Abstract
Family accommodation (FA) has been linked with myriad negative outcomes in pediatric obsessive–compulsive disorder (OCD), but extant literature has yielded differential relationships between FA and clinical variables of interest. Consequently, this study examined the phenomenology, clinical profile, and effects of comorbid psychopathology on FA to better understand these behaviors. A total of 150 youths and their caregivers completed clinician- and self-reported measures at a baseline visit for a larger randomized controlled trial. Sociodemographic variables were not associated with FA, but specific types of OCD symptom clusters were. Higher OC-symptom severity and functional impairment were associated with increased FA. Comorbid anxiety disorders moderated the relationship between OC-symptom severity and FA, but comorbid attention deficit hyperactivity, oppositional defiant, and mood disorders did not. Internalizing and externalizing problems both mediated the relationship between FA and functional impairment. These findings provide clinical implications for important treatment targets and factors that may impact FA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Family accommodation (FA) is a salient phenomenon observed in pediatric obsessive–compulsive disorder (OCD); up to 97% of families report the occurrence of FA and over half of the families report engaging in these behaviors on a daily basis [1,2,3,4,5]. FA is multifaceted and can encompass a wide variety of behaviors [6], including modification of the family’s schedule to accommodate a subject’s obsessive–compulsive symptoms, facilitation of avoidance, engagement in compulsions, and provision of OCD-related reassurance [7, 8]. Family members often engage in these behaviors with positive intentions, with hopes of decreasing the child’s distress and/or time occupied by symptoms [8,9,10]. However, these behaviors work in opposition to the therapeutic principles of exposure and response prevention, the first line treatment for childhood OCD [11]. Specifically, accommodating the child’s obsessive–compulsive symptoms feeds into the negative reinforcement cycle by preventing the child from facing the triggering situations [12] and the important learning experiences associated with doing so (e.g., that a feared consequence may not occur).
Higher FA has been linked with myriad deleterious effects at the child and family level. When considering clinical variables at the patient level, it has been linked with higher obsessive–compulsive symptom severity [13]. However, the relationship between obsessive–compulsive symptom severity and FA can vary depending on the aspect of accommodation examined [2, 6]. FA has predicted OCD-related impairment in youth as well [14]; indeed, accommodation mediates the relationship between obsessive–compulsive symptoms and functional impairment [15, 16]. It follows that higher FA in OCD has been repeatedly linked with decreased in-session compliance [17] and poorer treatment outcomes [18,19,20]. Specifically, Piacentini, et al. [21] found that decreases in FA generally preceded decreases in obsessive–compulsive symptoms, with others similarly elucidating links between improved treatment outcome and decreases in FA in pediatric OCD [19]. At the family level, higher rates of FA have been linked with higher family conflict [2], though higher family cohesion predicted lower participation in the child’s symptoms [6]. These findings highlight the impactful nature of these behaviors, underlining the importance of addressing them therapeutically [22, 23] and decreasing accommodation consistently over time [24].
Certain OCD symptom clusters have been linked to increased FA, with the contamination subtype emerging most robustly in the literature [3, 5, 6, 25]. Youth with contamination symptoms generally have more opportunities for accommodation (e.g., having family members move dirty items, asking others to wash their hands, requesting to have cleaning items purchased) relative to other symptom clusters. Additionally, the content of the symptoms may be easier to endorse more openly, compared to other symptoms that may be seen as more bizarre or unacceptable (e.g., harm-related obsessions). With regards to sociodemographic variables, age and gender have not been shown to systematically influence levels of FA [3, 13, 16, 26], though there are clinically important differences in managing FA depending on the child’s developmental status [3]. Specifically, younger children already receive increased support from caregivers for daily tasks, relative to their older counterparts. Consequently, the phenomenology of the accommodating behaviors may vary accordingly (e.g., accommodation with activities of daily living versus accommodation to help an adolescent complete academic or vocational demands).
Additionally, increased comorbid child psychopathology has been linked with higher levels of FA, including internalizing and externalizing behaviors [5, 16]. When considering depressive symptoms, findings have been inconsistent, as some studies found a significant relationship between higher depressive symptoms and certain aspects of FA [6] while others did not [3]. Externalizing disorders such as attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD) are of particular interest in understanding FA. Difficulties with disinhibition, emotion regulation, and oppositionality may contribute to anger outbursts, which occur with relative frequency and can functionally coerce families into giving in to the symptoms [27,28,29]. Furthermore, externalizing symptoms mediate the relationship between obsessive–compulsive symptom severity and FA [6]. Taken together, various forms of comorbid psychopathology have been linked to increased FA in youth with OCD, but examinations into how these symptoms may modulate the relationship between obsessive–compulsive symptoms and FA are still lacking. Additionally, although the link between FA and OCD-related functional impairment has been documented [4, 14, 16], no studies have investigated potential mediators of this specific relationship. Identifying mediators will help clarify how FA interacts with other factors and contributes to disorder-related burden, which will subsequently help better inform interventions. Given the compounding impact of co-occurring psychopathology and the exacerbating nature of comorbid externalizing symptoms and rage outbursts [29], it will be important to consider the intermediary role of comorbid internalizing and externalizing symptoms in the link between FA and impairment.
