Abstract
A burgeoning body of literature addresses the comorbidity of depression and OCD in adults. The purpose of this study was to extend this area of research to children and adolescents by examining the clinical correlates associated with co-occurring depressive disorders in a clinical sample of youth with OCD. Participants included children and adolescents seeking treatment at a university-based research clinic. One group was comprised of 28 children (ages 10–17 years) who met diagnostic criteria for OCD but had no comorbid depressive disorders, whereas the second group consisted of 28 children matched for age and gender who met diagnostic criteria for OCD and co-occurring depressive disorder. The two groups were compared on measures of broad-band psychopathology, internalizing problems, social difficulties, and family characteristics. As anticipated, findings revealed comorbid depression and OCD was associated with more severe internalizing problems, more extensive obsessive–compulsive symptomatology, and more social problems. Youth with comorbid depression and OCD also had higher family conflict and lower family organization compared to those with OCD and no depression. These results may have implications for the treatment of youth with comorbid OCD and depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obsessive–compulsive disorder (OCD) is a disorder marked by intrusive thoughts/images and/or compulsions and is often associated with concurrent anxiety and mood disorders [1]. Depression is one of the most frequent comorbid conditions reported in individuals with anxiety disorders in general [2] as well as OCD in particular [3, 4]. Although there is a burgeoning body of literature addressing the comorbidity of depression and OCD in adults, few studies have addressed this relationship in children and adolescents. Yet, high rates of comorbid problems including depression are common in youth with OCD [5].
The co-occurrence of depression and OCD has been shown to impede treatment response and is related to poorer treatment outcomes in adults [6, 7]. Pediatric OCD also has a differential treatment response with various comorbid conditions. While tic disorders do not appear to affect CBT outcomes for pediatric OCD [8], other comorbid conditions, including externalizing problems and depression, have been shown to negatively affect treatment outcome for youth with OCD [9, 10].
Only a few studies have examined specific risk factors for the development of depression in adults with OCD, and the findings are inconsistent. Age of onset, family history of depression, and specific comorbid conditions have been associated with the development of comorbid depression with OCD in some studies but not others [11–15]. More severe OCD symptoms and specific obsessive compulsive symptoms (aggressive, sexual, and religious obsessions) have also been associated with comorbid depression and OCD in adults [12–14]. Yet, even these studies with adults remain inconsistent.
When considering samples of youth, developmental and contextual factors such as family environment and specific parenting practices also need to be considered inasmuch as they might play influential roles in the development and maintenance of emotional disorders [16]. Family environment and parenting practices, including overprotection, high levels of parental control, rejection, and a lack of parental warmth, have been reported in youth with OCD [17, 18]. Similar family characteristics have been reported in youth with depression. Moreover, high conflict and hostility within families has been reported in youth with anxiety and depression [19–21]. To date, no studies have differentiated family environments between children with depression and OCD. However, adult retrospective reports indicate that patients with OCD report that their mothers were more overprotective and more rigidly “organized” compared to patients with depression alone [22]. Increasing evidence suggests that family accommodation also plays a significant role in the maintenance of obsessions and compulsions [23, 24]. Recently, Peris and colleagues [23] reported that families with higher cohesion have lower levels of parental distress when accommodating, and families with higher organization report less accommodation. Additionally, they report that families with higher conflict report more distress when accommodating OCD symptoms.
Finally, another risk factor for both OCD and depression is interpersonal difficulties and social problems (e.g., [25]). For example, excessive seeking of reassurance has been associated with depressive symptoms and reported as a significant predictor of interpersonal rejection [26]. One study reported that peer victimization mediated the relationship between depression and OCD symptoms [27], but a more thorough examination of the role of social problems and interpersonal difficulties in the comorbid presentation of OCD and depression is warranted.
