 4
Maternal responsiveness was assessed during two interaction tasks conducted at home. In the first task, mother and child were instructed to work together on a puzzle (60 pieces, picture of cats), and in the second task, they were asked to build a figure (according to a template) with toy building blocks. Each episode lasted for 6 min. Responsiveness was assessed using the 4-point rating scale “Responsiveness/Sensitivity/Appropriate Scaffolding” of the Mannheim Rating Scale for the Assessment of Mother–Child Interaction (MBS-MKI) by Polowczyk et al. [34]. Good responsiveness/sensitivity is defined as being attentive to the child’s behavior, interpreting his/her behavior accurately and reacting adequately while respecting the intentions and rhythm of the child, such that the mother often follows the child’s lead in the play interactions. Poor responsiveness/sensitivity is characterized by intrusive/overinvolved and/or non-responsive behavior of the mother. Inter-rater reliability was checked in 10% (n = 13) of the home visits and proved to be adequate (Kappa = 0.74). For further analyses, the ratings of the 30-second intervals were summed up.
RRC Tasks at Ages 4 and 5
At both ages, the RRF battery comprised three tasks that are commonly used in the preschool ADHD context. The Cookie-Delay Task and the Gift-Wrap Task from the Effortful Control Battery by Kochanska [35] use a waiting paradigm, which requires the child to wait for a reward (see [36, 37]). The Stranger-with-Toys Task by Asendorpf [38] was included to capture the component of increased approach tendency/exuberance (see [39, 40]).
In the Cookie-Delay Task (also termed Snack-Delay), the child was instructed to wait for the ringing of a bell before he/she could retrieve a sweet that was covered by a transparent cup. After a practice trial, six trials followed, with delay intervals between 10 and 40 s. Approach behaviors were scored (e.g. touching, lifting the cup, eating the sweet before the bell rang). The task has proven to be age-appropriate [41, 42], and factorial and construct validity have been demonstrated [36, 40].
In the Gift-Wrap Task, the child was instructed to sit behind the experimenter and not to look while the experimenter wrapped a present for the child. Approach behavior of the child was scored. The task has also proven to be age-appropriate [41, 42], has shown significant correlations with ADHD symptoms [43] and has been found to discriminate significantly between children with and without a positive ADHD family history [40].
As mentioned, the Stranger-with-Toys Task was conducted in order to include a measure of the approach tendency of the child that has been thought to underlie low RRC performance and has been regarded as a component of the ADHD-related motivational pathway. Similar tasks have been previously used to capture exuberance (e.g. [44]). In this task, the child sat at a table with one rather boring toy. A stranger entered the room, carrying a transparent bag of interesting toys, which she successively unpacked and played with while not attending to the child. After 3 min, she invited the child to play with her together with the toys and continued to talk kindly to the child for a further 2 min. The latency (seconds) until the child’s first spontaneous utterance directed to the stranger was scored. The measure has proven to be highly stable (0.74 across 2 years) and has shown significant associations with parent ratings of the child’s approach versus. withdrawal behavior and observed approach behavior in peer interactions [38]. The task has been demonstrated to load on a delay aversion factor and to discriminate between children with and without a positive ADHD family history [40].
The tasks were carried out and scored by two trained investigators who worked together. Interrater reliability was assessed in n = 30 cases. Results were as follows: Stranger-with-Toys ICC = 0.90, Cookie-Delay ICC = 0.99, Gift-Wrap K = 0.95. In accordance with the results of a previous study [45] and to reduce the number of variables, we summed up the z-transformed scores of the single tasks to an RRC composite score at each age. At the 5-year assessment, however, the Gift-Wrap task showed nearly no variance, i.e. no child left his/her seat or tried to peek. This task was therefore excluded from the analyses. The RRC score at age 5 thus comprised performance in the Cookie-Delay and the Stranger-with-Toys Task. Intercorrelation(s) (Spearman’s r) of the tasks ranged between 0.09 and 0.11 at age 4 and was 0.29 at age 5. Stability (rtt) of the composite score across the 12-month period was 0.41.
