Abstract
Oxidative stress is a great challenge to neurons following cerebral ischemia. PGC-1α has been shown to act as a potent modulator of oxidative metabolism. In this study, the effects of ZLN005, a small molecule that activate PGC-1α, against oxygen–glucose deprivation (OGD)- or ischemia-induced neuronal injury in vitro and in vivo were investigated. Transient middle cerebral artery occlusion (tMCAO) was performed in rats and ZLN005 was administered intravenously at 2 h, 4 h, or 6 h after ischemia onset. Infarct volume and neurological deficit score were detected to evaluate the neuroprotective effects of ZLN005. Well-differentiated PC12 cells, which were subjected to OGD for 2 h followed by reoxygenation for 22 h, were used as an in vitro ischemic model. Changes in expression of PGC-1α, its related genes, and antioxidant genes were determined by real-time quantitative PCR. The results showed that ZLN005 reduced cerebral infarct volume and improved the neurological deficit in rat with tMCAO, and significantly protected OGD-induced neuronal injury in PC12 cells. Furthermore, ZLN005 enhanced expression of PGC-1α in PC12 cells and in the ipsilateral hemisphere of rats with tMCAO. Additionally, ZLN005 increased antioxidant genes, including SOD1 and HO-1, and significantly prevented the ischemia-induced decrease in SOD activity. Taking together, the PGC-1α activator ZLN005 exhibits neuroprotective effects under ischemic conditions and molecular mechanisms possibly involve activation of PGC-1α signaling pathway and cellular antioxidant systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke, especially ischemic stroke, is a common neurological disease that leads to significant morbidity and mortality all over the world (Gao et al. 2015; Wang et al. 2014; Xue et al. 2016; Yang et al. 2014; Yu et al. 2014). At present, tissue plasminogen activator (tPA) is the only thrombolytic agent approved for acute ischemic stroke by the United States Food and Drug Administration (Gu et al. 2016; Xue et al. 2016), and thus the development of a novel treatment strategy is urgently needed to improve the prognosis of cerebral ischemia (Xue et al. 2016).
Reactive oxygen species (ROS) are continuously being generated in the normal brain due to the consumption of oxygen (Garcia et al. 2017). Antioxidant systems, including enzymatic antioxidant defense systems such as superoxide dismutase (SOD) and non-enzymatic antioxidants including ascorbic acid and glutathione, together with the generation of ROS, act to maintain redox balance (di Penta et al. 2013; O’Hare Doig et al. 2014). Oxidative stress results from remarkable disturbance of the balance, either by defects in antioxidant system or by the excessive production of ROS, and causes damage to cells (Bian et al. 2016; Ho et al. 2015; Liu et al. 2015; Mossakowski et al. 2015; Park et al. 2016). While oxidative stress affects all types of cells in the brain, neurons are particularly vulnerable to oxidative challenges, and oxidative damage caused by ROS has been implicated in ischemic stroke (Gao et al. 2015; Ritzel et al. 2016; Sharma et al. 2013; Shulyakova et al. 2014). Therefore, antioxidants have been implied to an effective therapeutic strategy in the treatment of ischemic stroke.
Peroxisome proliferator-activated receptor-gamma coactivator-1α (PGC-1α) is a transcriptional coactivator regulating cellular energy metabolism, which is abundantly expressed in the brain (Zhang et al. 2013). Evidence show that PGC-1α is associated with the regulation of the defense system against reactive oxygen species (Mäkelä et al. 2016; Singh et al. 2016; Szalardy et al. 2016; Wu et al. 2016), by enhancing the expression of antioxidant genes (Xiao and Goswami 2015). Additionally, upregulation of PGC-1α levels dramatically protected neural cells against oxidative stress-mediated death (Mudò et al. 2012; Peng et al. 2015), while loss of its activity resulted in an increase in mitochondrial-derived ROS (García-Quintans et al. 2016).
Heme oxygenase 1 (HO-1), an inducible enzyme in catalyzing heme to biliverdin, carbon monoxide, and iron, exerts a crucial role in restoring redox balance. Significant induction of HO-1 expression is discovered after acute cerebral ischemic injury and showed to protect neurons against oxidative stress (Ding et al. 2015; Qi et al. 2014). Furthermore, HO-1 was reported to improve SOD activity, suggesting the potent neuroprotection effect of HO-1 in stroke treatment.
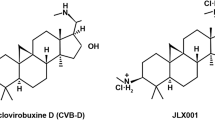
ZLN005, also known as 2-(4-tert-Butylphenyl) benzimidazole (Fig. 1a), is reported to be a PGC-1α transcriptional regulator (Zhang et al. 2013). It is speculated that ZLN005 elevates PGC-1α expression (Zhang et al. 2013), and protects cardiomyocytes against high glucose-induced oxidative stress, verified by enhanced cell viability and reduced apoptosis (Li et al. 2016b).