Family accommodation is a common, multifaceted phenomenon in pediatric OCD that affects families in a similarly multifaceted manner. Given the negative consequences of these behaviors, it is imperative to better understand factors that may influence the presentation and impact of accommodation. This is particularly important in light of the conflicting findings for the relationships between FA, obsessive–compulsive symptom severity, and comorbid symptomology [3, 6, 13]. Additionally, more detailed investigations that can provide a clinical profile of youth presenting with higher levels of accommodation are necessary. In hopes of filling the gaps in the literature and clarifying the impact of certain clinical factors on FA in pediatric OCD, the present study proposes the following aims:
-
(1)
Investigate the general phenomenology of FA.
-
(2)
Examine whether there is a specific sociodemographic (age, gender, parental education status) or clinical profile (OCD symptom severity, OCD symptom subtype) that is associated with increased FA.
-
(3)
Explore whether having a comorbid mood disorder, anxiety disorder, ADHD, or ODD moderates the relationship between obsessive–compulsive symptom severity and FA.
-
(4)
Examine if the severity of comorbid psychopathology symptoms (internalizing, externalizing) mediates the relationship between FA and OCD-related functional impairment.
Method
Participants and Procedure
Participants were recruited from the University of South Florida and Massachusetts General Hospital for a study examining the augmentation of cognitive behavioral therapy with d-cycloserine or placebo in treating pediatric OCD (see Storch et al. [30] for more study details). Informed consent was obtained from all individual participants included in the study. Data on diagnoses were collected at an initial screening visit to assess eligibility. All other data were collected at a second assessment session, approximately 1 week after this first assessment. Participants were included in the current study if the parent completed the measure of FA, if they presented with a current primary or co-primary OCD diagnosis, and had a CY-BOCS score ≥ 16. This resulted in a sample of 150 youth (75 from each site), with 50.7% of the sample being female and the mean age being 12.39 years (SD = 3.07, range = 7–17). The most common comorbid disorders were anxiety disorders (40.0%), ADHD (18.2%), mood disorders (14.0%), and ODD (14.0%).
Participants were predominantly of white non-Hispanic backgrounds (77.3%), with other participants reporting Hispanic (13.3%), African-American (3.3%), or other (5.3%) ethnic backgrounds. Most lived with both biological parents (76.7%), though a minority lived with a single parent (12.7%), with a parent and stepparent (3.3%), or had other living situations (7.3%). Parental education typically involved college: graduate professional degrees (fathers 30.0%, mothers 26.0%), undergraduate degrees (fathers 31.3%, mothers 40.0%), or partial college (fathers 25.3%, mothers 23.3%). High school education or less was reported by 12.0% of fathers and 10.7% of mothers. Most youth (76.0%) attended public schools, 16.7% attended private school, and 7.3% were home schooled. Over half of the participants (65.3%) had previously received therapy for emotional, psychiatric, or behavioral problems.
Measures
The Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version
The KSADS-PL [31] is a semi-structured clinician interview conducted with the parent and child to assess current and lifetime disorders according to DSM-IV [32] criteria. For the current study, only diagnoses that were reported as current and definite were included. Mood disorders included unipolar and bipolar depressive disorders. Anxiety disorders included panic disorder, agoraphobia, separation anxiety disorder, specific phobias, social anxiety disorder, and generalized anxiety disorder.
Children’s Yale-Brown Obsessive Compulsive Scale
The CY-BOCS [33] is a semi-structured, clinician-administered interview completed with the parent and the child, assessing OCD symptoms in the past week. The CY-BOCS assesses obsessions and compulsions in two ways. First, a symptom checklist is presented, organized into various symptom clusters. Each item is scored as 0 (absent) or 1 (present). Højgaard and colleagues [34] recently developed an updated factor model for the symptom checklist, consisting of harm/sexual symptoms (24 items), symmetry/hoarding (19 items) and contamination/cleaning (18 items). Total scores for each factor are calculated by summing the items in each factor. Second, there are ten severity items scored from 0 to 4 that assess the severity of obsessions and compulsions; the total severity score is calculated by summing the severity items. Excellent psychometric properties have been reported [33, 35]. In the current study, internal consistency of the total severity score was good (α = .86).
Clinical Global Impression Scale—Severity
The CGI-S [36] is a clinician-rated single item of global OCD severity rated from 0 (no illness) to 6 (extremely severe symptoms). Severity is rated according to the level of patient distress, observed symptoms, and functional impairment.
