Abstract
This study utilized parent ratings and self-report in assessing symptoms in children exposed to domestic violence, and in some cases, physical abuse. Data were collected from 83 parents and children in a domestic violence shelter. Children, ages 8–16, completed a questionnaire regarding exposure to physical abuse/DV and the TSCC—Alternate form (TSCC-A; Briere 1996). Parents of children, ages 3–12, completed the Trauma Symptom Checklist for Young Children (TSCYC; Briere 2005). Parent t-scores on were higher than matched t-scores for child self-report. Parent scores on most clinical scales were higher for Caucasian than non-Caucasian parents. Female children were rated as more depressed by their parents than males. Symptoms scores were positively correlated with the observation and experience of domestic violence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An estimated 3.3–10 million children live in households with domestic violence (DV; Carlson 1994; Strauss 1992). While definitions and terms associated with DV may include acts along a continuum from being psychologically abused to being battered in long-term abusive relationships, the definition here is partner-to-partner violence witnessed by children, rather than violence inflicted upon children. While studies have been done on the effects of DV on women’s health (Campbell 2002; Campbell and Lewandowski 1997), employment (Lindhorst et al. 2007; Lloyd 2002), and psychological functioning (e.g., Bonomi et al. 2006), relatively little is known about the psychological impact on children (Fantuzzo et al. 1997). Historically, the measures/instruments used in many studies have not been designed to assess symptoms commonly experienced by children exposed to trauma (Van Horn and Lieberman 2004).
This review and study will address symptoms (including trauma-related symptoms in children exposed to DV, as well as differences in symptom presentations based on demographic variables (e.g., race and sex). It also will address polyvictimization and dose-related effects, specifically witnessing the DV perpetrated against a parent plus a child’s own physical abuse.
Symptom Assessment
The extant literature suggests that children exposed to DV experience internalizing (Cummings et al. 1991; Kernic et al. 2003; McFarlane et al. 2006), as well as externalizing and combined symptoms (McFarlane et al. 2006). Holt et al. (2008) reviewed the literature examining the impact of DV on children from 1995 to 2006. They concluded that children exposed to DV are at increased risk of experiencing emotional and behavioral problems. Conversely, Grych et al. (2000) reported that 31 % of children exposed to DV did not exhibit any signs of maladjustment, and that about 30 % developed both externalizing and internalizing symptoms, 21 % developed externalizing symptoms only, and 18 % developed internalizing symptoms only. However, it should be noted that no measures of posttraumatic stress were included in their study. Johnson et al. (2002) used portions of the Trauma Symptom Checklist for Children (TSCC) and found that DV and/or physical abuse (PA) were significant predictors of child-reported anger and parent-reported aggression (PA and child-reported witnessing of violence), parent-reported depression (PA, child- and parent-reported witnessing of violence), child-reported depression (child-reported witnessing of violence), and self-reports of anxiety (child- and parent-reported witnessing of violence by the child). However, PTSD/dissociative symptoms were not examined. Evans et al. (2008) performed a meta-analysis of 60 studies. They included both published and unpublished studies in order to offset the problem of publication bias. Results supported the association between exposure to DV and internalizing, externalizing, and trauma symptoms. However, of the 61 samples included in the meta-analysis, only six studies assessed trauma in any fashion. They did not find a difference between boys and girls for externalizing symptoms, but did find that for girls, the association with internalizing behaviors was stronger than for boys. They also found that the strength of these relationships was similar regardless of samples (i.e., clinical settings, battered women’s shelters, community settings, or school settings). The authors conclude that:
Even the examination of trauma symptomatology, despite being the strongest outcome in the present meta-analysis, was limited to a small number of studies (k = 6). This dearth is especially concerning given the strong theoretical links between exposure to violence and PTSD related symptoms (Kilpatrick and Williams 1998; Margolin and Vickerman 2007) (Evans et al. 2008, p. 137).
Based on the Evans et al. (2008) meta-analysis, the Grych et al. study (2000) and the Johnson et al. (2002) studies, it would appear that trauma-related symptoms as a possible outcome for children witnessing DV has been largely ignored. Since DV likely represents a traumatic experience for child witnesses, it is logical to assess PTSD and dissociative symptoms. Moreover, according to some authors, posttraumatic stress has recently emerged as a unifying construct for understanding the impact on children of DV (Graham-Bermann 2001; Wekerle et al. 2006).
Demographic Variables
O’Keefe (1994a, b) has reported ethnic differences in behavior problems and social competence of children exposed to DV. That is, White children, especially boys, have greater externalizing behavior problems than African American children. Also, African-American mothers reported greater social competence in their children than mothers of White and Hispanic groups.