Given the emerging literature suggesting poorer treatment outcome for comorbid OCD and depression in both adults and youth, coupled with the limited and inconsistent findings regarding the correlates of comorbid OCD and depression, additional examination of these risk factors is warranted. The purpose of this study was to extend this area of research by investigating the clinical correlates and risk factors associated with co-occurring depressive disorders in a clinical sample of youth with OCD. It was expected that comorbid OCD and depression would be associated with more severe OCD symptomatology, internalizing problems, social problems, and comorbidity with other disorders. Additionally, family characteristics associated with co-occurring depressive disorders and OCD were examined. It was expected that youth with comorbid OCD and depression would have more difficulties within the family environment, specifically, higher levels of conflict. Other family dimensions that have been associated with OCD, including control, cohesion, and organization, were also explored.
Methods
Participants
Children and adolescents and their parents who presented for diagnostic assessment at a university-based research and treatment facility served as participants. A parent or guardian initiated these assessments based on clinical service provider recommendation or self-referral. All assessments procedures were in accordance with the ethical standards and Institutional Review Board approval of Boston University. Institutional Review Board approved consent and assent forms (for children 12 and over) signed prior to all assessments. A sample of 56 (28 females, 28 males) children and adolescents ages 10–17 (M = 14.5) drawn from a larger sample of youth who presented at the treatment facility were available for study purposes. All youth met diagnostic criteria for OCD, using the Anxiety Disorders Interview Schedule for Children (ADIS-IV C/P). The sample consisted primarily of Caucasian children (96.4%) and their parents.
Participants were divided into two groups based on the diagnostic assessment: (1) an OCD Alone group, and (2) an OCD + Depression group. The OCD Alone group consisted of 28 children (females = 14, males = 14) who met diagnostic criteria for OCD and had no comorbid depressive disorder or subclinical depression. The OCD + Depression group consisted of 28 age and gender matched youth who met diagnostic criteria for both OCD and a co-occurring depressive disorder: 67.9% (n = 19) had major depressive disorder; 14.3% (n = 4) had dysthymia; and 17.8% (n = 5) had a depressive disorder not otherwise specified. Both groups met criteria for other co-occurring disorders (see Table 1). Family demographic information is provided in Table 2.
Measures
Measures included a variety of assessments across multiple informants, including a clinician-rated interview, child self-reports, and parental reports. All of these measures have good psychometric properties, with sound reliability, validity, and clinical utility [28].
Anxiety Disorders Interview Schedule, Child and Parent Version (ADIS-IV-C/P; [29])
The ADIS-IV-C/P is a semi-structured interview, assessing anxiety, mood, and externalizing behavior disorders included in the DSM-IV disorders for youth. The ADIS-IV-C/P was administered by trained graduate-level clinicians and licensed clinicians. Impairment ratings were generated for each diagnosis using the Clinician Severity Rating (CSR, range = 0–8; ≥4 required to assign a clinical diagnosis). The clinician derived separate clinical diagnoses based on the reports of both children and parents. Assessments and diagnosis were reviewed and finalized by a group of trained ADIS-IV-C/P clinicians in order to determine the final consensus diagnosis. Given that the current sample is based on a review of records, inter-rater reliability analyses are available only for the total clinic, which does not include a portion of the current sample. Inter-rater reliability analyses from 60 individuals at this treatment site indicated good inter-rater agreement regarding primary diagnosis (κ = .866) and clinical severity (Pearson product-moment correlation r = .615). Inter-rater reliability for OCD diagnoses (κ = .949) and OCD clinical severity (Pearson product-moment correlation r = .745) were acceptable, as were the reliabilities for depressive disorder diagnoses (κ = .816) and depression clinical severity (Pearson product-moment correlation r = .54).
Child Behavior Checklist (CBCL; [30])
The CBCL is a widely used 113-item parental report designed to assess a broad range of child and adolescent behavioral and emotional functioning [31]. Parents are asked to rate the degree to which an item is true about their child (0 = not true; 1 = somewhat or sometimes true; 2 = very true or often true). The CBCL has two “broad-band” scales, Internalizing and Externalizing behaviors. The Internalizing scale includes items related to somatic complaints, anxiety, and depression, while the Externalizing scale assesses maladaptive behaviors related to oppositional problems, delinquency, and inattention. Within these two primary scales are several subscales, including anxiety/depression, withdrawn/depressed, somatic complaints, social problems, thought problems, attention problems, rule-breaking behavior, and aggressive behavior. Test–retest reliability has been reported to be .89 at 1 week and .74 at 3 months [31]. For the current study, the total Internalizing scale and the internalizing subscales, Withdrawn, Somatic Complaints, Anxious/Depressed, from the mother’s CBCL report were used. To assess interpersonal difficulties, the Social Problems subscale was also enlisted.