Children’s Depression Rating Scale—Revised
The CDRS [37] is a clinician-administered interview with the parent and child that assesses the severity of depression symptoms. It contains 17 items; 14 are scored from 1 to 7 and three items are scored from 1 to 5. The CDRS has good psychometric properties and is widely used to assess youth depressive symptoms [38]. The CDRS total score had good internal consistency in the present study (α = .85).
Child Obsessive–Compulsive Impact Scale, 21 Item Version
The COIS [39] assesses the functional impact of OCD across school, social, and home/family domains. There are separate parent-report (COIS-P) and child-report (COIS-C) versions. Items are scored from 0 (not at all) to 3 (very much). The first 20 items are summed to form a total impact score, and a final item not included in the total score assesses overall impact in these different areas. The total score and subscales have good reliability and show convergent validity with the CY-BOCS [39]. The internal consistency of the total scores were good for both parent- (α = .89) and youth- (α = .87) report versions in the present study.
Family Accommodation Scale for Obsessive–Compulsive Disorder Interviewer Rated
The FAS-IR [8] is a clinician-administered, semi-structured interview conducted with the parents. The FAS-IR assesses the presence, frequency, and severity of FA in the past week using 12 items scored from 0 (no/not applicable) to 4 (every day/extreme). These items assess accommodating behaviors such as participation in compulsions, the impact of OCD on the family, and modifications resulting from the OCD. The FAS-IR has good internal consistency (α = .82) and demonstrates convergent validity with OCD symptom severity, patient global functioning, and family functioning [8]. Current study internal consistency was moderate (α = 0.77).
Child Behavior Checklist
The CBCL [40] is a widely used parent-report measure of youth psychopathology consisting of 113 items scored from 0 (not true) to 2 (very true or often true). The current study utilized the internalizing (32 items) and externalizing (35 items) main scales. The CBCL has good sensitivity and specificity as a screening measure [41]. Internal consistency was good for the internalizing (α = .91) and externalizing (α = .89) problems scales in the present study.
Multidimensional Anxiety Scale for Children
The MASC [42] is a child self-report questionnaire of anxiety containing 39 items scored from 0 (never true) to 3 (often true about me). The anxiety symptoms assessed include social anxiety, separation anxiety, physical symptoms, and harm avoidance, which are summed to form a total score. The MASC has good reliability (α = .89) and validity [43]. Current study internal consistency of the MASC total score was good (α = .92).
Data Analysis
Non-parametric tests were selected for bivariate analyses as most variables were not normally distributed, as indicated by the Shapiro–Wilk test of normality (p < .001). Bivariate associations were examined using Spearman’s correlations for continuous independent variables, as well as the Mann–Whitney U and Kruskal–Wallis tests for categorical independent variables. Hierarchical linear regression was conducted to assess potential moderator variables. Moderation was indicated by a significant interaction effect between the moderator and the independent variable, and a statistically significant R-squared change associated with the interaction. If a significant interaction was detected, simple slopes analyses were conducted to examine group effects. Variable transformations were required to meet the assumptions of linear regression analyses; square-root transformation was performed on FAS-IR scores, and the CY-BOCS scores were mean-centered. Mediation analyses were conducted using the INDIRECT macro for SPSS [44], which utilizes a bootstrapping method to test the indirect effect of the mediator variable. The number of bootstrapped resamples was set at 5000, and the indirect mediation effect was considered significant if the 95% confidence interval of the effect did not include 0. If less than 10% of a scale’s items were missing, missing items were replaced using mean substitution. If more than 10% of the items were missing, the response was coded as missing.
Results
Phenomenology of FA
Descriptive data for FAS-IR items are presented in Table 1. The most commonly reported types of FA in the past week were providing reassurance (80.0%) and refraining from saying or doing things due to their child’s OCD (70.7%). Deliberately watching the child complete rituals (12.7%) and facilitating compulsions (26.0%) were reported most infrequently. Overall, 99.3% of parents reported some type of FA in the past week (at least 1 item > 0), and 82.7% reported engaging in at least one type of FA daily and/or in an “extreme” manner.
Bivariate Associations of FA with Sociodemographic and Clinical Variables
FAS-IR total scores were not significantly associated with any demographic variable, including age (rs = − .16, p = .06), gender (Mann–Whitney U = 2705.00, p = .69), child’s ethnicity (Kruskal–Wallis test = 4.08, df = 2, p = .13), or education levels of the father (Kruskal–Wallis test = 1.59, df = 3, p = .66) or mother (Kruskal–Wallis test = 1.97, df = 3, p = .58). It was also not significantly associated with the child’s history of previous mental health treatment (Mann–Whitney U = 2791.50, p = .34).