Spilsbury et al. (2007) assessed the associations of characteristics of DV incidents with clinically significant levels of traumatic symptoms and behavioral problems in 687 children participating in a community-service program for children witnessing violence. Results demonstrated that perceived threat and control were associated with greater odds of clinically significant levels of several trauma symptoms (and behavior problems in the case of perceived threat) after controlling for demographic factors and violence characteristics. Female sex and White ethnicity increased the odds of some trauma symptoms and behavior problems. Increasing age reduced odds of some trauma symptoms.
Tonelli (2002) examined the relationship between genders and self-reports of PTSD symptoms related to their exposure to DV in 75 treatment-seeking adolescents. No gender differences were found in regards to either PTSD symptomatology (as measured by the TSCC) or internalizing and externalizing behaviors (as measured by the Achenbach Youth Self-Report).
Dose Effects and Polyvictimization
Grethel (2005) examined the relationship between the severity of child symptoms and (a) severity of DV exposure, (b) child abuse history, and (c) psychosocial stressors. The findings of this study suggest that children exposed to more severe DV as measured by the Conflict Tactics Scale had higher rates of aggressive behavior, attentional difficulties, anxiety, depression, and dissociative symptomatology, as measured by the Child Behavior Checklist (CBCL) and the Trauma Symptom Checklist for Children, than those exposed to less severe DV. The study also found that children with co-occurring child abuse and exposure to DV were more likely to have dissociative symptoms. Additional research in this area is needed.
Children exposed to domestic violence may experience multiple forms of maltreatment or interpersonal traumas. Terms used to describe the co-occurrence of potentially abusive/traumatic events have included complex trauma (Cook et al. 2005), polvictimization (Ford et al. 2011), and cumulative adversity (Seery et al. 2010). Common traumatic or abusive events co-occurring include physical abuse, witnessing DV perpetrated against and/or by a parent, sexual abuse, emotional abuse, and neglect. Greeson et al. (2011) in a study of 2251 children found that for a subsample (n = 1584) experiencing complex trauma, the average number of traumatic events was 5.8 (SD = 2.1). Moreover, 72 % of their sample witnessed DV, 64 % experienced physical abuse, and 42 % experienced sexual abuse.
Ellens (2009) collected data from 93 mother-child pairs who were receiving services at a non-profit child abuse agency. Participants were categorized into either: (a) children who witnessed DV, but were not physically abused (witnesses only), and (b) children who witnessed DV and were also physically abused (abused witnesses). Child symptoms were measured using both the Child Behavior Checklist (Achenbach 1991) and the Trauma Symptom Checklist for Children (Briere 1996). Children from the abused witnesses group did not evidence more symptoms than children from the witnesses-only group as measured by both parental and child self-report data.
Conversely, Hughes et al. (1989) and Kernic et al. (2003) found that children who witness DV and who are themselves abused exhibit greater behavior problems than those witnessing violence only. Others have found that there is a graded or dose–response relationship between the number of types of childhood adverse experiences (e.g., child abuse, witnessing of violence directed towards mother) and both risk behavior (e.g., drug use, smoking) and disease (ischemic heart disease, cancer, skeletal fractures) in adulthood (Edwards et al. 2003; Felitti et al. 1998).
Levendosky et al. (2002) studied PTSD symptoms in 62 children (39 witnessed DV as per mother reports; 23 were living in the home when the DV occurred, but did not observe DV based on mother reports). Two purported measures of PTSD were used. The first was the PTSD scale from the CBCL, developed by Wolfe, Gentile, and Wolfe (1989). This scale accurately classifies PTSD-negative children, but does less well in accurately classifying PTSD-positive children. The second measure was an 18-item scale of PTSD symptoms developed for the study based on the DSM-IV criteria for PTSD symptoms, with the addition of symptoms relevant to young children’s traumatic responses. All children experienced at least one symptom of trauma, but only 3 % or 24 % of the children, depending on the measure used, met criteria for PTSD based on the DSM-IV. Children with re-experiencing trauma symptoms also exhibited more externalizing behavior problems.
Assessment of Exposure to DV
Children report differently than parents and other informants. For example O’Brien, John, Margolin, and Erel (1994) found that when one or both parents denied any exposure to DV for their children, 21 % of children were able to provide detailed descriptions of DV. Thus, it is important to assess children’s reports of exposure to DV.
Summary
Studies that examine differences by sex have found no differences in symptoms of externalizing problems as assessed by the CBCL (e.g., Evans et al. 2008; Tonelli 2002). Some of the same studies have found no difference for internalizing problems (i.e., Evans et al. 2008; Tonelli 2002). Tonelli (2002) also found that there were no differences by sex for trauma symptoms. However, Spilsbury et al. (2007) found that females exhibited more behavior problems and trauma symptoms. Dose effects for trauma have been found (Grethel 2005), and exposure to DV plus other forms of maltreatment are associated with more symptoms (Ellens 2009; Hughes et al. 1989; Kernic et al. 2003; Levendosky et al. 2002).