ZLN005 reduces brain damage and improves neurological deficit in rats after tMCAO. a Structure of ZLN005. ZLN005 reduced infarct volume (b, c) and improved the neurological deficit (d) in rat after tMCAO. Data are expressed as the mean ± SD of individual groups of rats (n = 8–12). *p < 0.05, **p < 0.01, ***p < 0.001 versus vehicle group (tMCAO), ### p < 0.001 versus sham group
In this study, we evaluated the neuroprotective effects of ZLN005 against ischemia/reperfusion injury in rat model of transient middle cerebral artery occlusion and oxygen–glucose deprivation (OGD) injury in well-differentiated PC12 cells. We further demonstrated that the neuroprotective effects of ZLN005 treatment were possibly mediated by activation of PGC-1α signaling pathway and improvement of antioxidant systems.
Materials and Methods
Materials
Compound ZLN005 was provided by Prof. Jia Li from Shanghai Institute of Materia Medica, Chinese Academy of Sciences. Dulbecco’s modified Eagles medium (DMEM), fetal bovine serum (FBS), and trypsin were purchased from Invitrogen (Carlsbad, CA, USA). 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT), 2, 3, 5-triphenyltetrazolium chloride (TTC), and poly-l-lysine and were purchased from Sigma-Aldrich (St Louis, MO, USA). Total RNA extraction reagent and SYBR Green Master Mix were purchased from Vazyme (Nanjing, Jiangsu, China). LDH release assay kit and SOD assay kit were purchased from Beyotime Biotechnology (Shanghai, China). All other chemicals and reagents were of analytical grade.
Animals
Male Sprague–Dawley (SD) rats weighing 250–280 g were provided by Zhejiang Laboratory Animals Center (Hangzhou, China). All animals were housed under standard environment and had free access to water and food. All procedures were conducted according to the NIH Guide for the Care and Use of Laboratory Animals published by the US National Academy of Sciences. All animal tests and experimental procedures were approved by the Administration Committee of Experimental Animals in Jiangsu Province and the Ethics Committee of China Pharmaceutical University.
Transient Middle Cerebral Artery Occlusion
Transient middle cerebral artery occlusion (tMCAO) was performed as reported previously (Pang et al. 2016; Wang et al. 2017b). Briefly, the animals were anesthetized and then the right common carotid artery (CCA), external carotid artery (ECA), and internal carotid artery (ICA) were isolated free from the surrounding tissues. A monofilament nylon suture (diameter of approximately 0.26 mm) was inserted into the ICA and gently advanced until it reached to the origin of the MCA. After 2 h of MCAO, the filament was removed to accomplish cerebral reperfusion.
Drug Treatment
Animals were randomly divided into five groups (n = 8–12 per group): sham, vehicle, and ZLN005-treated groups (a single administration of ZLN005 at 2, 4, or 6 h after ischemia onset). Rats in the vehicle group and ZLN005-treated groups were intravenously administered with DMSO or ZLN005 (2.5 mg/kg), respectively.
Measurement of Neurological Deficit and Cerebral Infarct Volume
Behavioral test was conducted at 24 h after tMCAO by a trained and blind observer as previously described (Longa et al. 1989). The neurologic deficits were assessed on a five-point scale: 0, no observable deficits; 1, unable to extend the left forepaw; 2, circling to the left side; 3, reclination to the left side at rest; and 4, failure to move spontaneously. After assessment of neurological deficit, rats were sacrificed and brains were cut into 2-mm-thick coronal sections. The brain sections were stained with 2% TTC for 10 min at 37 °C. The infarct size was measured by morphometric analysis (image-pro plus) as described previously (Pang et al. 2016).
Cell Culture
Well-differentiated PC12 cells were obtained from the Cell Resource Centre of Shanghai Institutes for Biological Sciences, Chinese Academy of Sciences (Shanghai, China). PC12 cells were cultured in DMEM supplement with 10% heat-inactivated FBS and penicillin/streptomycin at 37 °C under a humidified atmosphere of 95% air/5%CO2. For further experiments, PC12 cells were seeded into 24-well plates at a density of 5 × 104/mL cells.
Oxygen and Glucose Deprivation (OGD)
PC12 cells were pretreated with DMSO or ZLN005 (1, 2, 5 µM) for 24 h. After that, cells were washed with PBS for three times and then cultured in DMEM medium without glucose. Then cells were incubated in a hypoxia chamber (1% O2, 94% N2, and 5% CO2) for 2 h. After hypoxia, the cells were treated with ZLN005 (1, 2, or 5 µM) and then cultured in normal DMEM medium under normoxia conditions for 22 h (Liu et al. 2016). Control cells without OGD were maintained under normal conditions.
Semi-quantitative Polymerase Chain Reaction (qPCR)
To determine the levels of gene expression, total RNA was extracted from PC12 cells at 24 h after OGD or the brain cerebral cortex at 24 h after tMCAO using Trizol reagent. Semi-quantitative PCR was performed as reported previously (Xu et al. 2015). The primer pairs are shown in Table 1. The GAPDH normalized data are presented as the fold change in gene expression.
MTT Assay
Cell viability was determined by MTT assay as reported previously (Chang et al. 2016, 2017). Briefly, PC12 cells cultured in 96-well plates (6 × 103 cells per well) were treated with DMSO or various concentrations of ZLN005 (1, 2, 5 µM) for 24 h and then exposed to OGD for 2 h. After that, OGD was terminated and the cells were further cultured for 22 h with ZLN005 (1, 2, 5 µM). Then cells were incubated with MTT (0.5 mg/mL) for 4 h at 37 °C. The medium with MTT was then removed and DMSO was added to each well and absorbance was measured at 570 nm in a TACAN plate reader.