FAS-IR total scores were compared between individuals with different diagnostic profiles. FAS-IR total scores were significantly higher in those with comorbid ADHD (Md = 18, IQR = 13–26) than those without ADHD (Md = 13, IQR = 8–20), Mann–Whitney U = 2169.00, p < .01. FAS-IR total scores were also significantly higher in those with comorbid ODD (Md = 20.5, IQR = 14.25–26.00) compared to those without comorbid ODD (Md = 13, IRQ = 8–20), Mann–Whitney U = 1531.00, p < .01. FAS-IR total scores were not associated with the presence of a comorbid mood disorder (Mann–Whitney U = 1424.00, p = .71) or anxiety disorder (Mann–Whitney U = 2423.50, p = .29).
Table 2 presents the descriptive statistics of other clinical variables, along with their correlations with FAS-IR. FAS-IR total scores were significantly and positively correlated with OCD symptom severity (CY-BOCS and CGI-S), the number of contamination/cleaning OCD symptoms, CBCL subscales (internalizing and externalizing problems), and OCD-related impairment. FAS-IR total scores were negatively correlated with the number of harm/sexual OCD symptoms.
Moderating Effects of Comorbid Diagnoses on the Relationship Between FA and OCD Symptom Severity
Hierarchical linear regression was conducted to determine whether the presence of comorbid mood disorder, anxiety disorder, ODD, or ADHD significantly moderated the effect of the CY-BOCS total severity score on FAS-IR total scores. The presence of a comorbid anxiety disorder significantly moderated the relationship between OCD severity and FAS-IR; the increase in variation explained by the interaction between OCD severity and anxiety disorder status was 3.5%, F(1,146) = 5.67, p = .02. Simple slopes analysis indicated that there was a significant positive linear relationship between OCD severity and FA in those without comorbid anxiety [n = 90; β = 0.09, (95% CI: 0.05, 0.13), S.E. = 0.02, p < .001], but the relationship was not significant in those with a comorbid anxiety disorder [n = 60; β = 0.01, (95% CI: − 0.04, 0.06), S.E. = 0.02, p = .64].
The presence of a comorbid mood disorder did not moderate the relationship between OCD severity and FA, as the addition of the interaction between OCD severity and comorbid mood disorder status did not significantly increase the variation explained in the model [F(1,146) = 0.04, p = .84]. The relationship between OCD severity and FA was also not moderated by the presence of ADHD [F(1,144) = 1.46, p = .23], nor the presence of ODD (F(1,145) = 0.69, p = .41).
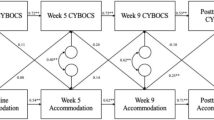
Mediation of the Relationship Between FA and the Impact of OCD by Internalizing/Externalizing Symptoms
Table 3 presents results from analyses regarding potential mediation of CBCL subscales in the relationship between FA and parent-reported impact of OCD (COIS-P). The results indicated that CBCL internalizing and externalizing both significantly and independently mediated the association between FA and OCD impact (Figs. 1, 2). In both cases, higher FA scores were associated with higher CBCL subscale scores, and each of the CBCL subscales were positively associated with OCD impact. The direct effect of FAS-IR on OCD impact remained significant after inclusion of mediators.
Discussion
The present study examined the clinical profile and impact of comorbid psychopathology on FA in pediatric OCD. Consistent with previous research, FA was a prominent construct occurring in practically every family in the past week [1,2,3,4,5]. The most common types of FA included verbal reassurance as well as refraining from certain behaviors to avoid triggering the child’s OCD, highlighting the active and passive forms of accommodation. Given the multifaceted nature of these behaviors, it is important to consider the various ways accommodation may manifest and target them accordingly in treatment.
We found that FA was not correlated with any sociodemographic variables. The lack of age and gender associations with FA is consistent with previous literature in pediatric OCD [3, 13, 16, 26], indicating that the levels of accommodation may not be commensurate with the child’s age or gender and that other factors are relevant. Despite these findings, it remains important to consider the phenomenological differences of how accommodating behaviors may differ between youths in various developmental stages; as parental support may be appropriate at younger ages, it is important to distinguish those behaviors from harmful accommodation specific to the child’s OCD symptomology. For instance, assisting a preschool-aged child with their meal preparation would generally be age-appropriate, though engaging in extensive, ritualized preparation of meals for children due to contamination concerns would be addressed as a symptom of OCD. The parents’ education level and the child’s history of previous mental health treatment were not associated with FA, suggesting the likely consistency of these behaviors regardless of these variables.
