Abstract
Childhood exposure to trauma has been associated with increased rates of somatic symptoms (SS), which may contribute to diminished daily functioning. One hundred and sixty-one children residing at a residential treatment home who had experienced neglect and/or abuse were administered the Trauma Symptom Checklist for Children (TSCC), the Multidimensional Anxiety Scale for Children, and the Children’s Depression Inventory (CDI). Primary caregivers completed the Child Behavior Checklist. Two composite measures of SS were formed to represent both child- and caregiver-rated SS. Over 95% of children endorsed at least one SS on the child-rated measure. Children who had experienced sexual abuse had higher rates of SS relative to children who had not. Child-rated SS were highly correlated with the CDI total score and the TSCC subscales of anxiety, depression, posttraumatic stress, dissociation, and anger. The TSCC anxiety subscale mediated the relationship between sexual abuse and child-rated SS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Somatic symptoms (SS) represent an array of physical complaints that encompass a range of severities. Although the experience of SS per se is not atypical among non-clinical pediatric populations, exposure to trauma has been associated with increased rates of SS such as stomachaches, headaches, and muscle tension [1–3]. Following childhood trauma, SS may cause significant interference in daily functioning and may negatively affect social, academic and emotional well-being due to impairment in memory and learning, missed school days, and decreased sleep [4–6]. Additionally, due to the chronicity and severity of many SS, children may undergo unnecessary and stressful medical evaluations, procedures and treatments to rule out organic conditions, oftentimes accruing large medical costs [7].
In general, studies have examined correlates of adulthood SS, finding connections with retrospective recall of childhood traumas [8, 9]. Although informative, the extant research does not touch upon the experience of SS in childhood following exposure to varied traumatic events. However, several studies have highlighted the relationship between exposure to natural disasters and SS in children and adolescents [1, 10]. Trait anxiety, severity of exposure, family psychopathology and severity of loss uniquely predicted both posttraumatic stress disorder (PTSD) and SS following a natural disaster-related trauma in childhood [1, 10].
Few data exist on SS in children experiencing abuse and neglect despite its clinical importance. Children in the child welfare system are a unique population that may shed light on the experience of SS following trauma. These children have often been exposed to multiple traumatic events including physical, emotional and sexual abuse, neglect, abandonment, and witnessing of domestic violence, in addition to being removed from their homes [11]. Symptomatically, children may present with typical Diagnostic and Statistical Manual of Mental Disorders, 4th edition text revision (DSM-IV-TR) PTSD symptom clusters including re-experiencing of symptoms (e.g., nightmares, play enacting the trauma), avoidance of trauma reminders (e.g., forgetting aspects of the trauma, anhedonia) and hyperarousal (e.g., hypervigilance, irritability, sleep problems) [12]. However, children’s reactions to trauma may often look quite different than the framework for PTSD highlighted by the DSM-IV-TR [13]. For instance, children may respond to trauma by exhibiting SS, depressive and anxiety symptoms [10], inattention/hyperactivity, and/or disruptiveness [14].
Several theories have been proposed to explain the presence of SS following childhood trauma. One such theory posits that both SS and negative reactions to trauma, such as PTSD, share a similar psychological vulnerability [15]. This theory has been expanded to elucidate that the shared vulnerability is dependent on trait anxiety sensitivity (i.e., the fear of anxiety related sensations) [1]. It is also suspected that anxiety may relate to the increase in arousal symptoms following trauma. Following childhood trauma, the arousal symptom cluster of PTSD, as described in the DSM-IV [12], may be heightened while other symptom clusters (e.g., avoidance or re-experiencing) may be suppressed. This may lead to an over-expression of hyperarousal and may be displayed as an increase in SS [2]. Children who exhibit high rates of trait anxiety sensitivity may fear the negative sensations associated with anxiety and therefore be more highly attuned to arousal symptoms. This theory explains both the experience of increased anxiety and posttraumatic arousal symptoms with the presence of SS. Additionally, studies addressing the prevalence of SS in children with anxiety disorders have shown that up to 95% of children with an anxiety disorder report at least one SS and on average report six SS [16]. It is therefore suspected that the mechanism driving the relationship between childhood trauma and SS is the presence of anxiety. Specifically, this theory posits that childhood exposure to trauma yields anxiety which is experienced as an increase in hyperarousal symptoms and expressed in part as SS.