ADHD Symptom Assessment at Ages 4 and 5
At both assessment waves, ADHD symptoms of the child were assessed by a structured clinical parent interview and by parent and teacher questionnaires. The Parental Account of Childhood Symptoms (PACS) interview [46] in the modified preschool version (PrePACS) by Daley [47] was conducted with the mother. The ADHD scale shows good test–retest reliability (0.78, 15-week interval) and discriminates significantly between children with ADHD and healthy controls [48]. Parents and nursery teachers filled in the preschool version of the ADHD rating scale (FBB-ADHS-V) by Döpfner et al. [33]. The questionnaire captures ADHD symptoms according to ICD-10 and DSM5. The parent and teacher version shows high homogeneity (Cronbach’s alpha: 0.94 and 0.93) and good validity (differentiation between children with and without an ADHD diagnosis) [49]. The three ADHD scores intercorrelated as follows (age 4, age 5): FBB-ADHS-V parent and teacher score: 0.29, 0.57; PrePacs score and FBB-ADHS-V teacher: 0.06, 0.31; PrePacs score and FBB-ADHS-V parent: 0.48, 0.63. At each age, the three scores were summed up after z-transformation. Stability (rtt) across the 12-month period was 0.76.
Control Variables
To control for possible influences of maternal ADHD symptoms, intelligence level of the child, and oppositional and emotional problems of the child on the hypothesized associations, we assessed these variables using the following methods.
Intelligence Level
Intelligence level of the child was assessed at the 5-year assessment wave using four subtests of the German version of the Wechsler Preschool and Primary Scale of Intelligence (WPPSI-III) [50], i.e. Word Reasoning, Vocabulary, Block Design, and Matrix Reasoning. These subtests have shown the highest reliability and loadings on the verbal and performance intelligence factors [50] and were used in the present study to approximate the child’s IQ.
Maternal ADHD Symptoms
Mothers filled in the German version of the Conners Adult ADHD Rating Scale (CAARS; [51]) and were interviewed using the Wender-Reimherr interview for adults [52]. Internal consistency (Cronbach’s alpha) of the interview scale is 0.82. The method validly differentiates between adults with and without an ADHD diagnosis [52]. The scores were summed up after z-transformation.
Symptoms of Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD)
Mothers filled in the German FBB-SSV questionnaire, which measures ODD/CD symptoms of the child [33] according to ICD-10. The scale shows high internal consistency (Cronbach’s alpha = 0.91) and validly discriminates between children with ODD/CD and controls [53].
Symptoms of Anxiety and Depression
The Anxious/Depressed scale of the German version of the Child Behavior Checklist (CBCL4-18) by Döpfner, Schmeck, Berner, Lehmkuhl, and Poustka [54] was employed. The scale shows significant associations with anxiety and emotional disorders, indicating good validity [54].
Statistical Analyses
After preliminary analyses of the intercorrelations of the study variables, a multiple hierarchical regression analysis was conducted to examine whether maternal responsiveness predicts the development of RRC between the assessments at 4 and 5 years. In this analysis, the RRC score at 5 years was used as the criterion variable while controlling for the concurrent RRC score at age 4. Analogously, we analyzed whether maternal responsiveness predicts ADHD development. In all analyses, we controlled for the child’s gender and age (in months at the 5-year wave). If significantly associated with the criterion variable, we additionally controlled for maternal symptoms of ADHD, intelligence level of the child and oppositional and emotional symptoms of the child.
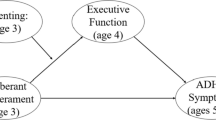
The prerequisites for a mediation relationship are fulfilled if the maternal responsiveness at 4 years and the RRC and ADHD score at 5 years intercorrelate significantly [55]. In this case, it was analyzed whether the link between maternal responsiveness at 4 years and ADHD symptoms at 5 years was mediated by the RRC score at 5 years using a path-analytic approach (see Fig. 1). In other words, the total link between maternal responsiveness and subsequent ADHD symptoms was apportioned into an indirect link via RRC (paths a and b) and a direct link (path c′). Path a represents the link between maternal responsiveness and RRC, and path b the link between RRC and ADHD symptoms while partialling out the influence of maternal responsiveness. To test the significance of the total mediation effect via RRC, we used the bootstrapping procedure (assumptions made by this procedure are more realistic compared to Sobel tests) recommended by Preacher and Hayes [56]. For these calculations, we used the SPSS Macro “Indirect” by Preacher and Hayes [56]. All calculations were conducted using IBM SPSS Statistics (IBM Corp.).