Children’s Depression Inventory (CDI; [32])
The CDI is a 27-item self-report measure assessing depressive symptomatology in children 7–17 years. Children are asked to select one of three statements that best described their feelings over the past 2 weeks. The CDI has a total score and five subscales (Negative Mood, Interpersonal Difficulties, Negative Self-Esteem, Ineffectiveness, Anhedonia). The CDI has demonstrated adequate internal consistency across various age groups and genders including coefficient reliability alphas ranging from .83 to .89, stable item-total score product-moment correlations, and test–retest coefficients of .74 and .77 [33]. The validity of the CDI has also been established [34]. For the present study, the CDI Total Score was used.
Multidimensional Anxiety Scale for Children (MASC; [35])
The MASC is a 39-item self-report measure assessing multiple aspects of anxiety. The MASC asks children to rate various anxiety symptoms (e.g., “I feel tense or uptight” or “I worry about doing something stupid or embarrassing”) on a four point Likert scale indicating how true the statement is about them (0 = never true about me; 1 = rarely true about me; 2 = sometimes true about me; 3 = often true about me). The MASC contains an overall total score in addition to four subscales: physical symptoms, harm avoidance, social anxiety, and separation/panic. The MASC has shown excellent psychometric properties. The internal reliability of all of the MASC scales ranges from .50 to .89, and test–retest reliability for the total score is .93 [35]. The measure also has adequate construct validity with a high correlation with other child anxiety questionnaire measures and adequate divergent validity [35]. For the current study, the MASC Total Score was used.
Penn State Worry Questionnaire for Children (PSWQ-C; [36])
The PSWQ-C is a 14-item self-report measure assessing children’s degree of excessive and uncontrollable worry. The PSWQ-C is a developmentally appropriate adaptation of the adult-version of the Penn-State Worry Questionnaire [37], and asks children to rate items on a 4-point Likert scale: 0 = Not at all true, 1 = Sometimes true, 2 = Most times true, and 4 = Always true. A total score is calculated by summing all items, allowing for a range of scores from 0 to 48, with higher scores reflecting more severe and excessive worry.
Family Environment Scale (FES; [38])
The FES is a 90-item, true/false, self-report measure that assesses various characteristics of family relationships. This measure contains ten subscales (9 items each) that are divided into three dimensions designed to assess socio-environmental aspects of family functioning. The reliability and validity of the FES are well-established [39]. Internal consistency reliability estimates for the FES subscales range from .61 to .78. Test–retest reliabilities for the subscales for 2-month, 3-month, and 12-month intervals range from .52 to .91 suggesting that the scale is reasonably stable across time. For the current study, the subscales, Cohesion, Conflict, Control, and Organization were examined. These subscales were specifically examined based on previous research indicating their potential associations with OCD and depression.
Procedure
All individuals were screened over the phone by a trained doctoral student in clinical psychology prior to being scheduled for a diagnostic assessment. Children having mental retardation, substance abuse, schizophrenia, psychosis, or need for immediate services due to homicidal or suicidal thoughts were referred to an outside community agency.
The assessment consisted of an in-person ADIS-IV-C/P semi-structured interview and several parent and child self-report measures. The ADIS was administered according to the guidelines provided by Silverman and Albano [29]. The same interviewer conducted both the child and parent versions (e.g., [40]) with the child portion of the ADIS administered prior to the parent interview in all cases. Separate diagnoses were determined for both child and parent interviews. The interviewer presented both the child and parent diagnoses, along with clinical observations obtained during the interviews, to a clinical team of trained ADIS-IV-C/P clinicians. Diagnoses were reviewed by the team to assign final consensus diagnoses.