Studies that have addressed demographic and clinical characteristics of SS among clinically anxious children have yielded mixed findings. Evidence regarding gender differences in the expression of SS has varied with studies showing either no gender differences [16] or a higher rate of SS in females [1, 17]. Similarly, evidence regarding age differences in SS has also been mixed with some studies finding no age differences [1, 17] or higher rates of SS in older children [16]. The question of whether varying abuse types influence the experience of SS in childhood has seldom been explored. However, childhood sexual abuse is a unique predictor of SS in childhood and adolescence [18] as well as young adulthood [3]. There is evidence to support the direct association between posttraumatic stress reactions following other types of trauma (e.g., natural disasters, witnessing community violence) and SS in children [1, 19].
The purpose of this study is to determine the extent to which SS are associated with sociodemographic (i.e., gender, age at assessment) and clinical variables (i.e., type of abuse, anxiety, posttraumatic stress symptoms, anger, dissociation and depression). There are several reasons why it is important to study SS in traumatized youth. First, significant associations between trauma and SS may indicate the need to include measures of SS in the routine psychological and physical assessment of children following traumatic events. In order to avoid unnecessary and costly medical testing, it is important that healthcare providers are cognizant of the fact that traumatized children may present with SS unrelated to any underlying medical cause. Second, treatments for posttraumatic symptoms and other adverse outcomes of trauma may need to include additional interventions that target SS. For example, addressing underlying anxiety with either cognitive-behavioral therapy or psychopharmacology may reduce SS [16, 17]. Finally, it is important to examine the physiological correlates of trauma yielding a better understanding of the phenomenology of posttraumatic reactions in children. We predicted that: (a) Consistent with previous research [17], there will be gender and age differences, with females and older children exhibiting higher rates of SS relative to males and younger children. (b) Consistent with others [3, 18], children who have experienced sexual abuse will have higher rates of SS relative to those children who have not experienced sexual abuse. (c) Duration in time since removal from home will be negatively associated with presence of SS. This prediction was based on literature indicating that psychosocial stressors such as loss, injury and trauma are associated with increased SS [10]. (d) Somatic symptoms in traumatized children will be directly related to anxiety, posttraumatic stress, and depressive symptoms. (e) In accordance with previous research that posits that health anxiety may increase awareness to arousal symptoms, thereby increasing the experiencing of SS [9], we predict that anxiety will mediate the relationship between trauma and SS. Additionally, the mediational analysis will focus on sexual abuse as previous research has noted the strong connection between sexual abuse, health anxiety, and SS [3, 9, 18].
Method
Participants
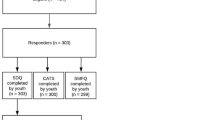
Archival data were reviewed for 161 children residing in a residential setting for foster children necessitating a higher level of care than can be provided in a traditional foster home. All records were reviewed for children living in the home between 1996 and 2011. On average, the residential setting admits four new children per month. For study purposes, all children who met the following inclusion criteria were included in analyses: (a) at least 8 years of age (3 excluded), (b) had completed the Multidimensional Anxiety Scale for Children (MASC; [20]) (217 excluded), the Trauma Symptom Checklist for Children (TSCC; [21]) (10 excluded), and the Children’s Depression Inventory (CDI; [22]) (2 excluded), (c) Primary caregivers (i.e., house-parents in the children’s units) had completed the Child Behavior Checklist (CBCL) (7 excluded), and (d) background information regarding the child’s psychosocial history was available in the file (2 excluded). Two-hundred and forty-one children were excluded based on the above mentioned criteria. There were no significant differences on clinical (e.g. abuse type) or demographic variables (e.g., ethnicity) for the children included versus the children excluded from this study. The sample consisted of 44.7% females, with an ethnic breakdown of 54.7% Caucasian, 24.5% African American, 6.3% Hispanic and 14.5% Biracial/Other and an age range of 8–17 with a mean age of 10.89 years (SD = 2.23 years). Measures were administered by a trained clinician between 3 and 6 months after the child was admitted. For children that had been admitted, released, and readmitted, data were used from their initial assessment battery.