Spilsbury et al. (2007) reported that as age increased, symptoms of trauma decreased. Evans et al. (2008) also found no differences in symptomatology based on setting (e.g., community vs. shelter). Finally, only O’Keefe (1994a, b) and Spilsbury et al. (2007) reported differences associated with race indicating that white children exhibited more externalizing behavior (O’Keefe 1994a, b; Spilsbury et al. 2007) and trauma symptoms (Spilsbury et al. 2007).
Thus, the purpose of this study was to utilize both parent ratings and self-report in assessing behavioral, emotional, and trauma symptoms in children exposed to DV and abuse. Issues of sex, race, and age were examined along with dose effects. Finally, agreement between reports/knowledge of mothers and children for physical abuse of children was examined.
Method
Procedure
Data were collected from parents and children in a DV shelter. Consent and assent were obtained as per IRB guidelines. Children, ages 8-16, completed The Health Resiliency Intervention for Violence Exposure (THRIVE): Student Screening Questionnaire (Goodkind 2004) regarding exposure to phyical abuse/DV. Parents were asked about a history of physical/sexual abuse in their children using the Abuse Dimensions Inventory (ADI; Chaffin et al. 1997). Children, ages 8–16, completed the TSCC—Alternate form (TSCC-A; Briere 1996). Parents of children, ages 3–12, completed the Trauma Symptom Checklist for Young Children (TSCYC; Briere 2005). Not all children completed all measures since some measures were standardized using a limited age range.
The parent and child were approached independently and asked if they would volunteer to participate in a study. As noted above, assent and consent were obtained from children and parents, respectively. There was no compensation offered for their participation since the information provided had the potential to benefit the clients’ treatment.
Participants
The children (n = 83; mean age = 9.83, SD = 2.96) were female (39.5 %) and male (60.5 %); ethnicity of the sample was Latino (44 %), African American (17 %), Caucasian (19 %), and Biracial (20 %). All informants (children and their corresponding parent) were English-speaking. Not all measures were completed by or for each child due to non-overlapping age requirements (e.g., the self-report measure, TSCC-A, [ages 8–12] and the caregiver rating, TSCYC [ages 2–12]) or due to the refusal to complete some items in part or whole.
Measures
The Health Resiliency Intervention for Violence Exposure (THRIVE): Student Screening Questionnaire
(Stein et al. 2003). Only nine items from the longer Recent Exposure to Violence Scale were used. This 9-item version was adapted by Stein et al. (2003) and can be found in Table 1. The Student Screening Questionnaire asks children to rate the frequency of specific violent actions either observed or experienced in a family setting. Goodkind (2004) reported Cronbach’s alpha scores ranging from 0.67 to 0.86 across four points in time. Internal consistency was calculated for all nine items from the current study and yielded a Cronbach’s alpha of 0.69—approximating a score in the acceptable range. The THRIVE was administered to children ages 8 and above, though several children, age 7, were proficient readers and completed the measure. Due to the age distribution, there were 25 participants who did not complete the THRIVE, and another 4 who provided answers to only some items. Allegations by the child of physical abuse were reported to the agency staff and discussed prior to hotline reports. The agency did not allow the researchers to inquire of the child about a potential history of sexual abuse.
The Trauma Symptom Checklist for Young Children (TSCYC; Briere 2005)
The TSCYC, developed by Briere in 1999 and published in 2005, is a 90-item parent report measure for the assessment of trauma-related symptoms in children ages 3 to 12. There were 65 children between the ages of 3 and 12; however, 60 mothers completed the TSCYC to describe their behavior. The clinical scales include Posttraumatic Stress – Intrusion, Posttraumatic Stress – Avoidance, Posttraumatic Stress – Arousal, Sexual Concerns, Anxiety, Depression, Dissociation, and Anger/Aggression. The scores of the Posttraumatic Stress scales sum to a Posttraumatic Stress – Total scale score. The clinical scales had good reliability with alphas ranging from 0.81 to 0.93. Additionally, TSCYC scales were predictive of exposure to sexual abuse, physical abuse, and witnessing DV. In the current study, the Cronbach alphas for the TSCYC ranged from 0.89 for Dissociation to 0.80 for Anxiety with one outlier. That is the alpha for Sexual Concerns was 0.54.