LDH Assay
Cell death after exposed to OGD was determined by measuring the activity of lactate dehydrogenase (LDH) released into culture medium. Briefly, PC12 cell seeded in 96-well plates were treated with ZLN005 (1, 2, 5 µM) for 24 h and then exposed to OGD injury for 2 h. The culture medium was collected and the LDH activity was measured using the LDH release assay kit according to the manufacturer’s recommendations.
SOD Measurement
The SOD assay kit was purchased from Beyotime Biotechnology (Shanghai, China). Brain cortices were collected at 24 h after MCAO and then homogenized. The SOD activity was measured using the SOD assay kit according to the manufacturer’s instructions.
Western Blotting
At 24 h after tMCAO, rat brain cortex samples were collected and homogenized with RIPA buffer (Vazyme, Jiangsu, China). The extracted protein was quantified by BCA kit (Thermo, Rockford, IL). Western blot was performed as previously described (Xu et al. 2015). Briefly, proteins were separated by SDS-PAGE gels and then transferred onto polyvinylidene difluoride (PVDF) membranes. The membranes were blocked for 2 h with 3% bovine serum albumin (BSA) and then incubated overnight at 4 °C with primary antibodies including HO-1 (1:250, Abcam, Cambridge, MA, USA), PGC-1α (1:1000, #A12348, ABclonal, Wuhan, China), and β-actin (1:1000, Santa Cruz Biotechnology, CA, USA). After washing for five times (6 min per wash) with TBST, the membranes were incubated with the secondary antibodies for 1 h at room temperature. The membranes were then washed again and the transferred proteins were visualized with a Bio-Rad ChemiDoc XRS.
Statistical Analysis
All data were expressed as Mean ± standard deviation (SD) from at least three independent experiments. Statistical analysis was performed using one-way ANOVA followed by Bonferroni’s test. A p < 0.05 was considered statistically significant.
Results
ZLN005 Reduced Brain Damage and Improved Neurological Deficit in Rats After tMCAO
To evaluate whether treatment with ZLN005, also known as 2-(4-tert-Butylphenyl) benzimidazole (Fig. 1a), protects brain against ischemia-induced damage, rats were subjected to tMCAO model and intravenously treated with vehicle or ZLN005 (2.5 mg/kg) at 2, 4, or 6 h after ischemia onset. Two correlated parameters, brain infarct volume and neurological deficit, were measured at 24 h after tMCAO. Tissue damage was observed on the ipsilateral hemisphere as illustrated by the white area with an accurate delineation of the penumbra after ischemic injury (Fig. 1b). There was a significant reduction in infarct volume in ZLN005-treated groups as compared with vehicle group (p < 0.001 for 2 h group, p < 0.001 for 4 h group, and p < 0.01 for 6 h group, Fig. 1b, c). As shown in Fig. 1d, treatment with ZLN005 at 4 h after ischemia onset significantly improved the neurological deficit compared to the vehicle group (p < 0.05 vs. vehicle). These results showed that ZLN005 improved neurological outcomes caused by ischemic stroke. As ZLN005 administration at 4 h after ischemia onset performed a maximum protective effect, this time point was chosen to further study the neuroprotective mechanism of ZLN005.
ZLN005 Activated PGC-1α and Related Genes in Rats After tMCAO
Emerging evidence demonstrate that activation of PGC-1α protects against ischemia-induced brain damage (Li et al. 2016a; Ma et al. 2016). ZLN005 has been reported as a PGC-1α activator in myotubes (Zhang et al. 2013). We checked the expression of PGC-1α and its related genes (cytochrome c, COX5b, and AOX) in the ipsilateral cerebral cortices following tMCAO. There was a significant increase in PGC-1α mRNA expression in ZLN005-treated group compared to the vehicle group (p < 0.05 vs. vehicle, Fig. 2a). Moreover, post-ischemia treatment with ZLN005 also significantly increased the mRNA expression of PGC-1α target genes, cytochrome c (p < 0.001 vs. vehicle, Fig. 2b), COX5b (p < 0.01 vs. vehicle, Fig. 2c), and AOX (p < 0.01 vs. vehicle, Fig. 2d). These results showed that ZLN005 exhibited neuroprotective effect possibly via the upregulation of PGC-1α and related genes.
ZLN005 increases PGC-1α and related genes expression in rat brain. ZLN005 upregulated the mRNA expression of PGC-1α (a) and related genes: cytochrome c (b), COX5b (c), and AOX (d) in the ipsilateral hemisphere of rat brain after tMCAO when compare to vehicle. GAPDH was used as an internal control. Data are expressed as the mean ± SD of individual group of rats (n = 4). *p < 0.05, **p < 0.01, ***p < 0.001 versus vehicle group
ZLN005 Enhanced Expression of the Antioxidant Genes in Rats After tMCAO
Oxidative stress is a fundamental mechanism of cell damage following cerebral ischemia (Shirley et al. 2014). Hence, we evaluated ROS-detoxifying potentials of ZLN005 by quantifying mRNA expression of antioxidant genes SOD1 and HO-1, detecting the expression of HO-1 protein and measuring SOD activities. There was a significant increase in SOD1 and HO-1 mRNA expression (p < 0.05 for SOD1, p < 0.05 for HO-1, Fig. 3a, b) and HO-1 protein expression (p < 0.05 vs. vehicle, Fig. 3c) in the ipsilateral cortices of ZLN005-treated group when compared with vehicle group. SOD activity in the vehicle group was markedly decreased at 24 h after tMCAO compared to sham group, while ZLN005 treatment significantly improved SOD activity (p < 0.05 vs. vehicle, Fig. 3d). These results indicated that compound ZLN005 improved ischemic stroke-induced reduction in antioxidant activities, which may contribute to the neuroprotective effect of ZLN005.