Mediation model. Direct and indirect paths for the link between maternal responsiveness at age 4 (4y) and ADHD symptoms at age 5 (5y). Corresponding path coefficients and significance tests are listed in Table 4
Results
Table 2 shows the bivariate intercorrelations of the study variables. Between the 4- and 5-year assessments, stability of RRC was of medium size while stability of the ADHD symptom score was high. While the RRC score at 5 years was not associated with any of the control variables, the ADHD score at 5 years was significantly associated with behavioral and emotional symptoms and intelligence of the child.
Prediction of Change in RRC Capacity
To analyze whether maternal responsiveness at 4 years predicts change in RRC between the 4- and 5-year assessments, a multiple hierarchical regression analysis was conducted (see Table 3). After controlling for gender and age of the child and the RRC score at 4 years, maternal responsiveness was significantly associated with the RRC score at 5 years, indicating a significant prediction of an increase in RRC between 4 and 5 years by high maternal responsiveness.
Prediction of ADHD Symptoms
Maternal responsiveness was significantly negatively associated with the ADHD symptoms of the child at age 4 and at age 5 (Table 2). The higher the ADHD symptoms of the child were at age 4 and 5, the poorer was the mother’s responsiveness/sensitivity. After controlling for the ADHD score at 4 years, maternal responsiveness was no longer associated with the ADHD score at 5 years (Fchange = 0.06, p = .82), indicating that maternal responsiveness/sensitivity was negatively associated with the stability of the ADHD symptoms between ages 4 and 5.
Mediation Analysis
The associations between maternal responsiveness, 5-year RRC and ADHD symptoms were statistically significant. Thus, the prerequisites for the hypothesized mediation effect were given. Table 4 shows the results of the mediation analysis. In the path-analytic approach, the total effect of maternal responsiveness on ADHD symptoms is divided into an indirect effect via RRC at 5 years and a direct effect. Here, the indirect effect proved to be statistically significant, while the direct link was not statistically significant, indicating that the link between maternal responsiveness and ADHD symptoms was completely mediated by RRC capacity at 5 years. This result did not change after controlling for gender and age of the child. Controlling for oppositional and emotional symptoms, however, led to a non-significant total association between maternal responsiveness and ADHD symptoms, making a mediation analysis dispensable.
Discussion
The primary aim of the present study was to examine whether maternal responsiveness/sensitivity predicts developmental changes in RRC performance, i.e. an increase in the capacity to suppress dominant, reward-related responses. In a second step, we analyzed whether the putative association between maternal responsiveness/sensitivity and ADHD symptoms is mediated by RRC development. We expected to find the hypothesized associations within the preschool period, because critical developmental changes in RRC performance and the underlying brain circuitry have been thought to lead to an increased sensitivity to environmental conditions such as responsive, sensitive parenting.
In the present study, RRC and maternal responsiveness/sensitivity were assessed by blinded examiners in independent settings (maternal responsiveness during a home visit, the child’s RRC performance in playroom sessions at the childcare facilities). RRC and maternal responsiveness were measured by age-appropriate, valid tasks/procedures. The stability in RRC performance across the 12-month period was of medium size, indicating temporal continuity but also developmental change. We confirmed our hypothesis that responsive/sensitive parenting predicts RRC development between 4 and 5 years. Specifically, high maternal responsiveness/sensitivity measured at age 4 was associated with an increase in the child’s RRC capacity across the 12-month period between 4 and 5 years. Our result is in line with the findings of Li-Giring [30], who demonstrated that dyadic connectedness (regarded as a proxy for optimal parenting) was associated with concurrent RRC performance in the preschool period. It is also consistent with Lengua et al. [24] finding that responsiveness/respect for autonomy and adequate limit setting predicted effortful control development between 33 and 40 months. Maternal responsiveness, therefore, might foster the developing RRC capacity.
Responsive parenting represents an enduring attitude of a parent that enables the recognition and reassurance of the child’s emotional/motivational states and appropriate regulatory responses (adjusted to the specific child and without under- or overcontingency) in everyday life [57]. This social exchange process has been found to lead to a variety of positive adjustment outcomes in the child, including verbal ability, symbolic competence, and social facility as well as a sense of security and trust in the availability and reliability of the parent [57]. Maternal responsiveness has been thought to influence self-regulation development via an improvement in self-directed internal speech and the adoption of effective regulation strategies [22]. Moreover, the secure and trustful relationship with the parent might enhance the child’s cooperation, his/her compliance with the rules of the parent and the wider social environment [23]. It seems very probable that these mechanisms lead to a successive improvement in RRC. However, although our longitudinal results and those of others point to the possibility of such causal effects, influences of confounding and mediating variables (e.g. genetic effects) cannot be ruled out. To examine whether parenting behavior actually causes an improvement in RRC, future research should employ randomized controlled trials (e.g. on the effect of responsiveness/sensitivity training on RRC development).