Measures
Childhood Background Information
Childhood background information was obtained through psychosocial write-ups found in each child’s file. The psychosocial reports were comprised of comprehensive accounts of the children’s history and background based on a multi-informant collaboration of individuals and service providers involved with the child. Assessments were taken within 30 days after admission to the residential facility and recorded by trained clinicians. Information provided in the psychosocial reports included the child’s demographic information (age, sex, gender, ethnicity), number of placements, documented trauma history and perpetrator, educational background and status, as well as significant medical and/or psychiatric histories of the child, his/her biological mother, father, and sibling(s).
Child Behavior Checklist (CBCL; [23])
The CBCL is a 118-item parent or primary caregiver report of their child’s behavior. Parents/primary caregivers respond to each question utilizing a 3-point Likert scale (0 = not true, 1 = somewhat or sometimes true, 2 = very or often true). Eight subscales are derived from the 118 questions and include anxiety/depression, withdrawn behaviors, somatic complaints, social problems, attention problems, thought problems, delinquent behaviors and aggressive behaviors. Internalizing, externalizing and total scores are generated. The CBCL is a widely used behavior scale with good psychometric properties [23] including strong discriminant and predictive validity [24, 25].
Children’s Depression Inventory (CDI; [22])
The CDI is a child-report measure that asks children to rate the presence and severity of 27 symptoms of depression. The child is presented with three statements and asked to circle the statement that best expresses how they have felt over the last 2 weeks (i.e. “I am sad once in a while” “I am sad many times” “I am sad all the time”). Individual items range in score from 0 to 2 ultimately producing a total summed score of 0–54. Additionally, the CDI produces scores for five subscales including negative mood, interpersonal problems, ineffectiveness, anhedonia and negative self-esteem. The CDI has sound psychometric properties including good test–retest reliability, predictive validity, internal consistency and construct validity [22, 26, 27].
Multidimensional Anxiety Scale for Children (MASC; [20])
The MASC is a child-report measure that consists of 39-items addressing various symptoms of anxiety. Scores are rated on a 4-point Likert scale (0 = never, 1 = sometimes, 2 = often, 3 = always). The MASC yields a total score derived from the sum of all items as well as four subscale scores, three of which are further divided into two sections each: physical symptoms (somatic symptoms and tense symptoms), social anxiety (humiliation fears and performance fears), harm avoidance (perfectionism and anxious coping) and separation/panic. The MASC has good psychometric properties including test–retest reliability, convergent and divergent validity [20, 28, 29].
Trauma Symptom Checklist for Children (TSCC; [21])
The TSCC is 54-item child-report measure of trauma-related symptoms in children. Items are answered using a 4-point Likert scale (where 0 = never, 1 = sometimes, 2 = lots of times, and 3 = almost all of the time). Symptomatology is measured in 10 domains: Anxiety, Depression, Anger, Overt-Dissociation, Dissociation, Dissociation-Fantasy, Posttraumatic Stress Symptoms, Sexual Concerns, Sexual Distress, Sexual Preoccupation and Validity of responses (both Underresponse and Hyperresponse). The TSCC has strong psychometric properties including convergent and discriminant validity [30], internal consistency and predictive validity [31, 32].
Somatic Symptoms Measures
Similar to Ginsburg et al. [16] and Storch et al. [17], two composite measures of SS were formed to represent both child- and caregiver-rated SS. The child-rated measure was derived by summing the 12 items on the MASC that assessed SS. The primary caregiver-rated measure was compiled by summing the 9 items of the CBCL that addressed SS. Similar to Storch et al. [17], we believed that creating separate composite measures for child- and caregiver-rated SS would provide valuable information regarding the consistencies and differences in multi-informant reporting of SS. Cronbach’s alpha for child- and primary caregiver-rated SS were 0.82 and 0.62, respectively.
Procedure
Children living in the residential facility were administered the above measures and other instruments not germane to this investigation 3–6 months after they were admitted. For the purposes of this study, all files collected between 1996 and 2011 in the archives of the residential facility were examined. The CBCL was completed utilizing a primary caregiver model in which the child’s “house parent” filled out the measure.