ZLN005 enhances the expression of antioxidant genes in rats after tMCAO. Semi-quantitative PCR evaluation of SOD1 (a) and HO-1 (b) mRNA expression showed significant increase in gene upregulation on the ipsilateral hemisphere of rat brain 24 h after tMCAO. c Effect of ZLN005 on HO-1 protein expression in the ipsilateral hemisphere of rat brain 24 h after tMCAO. β-actin was used as an internal control. d SOD activities were decreased in vehicle group but increased in ZLN005-treated group. Data are expressed as the mean ± SD of individual group of rats (n = 4). *p < 0.05 versus vehicle group, ### p < 0.001 versus sham group
ZLN005 Protected PC12 Cells Against OGD-Induced Neuronal Injury
To determine the biologically safe concentration of ZLN005, PC12 cells were exposed to ZLN005 with increasing concentrations from 1 to 5 μM for 48 h. MTT assay revealed that ZLN005 has no cytotoxicity in PC12 cells (Fig. 4a). Furthermore, in order to investigate the neuroprotective effect of ZLN005 in vitro, PC12 cells were pretreated with vehicle or ZLN005 (1, 2, or 5 μM) for 24 h followed by exposure to OGD injury for another 2 h. MTT assay (p < 0.05 for 1 μM group, p < 0.001 for 2 μM group, and p < 0.01 for 5 μM group vs. OGD group, Fig. 4b) and LDH assay (p < 0.05 for 1 μM group, p < 0.01 for 2 μM group, and p < 0.01 for 5 μM group vs OGD group, Fig. 4c) results showed that ZLN005 significantly prevented OGD-induced neuronal injury in PC12 cells.
ZLN005 protects PC12 cells against OGD-induced neuronal death. a MTT assay showed that ZLN005 (1–5 μM) had no toxic in PC12 cells after 48-h incubation. Values were obtained from three independent experiments and are expressed as mean ± SD (% of control). b Protective potential of ZLN005 (1–5 μM) on cell viability in PC12 cells exposed to 2-h OGD/R. c The measurement of LDH released into culture medium after 2-h OGD indicated the protection of ZLN005 (1–5 μM) against OGD-induced neuronal injury. *p < 0.05, **p < 0.01, ***p < 0.001 versus OGD group, ### p < 0.001 versus control group
ZLN005 Activated PGC-1α and Cytochrome c in PC12 Cells Under OGD Condition
To study whether ZLN005 activates PGC-1α pathway in vitro, PC12 cells were treated with ZLN005 (2 µM) for different time points as indicated in Fig. 5a. PCR results showed that ZLN005 enhanced the mRNA expression of PGC-1α (p < 0.01 for 12 h and p < 0.05 for 24 h vs. 0 h, Fig. 5a) and cytochrome c (p < 0.05 vs. 0 h, Fig. 5b) in PC12 cells with a time-dependent manner. Furthermore, in order to investigate the effect of ZLN005 on PGC-1α pathway under OGD/R injury, PC12 cells were pretreated with varying concentrations of ZLN005 (1, 2, or 5 µM) followed by exposed to OGD condition for 2 h. Then the cells were incubated for further 22 h with or without ZLN005 (1, 2, or 5 µM) in normal condition. Then the mRNA expression for PGC-1α and cytochrome c was detected using PCR. In Fig. 5c, there was a significant upregulation of PGC-1α gene in OGD condition when compared with control (p < 0.05 vs. control). However, ZLN005 (2, 5 µM) showed a significant increase in PGC-1α mRNA expression (p < 0.01 for 2 μM group and p < 0.05 for 5 μM group vs. OGD group, Fig. 5c) and protein level (p < 0.01 for 2 μM group and p < 0.01 for 5 μM group vs. OGD group, Fig. 5e) when compared with OGD group. Furthermore, there was a remarkable increase in mRNA expression of cytochrome c in ZLN005-treated cells when compared to OGD group (p < 0.05 for 2 μM group vs. OGD group, Fig. 5d). The results showed that the beneficial effect of ZLN005 against OGD-induced neuronal injury may be mediated by PGC-1α activation.