We found the expected link between maternal responsiveness/sensitivity and ADHD symptoms of the child. Low responsiveness was associated with continuously high ADHD symptoms across the 12-month period. The longitudinal association between maternal responsiveness and ADHD symptoms at age 5 was shared with oppositional symptoms. In other words, after controlling for oppositional symptoms, ADHD symptoms were no longer associated with preceding maternal responsiveness/sensitivity. The findings correspond to observations that children with ADHD symptoms frequently also show oppositional behavior problems, and that specifically combined ADHD plus oppositional symptoms are associated with inadequate parenting [58]. Coercive cycles have been assumed, with increasingly inadequate parenting and worsening of behavior problems of the child [16]. Our results are well in line with this assumption.
We analyzed whether the link between responsiveness and ADHD symptoms was mediated by RRC. In the hypothesized mediation model, the indirect link between maternal responsiveness/sensitivity at age 4 and ADHD symptoms at age 5 via RRC at age 5 proved to be statistically significant and completely mediated the total link. The result is in line with the notion that maternal responsiveness/sensitivity fosters RRC development, which in turn lessens the ADHD symptoms of the child. This mediation effect, however, did not persist after adjustment for oppositional symptoms, indicating that the obtained effect applied to ADHD symptoms that occurred in combination with oppositional symptoms. The result corresponds well with the description of increased aggressive, oppositional symptoms associated with the motivational pathway to ADHD.
The following limitations of our study should be mentioned. First, though statistically significant, the effect sizes of the associations involving ADHD symptoms were predominantly small. However, as pointed out above, ADHD symptoms comprise a set of etiologically and phenotypically heterogeneous subcomponents. Only some of these might be associated with maternal responsiveness and RRC. Therefore, larger effects cannot be expected. Second, the child’s RRC and ADHD symptom development might also involve paternal parenting behaviors, which we did not consider. The inclusion of paternal parenting behaviors could have increased the amount of explained variance. Third, we adopted a dimensional measurement approach to ADHD in a community-based sample. A comprehensive review by Coghill and Sonuga-Barke [59] strongly suggests a dimensional nature of ADHD, and specifically in the preschool period, such an approach is regarded as more sensitive for capturing the putative precursor stages of the disease [60]. Fourth, the RRC tasks at age 4 intercorrelated weakly, implying low homogeneity of the summary score at that age. Using the three single RRC scores (instead of the summary score) as control variables in the regression analysis, however, did not change the significance of the prediction by maternal responsiveness. Moreover, the stability of the RRC summary score was significant and of medium size, indicating an adequate test–retest reliability across 12 months.
To conclude, our study extended previous research by showing that maternal responsiveness predicted an increase in RRC performance in the preschool period. Maternal responsiveness/sensitivity might facilitate RRC development via an improvement in internal language and in the child’s cooperation with his/her caregiver. As it seems possible that a specific subtype of children who show ADHD symptoms combined with oppositional symptoms and low RRC capacity could benefit from responsive/sensitive parenting, it would be worthwhile to analyze whether interventions focusing on maternal responsiveness could improve self-regulation and social adjustment development in these preschoolers in particular.
Summary
In the present study, we analyzed whether maternal responsiveness/sensitivity predicts the development of reward-related, “hot” effortful control (RRC) between 4 and 5 years and whether RRC mediates a putatively negative link between maternal responsiveness and ADHD symptoms. Regarding these questions empirical research has been sparse and the few existing studies showed conflicting results. Our sample consisted of 125 4-year-old children (71 boys; 57%) and their primary caregivers. Parent–child pairs were seen twice, at the child’s age of 4 years and 12 months later, at age 5. Maternal responsiveness/sensitivity was assessed by an at-home observation procedure, RRC by a set of neuropsychological tasks, and ADHD symptoms via a structured clinical interview with the mother and questionnaires filled in by parents and teachers. We confirmed our hypothesis that high maternal responsiveness/sensitivity at age 4 predicts an increase in the child’s RRC capacity across the 12-months period. The negative link between maternal responsiveness/sensitivity at 4 years and ADHD symptoms at 5 years was completely mediated by RRC performance at 5 years. We concluded that maternal responsiveness/sensitivity might facilitate RRC development. Preschoolers showing ADHD symptoms and low RRC capacity in particular might benefit from responsive/sensitive parenting.