Results
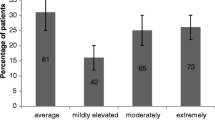
The OCD + Depression group had significantly higher OCD severity (ADIS CSR), t = −2.44, p < .05; therefore, all subsequent analyses controlled for OCD severity. Three multivariate analyses of covariances were performed for two primary purposes: (1) in order to control for OCD severity, and (2) on the theoretical basis of categorizing similar constructs and dependent variables together. Thus, separate multivariate analysis of covariance analyses were analyzed for the internalizing measures, the CBCL subscales, and the FES. Effect sizes were also analyzed using partial eta-squared, interpreted similarly to R-square as the proportion of variance explained [41, 42]. According to Cohen’s [42] guidelines, partial eta squared values can be interpreted in terms of small (.01), medium (.06), and large (.14) effect sizes.
Clinical Correlates on Internalizing Difficulties
The two groups were compared on measures of internalizing symptoms (CDI, MASC, PSWQ, CBCL Internalizing Scale), using a multivariate analysis of covariance. It was hypothesized that children with comorbid OCD and depression would have more severe internalizing difficulties. As anticipated, a multivariate effect was obtained (F (4,34) = 8.21, p < .001; Wilks’ Lambda = .51; partial eta squared = .491). The groups differed significantly on all clinical correlates, each having large effect sizes (See Table 3). The OCD + Depression group had significantly higher depression, pervasive worry, anxiety, and internalizing problems compared to the OCD Alone group.
A multivariate analysis of covariance, controlling for OCD severity, was also used to examine the following CBCL subscales: Withdrawn, Somatic Complaints, Anxious/Depressed, and Social Problems. A significant multivariate effect was obtained (F (4,42) = 4.24, p < .01; Wilks’ Lambda = .712; partial eta squared = .288). Analyses of each dependent variable revealed that the groups differed on all subscales, with the OCD + Depression group having significantly higher scores on all subscales (See Table 4). Effect sizes were medium for both Somatic Complaints and Social Problems, and large for Withdrawn and Anxious/Depressed.
Family Environment
The groups were compared on family environment. It was expected that mothers of youth in the OCD + Depression group would report higher conflict. Other family dimensions examined were exploratory in nature given that they have been associated with OCD but not necessarily depression or comorbid OCD and depression. These other family features included measures of control, cohesion, and organization. A multivariate analysis of covariance, controlling for OCD severity, examined the FES subscales: Cohesion, Conflict, Control, and Organization. A multivariate effect was obtained (F (4,22) = 3.12, p < .05; Wilks’ Lambda = .638; partial eta squared = .362). Subsequent analyses of each dependent variable indicated that the groups differed on Conflict (F (1,26) = 4.60, p ≤ .05) and Organization (F (1,26) = 4.59, p ≤ .05), and approached significance for Control (F (1,26) = 3.41, p = .077) but not Cohesion (F (1,26) = 2.69, p = .114). Mothers in the OCD + Depression group reported significantly more Conflict and less Organization within the family compared to mothers of the OCD Alone group (See Table 5).
Comorbidity
Previous research has suggested that children with comorbid OCD and depression may have a higher frequency of additional comorbid anxiety disorders [13]; therefore, frequency of comorbid conditions was examined between the two groups. Due to such a small proportion of children in this study having externalizing conditions in both the OCD Alone group (n = 4) and OCD + Depression group (n = 5), the groups were compared statistically only on the frequency of having an additional anxiety disorder. This difference was significant (χ2 = 4.46, p < .05), indicating that the OCD + Depression group had more youth (n = 24, 85.7%) with an additional anxiety disorder compared to the OCD Alone group (n = 17, 60.7%). All of the anxiety disorders, with the exception of separation anxiety disorder, were more common in the OCD + Depression group, although these differences were not tested for significance due to small sample sizes (several cell sizes <5). The anxiety disorders most commonly associated with comorbid OCD and depression were social phobia (46.4%) and generalized anxiety disorder (35.7%).