Analytic Plan
Independent samples t-tests were used to examine group differences on child-rated and caregiver-rated SS as a function of gender and type of trauma (presence/absence of physical abuse, emotional abuse, sexual abuse, neglect, abandonment, and witnessing of domestic violence was used because children may have experienced multiple abuse types). Pearson correlations were used to examine associations between child- and caregiver-rated SS, as well as relationships between SS and age at assessment, time in years since removal from home, TSCC anxiety, depression, posttraumatic stress, anger and dissociation subscales, and CDI total score.
Mediational analyses addressed whether anxiety as measured by the TSCC mediated the relationship between abuse type and SS. This analysis was first completed with the child-rated composite measure of SS as the outcome and second with the caregiver-rated measure of SS as the outcome. Using the bootstrapping mediation method, the provided sample was resampled k = 5,000 times generating a 95% confidence interval. Bootstrapping involves the repeated random resampling from the data with replacement, which yields an estimation of the indirect effect of the mediator. Replacement allows for a new sample of size n to be determined by sampling cases from the original sample. The criterion for mediation was the exclusion of zero between the lower and upper bound of the confidence interval. If zero was not present it indicated that the indirect effect of the mediator on the outcome was not zero with 95% confidence [33].
Results
Clinical Characteristics
Rates of SS were high with 95.2% of children endorsing at least one SS on the child-rated measure and 80.7% experiencing at least one SS as indicated by the caregiver-rated measure. Independent samples t-tests revealed a significant group difference on child-rated SS between children who had experienced sexual abuse as compared to those who had not (t(159) = 2.69, p < 0.01). No group difference was noted for presence/absence of sexual abuse on caregiver-rated SS. No group differences were found for children with the presence/absence of physical abuse, emotional abuse, neglect, abandonment or witnessing of domestic violence.
Independent samples t-tests revealed gender differences on total scores for the child-rated measure of SS (t(159) = 2.20, p < 0.05; d = 0.35), but not for the caregiver-rated measure of SS (t(159) = 0.67, p = 0.50; d = 0.10). Additionally, on the child-rated measure of SS, gender differences were found for individual items including dizziness (t(159) = 2.67, p < 0.01; d = 0.41) and feeling sick to the stomach (t(159) = 2.38, p < 0.05; d = 0.38), with females endorsing higher rates of both symptoms as compared to males (Table 1). On the caregiver-rated measure of SS, gender differences were noted for individual items including restlessness (t(159) = − 2.48, p < 0.05; d = 0.40), dizziness (t(159) = 2.05, p < 0.05; d = 0.31), nausea (t(159) = 2.05, p < 0.05; d = 0.30), stomachaches (t(159) = 2.50, p < 0.05; d = 0.38), and vomiting (t(159) = 2.28, p < 0.05; d = 0.34), with males experiencing higher rates of restlessness and females exhibiting higher rates of dizziness and gastrointestinal symptoms (Table 2).
Pearson correlations revealed that age at assessment was negatively correlated with child-rated SS (r = − 0.21, p < 0.01) but positively correlated with caregiver-rated SS (r = 0.17, p < 0.05). Child-rated SS were positively correlated with CDI total score (r = 0.50, p < 0.01) and the TSCC subscales of anxiety (r = 0.57, p < 0.01), depression (r = 0.62, p < 0.01), posttraumatic stress (r = 0.56, p < 0.01), dissociation (r = 0.59, p < 0.01) and anger (r = 0.40, p < 0.01). No further significant correlations with the CDI total score or TSCC subscales were found with the caregiver-rated SS measure (Table 3).
Mediational Analyses
Two mediational analyses were conducted in which the independent variable was sexual abuse (presence/absence), the mediating variable was the TSCC anxiety subscale, and the dependent variable was either child- or caregiver-rated SS. Bootstrapping confidence intervals revealed that the TSCC anxiety subscale mediated the relationship between sexual abuse and child-rated SS (−1.81; 95% CI −3.64 to −0.37) but did not for caregiver-rated SS (−0.03; 95% CI −0.24 to 0.06). The mediation model accounted for 33% of the variance in child-reported SS, but only 0.96% of the variance in caregiver-reported SS.