ZLN005 activates PGC-1α pathway in well-differentiated PC12 cells. a, b PC12 cells were incubated with ZLN005 (2 μM) for different time points. The mRNA expression of PGC-1α and its related gene, cytochrome c, was detected by PCR. c–e PC12 cell were incubated with ZLN005 (1, 2, 5 µM) for 24 h and then subjected to OGD condition for 2 h, followed by treated with ZLN005 (1, 2, 5 µM) for further 22 h. PCR analysis showed an increase in PGC-1α (c) and cytochrome c (d) gene expression in ZLN005-treated groups, with the highest being at 2 µM in both experiments. GAPDH was used as an internal control. Western blot result showed that ZLN005 upregulated PGC-1α protein expression in PC12 cells after exposure to OGD/R injury (e). Data are expressed as mean ± SD. *p < 0.05, **p < 0.01 versus OGD group, # p < 0.05, ## p < 0.01 versus control group (CN or 0 h)
ZLN005 Upregulated the Expression of the Antioxidant Genes in PC12 Cells Under OGD Condition
Oxidative stress caused by reactive oxygen species (ROS) generated during cerebral ischemia and reperfusion (I/R) easily leads to neuronal cell death and consequent brain damage (Li et al. 2015). However, antioxidant strategies for ischemic stroke have achieved encouraging results in extensive studies (Gao et al. 2015; Liu et al. 2016). In this study, we evaluated the antioxidant potentials of ZLN005 on PC12 cells injured by 2-h OGD. There was a significant increase in the mRNA expression of SOD1 (p < 0.01 for 2 μM group vs. OGD group, Fig. 6a) and HO-1 mRNA (p < 0.05 for 2 μM group vs. OGD group, Fig. 6b) in ZLN005-treated cells when compared with OGD group.
ZLN005 upregulates the gene expression of antioxidant genes in PC12 cells under OGD condition. PC12 cells were treated with or without ZLN005 (1, 2, 5 µM) under OGD condition. There was an increase in SOD1 (a) and HO-1 (b) mRNA expression. GAPDH was used as an internal control. Data are expressed as mean ± SD. *p < 0.05, **p < 0.01 versus OGD group
Discussion
Stroke is a major cause of severe disability and mortality around the world (Wang et al. 2014). At present, for most patients there are few effective treatments currently available for ischemic stroke (Yu et al. 2014). Therefore, we assessed the neuroprotective effect of ZLN005 after ischemic stroke in vivo and in vitro. The experiment of tMCAO in rats is a well-established animal model in the research of clinical ischemic stroke (Chen et al. 2014). In the present study, we demonstrated that treatment with ZLN005 significantly reduced brain infarction volume and improved neurological deficit at 24 h after tMCAO onset, indicating that compound ZLN005 ameliorated ischemic stroke-related brain damage and disability. Well-differentiated PC12 cells, a rat pheochromocytoma cell line, have been generally applied as an in vitro model in investigating neuronal survival and developing potential neuroprotection compounds (Wu et al. 2007). Thus, the protective effect of ZLN005 in vitro was further assessed in PC12 cells exposed to oxygen–glucose–deprivation/reoxygenation (OGD/R) injury. We found that ZLN005 improved OGD/R-induced PC12 cell viability loss. These results indicated that ZLN005 exhibited a potent neuroprotective effect in vivo and in vitro.
PGC-1α serves as a master regulator of energy metabolism and governs a series of gene transcription involving cytochrome c, COX5B, and alternative oxidase (AOX) (Zhang et al. 2013). Prior researches have generally confirmed that ischemia injury increases the expression of PGC-1α and suppression of PGC-1α exacerbates brain damage, indicating the neuroprotective role of PGC-1α against cerebral ischemia (Li et al. 2016a; Ma et al. 2016). ZLN005 has been implicated as a PGC-1α activator in myotubes and skeletal muscle (Zhang et al. 2013). Indeed, we found that post-ischemia administration of ZLN005 increased the expression of PGC-1α and its related target genes. In addition, we also observed that ZLN005 upregulated PGC-1α expression after exposure to OGD injury in PC12 cells. Taken together, upregulation of PGC-1α may be responsible for the neuroprotective properties of ZLN005.
PGC-1α plays a central role in governing the transcriptional regulatory network for mitochondrial biogenesis and respiratory function. Activation of PGC-1α results in improvement of neuronal mitochondrial dysfunction (Chen et al. 2011). It has been well known that mitochondrial metabolism is the major source of ROS production. After cerebral ischemia, oxidative stress is induced with the disturbed balance between ROS generation and clearance and causes cell injury. In ischemic neurons, PGC-1α is increased upon oxidative stress, which further triggering upregulation of genes that involves ROS-detoxifying system, including SOD1, SOD2, ANT1, and UCP2. Meanwhile, PGC-1α activation also stimulates mitochondrial biogenesis and respiration, which may protect neurons against ischemic injury (Chen et al. 2010; Yin et al. 2008). A recent study has reported that PGC-1α exerts a protective role through Sirt3 signaling pathway in spinal cord neurons against ischemic injury (Liu et al. 2017). While the molecular mechanisms underlying neuroprotective effect of PGC-1α has remained largely unclear, we further explored the pathways possibly involved in the neuroprotective properties of ZLN005.