The Trauma Symptom Checklist for Children-Alternate (TSCC-A; Briere 1996)
The TSCC-A is a standardized, self-report measure for assessing trauma-related symptoms in children ages 8–16. There were 61 children between the ages of 8 and 12, though only 57 completed the TSCC-A. The TSCC-A yields raw scores and T-scores for validity scales and clinical scales. The clinical scales include Anxiety, Depression, Anger, Post-traumatic stress, and Dissociation. The alpha coefficients for clinical scales range from 0.77 to 0.89 in the standardization sample. Adequate convergent, discriminant, and predictive validity have been demonstrated in normative and clinical samples. In this study, the Cronbach alphas ranged from a high of 0.87 (Depression) to a low of 0.77 (Dissociation).
Abuse Dimensions Inventory (ADI; Chaffin et al. 1997)
The ADI is a 15-scale instrument designed to measure the severity of physical and sexual abuse. There are scales measuring abuse severity, duration of abuse, number of most severely rated incidents, number of total incidents, abuser reaction to disclosure, use of force or coercion to gain submission or compliance, use of force or coercion to gain secrecy, and relationship of the abuser to the victim. The ordering of items in terms of severity was obtained by surveying a national sample of mental health professionals belonging to a national abuse organization. Coefficients of concordance for orderings averaged 0.87. Inter-rater reliability of the scales based upon a semi-structured interview with non-accused parents ranged from 0.84 to 0.99, and factor analysis of the instrument produced a four factor solution with separate factors for physical abuse behaviors, sexual abuse behaviors, number and duration of physical abuse events, and number and duration of sexual abuse events (Chaffin et al. 1997). The severity of sexual and physical abuse were the only ADI sections utilized. Parents were asked about the child’s experience of physical abuse and sexual abuse. The participating agency did not allow the children to be asked about their potential experience of sexual abuse. Allegations by the mother of physical abuse of the child were reported to the agency staff and discussed prior to hotline reports.
Analysis Procedure
Although a multiple regression was conducted, the problem of missing data due to non-overlapping ages for administration of certain tests (e.g., the TSCC-A and TSCYC) reduced the numbers for analysis. Additionally, 5 % of the sample of children, age 8 or above, elected to not complete the THRIVE, lowering the number of participants available for the multiple regression. With the five predictor variables, a sample size of approximately 50 would be required to detect even large effect sizes. Medium effect sizes would require approximately 90 participants (Field 2009). The analysis for the TSCC-A as the outcome variable included 49 participants and the analysis of the TSCYC included 35 participants. Thus, separate analyses by age groups, race, and sex were completed.
Results
Experience of Violence
Children described their experience of being threatened, slapped or beaten and reported a mean of 1.87 types of abusive events (SD = 1.92 events) with a range of 0–7 events. Moreover, the computed z-score for skewness was 0.992/0.322 = 3.08 indicating a significant number of low scores (e.g., 18 participants had been threatened, slapped, beaten, etc. on no occasion; i.e., n = 0). Children also reported on other family members being threatened, slapped, beaten, attacked with a knife, threatened with a gun, or shot with a gun and reported a cumulative mean of 1.77 events (SD = 1.89) observed. The percentages for either witnessing or experiencing abusive events are found in Table 1.
Symptoms by Reporter
Parents’ reports of symptoms (t-scores) for their individual child were higher than the matched child self-reports for the scales of Anxiety, Depression, Anger, and PTSD (see Table 2). However, none of the means were in the clinical range.
Agreement Between Parent and Child for Physical Abuse Experienced
Parents were asked about a history of sexual abuse and physical abuse for their children using the Abuse Dimensions Inventory (Chaffin et al. 1997). Children were asked about their experiences of physical abuse using the THRIVE Student Screening (Goodkind 2004). Only seven (7) of 83 parents reported that their child had experienced physical abuse. However, 29 (or 34.9 %) of children reported experiencing physical abuse when the mother did not report. (See Table 3.)
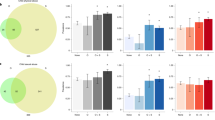
Group Differences by Sex
There were no significant differences in the number of DV events observed, experienced, or combined based on sex. Similarly, there were no differences on the TSCC clinical scales based on sex. For the TSCYC, there were no significant differences on clinical scales based on sex with the exception of Depression. That is, the Depression T-score was higher for females (M = 62.27, SD = 16.56) than for males (M = 53.31, SD = 13.83), t (55) = 2.21, p = .032. Additionally, 22.7 % of females scored in the clinical range for Depression (T score ≥ 65) while only 8.6 % of males scored in the clinical range.