As predicted, certain clinical features were associated with the severity of FA. Higher obsessive–compulsive symptom severity was linked to higher FA, regardless of which severity measure was examined. This is in line with findings from a recent meta-analysis [13], and it is likely that youths presenting with higher symptom severity demand increased FA. The OCD cluster of contamination symptoms was linked to higher FA, which is also supported by previous findings [3, 5, 6, 25]. However, higher harm/sexual symptoms were linked to decreased FA. The discrepant findings between different symptom clusters could be attributed to the opportunities for accommodation and how sensitive the content may be for the child. For instance, youths with contamination symptoms can receive accommodation in myriad ways throughout the day, such as asking family members to facilitate avoidance (e.g., opening doors or touching dirty objects for them), engage in compulsions (e.g., washing their hands in a specific way), and providing items necessary for compulsions (e.g., purchasing more cleaning supplies). Alternatively, children presenting with harm/sexual symptoms may have decreased opportunities for accommodation, as accommodation may be mostly constrained to reassurance-seeking. This is particularly true if the child struggles with sharing the content s/he perceives as grotesque or amoral, making him/her less apt to seek accommodation from family members. Lastly, in line with the theory that accommodation feeds into the negative reinforcement cycle of OCD, these behaviors were linked to higher levels of OCD-related impairment [14, 16]. As families continue to give into the OCD, the symptomology and related impairment are functionally maintained through the accommodation behaviors [15].
Family accommodation was positively correlated with parent-reported internalizing symptoms, which is consistent with previous research [5, 16]. When anxiety and depression were examined separately, a different pattern emerged; FA was not significantly correlated with depression or anxiety symptoms, nor with the presence/absence of the respective diagnoses. The inconsistencies between these findings deserve further examination. There are differences in reporters across measures, which could account for some differences in findings; the measures include parent self-report measures about their child, clinician consensus of parent and child reports, and child self-report. Alternatively, the results may reflect a relationship between FA and the range of symptoms assessed in the CBCL internalizing scale’s anxiety, depression, withdrawal, and somatic symptoms. The role of specific internalizing symptoms should thus be explored in future research. Further, the lack of association between depression and overall FA is consistent with findings from Stewart, et al. [3], and it is possible that depression is related only to specific types of FA such as modification of routines [6]. The prevalence and presentation of FA is similar in youth with OCD and anxiety disorders [4, 45, 46], so it is also conceivable that anxiety disorders alone do not significantly increase FA over and above the influence of OCD.
Higher parent-reported externalizing behaviors were significantly correlated with increased FA, and youths with comorbid ADHD and ODD diagnoses both demonstrated higher levels of accommodation than youth without these disorders. The findings of an association between externalizing problems and FA is consistent with previous research [5, 6, 16], and illustrates the impactful nature of problematic externalizing behaviors. Difficulties with attention, impulse control, and anger outbursts make it challenging for the child to tolerate distress and adaptively manage their anxiety independently; these outward expressions of distress occur in pediatric OCD with relative frequency, often leading to higher incidences of accommodation [29]. Given these considerations, it is important for clinicians to effectively manage these behaviors within the context of treating the child’s OCD, including evidence-based parent management strategies to help support the child to better cope with the OCD-related distress with self-efficacy [47].
Moderation analyses were conducted to see if the relationship between FA and OCD severity differed according to the presence of specific comorbid disorders. There was no evidence of a moderation effect for comorbid ADHD, ODD, or mood disorders. As such, the presence of these disorders may not impact the relationship between OCD symptom severity and FA. Instead, it could be that individual symptoms (externalizing, internalizing) are more directly related to FA regardless of OCD symptom severity, given their positive correlations with one another. Interestingly, there was significant moderation effect of anxiety disorders, such that there was a positive association between FA and OCD symptom severity in those without a comorbid anxiety disorder, but there was no association in those with an anxiety disorder. Again, given that youth with anxiety disorders present with similar levels of FA [4, 45, 46], these youth may already seek FA with relative frequency due to their heightened anxiousness, irrespective of OCD symptom severity. Without the presence of a comorbid anxiety disorder, a more linear relationship between OCD and FA can appear. In considering OCD-related impairment, internalizing and externalizing problems were found to mediate the relationship between FA and OCD-related functional impairment. As FA occurs, it reinforces the obsessional distress, given that it feeds into the negative reinforcement cycle that maintains OCD. As such, youth are not able to learn alternative methods to manage their anxiety, sustain their attention, and cope with the distress at hand, nor self-regulate when they experience rage outbursts triggered by their OCD. The confluence of all these factors feed into their heightened level of impairment, exacerbating the disability and impairment related to OCD.