References
Mischel W, Ayduk O, Berman MG, Casey BJ, Gotlib IH, Jonides J, Kross E, Teslovich T, Wilson NL, Zayas V, Shoda Y (2011) ‘Willpower’ over the life span: decomposing self-regulation. Soc Cogn Affect Neurosci 6(2):252–256
Rothbart MK, Bates JE (2006) Temperament. In: Eisenberg N, Damon W, Lerner RM (eds) Handbook of child psychology, vol 3. Social, emotional, and personality development. Wiley, Hoboken, pp 105–176
Eisenberg N, Spinrad TL, Eggum ND (2010) Emotion-related self-regulation and its relation to children’s maladjustment. Annu Rev Clin Psychol 6:495–525
Kim S, Nordling JK, Yoon JE, Boldt LJ, Kochanska G (2013) Effortful control in “hot” and “cool” tasks differentially predicts children’s behavior problems and academic performance. J Abnorm Child Psychol 41(1):43–56
Barkley RA (1997) Behavioral inhibition, sustained attention, and executive functions:constructing a unifying theory of ADHD. Psychol Bull 121(1):65–94
Garon N, Bryson SE, Smith IM (2008) Exekutive function in preschoolers: a review using an integrative framework. Psychol Bull 134 (1):31–60
Petersen SE, Posner MI (2012) The attention system of the human brain: 20 years after. Annu Rev Neurosci 35:73–89
Willoughby M, Kupersmidt J, Voegler-Lee M, Bryant D (2011) Contributions of hot and cool self-regulation to preschool disruptive behavior and academic achievement. Dev Neuropsychol 36(2):162–180. doi:10.1080/87565641.2010.549980
Zelazo PD, Carlson SM (2012) Hot and cool executive function in childhood and adolescence: development and plasticity. Child Dev Perspect 6(4):354–360
Hwang K, Velanova K, Luna B (2010) Strengthening of top-down frontal cognitive control networks underlying the development of inhibitory control: a functional magnetic resonance imaging effective connectivity study. J Neurosci 30(46):15535–15545
Plichta MM, Scheres A (2014) Ventral-striatal responsiveness during reward anticipation in ADHD and its relation to trait impulsivity in the healthy population: a meta-analytic review of the fMRI literature. Neurosci Biobehav Rev 38:125–134
Rubia K (2013) Functional brain imaging across development. Eur Child Adolesc Psychiatry 22(12):719–731
Rothbart MK, Sheese BE, Rueda MR, Posner MI (2011) Developing mechanisms of self-regulation in early life. Emot Rev 3(2):207–213
Posner MI, Rothbart MK, Sheese BE, Voelker P (2012) Control networks and neuromodulators of early development. Dev Psychol 48(3):827–835
Nigg JT, Goldsmith HH, Sachek J (2004) Temperament and attention deficit hyperactivity disorder: the development of a multiple pathway model. J Clin Child Adolesc 33(1):42–53
Sonuga-Barke EJ, Auerbach J, Campbell SB, Daley D, Thompson M (2005) Varieties of preschool hyperactivity: multiple pathways from risk to disorder. Dev Sci 8(2):141–150
Luman M, Oosterlaan J, Sergeant JA (2005) The impact of reinforcement contingencies on AD/HD: a review and theoretical appraisal. Clin Psychol Rev 25(2):183–213
Nigg JT (2006) Temperament and developmental psychopathology. J Child Psychol Psychiatry 47(3–4):395–422
Pauli-Pott U, Becker K (2011) Neuropsychological basic deficits in preschoolers at risk for ADHD: a meta-analysis. Clin Psychol Rev 31(4):626–637
Pauli-Pott U, Becker K (2015) Time windows matter in ADHD-related developing neuropsychological basic deficits: A comprehensive review and meta-regression analysis. Neurosci Biobehav Rev 55:165–172. doi:10.1016/j.neubiorev.2015.04.011
Murray J, Theakston A, Wells A (2016) Can the attention training technique turn one marshmallow into two? Improving children’s ability to delay gratification. Behav Res Ther 77:34–39
Hammond SI, Muller U, Carpendale JIM, Bibok MB, Liebermann-Finestone DP (2012) The effects of parental scaffolding on preschoolers’ executive function. Dev Psychol 48(1):271–281
Kochanska G, Murray KT, Harlan ET (2000) Effortful control in early childhood: continuity and change, antecedents, and implications for social development. Dev Psychol 36(2):220–232