Group Differences by Age
Age was re-coded as young (ages 4–12) or adolescent (age 13 and older). There were no differences between age groups for observed, experienced, or combined violence in the home. There were only three significant differences for the TSCC; for all three scales, younger children reported higher t-scores than their older counterparts. Specifically, younger children reported higher scores on the Hyperresponsive Scale (M = 61.87, SD = 21.57) than their older counterparts (M = 48.15, SD = 5.68), t = 3.90, df = 57.99, p = .000; younger children also reported higher scores on the Anxiety Scale (M = 52.89, SD = 14.90) than their older counterparts (M = 46.23, SD = 5.79), t = 2.47, df = 51.32, p = .011. Younger children also reported higher PTSD Total scores (M = 50.49, SD = 11.81) than their older counterparts (M = 45.75, SD = 5.10), t = 2.09, df = 42.61, p = .042. Since the TSCYC is not administered for children over the age of 12, there were no TSCYC scores to compare by age.
Group Differences by Race
There was no significant difference for the number of DV/abusive events observed, experienced, or combined based on race. However, there were significant differences based on race for scales of the TSCYC including Anxiety, Anger, PTSD Total, and Dissociation Total Specifically, scores for the Caucasian group were higher on the Anxiety Scale (F (3,52) = 6.84, p < .01) and all other races. Post hoc comparisons using the Tukey HSD test indicated that Caucasian (M = 72.50, SD = 16.08) scored significantly higher than African Americans (M = 56.40, SD = 16.45), Latinos (M = 52.73, SD = 10.12), and biracial children (M = 58.05, SD = 14.54).
Scores for the Caucasian group were higher on the TSCYC PTSD Total Scale (F (3,52) = 10.46, p < .001) and all other races. Post hoc comparisons using the Tukey HSD test indicated that Caucasian (M = 76.50, SD = 18.92) scored significantly higher than African Americans (M = 55.10, SD = 15.18), Latinos (M = 52.14, SD = 10.38), and biracial children (M = 52.42, SD = 7.04).
Scores for the Caucasian group were higher on the TSCYC Dissociation Scale (F (3,52) = 3.98, p < .05) and all other races. Post hoc comparisons using the Tukey HSD test indicated that Caucasian (M = 63.00, SD = 9.79) scored significantly higher than African Americans (M = 50.30, SD = 7.72), Latinos (M = 52.18, SD = 12.22), and biracial children (M = 49.50, SD = 11.44). Finally, Caucasians (M = 70.50, SD = 17.68) scored higher on the TSCYC Anger Scale (F (3, 52) = 4.90, p < .01 than Latinos (M = 51.05, SD = 8.69), as per the Tukey HSD post-hoc analysis. (See Table 4.) There were no significant differences based on race for any of the TSCC clinical scales.
Correlations Between Level of Family Violence and TSCC-A/TSCYC Scores
There were 10 correlations (see Table 5), which were significant between symptoms and violence experienced in contrast to violence observed with six. There were seven correlations between experienced violence and self-reported symptoms in contrast to three parent reported, significant correlations. Thus, self-reported symptoms and self-reported violence experienced resulted in the greatest number of significant correlations.
Multiple Regression for Observed and Experienced DV/Physical Abuse on Symptoms
A multiple regression analysis was performed to determine how well the predictor variables of gender, age, race, experienced violence, and witnessed violence predicted symptomatology in children as measured by the clinical scales of the TSCC-A (n = 49) and TSCYC (n = 35). Multicollinearity was assessed by examination of the correlation matrix for the predictor variables, by examination of the variance inflation factors (VIF), and the inspection of the tolerance statistic. The only significant correlation was for experienced violence and witnessed violence, with r = 0.358 (p < .01). This correlation is not surprising since all items are derived from the THRIVE. The VIFs for the multiple regressions ranged from 1.000 to 1.098 for the TSCYC and from 1.000 to 1.166 for the TSCC analyses. The tolerance statistic was 0.911 or higher for the TSCYC analyses and 0.858 or higher for the TSCC analyses—all above the recommended cutoff of 0.2 suggested by Menard (1995).
None of the predictor variables were significant for parent ratings on the TSCYC scales of Anxiety, Dissociation or Sexual Concerns. However, experienced violence was a significant predictor for Total PTSD (F (1, 33) = 5.03, p < .05, accounting for 13.2 % of the variance), Depression (F (1, 33) = 8.99, p < .01, accounting for 21.4 % of the variance), and Anger scores (F (1, 33) = 11.07, p < .01, accounting for 25.1 % of the variance). Ethnicity also significantly predicted Total PTSD scores of the TSCYC (F (1, 29) = 9.12, p < .01), with Caucasians (M = 76.5, SD = 18.92) scoring higher (F (3, 52) = 10.46, p < .001) than African Americans (M = 55.10, SD = 15.18, Latinos (M = 52.14, SD = 10.38), and Biracial children (M = 52.42, SD = 7.04).