These findings should be interpreted in light of several limitations. First, data were cross-sectional in nature, limiting the ability to draw inferences of causality and directionality. However, it is noted that examinations of reverse meditational models were conducted and found to be nonsignificant to ensure that mediation findings were not spurious. Future studies should seek to clarify the direction of the effects, though it is likely that the impacts are bidirectional. Second, given that different results were found depending on the informant of the measure, it is important to highlight the utility of using multiple informants to gather a more holistic representation of the symptomology. It may be preferable to use parallel parent and child versions of the same measure to improve interpretability of parent and child reports. Future studies should seek to continue to use multi-informant, multi-method measures and investigate potential reasons for differences in reporting. Third, the type of measure used for assessing FA may also partly explain differences in findings, given that there are different relationships between obsessive–compulsive symptom severity and accommodation depending on which FA questionnaire is used [13]. Moving forward, future studies should seek to use more consistent and standardized methods for evaluating FA to enhance comparability across studies.
Summary
Ultimately, this study elucidated the phenomenology, related clinical variables, and impact of comorbid psychopathology on FA in pediatric OCD. FA continues to be linked with increased functional impairment and higher obsessive–compulsive symptom severity, reflecting the importance of targeting these behaviors in treatment. However, less has been known about how other factors, such as comorbid psychopathology, may modulate the relationship between FA and other variables. Based on the present findings, externalizing behaviors and comorbid diagnoses of ADHD and ODD were repeatedly associated with increased FA in various manners, illustrating the compounded, negative effect of these symptomology. Similarly, continued accommodation may lead to increased internalizing and externalizing problems, resulting in higher OCD-related impairment. Youths presenting with these symptoms are typically characterized as having amplified difficulties with managing their symptoms in an independent and adaptive manner, underscoring the need for additional supports to help them develop more appropriate coping skills and familial responses in treatment. As such, family-based treatments designed to target these specific symptoms and integrate family members in the therapeutic process are expected to be particularly efficacious. Taken collectively, future studies should conduct more nuanced investigations to determine how various factors may contribute to increased FA and impact its relationship with other clinical variables of interest.
References
Futh A, Simonds LM, Micali N (2012) Obsessive-compulsive disorder in children and adolescents: parental understanding, accommodation, coping and distress. J Anxiety Disord 26:624–632
Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J (2008) Correlates of accommodation of pediatric obsessive-compulsive disorder: parent, child, and family characteristics. J Am Acad Child Adolesc Psychiatry 47:1173–1181
Stewart SE, Beresin C, Haddad S, Egan Stack D, Fama J, Jenike M (2008) Predictors of family accommodation in obsessive-compulsive disorder. Ann Clin Psychiatry 20:65–70
Lebowitz ER, Panza KE, Bloch MH (2016) Family accommodation in obsessive-compulsive and anxiety disorders: a five-year update. Expert Rev Neurother 16:45–53
Lebowitz ER, Panza KE, Su J, Bloch MH (2012) Family accommodation in obsessive-compulsive disorder. Expert Rev Neurother 12:229–238
Wu MS, Lewin AB, Murphy TK, Geffken GR, Storch EA (2014) Phenomenological considerations of family accommodation: related clinical characteristics and family factors in pediatric OCD. J Obsessive Compuls Relat Disord 3:228–235
Calvocoressi L, Lewis B, Harris M, Trufan SJ, Goodman WK, McDougle CJ et al (1995) Family accommodation in obsessive-compulsive disorder. Am J Psychiatry 152:441–443
Calvocoressi L, Mazure CM, Kasl SV, Skolnick J, Fisk D, Vegso SJ et al (1999) Family accommodation of obsessive-compulsive symptoms: instrument development and assessment of family behavior. J Nerv Ment Dis 187:636–642
Storch EA, Björgvinsson T, Riemann B, Lewin AB, Morales MJ, Murphy TK (2010) Factors associated with poor response in cognitive-behavioral therapy for pediatric obsessive-compulsive disorder. Bull Menn Clin 74:167–185
Lewin AB (2014) Tractable impediments to cognitive behavioral therapy for pediatric obsessive compulsive disorder. In: McKay D, Storch EA (eds) Obsessive–compulsive disorder and its spectrum: a lifespan approach. American Psychological Association Press, Washington DC, pp 81–96
American Academy of Child and Adolescent Psychiatry (2012) Practice parameters for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 51:98–113