Discussion
The current study sought to differentiate clinical correlates and family environments between youth with OCD and those with comorbid depression and OCD. Consistent with previous research [9, 12–14], our results suggest that youth who are comorbid with depression report more severe internalizing symptomatology. Specifically, comorbid OCD and depression were associated not only with higher clinical severity ratings for their OCD but also with more severe depression, anxiety, excessive worry, and higher rates of other comorbidities.
Consistent with previous research in the adult literature, our results suggest that youth with comorbid OCD and depression had more comorbid diagnoses [13]. As discussed by Hong and colleagues [13] individuals with OCD and depressive disorders may present as a “highly comorbid group.” Although not tested for significance, our results indicated that social phobia and generalized anxiety disorder were the most frequent comorbid conditions. Generalized anxiety disorder has been found to be the most comorbid condition with comorbid OCD and depression in adult studies [14, 15], and in such cases, it may indicate a possible continuum of worries related to generalized anxiety in addition to depressive and obsessive worries [14]. In our sample, the comorbid OCD and depression group had not only more comorbid diagnoses, but they also had more severe OCD symptomatology. Recently, depression was reported to predict OCD-related functional impairment [43]. As these authors discuss, perhaps depression is related to negative cognitive styles that are impacting children’s functioning and/or perceptions of their functional impairment. Finally, as expected, our results indicated that social problems were also found to be higher in youth with comorbid depression and OCD (e.g., [25]). Interpersonal difficulties have been associated with depression and OCD, including for example peer victimization and excessive re-assurance seeking [26, 27]. Our results suggest that children with comorbid OCD and depression have more social difficulties. Further exploring these specific interpersonal difficulties may be warranted in this population.
Results also indicate that reported family environments were different between the two groups. Mothers of children with comorbid depression and OCD reported higher conflict and less organization compared to those with no depression. These results are consistent with previous research indicating high conflict within the family environment for adolescents with depression [21]. Higher conflict has also been associated with more distress when families report accommodating OCD symptoms in their daughters and sons [23]. Moreover, it is has been suggested that more distress within the family environment might increase the severity of OCD symptoms [44], and that greater OCD severity subsequently might lead to depression. Such a possibility remains to be prospectively examined, however.
Youth with comorbid depression and OCD also evidenced less organization within the family. Recent research [23] suggests that families with more organization report less accommodation of OCD symptoms. Although family accommodation was not examined in this study, it is possible that the families with less organization had more difficulty disengaging from accommodating OCD symptoms [23], thus maintaining the symptoms and potentially resulting in more family distress and/or depression [38]. Again, however, these speculations await prospective verification. There were no differences between the groups on family control or cohesion. However, this finding is not unlike findings in earlier research that document “child psychopathology in general” is marked by lower family cohesion [45] and may not be related to specific patterns of comorbidity. Additionally, it is possible that no differences emerged on control and cohesion perhaps due to these family dimensions being attributed to OCD and not depression, thus being experienced in both groups of children in this sample. In sum, family environments on some important dimensions differed between youth with OCD and those with comorbid depression and OCD.
Various theoretical and treatment models have been proposed regarding comorbid anxiety and depression [2, 46] but remain to be investigated specifically for OCD and depression. For example, within the tripartite model of anxiety and depression, anxiety and depression are thought to share a common component of high negative affectivity, but differ in other domains such that anxiety is marked by high physiological arousal whereas depression is characterized by low positive affectivity [2]. Future research will also need to examine the relationship between OCD and depression in longitudinal designs in order to shed light onto understanding those cases in which the depression or OCD develops first. Gaining a better understanding of this relationship may better inform prevention and intervention programs. Similarly, depression has recently been shown to negatively impact CBT treatment for OCD in youth [10] and may serve to decrease anxiety habituation during exposures [6].Given that there are significant differences in children having OCD with versus without depression, particularly increased severity in a variety of domains, these findings might also have implications for the treatment of OCD in youth. Several factors have been associated with treatment response for youth with OCD, including depression, other comorbidities, and family dysfunction [47]. Youth with comorbid OCD and depression may therefore need to undergo a different or adapted treatment, and these treatment modifications should be examined in this particular population. For example, researchers have discussed differing approaches such as targeting depressive symptomatology prior to the treatment of OCD in a hierarchical, sequential fashion [10] or alternatively, targeting the depression and OCD simultaneously in a unified, integrated approach [48].