Discussion
Overall, the present findings reflect on the frequency and characteristics of SS in traumatized children. Specifically, most youth in this sample (95.2%) self-reported at least one SS and over 80% of caregivers reported that children experienced at least one SS. Over 55% of youth endorsed feeling tense/uptight, jumpy, sick to their stomach, and/or having sweaty hands. These findings must be interpreted with caution as no measure of lie detection was utilized to ensure that children and caregivers were accurately reporting the presence of SS. Clinical characteristics of SS revealed significant gender differences on child-reported total SS. Of note, dizziness and gastrointestinal symptoms were reported more often in females relative to males on both child-reported and caregiver-reported measures of SS. This difference may be indicative of a physiological sensitivity of anxious females over males to experience and express dizziness and gastrointestinal distress, which has been found by others [17]. It is also possible that girls are more willing to express, whether through child-report or to caregivers, that they are experiencing SS [34]. Caregiver-reports of SS indicated that males experienced higher rates of restlessness as compared to females. This specific SS may reflect on males’ trauma-related coping techniques as well as males’ tendency towards heightened externalizing symptoms after trauma exposure [35]. Interestingly, no significant gender difference was noted for total caregiver-rated SS, highlighting a possible and essential difference between self- and caregiver-reported measures for SS. This finding may be reflective of a shared posttraumatic experience across genders, indicating that males and females may appear quite similar in terms of physiological responses to traumatic events. Additionally, this finding—and the modest difference in rates of SS reported between children and non-parent caregivers—may be due to children not reporting SS to caregivers, adult respondents not being aware of such symptoms, and/or that children are more accurate reporters of internalizing symptoms relative to caregivers [36].
Consistent with findings of high prevalence of SS in youth following sexual abuse [18], differences were noted when comparing child-reported SS in children who had or had not experienced sexual abuse. One explanation for the high rates of SS in children who have experienced sexual abuse involves the experience of a heightened sense of health anxiety [9]. This concept reflects on trait anxiety sensitivity theory in that the fear of negative sensations associated with anxiety result in a heightened awareness of arousal symptoms. In turn, health anxiety related to these arousal symptoms may increase stress-related physiological reactions, yielding even more SS. No differences were noted when comparing the presence/absence of physical abuse, emotional abuse, neglect, abandonment or witnessing of domestic violence on child-reported or caregiver-reported SS; additionally, no group differences were noted for sexual abuse presence/absence and caregiver-reported SS. These findings may reflect on a variation in symptom cluster experiencing for children following various types of trauma. Specifically, children who have experienced neglect and non-sexual abuse may experience high rates of re-experiencing and avoidance symptoms and lower rates of hyperarousal symptoms, thereby not relating to an increase in SS.
Correlational findings highlight other factors related to SS in traumatized children. Interestingly, opposite effects, albeit both modest in magnitude, were noted for age at assessment and child-reported versus caregiver-reported SS. On the child-reported measure of SS, age was negatively correlated with rates of SS, yet on the caregiver-report measure of SS age was positively correlated with rates of SS. Younger children may be more likely to honestly report symptoms that may be embarrassing or private, such as having gastrointestinal distress. Alternatively, caregivers may be better attuned to older children’s SS as older youth may refrain from activities due to the experience of SS.
The discrepancy between child- and non-parent caregiver-reported SS as indicated by many study findings may be explained in several ways. First, caregivers may not be accurate reporters of internalizing symptoms in children and adolescents relative to the youngster him/herself [36]. Second, children may be reluctant to express complaints of SS to caregivers, especially in a sample of abused children who may not have trusting relationships with adults and who may not have formed close relationships with their relatively new and temporary caregivers [37]. Third, the limited findings for caregiver-rated SS may reflect the low internal consistency of the caregiver-rated measure. Finally, caregivers may be attuned to behaviors and symptoms such as aggression that warrant immediate interventions to keep children safe in their residential settings. This in turn, may interfere with caregivers’ ability to recognize or attend to symptomatic expressions of trauma (e.g., SS, anxiety, sadness) that do not cause significant disruption to the home environment.