Abramowitz JS, Taylor S, McKay D (2009) Obsessive-compulsive disorder. Lancet 374:491–499
Wu MS, McGuire JF, Martino C, Phares V, Selles RR, Storch EA (2016) A meta-analysis of family accommodation and OCD symptom severity. Clin Psychol Rev 45:34–44
Storch EA, Larson MJ, Muroff J, Caporino N, Geller D, Reid JM et al (2010) Predictors of functional impairment in pediatric obsessive-compulsive disorder. J Anxiety Disord 24:275–283
Caporino NE, Morgan J, Beckstead J, Phares V, Murphy TK, Storch EA (2012) A structural equation analysis of family accommodation in pediatric obsessive-compulsive disorder. J Abnorm Child Psychol 40:133–143
Storch EA, Geffken GR, Merlo LJ, Jacob ML, Murphy TK, Goodman WK et al (2007) Family accommodation in pediatric obsessive-compulsive disorder. J Clin Child Adolesc Psychol 36:207–216
Morgan J, Caporino NE, Nadai AS, Truax T, Lewin AB, Jung L et al (2013) Preliminary predictors of within-session adherence to exposure and response prevention in pediatric obsessive–compulsive disorder. Child Youth Care Forum 42:181–191
Ferrao YA, Shavitt RG, Bedin NR, de Mathis ME, Carlos Lopes A, Fontenelle LF et al (2006) Clinical features associated to refractory obsessive-compulsive disorder. J Affect Disord 94:199–209
Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA (2009) Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. J Consult Clin Psychol 77:355–360
Garcia AM, Sapyta JJ, Moore PS, Freeman JB, Franklin ME, March JS et al (2010) Predictors and moderators of treatment outcome in the pediatric obsessive compulsive treatment study (POTS I). J Am Acad Child Adolesc Psychiatry 49:1024–1033
Piacentini J, Bergman RL, Chang S, Langley A, Peris TS, Wood JJ et al (2011) Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 50:1149–1161
Thompson-Hollands J, Abramovitch A, Tompson MC, Barlow DH (2015) A randomized clinical trial of a brief family intervention to reduce accommodation in obsessive-compulsive disorder: a preliminary study. Behav Ther 46:218–229
Thompson-Hollands J, Edson A, Tompson MC, Comer JS (2014) Family involvement in the psychological treatment of obsessive-compulsive disorder: a meta-analysis. J Fam Psychol 28:287–298
Gomes JB, Cordioli AV, Heldt E (2017) Obsessive-compulsive disorder and family accommodation: a 3-year follow-up. Psychiatry Res 253:107–109
Albert U, Bogetto F, Maina G, Saracco P, Brunatto C, Mataix-Cols D (2010) Family accommodation in obsessive-compulsive disorder: Relation to symptom dimensions, clinical and family characteristics. Psychiatry Res 179:204–211
Flessner CA, Sapyta J, Garcia A, Freeman JB, Franklin ME, Foa E et al (2009) Examining the psychometric properties of the family accommodation scale-parent-report (FAS-PR). J Psychopathol Behav Assess 31:38–46
Lebowitz ER, Omer H, Leckman JF (2011) Coercive and disruptive behaviors in pediatric obsessive-compulsive disorder. Depress Anxiety 28:899–905
Lebowitz ER, Vitulano LA, Omer H (2011) Coercive and disruptive behaviors in pediatric obsessive compulsive disorder: a qualitative analysis. Psychiatry 74:362–371
Storch EA, Jones AM, Lack CW, Ale CM, Sulkowski ML, Lewin AB et al (2012) Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. J Am Acad Child Adolesc Psychiatry 51:582–592
Storch EA, Wilhelm S, Sprich S, Henin A, Micco J, Small BJ et al (2016) Efficacy of augmentation of cognitive behavior therapy with weight-adjusted d-Cycloserine vs placebo in pediatric obsessive-compulsive disorder: a randomized clinical trial. JAMA Psychiatry 73:779–788
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders 4th edn. American Psychiatric Association, Washington, DC
Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK et al (1997) Children’s yale-brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 36:9
Højgaard DRMA, Mortensen EL, Ivarsson T, Hybel K, Skarphedinsson G, Nissen JB et al (2016) Structure and clinical correlates of obsessive–compulsive symptoms in a large sample of children and adolescents: a factor analytic study across five nations. Eur Child Adolesc Psychiatry:1–11. https://doi.org/10.1007/s00787-016-0887-5
Storch EA, Murphy TK, Geffken GR, Soto O, Sajid M, Allen P et al (2004) Psychometric evaluation of the children’s yale-brown obsessive-compulsive scale. Psychiatry Res 129:91–98
Guy W (1976) Clinical global impressions. Guy W (ed) ECDEU assessment manual for psychopharmacology. National Insitute of Mental Health, Rockville
Poznanski EO, Mokros HB (1996) Children’s depression rating scale, revised manual. Western Psychological Services, Los Angeles
Myers K, Winters NC (2002) Ten-year review of rating scales. II: scales for internalizing disorders. J Am Acad Child Adolesc Psychiatry 41:634–659
Piacentini J, Jaffer M, Bergman RL, McCracken J, Keller M (2001) Measuring impairment in childhood OCD: Psychometric properties of the COIS. Proceedings of the American Academy of Child and Adolescent Psychiatry Meeting, p 146
Achenbach TM, Rescorla LA (2001) Manual for AESBA school-age forms & profiles. Research Center for Children, Youth, & Families, University of Vermont, Burlington