Limitations
This study possesses several limitations. Unfortunately, the current study did not use the Children’s Yale-Brown Obsessive–Compulsive Scale (CY-BOCS; [49]), the most common assessment measure for childhood OCD. As a result, the relationship between various OCD symptom types with depression was unable to be determined (see [50]). Additionally, the same diagnostician administered both the child and parent sections of the ADIS, which has the potential to bias the diagnostic information gathered during the ADIS interview; however, this practice is recommended by Silverman and Albano [29]. Furthermore, the sample was comprised largely of middle-class, Caucasian families and the study findings may not generalize to families of other races/ethnicities or circumstance. Finally, given the high rates of family accommodation with OCD symptoms [24, 44], future studies may examine the association between comorbid depression and OCD and family accommodation styles. This possibility was not examined in the current study.
Summary
This study is the first to specifically examine clinical correlates and potential risk factors for comorbid depression and OCD in youth. Building upon the bourgeoning adult literature, clinical correlates for depression and OCD included more severe internalizing and OCD symptomatology, differential family characteristics, and more social difficulties. In summary, this study provides preliminary data on the clinical correlates of comorbid OCD and depression in a clinical sample of children and adolescents ages 10–17 years. Twenty-eight children with OCD and no depressive disorder were compared to an age and gender matched group of youth with OCD and a co-occurring depressive disorder on a variety of measures assessing psychopathology and family characteristics. The findings suggest that children with comorbid OCD and depression have significantly more difficulties in a variety of domains compared to children with OCD and no depression. Specifically, youth with comorbid OCD and depression experienced more internalizing psychopathology, including more severe OCD symptoms, worry, depression, and anxiety. Additionally, youth with comorbid OCD and depression had more comorbid anxiety disorders as well as more social problems. Finally, youth with comorbid OCD and depression may have differential family environments, with higher family conflict and less family organization compared to children with OCD and no depression. These findings suggest that youth with comorbid OCD and depression may present with more severe and differing clinical correlates than those youth presenting with OCD and no depressive disorder.
References
Nestadt G, Samuels J, Riddle M, Liang KY, Beinvenu O, Hoehn-Saric R et al (2001) The relationship between obsessive-compulsive disorder and anxiety and affective disorders: Results from the Johns Hopkins OCD Family Study. Psychol Med 31:481–487
Seligman LD, Ollendick TH (1998) Comorbidity of anxiety and depression in children and adolescents: and integrative review. Clin Child Fam Psychol Rev 1(2):125–144
Crino R, Andrews G (1996) Obsessive-compulsive disorder and Axis I comorbidity. J Anxiety Disord 10:37–46
Tükel R, Polat A, Ozdemir O, Aksut D, Turksoy N (2002) Comorbid conditions in obsessive-compulsive disorder. Compr Psychiatry 43:204–209
Geller DA, Beiderman J, Griffin S, Jones J (1996) Comorbidity of juvenile obsessive-compulsive disorder with disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry 35:1637–1646
Abramowitz JS (2004) Treatment of obsessive-compulsive disorder in patients who have comorbid major depression. J Clin Psychol 60:1133–1141
Abramowitz JS, Franklin ME, Street G, Kozak M, Foa EB (2000) Effects of comorbid depression on response to treatment for obsessive-compulsive disorder. Behav Ther 31:517–528