SOD, an important antioxidant enzyme, specifically catalyzes superoxide to hydrogen peroxide resulting in the clearance of free radicals. Among three isoforms of SOD expressed in mammals, SOD1, also known as Cu–Zn superoxide dismutase, acts as an indispensable role in regulating ROS activities and improving neuronal cell survival after acute ischemia (Qiao et al. 2012). Exposure to ischemia induces defect of SOD activity, and thus stimulating SOD1 expression and increasing SOD activity would be expected to diminish oxidative stress and protect brain from ischemic damage. Furthermore, PGC-1α has been reported to regulate the antioxidant genes expression, including SOD1, and ameliorate oxidative stress-induced neuronal injury (Mäkelä et al. 2016; Singh et al. 2016; St-Pierre et al. 2006; Xiao and Goswami 2015). Thus, we propose that neuroprotective effect of ZLN005 may be strongly associated with PGC-1α-mediated upregulation of SOD1 expression and restoration of SOD activity. Our results confirmed that ischemic injury induced a marked reduction of SOD activity, while treatment with ZLN005 enhanced SOD activity and SOD1 gene expression. In addition, we found that ZLN005 treatment significantly upregulated SOD1 expression in PC12 cell after OGD injury. These results suggested that the beneficial effect of ZLN005 against ischemia-induced neuronal injury might be related to the restoration of antioxidant system. Further studies are needed to clarify the detailed molecular mechanisms responsible for the relationship between PGC-1α activation and SOD restoration after ZLN005 treatment in ischemic stroke model.
HO-1 is a stress-inducible enzyme and exerts potent antioxidant activity in ischemic stroke (Wang et al. 2017a; Won et al. 2013). Our results were in agreement with the previous reports that HO-1 mRNA expression was induced in acute post-ischemia period (Zhang et al. 2014). Due to the individual variability in animal samples, overexpression of HO-1 protein after acute ischemia was not observed in our study. However, after treatment with ZLN005, the HO-1 mRNA and protein levels were significantly upregulated in rats with tMCAO. Similarly, we demonstrated that ZLN005 increased HO-1 gene expression after exposure to OGD-induced injury in PC12 cells. These results indicated that HO-1 activation may be partly responsible for the neuroprotective effect of ZLN005.
Conclusion
In summary, ZLN005, a known PGC-1α activator, showed a neuroprotective role in ischemic rat model and PC12 cells model with OGD/R. For the first time, the beneficial effects of ZLN005 in cerebral ischemic stroke were demonstrated. Besides, ZLN005 was shown to activate PGC-1α and its neuroprotective effects may be possibly through induction of cellular antioxidant systems. Therefore, our results may provide the therapeutic potential of ZLN005 for the treatment of ischemic stroke.
References
Bian M et al (2016) Celastrol protects mouse retinas from bright light-induced degeneration through inhibition of oxidative stress and inflammation. J Neuroinf 13:50. https://doi.org/10.1186/s12974-016-0516-8
Chang R et al (2016) Protective effects of aloin on oxygen and glucose deprivation-induced injury in PC12 cells. Brain Res Bull 121:75–83. https://doi.org/10.1016/j.brainresbull.2016.01.001
Chang S et al (2017) The natural product 4,10-aromadendranediol induces neuritogenesis in neuronal cells in vitro through activation of the ERK pathway. Acta Pharmacol Sin 38:29–40. https://doi.org/10.1038/aps.2016.115
Chen SD et al (2010) Activation of calcium/calmodulin-dependent protein kinase IV and peroxisome proliferator-activated receptor γ coactivator-1α signaling pathway protects against neuronal injury and promotes mitochondrial biogenesis in the hippocampal CA1 subfield after transient global ischemia. J Neurosci Res 88:3144–3154. https://doi.org/10.1002/jnr.22469
Chen SD, Yang DI, Lin TK, Shaw FZ, Liou CW, Chuang YC (2011) Roles of oxidative stress, apoptosis, PGC-1α and mitochondrial biogenesis in cerebral ischemia. Int J Mol Sci 12:7199–7215. https://doi.org/10.3390/ijms12107199
Chen T et al (2014) Nafamostat mesilate attenuates neuronal damage in a rat model of transient focal cerebral ischemia through thrombin inhibition. Sci Rep 4:5531. https://doi.org/10.1038/srep05531
di Penta A et al (2013) Oxidative stress and proinflammatory cytokines contribute to demyelination and axonal damage in a cerebellar culture model of neuroinflammation. PLoS ONE 8:e54722. https://doi.org/10.1371/journal.pone.0054722
Ding Y, Chen M, Wang M, Li Y, Wen A (2015) Posttreatment with 11-Keto-β-Boswellic acid ameliorates cerebral ischemia-reperfusion injury: nrf2/HO-1 pathway as a potential mechanism. Mol Neurobiol 52:1430–1439. https://doi.org/10.1007/s12035-014-8929-9