Lengua LJ, Honorado E, Bush NR (2007) Contextual risk and parenting as predictors of effortful control and social competence in preschool children. J Appl Dev Psychol 28(1):40–55
Chang H, Olson SL, Sameroff AJ, Sexton HR (2011) Child effortful control as a mediator of parenting practices on externalizing behavior: evidence for a sex-differentiated pathway across the transition from preschool to school. J Abnorm Child Psychol 39(1):71–81
Bernier A, Carlson SM, Whipple N (2010) From external regulation to self-regulation: early parenting precursors of young children’s executive functioning. Child Dev 81(1):326–339
Hughes C, Ensor R (2005) Executive function and theory of mind in 2 year olds: a family affair? Dev Neuropsychol 28(2):645–668
Olson SL, Tardif TZ, Miller A, Felt B, Grabell AS, Kessler D, Wang L, Karasawa M, Hirabayashi H (2011) Inhibitory control and harsh discipline as predictors of externalizing problems in young children: a comparative study of U.S., Chinese, and Japanese preschoolers. J Abnorm Child Psychol 39(8):1163–1175
Sulik MJ, Blair C, Mills-Koonce R, Berry D, Greenberg M, Investigators FLP (2015) Early parenting and the development of externalizing behavior problems: longitudinal mediation through children’s executive function. Child Dev 86(5):1588–1603
Li-Grining CP (2007) Effortful control among low-income preschoolers in three cities: Stability, change, and individual differences. Dev Psychol 43(1):208–221
Wass SV, Scerif G, Johnson MH (2012) Training attentional control and working memory—Is younger, better? Dev Rev 32(4):360–387
Sonuga-Barke EJ, Halperin JM (2010) Developmental phenotypes and causal pathways in attention deficit/hyperactivity disorder: potential targets for early intervention? J Child Psychol Psychiatry 51(4):368–389
Döpfner M, Görtz-Dorten A, Lehmkuhl G (2008) DISYPS-II Diagnostik-System für psychische Störungen nach ICD-10 und DSM-IV für Kinder und Jugendliche - II. Huber, Bern
Polowczyk M, Trautmann-Villalba P, Dinter-Jörg M, Gerhold M, Laucht M, Schmidt M, Esser G (2000) Auffällige Mutter-Kind-Interaktion im Vorschulalter bei Kindern mit hyperkinetischen und Sozialverhaltensauffälligkeiten. Z Klin Psychol Psychothera 29(4):293–304
Kochanska G (2009) Family study. Effortful control batteries. University of Iowa, Iowa City
Dalen L, Sonuga-Barke EJ, Hall M, Remington B (2004) Inhibitory deficits, delay aversion and preschool AD/HD: implications for the dual pathway model. Neural Plast 11(1–2):1–11
Marakovitz SE, Campbell SB (1998) Inattention, impulsivity, and hyperactivity from preschool to school age: performance of hard-to-manage boys on laboratory measures. J Child Psychol Psychiatry 39(6):841–851
Asendorpf JB (1990) Development of inhibition during childhood: Evidence for situational specificity and a two-factor model. Dev Psychol 26:721–730
Pauli-Pott U, Dalir S, Mingebach T, Roller A, Becker K (2014) Attention deficit/hyperactivity and comorbid symptoms in preschoolers: differences between subgroups in neuropsychological basic deficits. Child Neuropsychol 20(2):230–244
Pauli-Pott U, Roller A, Heinzel-Gutenbrunner M, Mingebach T, Dalir S, Becker K (2014) Inhibitory control and delay aversion in unaffected preschoolers with a positive family history of attention deficit hyperactivity disorder. J Child Psychol Psychiatry 55(10):1117–1124
Carlson SM (2005) Developmentally sensitive measures of executive function in preschool children. Dev Neuropsychol 28(2):595–616
Petersen IT, Hoyniak CP, McQuillan ME, Bates JE, Staples AD (2016) Measuring the development of inhibitory control: the challenge of heterotypic continuity. Dev Rev 40:25–71
Breaux RP, Griffith SF, Harvey E (2016) Preschool neuropsychological measures as predictors of later attention deficit hyperactivity disorder. J Abnorm Child Psychol 44(8):1455–1471