For the TSCC-A experiencing violence significantly predicted scores on PTSD (F (1, 47) = 18.02, p < .001, accounting for 27.7 % of the variance), Depression (F (1, 47) = 17.63, p < .001, accounting for 27.3 % of the variance), Anger (F (1, 47) = 19.60, p < .001, accounting for 29.4 %% of the variance), Dissociation (F (1, 45) = 9.44, p < .01, accounting for 16.6 % of the variance), and Anxiety (F (1, 47) = 22.96, p < .001, accounting for 32.8 % of the variance), For PTSD, witnessed violence also accounted for a significant though smaller percentage of the variance (F (1, 46) = 4.54, p < .05, accounting for 6.5 % of the variance). For Anxiety, the child’s age also accounted a significant though smaller percentage of the variance (F (1, 44) = 7.54, p < .01, accounting for 9.0 % of the variance), inasmuch as younger children experience more Anxiety symptoms. (See Table 6.)
Discussion
These findings underscore the importance of measuring trauma-related symptoms (e.g., PTSD and dissociation) in children who have witnessed DV and/or experienced physical abuse in the context of a domestically violent home. There also is a relationship between self-reported symptoms by children and the number of DV event types. Results of the multiple regression indicate that in predicting symptoms, both parent and self-report measures are useful. Additionally, there is a need to assess for trauma-related symptoms specifically with instruments which are reliable, valid and normed (e.g., the TSCC and TSCYC).
Also, there were differences between parent reports of child symptoms and a child’s self-reported symptoms with parents endorsing higher T-scores on similar constructs (except for dissociation). This may be a spurious finding related to the fact that the different measures for self-report and parent ratings do not measure identical symptoms. Conversely, the higher ratings could be a function of the parent’s own distress. Jarvis et al. (2005) found that maternal anxiety and anger were related to child behavioral problems, but that PTSD symptoms in children were related solely to physical violence. For the clinician, the dilemma often is which report is accurate—the child’s self-report or the parent or caregiver rating? Until additional research elucidates this issue, practitioners and researchers may elect to consider as present PTSD symptoms endorsed by either parent or child—especially since there are so few studies directly assessing trauma symptoms in children exposed to DV.
Younger children self-reported more symptoms of anxiety and PTSD than did teens. Since onset and duration of DV/trauma and symptoms were not assessed, it is unclear if younger children were merely more frightened and anxious by events which were threatening to their sense of security. However, if teens experienced longer durations of DV, explanations incorporating possible adaptive responses deserve exploration. Additionally, the self-report measure (TSCC-A) does not contain items which are identical to those items on the caregiver rating (TSCYC).
Fewer relationships between parent ratings of children and DV event types may reflect an underestimate of the extent of exposure rather than merely a lack of awareness of symptoms. Since 34.9 % of cases involved children who reported experiencing interpersonal violence (without knowledge or confirmation by mothers), this topic deserves additional attention. Based on the design of this and many IRB-approved studies, it would be difficult to determine the exact distribution of mothers who knew of child-experienced physical abuse and elected not to report it in the study versus those mothers who had no knowledge of the physical abuse experienced by the child. Possible under-reporting of children experiencing physical abuse is not limited to the caregiver’s knowledge or possible defensiveness. That is, four children (5 %) refused to complete some of the THRIVE questions. The motivation for not answering is impossible to surmise, but might reflect some protectiveness by a small portion of children.
The findings related to race are somewhat difficult to interpret. Specifically, Caucasian parents endorsed more symptoms in their children for several clinical scales than did parents of African American, Latino, or biracial children. However, there were no differences in self-reported symptoms (i.e., the TSCC) based on race. This difference between races for parent report, but not child report may be a function of the intersection of culture and attitudes about mental health symptomatology for adults. However, through self-reports and free from stigma about mental health or cultural, children may merely report existing symptoms. In any event, it deserves further study. The role of SES was not assessed in this study and is a shortcoming as it relates to these differences in race. However, as mentioned, all children were English-speaking.
One of the primary limitations of the current sample is the small sample size. Additionally, the sample included only DV shelter residents and did not include a community sample. Therefore, the ability to generalize beyond a shelter population is precluded. However, Evans et al. (2008) in their meta-analysis found no significant differences among symptoms in children based on community versus shelter samples. The sample also was a convenience sample, and there was no information available about the characteristics of those mothers who refused to participate in the study. SES also was not assessed and may confound the interpretation of differences in some symptoms based on race. Another limitation is that maternal anxiety and anger were not assessed. Jarvis et al. (2005) found that child behavior problems were related only to maternal anxiety and anger; PTSD was related solely to physical violence. Finally, there is little known about the psychometric properties of the THRIVE Student Screening Questionnaire (SSQ). The internal consistency of the nine SSQ items for this sample merely approached acceptable (α = 0.69). Unfortunately, scale development for identification of traumatic events has been slow.