Gao Y et al (2015) Totarol prevents neuronal injury in vitro and ameliorates brain ischemic stroke: potential roles of Akt activation and HO-1 induction. Toxicol Appl Pharmacol 289:142–154. https://doi.org/10.1016/j.taap.2015.10.001
Garcia G et al (2017) Bioaccessible (poly)phenol metabolites from raspberry protect neural cells from oxidative stress and attenuate microglia activation. Food Chem 215:274–283. https://doi.org/10.1016/j.foodchem.2016.07.128
García-Quintans N et al (2016) Oxidative stress induces loss of pericyte coverage and vascular instability in PGC-1α-deficient mice. Angiogenesis 19:217–228. https://doi.org/10.1007/s10456-016-9502-0
Gu WW et al (2016) 2-(3′,5′-Dimethoxybenzylidene) cyclopentanone, a novel synthetic small-molecule compound, provides neuroprotective effects against ischemic stroke. Neuroscience 316:26–40. https://doi.org/10.1016/j.neuroscience.2015.11.052
Ho YH, Lin YT, Wu CW, Chao YM, Chang AY, Chan JY (2015) Peripheral inflammation increases seizure susceptibility via the induction of neuroinflammation and oxidative stress in the hippocampus. J Biomed Sci 22:46. https://doi.org/10.1186/s12929-015-0157-8
Li L et al (2015) Chinese herbal medicine formula tao hong si wu decoction protects against cerebral ischemia-reperfusion injury via PI3 K/Akt and the Nrf2 signaling pathway. J Nat Med 69:76–85. https://doi.org/10.1007/s11418-014-0865-5
Li L et al (2016a) Sestrin2 silencing exacerbates cerebral ischemia/reperfusion injury by decreasing mitochondrial biogenesis through the AMPK/PGC-1α pathway in rats. Sci Rep 6:30272. https://doi.org/10.1038/srep30272
Li W et al (2016b) ZLN005 protects cardiomyocytes against high glucose-induced cytotoxicity by promoting SIRT1 expression and autophagy. Exp Cell Res 345:25–36. https://doi.org/10.1016/j.yexcr.2016.05.012
Liu P et al (2015) MicroRNA-424 protects against focal cerebral ischemia and reperfusion injury in mice by suppressing oxidative stress. Stroke 46:513–519. https://doi.org/10.1161/STROKEAHA.114.007482
Liu X, Zhu X, Chen M, Ge Q, Shen Y, Pan S (2016) Resveratrol protects PC12 cells against OGD/R-induced apoptosis via the mitochondrial-mediated signaling pathway. Acta Biochim Biophys Sin (Shanghai) 48:342–353. https://doi.org/10.1093/abbs/gmw011
Liu SG, Wang YM, Zhang YJ, He XJ, Ma T, Song W, Zhang YM (2017) ZL006 protects spinal cord neurons against ischemia-induced oxidative stress through AMPK-PGC-1α-Sirt3 pathway. Neurochem Int 108:230–237. https://doi.org/10.1016/j.neuint.2017.04.005
Longa EZ, Weinstein PR, Carlson S, Cummins R (1989) Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 20:84–91
Ma X, Xie Y, Chen Y, Han B, Li J, Qi S (2016) Post-ischemia mdivi-1 treatment protects against ischemia/reperfusion-induced brain injury in a rat model. Neurosci Lett 632:23–32. https://doi.org/10.1016/j.neulet.2016.08.026
Mäkelä J, Tselykh TV, Kukkonen JP, Eriksson O, Korhonen LT, Lindholm D (2016) Peroxisome proliferator-activated receptor-γ (PPARγ) agonist is neuroprotective and stimulates PGC-1α expression and CREB phosphorylation in human dopaminergic neurons. Neuropharmacology 102:266–275. https://doi.org/10.1016/j.neuropharm.2015.11.020
Mossakowski AA et al (2015) Tracking CNS and systemic sources of oxidative stress during the course of chronic neuroinflammation. Acta Neuropathol 130:799–814. https://doi.org/10.1007/s00401-015-1497-x
Mudò G et al (2012) Transgenic expression and activation of PGC-1α protect dopaminergic neurons in the MPTP mouse model of Parkinson’s disease. Cell Mol Life Sci 69:1153–1165. https://doi.org/10.1007/s00018-011-0850-z
O’Hare Doig RL, Bartlett CA, Maghzal GJ, Lam M, Archer M, Stocker R, Fitzgerald M (2014) Reactive species and oxidative stress in optic nerve vulnerable to secondary degeneration. Exp Neurol 261:136–146. https://doi.org/10.1016/j.expneurol.2014.06.007
Pang T et al (2016) A novel GSK-3β inhibitor YQ138 prevents neuronal injury induced by glutamate and brain ischemia through activation of the Nrf2 signaling pathway. Acta Pharmacol Sin 37:741–752. https://doi.org/10.1038/aps.2016.3
Park JH, Park YS, Lee JB, Park KH, Paik MK, Jeong M, Koh HC (2016) Meloxicam inhibits fipronil-induced apoptosis via modulation of the oxidative stress and inflammatory response in SH-SY5Y cells. J Appl Toxicol 36:10–23. https://doi.org/10.1002/jat.3136
Peng H et al (2015) Lack of PGC-1α exacerbates high glucose-induced apoptosis in human umbilical vein endothelial cells through activation of VADC1. Int J Clin Exp Pathol 8:4639–4650