Large direct associations were noted between child-rated SS and the CDI total score, the TSCC anxiety subscale, the TSCC depression subscale, the TSCC posttraumatic stress subscale, the TSCC dissociation subscale and the TSCC anger subscale. These relationships may be understood in several ways. First, anxiety and depressive symptoms in traumatized youth may also manifest themselves as SS. Indeed, diagnostic criteria for anxiety and depressive disorders include robust somatic domains such as symptoms related to sleep, appetite, restlessness, and muscle tension. Therefore, children who are experiencing significant anxiety and depression posttrauma may exhibit high rates of SS. These findings raise the question of whether SS change as a function of treatment for anxiety, depression and posttraumatic stress with some evidence for reductions in SS with psychopharmacological (i.e., selective serotonin reuptake inhibitors; SSRIs) or psychotherapeutic (i.e., cognitive-behavioral therapy; CBT) interventions [16, 17]. Second, consistent with previous research, symptoms of dissociation following trauma are highly associated with SS [38–41]. Third, it is possible that relations are a product of shared method or source variance. No significant correlations were noted between clinical characteristics and caregiver-rated SS. This finding may highlight children’s ability to report more accurately on internalizing symptoms relative to caregivers [36] and/or that children may not be reporting SS or anxiety and depression to their non-parent caregivers.
Mediation analyses found that child reported anxiety mediated the relationship between sexual abuse and child-rated SS, but not caregiver-rated SS. Of note, this finding highlights the role of anxiety in the presence of SS and provides further evidence for the concept of trait anxiety sensitivity as an essential aspect in the experience of SS following trauma. This mediational model may suggest that the experience of sexual abuse relates to heightened health-anxiety (or the fear of consequences related to SS) as children become more attuned to symptoms of hyperarousal; this in turn predisposes the child to higher rates of SS. It is important to fully understand the route of expression of SS in children to tailor interventions to address these symptoms. Treatments aimed at the amelioration of posttraumatic symptomology must factor in the essential role of anxiety in the expression of SS. For example, cognitive-behavioral therapeutic approaches that focus on addressing traumatic anxiety may also work to reduce SS. Additionally, healthcare providers should be aware of the potential presence of SS following traumatic events in childhood. An awareness and attention to SS in traumatized children may: 1), allow for the proper treatment of posttraumatic physiological sequelae and 2), prevent children from undergoing invasive and unnecessary medical testing. Additionally, implications regarding discrepancies presented in health care settings must be considered by health care professionals. It is evident that differences between self- and caregiver- reports are prevalent, pointing to the importance of utilizing a multi-modal and multi-informant approach to understanding somatic symptoms in traumatized youth. Additionally, a multi-informant assessment of somatic symptoms may yield a more accurate clinical picture and allow for the application of appropriate interventions. Ultimately, SS are highly prevalent in children following traumatic events and reflect a need for tailored treatments aimed at the attenuation of SS.
Limitations
This study is not without limitations. First, we utilized unstandardized child- and caregiver-report measures of SS derived from standardized measures of behavior and anxiety in children. Second, it was not possible to ascertain whether children had organic physical problems that may cause rates of SS to occur. Third, certain SS were not measured by both child- and caregiver-reported measures of SS. Forth, no measure of lie detection was utilized and therefore complete validation of self- and caregiver- reported somatic symptoms is not possible. Findings must therefore be interpreted with caution. Finally, children’s history of abuse was based on documented cases only. In the child welfare system, children are exposed to myriad of traumatic events, and it is therefore impossible to determine additional undocumented traumas. Within these limitations, this study contributes to the literature by examining SS in a large, diverse sample of children who had been exposed to varied traumas.
Summary
Childhood exposure to trauma has been associated with increased rates SS, which may contribute to diminished daily functioning. Trait anxiety theory posits that children who exhibit high anxiety sensitivity may fear the negative sensations associated with anxiety and therefore be more highly attuned to arousal symptoms. One hundred and sixty-one children residing at a residential treatment group home who had experienced neglect, abandonment, physical, emotional, and/or sexual abuse were administered the TSCC, the MASC, and the CDI shortly after their admission. Primary caregivers (i.e., direct care staff in the children’s cottages) completed the CBCL. Two composite measures of SS were formed to represent both child- and caregiver-rated SS. The child-rated measure was derived by summing the 12 MASC items that assessed SS, and the primary caregiver-rated measure was compiled by summing the 9 CBCL items that addressed SS. Over 95% of children endorsed at least one SS on the child-rated measure. Children who had experienced sexual abuse had higher rates of SS relative to children who had not. Gender differences were found for overall child-rated SS, as well as for individual SS on both the child- and caregiver-rated measures. Child-rated SS were highly correlated with the CDI total score and the TSCC subscales of anxiety, depression, posttraumatic stress, dissociation, and anger. The TSCC anxiety subscale mediated the relationship between sexual abuse and child-rated SS. These findings highlight the prevalence of SS following childhood trauma, as well as demographic and clinical characteristics related to SS. Identifying SS following childhood trauma is essential to understanding a complete clinical picture of posttraumatic reactions. Additionally, treatments previously focused on solely psychological outcomes of trauma should take into account the distress and impairment related to SS.