These findings suggest the need to continue to use ratings of child symptoms from both children and parents. Similarly, reports of interpersonal violence observed, experienced (including physical abuse of children), and combined and rates of agreement between mothers and children deserve further study. Finally, mixed findings for symptom presentations for female and male children deserve more detailed study and consideration of maternal factors which may contribute to symptom presentations. This line of research would potentially have policy implications in regions or among shelters where boys beyond a certain age are excluded from residing in a shelter based on concerns about aggressive behavior.
References
Achenbach, T. M. (1991). Manual for the child behavior checklist/4-18 and 1991 profile. Burlington: University of Vermont, Department of Psychiatry.
Bonomi, A. E., Thompson, R. S., Anderson, M., Reid, R. J., Carrell, D., Dimer, J. A., & Rivara, F. P. (2006). Intimate partner violence and women’s physical, mental, and social functioning. American Journal of Prevetive Medicine, 30(6), 458–466.
Briere, J. (1996). The trauma symptom checklist. Odessa: Psychological Assessment Resources.
Briere, J. (2005). The trauma symptom checklist for young children. Odessa: Psychological Assessment Resources.
Campbell, J. C. (2002). Health consequences of intimate partner violence. The Lancet, 13, 1331–1336.
Campbell, J. C., & Lewandowski, L. A. (1997). Mental and physical health effects of intimate partner violence on women and children. Psychiatric Clinics of North America, 20(2), 353–374.
Carlson, B. E. (1994). Children’s observations of interparental violence. In A. R. Roberts (Ed.), Battered women and their families (pp. 201–267). New York: Springer.
Chaffin, M., Wherry, J. N., Newlin, C., Crutchfield, A., & Dykman, R. (1997). The abuse dimensions inventory: initial data on a research measure of abuse severity. Journal of Interpersonal Violence, 12, 569–589.
Cook, A., Spinazzola, J., Ford, J., Lanktree, C., Blaustein, M., Cloitre, M., DeRosa, R., Hubbard, R., Kagan, R., Liautaud, J., Mallah, K., Olafson, E., & van der Kolk, B. (2005). Complex trauma in children and adolescents. Psychiatric Annals, 35, 390–398.
Cummings, E. M., Ballard, M., & El-Sheikh, M. (1991). Responses of children and adolescents to interadult anger as a function of gender, age, and mode of expression. Merrill-Palmer Quarterly, 37, 543–560.
Edwards, V. J., Holden, G. W., Felitti, V. J., & Anda, R. F. (2003). Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study, American Journal of Psychiatry, 160(8), 1453–1460.
Ellens, J. K. (2009). The effects of domestic violence, child abuse, and parenting stress on psychological distress in children. Dissertation Abstracts International, 70, Vol 70(2-B).
Evans, S. E., Davies, C., & DiLillo, D. (2008). Exposure to domestic violence: a meta-analysis of child and adolescent outcomes. Aggression and Violent Behavior, 13(2), 131–140.
Fantuzzo, J., Boruch, R., Beriama, A., Atkins, M., & Marcus, S. (1997). Domestic violence and children: prevalence and risk in five major U.S. cities. Journal of the American Academy of Child and Adolescent Psychiatry, 36(1), 116–122.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258.
Field, A. (2009). Discovering statistics using SPSS (3rd ed.). Thousand Oaks: Sage.
Ford, J. D., Wasser, T., & Connor, D. F. (2011). Identifying and determining the symptom severity associated with polyvictimization among psychiatrically impaired children in an outpatient setting. Child Maltreatment, 16, 216–226.
Goodkind, J. (2004) Student Screening Questionnaire. Unpublished work, Center for Health Promotion and Disease Prevention, University of New Mexico, Albuquerque, New Mexico, United States.
Graham-Bermann, S. A. (2001). Designing intervention evaluations for children exposedto domestic violence: Applications of research and theory. In S. A. Graham-Bermann (Ed.), Domestic violence in the lives of children (pp. 237–267). Washington: American Psychological Association.
Greeson, J. P., Briggs, E. C., Kisiel, C. L., Layne, C. M., Ake, G. S., III, Ko, S. J., & Fairbank, J. A. (2011). Complex trauma and mental health in children and adolescents placed in foster care: findings from the national child traumatic stress network. Child Welfare, 90(6), 91–108.
Grethel, S. (2005). Correlates of psychological symptoms among children exposed to domestic violence: Severity of domestic violence exposure, child abuse, and psychosocial stressors. Dissertation Abstracts International, 65, (10-B).
Grych, J. H., Jouriles, E. N., Swank, P. R., McDonald, R., & Norwood, W. D. (2000). Patterns of adjustment among children of battered women. Journal of Consulting and Clinical Psychology, 68, 84–94.
Holt, S., Buckley, H., & Whelan, S. (2008). The impact of exposure to domestic violence on children and young people: a review of the literature. Child Abuse & Neglect, 32(8), 797–810.