Warnick EM, Bracken MB, Kasl S (2008) Screening efficiency of the child behavior checklist and strengths and difficulties questionnaire: a systematic review. Child Adolesc Ment Health 13:140–147
March JS, Parker JDA, Sullivan K, Stallings P, Conners CK (1997) The multidimensional anxiety scale for children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry 36:554–565
Baldwin JS, Dadds MR (2007) Reliability and validity of parent and child versions of the multidimensional anxiety scale for children in community samples. J Am Acad Child Adolesc Psychiatry 46:252–260
Preacher KJ, Hayes AF (2008) Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods 40:879–891
Lebowitz ER, Scharfstein LA, Jones J (2014) Comparing family accommodation in pediatric obsessive-compulsive disorder, anxiety disorders, and nonanxious children. Depress Anxiety 31:1018–1025
Lebowitz ER, Woolston J, Bar-Haim Y, Calvocoressi L, Dauser C, Warnick E et al (2013) Family accommodation in pediatric anxiety disorders. Depress Anxiety 30:47–54
Lebowitz ER (2013) Parent-based treatment for childhood and adolescent OCD. J Obsessive Compuls Relat Disord 2:425–431
Acknowledgements
The authors would like to acknowledge the contributions of Chelsea Ale, Ph.D., Noah Berman, Ph.D., Jennifer Britton, Ph.D., Ashley Brown, B.A., Kathleen Carey, CNS, Anne Chosak Ph.D., Allison Cooperman BA, Angelina Gomez, B.A., David Greenblatt, M.D., Marni Jacob, Ph.D., Joseph McGuire, Ph.D., Nicole McBride, B.S., Scott Orr, Ph.D., Jennifer Park, Ph.D., David Pauls, Ph.D., Kesley Ramsey, B.A., Robert Selles, Ph.D., Abigail Stark, B.A., and Christine Cooper Vince, Ph.D.
Funding
This work was supported by grants to the second and last authors from the National Institutes of Health (Grant Nos. 5R01MH093402 and 1R01MH09338). The funding organization was not involved in the design or conduct of the study, collection, management, analysis, and interpretation of the data or preparation, review, and approval of the manuscript. The views in this manuscript reflect that of the authors and not the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
MSW, SCS, and EAS all contributed to the initial draft of the manuscript. SCS and BJS spearheaded the statistical analyses. DAG, TKM, and SW were key personnel in the trial and have reviewed/approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Wu has received grant or research support from the NIMH (T32MH073517). Dr. Geller reports grant support from NIH and book honorarium from the American Academy of Child and Adolescent Psychiatry, speaking honoraria for Advanced Institute lectures from the American Academy of Child and Adolescent Psychiatry and Massachusetts General Hospital Psychiatry Academy in educational programs supported through independent medical education grants from pharmaceutical companies. Lifetime funding includes support from the Obsessive Compulsive Disorder Foundation, The Tourette Syndrome Association, The McIngvale Family Foundation, Eli Lilly, Pfizer, and Glaxo Smith Kline. Drs. Schneider and Small have no conflicts of interest to report. Dr. Murphy reports having received or is receiving research funding from Auspex Pharmaceuticals, National Institute of Mental Health, Shire Pharmaceuticals, Pfizer, F. Hoffmann–La Roche Ltd, AstraZeneca Pharmaceuticals, Centers for Disease Control and Prevention, Massachusetts General Hospital, Sunovion Pharmaceuticals, Neurocrine Biosciences, PANDAS Network, and Psyadon Pharmaceuticals. Dr. Wilhelm has received research support in the form of free medication and matching placebo from Forest Laboratories for clinical trials funded by the NIH. Dr. Wilhelm is a presenter for the Massachusetts General Hospital Psychiatry Academy in educational programs supported through independent medical education grants from pharmaceutical companies; she has received royalties from Elsevier Publications, Guilford Publications, New Harbinger Publications, and Oxford University Press. Dr. Wilhelm has also received speaking honorarium from various academic institutions and foundations, including the International Obsessive Compulsive Disorder Foundation and the Tourette Association of America. In addition, she received payment from the Association for Behavioral and Cognitive Therapies for her role as Associate Editor for the Behavior Therapy journal, as well as from John Wiley & Sons, Inc. for her role as Associate Editor on the journal Depression & Anxiety. Dr. Wilhelm has also received salary support from Novartis and Telefonica Alpha, Inc. Dr. Storch has received funding from the National Institute of Health and All Children’s Hospital Research Foundation. He receives book royalties from Elsevier, Springer, Wylie, and American Psychological Association.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, M.S., Geller, D.A., Schneider, S.C. et al. Comorbid Psychopathology and the Clinical Profile of Family Accommodation in Pediatric OCD. Child Psychiatry Hum Dev 50, 717–726 (2019). https://doi.org/10.1007/s10578-019-00876-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-019-00876-7