March JS, Franklin ME, Leonard H, Garcia A, Moore P, Freeman J, Foa E (2007) Tics moderate treatment outcome with setraline but not cognitive-behavior therapy in pediatric obsessive-compulsive disorder. Biol Psychiatry 61:344–347
Storch EA, Larson MJ, Merlo LJ, Keeley ML, Jacob ML, Geffken GR, Murphy TK, Goodman WK (2008) Comorbidity of pediatric obsessive-compulsive disorder and anxiety disorders: impact on symptom severity and impairment. J Psychopathol Behav Assess 30:111–120
Storch EA, Merlo LJ, Larson MJ, Geffken GR, Lehmkuhl HD, Jacob ML, Murphy TK, Goodman WK (2008) Impact of comorbidity on cognitive-behavioral therapy response in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 47:583–591
Bellodi L, Sciuto G, Diaferia G, Ronshi P, Smeraldi E (1991) Psychiatric disorder in the families of patients with obsessive-compulsive disorder. Psychiatry Res 42:111–120
Besirolglu L, Uguz F, Saglam M, Agargun MY, Cilli AS (2007) Factors associated with major depression occurring after the onset of obsessive-compulsive disorder. J Affect Disord 102:73–79
Hong JP, Samuels J, Bienvenu J, Cannistraro P, Grados M, Riddle M (2004) Clinical correlates of recurrent major depression in obsessive-compulsive disorder. Depress Anxiety 20:86–91
Perugi G, Akiskal HS, Pfanner C, Presta S, Gemignani A, Milanfranchi A et al (1997) The clinical impact of bipolar and uniploar affective comorbidity on obsessive-compulsive disorder. J Affect Disord 46:15–23
Tükel R, Meteris H, Koyuncu A, Tecer A, Yazici O (2006) The clinical impact of mood disorder comorbidity on obsessive-compulsive disorder. Eur Arch Psychiatry Clin Neurosci 256:240–245
Rapee RM (1997) Potential role of childrearing practices in the development of anxiety and depression. Clin Psychol Rev 17:47–67
Alonso P, Menchon JM, Mataix-Cols D, Pifarre J, Urretavizcaya M, Crespo JM, Jimenez S, Vallejo G, Vallejo J (2004) Perceived parental rearing style in obsessive-compulsive disorder: relation to symptom dimensions. Psychiatry Res 127:267–278
Yoshida Y, Taga C, Matsumoto Y, Fukui AK (2005) Paternal overprotection in obsessive-compulsive disorder and depression with obsessive traits. Psychiatry Clin Neurosci 59:533–538
Stark KD, Humphrey LL, Crook K, Lewis K (1990) Perceived family environments of depressed and anxious children: child’s and maternal figure’s perspectives. J Abnorm Child Psychol 18:524–547
Sheeber L, Hopes H, Alpert A, Davis B, Andrews J (1997) Family support and conflict: prospective relations to adolescent depression. J Abnorm Child Psychol 25:333–345
Shiner RL, Marmorstein NR (1998) Family environments of adolescents with lifetime depression: associations with maternal depression history. J Am Acad Child Adolesc Psychiatry 37:1152–1160
Merkel WT, Pollard CA, Wiener RL, Staebler CR (1993) Perceived parental characteristics of patients with obsessive-compulsive disorder, depression, and panic disorder. Child Psychiatry Hum Dev 21(1):49–57
Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J (2008) Correlates of accommodation of pediatric obsessive-compulsive disorder: parent, child, and family characteristics. J Am Acad Child Adolesc Psychiatry 47:1173–1181
Storch EA, Geffken GR, Merlo LJ, Jacob ML, Murphy TK, Goodman WK et al (2007) Family accommodation in pediatric obsessive-compulsive disorder. J Clin Child Adolesc Psychol 36:207–216
Garber J (2006) Depression in children and adolescents: linking risk research and prevention. Am J Prev Med 31(6):S104–S125
Joiner TE (1999) A test of interpersonal theory of depression in youth psychiatric inpatients. J Abnorm Child Psychol 27(1):77–85
Storch EA, Ledley DR, Lewin AB, Murphey TK, Johns NB, Goodman WK, Geffken JR (2006) Peer victimization in children with obsessive-compulsive disorder: relations with symptoms of psychopathology. J Clin Child Adolesc Psychol 35(3):446–455
Silverman WK, Ollendick TH (2005) Evidenced-based assessment of anxiety and its disorders in children and adolescents. J Clin Child Adolesc Psychol 34(3):380–411