References
Hensley L, Varela R (2008) PTSD symptoms and somatic complaints following Hurricane Katrina: the roles of trait anxiety and anxiety sensitivity. J Clin Child Adolesc Psychol 37:542–552
Nader KO, Fairbanks LA (1994) The suppression of reexperiencing: impulse control and somatic symptoms in children following traumatic exposure. Anxiety Stress Coping 7:229–239
Sesar K, Simic N, Barisic M (2010) Multi-type childhood abuse, strategies of coping, and psychological adaptations in young adults. Croat Med J 51:406–416
Campo JV, Jansen-McWilliams L, Comer DM, Kelleher KJ (1999) Somatization in pediatric primary care: association with psychopathology, functional impairment, and use of services. J Am Acad Child Adolesc Psychiatry 38:1093–1101
Carlsson J, Larsson B, Mark A (1996) Psychosocial functioning in schoolchildren with recurrent headaches. Headache 36:77–82
Robinson JO, Alverez JH, Dodge JA (1990) Life events and family history in children with recurrent abdominal pain. J Psychosom Res 34:171–181
Dorn LD, Campo JC, Thato S, Dahl RE, Lewin D, Chandra R, Di Lorenzo C (2003) Psychological comorbidity and stress reactivity in children and adolescents with recurrent abdominal pain and anxiety disorders. J Am Acad Child Adolesc Psychiatry 42:66–75
Spertus IL, Yehuda R, Wong CM, Halligan S, Seremetis SV (2003) Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice. Child Abuse Negl 27:1247–1258
Stein MB, Lang AJ, Laffaye C, Satz LE, Lenox RJ, Dresselhaus TR (2004) Relationship of sexual assault history to somatic symptoms and health anxiety in women. Gen Hosp Psychiatry 26:178–183
Vijayakumar L, Kannan GK, Daniel SJ (2006) Mental health status in children exposed to tsunami. Int Rev Psychiatry 18:507–513
Maluccio AN (2006) The nature and scope of the problem. In: Webb NB (ed) Working with traumatized youth in child welfare. The Guildford Press, New York, pp 3–12
APA (2000) Diagnostic and statistical manual of mental disorders (4th-TR). American Psychiatric Association, Washington, DC
Kaminer D, Seedat S, Stein DJ (2005) Post-traumatic stress disorder in children. World Psychiatry 4:121–125
Cameron M, Elkins J, Guterman N (2006) Assessment of trauma in children and youth. In: Webb NB (ed) Working with traumatized youth in child welfare. The Guilford Press, New York, pp 53–66
Asmundson GJ, Coons MJ, Taylor S, Katz J (2002) PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry 47:930–937
Ginsburg GS, Riddle MA, Davies M (2006) Somatic symptoms in children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry 45:1179–1187
Storch EA, Merlo LJ, Keeley ML, Grabill K, Milsom VA, Geffken GR, Goodman WK (2008) Somatic symptoms in children and adolescents with obsessive-compulsive disorder: associations with clinical characteristics and cognitive-behavioral therapy response. Behav Cogn Psychother 36:283–297
Rimsza ME, Berg RA, Locke C (1988) Sexual abuse: somatic and emotional reactions. Child Abuse Negl 12:201–208
Bailey BN, Delaney-Black V, Hannigan JH, Ager J, Sokol RJ, Covington CY (2005) Somatic complaints in children and community violence exposure. J Dev Behav Pediatr 26:341–348
March JS, Parker JD, Sullivan K, Stallings P, Conners CK (1997) The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry 36:554–565
Briere J (1996) Trauma symptom checklist for children (TSCC). Psychological Assessment Resources, Odessa
Kovacs M (1992) The Children’s Depression Inventory manual. Multi-Health Systems, Inc., North Tanawanda
Achenbach TM (1991) Manual for the child behavior checklist/4-18 and 1991 profile. University of Vermont Department of Psychiatry, Burlington