Fox NA, Henderson HA, Rubin KH, Calkins SD, Schmidt LA (2001) Continuity and discontinuity of behavioral inhibition and exuberance: psychophysiological and behavioral influences across the first four years of life. Child Dev 72(1):1–21
Pauli-Pott U, Dalir S, Mingebach T, Roller A, Becker K (2013) Do different ADHD-related etiological risks involve specific neuropsychological pathways? An analysis of mediation processes by inhibitory control and delay aversion. J Child Psychol Psychiatry 54(7):800–809
Taylor E, Schachar R, Thorley G, Wieselberg M (1986) Conduct disorder and hyperactivity: I. Separation of hyperactivity and antisocial conduct in British child psychiatric patients. Br J Psychiatry 149:760–767
Daley D (2010) Preschool-parent account of child symptoms (Pre-Pacs). University of Southampton, Southampton
Sonuga-Barke EJ, Dalen L, Remington B (2003) Do executive deficits and delay aversion make independent contributions to preschool attention-deficit/hyperactivity disorder symptoms? J Am Acad Child Adolesc Psychiatry 42(11):1335–1342
Breuer D, Dopfner M (2008) Development of a questionnaire for the assessment of attention-deficit-/hyperactivity disorder (ADHD) in preschoolers by parents and/or teacher ratings. Z Entwickl Padagogis 40(1):40–48
Petermann F (ed) (2009) WPPSI-III, Wechsler Preschool and Primary Scale of Intelligence-III; German Version. Pearson Assessment & Information GmbH, Frankfurt am Main
Christiansen H, Kis B, Hirsch O, Matthies S, Hebebrand J, Uekermann J, Abdel-Hamid M, Kraemer M, Wiltfang J, Graf E, Colla M, Sobanski E, Alm B, Rosler M, Jacob C, Jans T, Huss M, Schimmelmann BG, Philipsen A (2012) German validation of the Conners Adult ADHD Rating Scales (CAARS) II: reliability, validity, diagnostic sensitivity and specificity. Eur Psychiatry 27(5):321–328
Rösler M, Retz-Junginger P, Retz W, Stieglitz R-D (2008) HASE Homburger ADHS-Skalen für Erwachsene. Hogrefe, Göttingen
Gortz-Dorten A, Ise E, Hautmann C, Walter D, Dopfner M (2014) Psychometric properties of a german parent rating scale for oppositional defiant and conduct disorder (FBB-SSV) in clinical and community samples. Child Psychiatry Hum Dev 45(4):388–397
Döpfner M, Schmeck K, Berner W, Lehmkuhl G, Poustka F (1994) Reliabilität und Validität der Child-Behavior-Checklist. Z Kinder- und Jugendpsychiat Psychother 22(3):189–205
Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51(6):1173–1182
Preacher KJ, Hayes AF (2008) Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods 40(3):879–891
Bornstein MH, Manian N (2013) Maternal responsiveness and sensitivity reconsidered: Some is more. Dev Psychopathol 25(4):957–971
Deault LC (2010) A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/ hyperactivity disorder (ADHD). Child Psychiatry Hum Dev 41:168–192
Coghill D, Sonuga-Barke EJ (2012) Annual research review: categories versus dimensions in the classification and conceptualisation of child and adolescent mental disorders–implications of recent empirical study. J Child Psychol Psychiatry 53(5):469–489
Sonuga-Barke EJ, Koerting J, Smith E, McCann DC, Thompson M (2011) Early detection and intervention for attention-deficit/hyperactivity disorder. Expert Rev Neurother 11(4):557–563
Funding
The research for this article was funded by a grant from the University Medical Centre Giessen-Marburg and by grants from the German Research Foundation (DFG, Be2573/3-1,2) to Prof Dr. Katja Becker and Prof. Dr. Ursula Pauli-Pott.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pauli-Pott, U., Schloß, S. & Becker, K. Maternal Responsiveness as a Predictor of Self-Regulation Development and Attention-Deficit/Hyperactivity Symptoms Across Preschool Ages. Child Psychiatry Hum Dev 49, 42–52 (2018). https://doi.org/10.1007/s10578-017-0726-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-017-0726-z