Hughes, H. M., Parkinson, D., & Vargo, M. (1989). Witnessing spouse abuse and experiencing physical abuse: a “double whammy”? Journal of Family Violence, 4, 197–209.
Jarvis, K., Gordon, E., & Novaco, R. (2005). Psychological distress of children and mothers in domestic violence emergency shelters. Journal of Family Violence, 20(6), 389–402.
Johnson, R. M., Kotch, J. B., Catellier, D. J., Winsor, J. R., Dufort, V., Hunter, W., & Amaya-Jackson, L. (2002). Adverse behavioral and emotional outcomes from child abuse and witnessed violence. Child Maltreatment, 7(3), 179–186.
Kernic, M. A., Wolf, M. E., Holt, V. L., McKnight, B., Huebner, C. E., & Rivara, F. P. (2003). Behavioral problems among children whose mothers are abused by an intimate partner. Child Abuse & Neglect, 27, 1231–1246.
Kilpatrick, K. L., & Williams, L. M. (1998). Potential mediators of post-traumatic stress disorder in child witnesses to domestic violence. Child Abuse and Neglect, 22, 319–330.
Levendosky, A., Huth-Bocks, A., Semel, A., & Shapiro, D. (2002). Trauma symptoms in preschool-age children exposed to domestic violence. Journal of Interpersonal Violence, 17, 150–163.
Lindhorst, T., Oxford, M., & Gillmore, M. R. (2007). Longitudinal effects of domestic violence on employment and welfare outcomes. Journal of Interpersonal Violence, 22(7), 812–828.
Lloyd, S. (2002). The effects of domestic violence on women’s employment. Law & Policy, 19(2), 139–167.
Margolin, G., & Vickerman, K. A. (2007). Posttraumatic stress in children and adolescents exposed to family violence: I. Overview and issues. Professional Psychology: Research and Practice, 38, 613–619.
McFarlane, J., Groff, J., O’Brien, J., & Watson, K. (2006). Secondary prevention of intimate partner violence. Nursing Research, 55(1), 52–61.
Menard, S. (1995). Applied logistic regression analysis (Sage university paper series on quantitative applications in the social sciences, 07-106). Thousand Oaks: Sage.
O’Brien, M., John, R. S., Margolin, G., & Erel, O. (1994). Reliability and diagnostic efficacy of parents’ reports regarding children’s exposure to marital aggression. Violence and Victims, 9(1), 45–62.
O’Keefe, M. (1994a). Linking marital violence, mother–child/father–child aggression, and child behavior problems. Journal of Family Violence, 9, 63–78.
O’Keefe, M. (1994b). Racial/ethnic differences among battered women and their children. Journal of Child and Family Studies, 3, 283–305.
Seery, M. D., Holman, E. A., & Silver, R. C. (2010). Whatever does not kill us: cumulative lifetime adversity, vulnerability, and resilience. Journal of Personality and Social Psychology, 99(6), 102–1041.
Spilsbury, J., Belliston, L., Drotar, D., Drinkard, A., Kretschmar, J., Creeden, R., & Friedman, S. (2007). Clinically significant trauma symptoms and behavioral problems in a community-based sample of children exposed to domestic violence. Journal of Family Violence, 22(6), 487–499.
Stein, B. D., Jaycox, L. H., Kataoka, S. H., Wong, M., Tu, W., Elliott, M. N., et al. (2003). A mental health intervention for schoolchildren exposed to violence: a randomized control trial. Journal of the American Medical Association, 290, 603–611.
Strauss, M. A. (1992). Children as witnesses to marital violence: A risk factor for lifelong problems among a nationally representative sample of American men and women (Report of the 23rd Ross Roundtable). Columbus: Ross Laboratories.
Tonelli, K. (2002). Are there gender differences in self-report symptomatology of children and adolescents exposed to domestic violence? Dissertation Abstracts International, 63 (5-B).
Van Horn, P., & Lieberman, A. F. (2004). Early intervention with infants, toddlers, and preschoolers. In B. T. Litz (Ed.), Early intervention for trauma and traumatic loss (pp. 112–130). New York: Guilford Press.
Wekerle, C., Miller, A. L., Wolfe, D. A., & Spindel, C. B. (2006). Childhood maltreatment. Cambridge: Hogrefe & Huber.
Wolfe, V. V., Gentile, C., & Wolfe, D. A. (1989). The impact of sexual abuse on children: A PTSD formulation. Behavior Therapy, 20(2), 215–228.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wherry, J.N., Medford, E.A. & Corson, K. Symptomatology of Children Exposed to Domestic Violence. Journ Child Adol Trauma 8, 277–285 (2015). https://doi.org/10.1007/s40653-015-0048-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40653-015-0048-x