Silverman WK, Albano AM (1996) The anxiety disorders interview schedule for children for DSM-IV: child and parent versions. Psychological Corporation, San Antonio, TX
Achenbach TM (1991) Manual for the child behavior checklist/4–18 and 1991 profile. University of Vermont, Department of Psychiatry, Burlington, VT
Achenbach TM, Edelbrock CS (1979) The Child Behavior Profile: II. Boys aged 12–16 and girls aged 6–11 and 12–16. J Consult Clin Psychol 47(2):223–233
Kovacs M (1992) The children’s depression inventory. Multi-Health Systems, Inc., Toronto, ON
Smucker MR, Craighead WE, Craighead LW (1986) Normative and reliability data for the Children’s Depression Inventory. J Abnorm Child Psychol 14(1):25–39
Kovacs M, Beck AT (1977) An empirical-clinical approach toward a definition of childhood depression. In: Schulterbrandt JG, Raskin A (eds) Depression in childhood: diagnosis, treatment, and conceptual models. Raven Press, New York, pp 1–25
March JS, Parker JD, Sullivan K, Stallings P, Conners CK (1997) The Multidimensional Anxiety Scale for Children: factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry 36:554–565
Chorpita BF, Tracey SA, Brown TA, Collica TJ, Barlow DH (1994) Assessment of worry in children and adolescents: an adaptation of the Penn State Worry Questionnaire. Behavior Research and Therapy 35:569–581
Meyer TJ, Miller ML, Metzger RL, Borkovec TD et al (1990) Development and validation of the Penn State Worry Questionnaire. Behav Res Ther 28(6):487–495
Moos RH, Moos BS (1994) Family environment scale manual. Consulting Psychologists Press, Palo Alto, CA
Moos RH, Moos BS (1981) Family environment scale manual. Consulting Psychologists Press, Palo Alto, CA
Silverman WK, Eisen AR (1992) Age differences in the reliability of parent and child reports of child anxious symptomology using a structured interview. J Am Acad Child Adolesc Psychiatry 31(1):117–124
Cohen J (1973) Eta-squared and partial eta squared in fixed factor anova designs. Edu Psychol Measur 33:107–112
Cohen J (1988) Statistical power analysis for the behavioral sciences. Plenum, New York
Storch EA, Larson MJ, Muroff J, Caporino N, Geller D, Reid JM et al (2010) Predictors of functional impairment in pediatric obsessive-compulsive disorder. J Anxiety Disord 24:275–283
Renshaw KD, Steketee G, Chambless DL (2005) Involving family members in the treatment of OCD. Cogn Behav Ther 34:164–175
Jewell JD, Stark KD (2003) Comparing the family environments of adolescents with conduct disorder or depression. J Child Fam Stud 12:77–89
Ollendick TH, Jarrett MA, Grills-Taquechel AE, Hovey LD, Wolff J (2008) Comorbidity as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention deficit/hyperactivity disorder, and oppositional/conduct disorders. Clin Psychol Rev 28(8):1447–1471
Keeley ML, Storch EA, Merlo LJ, Geffken GR (2008) Clinical predictors of response to cognitive-behavioral therapy for obsessive-compulsive disorder. Clinical Psychology Review 28:118–130
Ehrenreich JT, Goldstein CR, Wright LR, Barlow DH (2009) Toward a unified treatment for emotional disorders in youth. Child Fam Behav Ther 31:20–37
Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK et al (1997) Children’s Yale-Brown Obsessive Compulsive Scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 36:844–852
Ricciardi J, McNally RJ (1995) Depressed mood is related to obsessions, but not to compulsions, in obsessive-compulsive disorder. J Anxiety Disord 9:249–256
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Canavera, K.E., Ollendick, T.H., Ehrenreich May, J.T. et al. Clinical Correlates of Comorbid Obsessive–Compulsive Disorder and Depression in Youth. Child Psychiatry Hum Dev 41, 583–594 (2010). https://doi.org/10.1007/s10578-010-0189-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-010-0189-y