Aschenbrand SG, Angelosante AG, Kendall PC (2005) Discriminant validity and clinical utility of the CBCL with anxiety-disordered youth. J Clin Child Adolesc Psychol 34:735–746
Pauschardt J, Remschmidt H, Mattejat F (2010) Assessing child and adolescent anxiety in psychiatric samples with the Child Behavior Checklist. J Anxiety Disord 24:461–467
Figueras Masip A, Amador-Campos JA, Gomez-Benito J, del Barrio Gandara V (2010) Psychometric properties of the Children’s Depression Inventory in community and clinical sample. Span J Psychol 13:990–999
Timbremont B, Braet C, Dreessen L (2004) Assessing depression in youth: relation between the Children’s Depression Inventory and a structured interview. J Clin Child Adolesc Psychol 33:149–157
Baldwin JS, Dadds MR (2007) Reliability and validity of parent and child versions of the multidimensional anxiety scale for children in community samples. J Am Acad Child Adolesc Psychiatry 46:252–260
March JS, Sullivan K (1999) Test-retest reliability of the Multidimensional Anxiety Scale for Children. J Anxiety Disord 13:349–358
Lanktree CB, Gilbert AM, Briere J, Taylor N, Chen K, Maida CA, Saltzman WR (2007) Multi-informant assessment of maltreated children: convergent and discriminant validity of the TSCC and TSCYC. Child Abuse Negl 32:621–625
Lanktree CB, Briere J (1995) Outcome of therapy for sexually abused children: a repeated measures study. Child Abuse Negl 19:1145–1155
Sadowski C, Friedrich WN (2000) Psychometric properties of the Trauma Symptom Checklist for Children (TSCC) with psychiatrically hospitalized adolescents. Child Maltreat 5:364–372
Hayes AF (2009) Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr 76:408–420
Kelly C, Molcho M, Doyle P, Gabhainn SN (2010) Psychosomatic symptoms among schoolchildren. Int J Adolesc Med Health 22:229–235
Leadbeater BJ, Kuperminc GP, Blatt SJ, Hertzog C (1999) A multivariate model of gender differences in adolescents’ internalizing and externalizing problems. Dev Psychol 35:1268–1282
Sourander A, Helstela L, Helenius H (1999) Parent-adolescent agreement on emotional and behavioral problems. Soc Psychiatry Psychiatr Epidemiol 34:657–663
Crenshaw DA, Hardy KV (2006) Understanding and treating the aggression of traumatized children in out-of-home care. In: Webb NB (ed) Working with traumatized youth in child welfare. The Guilford Press, New York, pp 171–195
Anderson G, Yasenik L, Ross CA (1993) Dissociative experiences and disorders among women who identify themselves as sexual abuse survivors. Child Abuse Negl 17:677–686
Dimoulas E, Steffian L, Steffian G, Doran AP, Rasmusson AM, Morgan C (2007) Dissociation during intense military stress is related to subsequent somatic symptoms in women. Psychiatry (Edgmont) 4:66–73
Diseth TH (2006) Dissociation following traumatic medical treatment procedures in childhood: a longitudinal follow-up. Dev Psychopathol 18:233–251
Saxe GN, Chinma G, Berkowitz R, Hall K, Lieberg G, Schwartz J, van der Kolk BA (1994) Somatization in patients with dissociative disorders. Am J Psychiatry 151:1329–1334
Author information
Authors and Affiliations
Corresponding author
Additional information
The contributions of Samantha Nagy, B.A. are greatly appreciated.
Rights and permissions
About this article
Cite this article
Kugler, B.B., Bloom, M., Kaercher, L.B. et al. Somatic Symptoms in Traumatized Children and Adolescents. Child Psychiatry Hum Dev 43, 661–673 (2012). https://doi.org/10.1007/s10578-012-0289-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-012-0289-y