Qi D et al (2014) HO-1 attenuates hippocampal neurons injury via the activation of BDNF-TrkB-PI3 K/Akt signaling pathway in stroke. Brain Res 1577:69–76. https://doi.org/10.1016/j.brainres.2014.06.031
Qiao H et al (2012) Protective effect of luteolin in experimental ischemic stroke: upregulated SOD1, CAT, Bcl-2 and claudin-5, down-regulated MDA and Bax expression. Neurochem Res 37:2014–2024. https://doi.org/10.1007/s11064-012-0822-1
Ritzel RM et al (2016) Early retinal inflammatory biomarkers in the middle cerebral artery occlusion model of ischemic stroke. Mol Vis 22:575–588
Sharma DR, Sunkaria A, Wani WY, Sharma RK, Kandimalla RJ, Bal A, Gill KD (2013) Aluminium induced oxidative stress results in decreased mitochondrial biogenesis via modulation of PGC-1α expression. Toxicol Appl Pharmacol 273:365–380. https://doi.org/10.1016/j.taap.2013.09.012
Shirley R, Ord EN, Work LM (2014) Oxidative stress and the use of antioxidants in stroke. Antioxidants (Basel) 3:472–501. https://doi.org/10.3390/antiox3030472
Shulyakova N, Sidorova-Darmos E, Fong J, Zhang G, Mills LR, Eubanks JH (2014) Over-expression of the Sirt3 sirtuin Protects neuronally differentiated PC12 Cells from degeneration induced by oxidative stress and trophic withdrawal. Brain Res 1587:40–53. https://doi.org/10.1016/j.brainres.2014.08.066
Singh SP, Schragenheim J, Cao J, Falck JR, Abraham NG, Bellner L (2016) PGC-1 alpha regulates HO-1 expression, mitochondrial dynamics and biogenesis: role of epoxyeicosatrienoic acid. Prostaglandins Other Lipid Mediat 125:8–18. https://doi.org/10.1016/j.prostaglandins.2016.07.004
St-Pierre J et al (2006) Suppression of reactive oxygen species and neurodegeneration by the PGC-1 transcriptional coactivators. Cell 127:397–408
Szalardy L, Molnar M, Torok R, Zadori D, Kovacs GG, Vecsei L, Klivenyi P (2016) Lack of age-related clinical progression in PGC-1α-deficient mice – implications for mitochondrial encephalopathies. Behav Brain Res 313:272–281. https://doi.org/10.1016/j.bbr.2016.07.021
Wang LQ et al (2014) Timing and dose regimens of marrow mesenchymal stem cell transplantation affect the outcomes and neuroinflammatory response after ischemic stroke. CNS Neurosci Ther 20:317–326. https://doi.org/10.1111/cns.12216
Wang Y et al (2017a) A dual AMPK/Nrf2 activator reduces brain inflammation after stroke by enhancing microglia M2 polarization. Antioxid Redox Signal. https://doi.org/10.1089/ars.2017.7003
Wang Y et al (2017b) Balasubramide derivative 3C modulates microglia activation via CaMKKβ-dependent AMPK/PGC-1α pathway in neuroinflammatory conditions. Brain Behav Immun. https://doi.org/10.1016/j.bbi.2017.08.006
Won YW, Lee M, Kim HA, Bull DA, Kim SW (2013) Hypoxia-inducible plasmid expressing both miSHP-1 and HO-1 for the treatment of ischemic disease. J Control Release 165:22–28. https://doi.org/10.1016/j.jconrel.2012.10.014
Wu Y, Shang Y, Sun SG, Liu RG, Yang WQ (2007) Protective effect of erythropoietin against 1-methyl-4-phenylpyridinium-induced neurodegenaration in PC12 cells. Neurosci Bull 23:156–164
Wu KL, Wu CW, Chao YM, Hung CY, Chan JY (2016) Impaired Nrf2 regulation of mitochondrial biogenesis in rostral ventrolateral medulla on hypertension induced by systemic inflammation. Free Radic Biol Med 97:58–74. https://doi.org/10.1016/j.freeradbiomed.2016.05.012
Xiao W, Goswami PC (2015) Down-regulation of peroxisome proliferator activated receptor gamma coactivator 1α induces oxidative stress and toxicity of 1-(4-Chlorophenyl)-benzo-2,5-quinone in HaCaT human keratinocytes. Toxicol In Vitro 29:1332–1338. https://doi.org/10.1016/j.tiv.2015.05.009
Xu Y et al (2015) Telmisartan prevention of LPS-induced microglia activation involves M2 microglia polarization via CaMKKβ-dependent AMPK activation. Brain Behav Immun 50:298–313. https://doi.org/10.1016/j.bbi.2015.07.015
Xue F et al (2016) Nrf2/antioxidant defense pathway is involved in the neuroprotective effects of Sirt1 against focal cerebral ischemia in rats after hyperbaric oxygen preconditioning. Behav Brain Res 309:1–8. https://doi.org/10.1016/j.bbr.2016.04.045
Yang F et al (2014) NLRP3 deficiency ameliorates neurovascular damage in experimental ischemic stroke. J Cereb Blood Flow Metab 34:660–667. https://doi.org/10.1038/jcbfm.2013.242
Yin W, Signore AP, Iwai M, Cao G, Gao Y, Chen J (2008) Rapidly increased neuronal mitochondrial biogenesis after hypoxic-ischemic brain injury. Stroke 39:3057–3063. https://doi.org/10.1161/STROKEAHA.108.520114
Yu S, Cheng Q, Li L, Liu M, Yang Y, Ding F (2014) 2-(4-Methoxyphenyl)ethyl-2-acetamido-2-deoxy-beta-d-pyranoside confers neuroprotection in cell and animal models of ischemic stroke through calpain1/PKA/CREB-mediated induction of neuronal glucose transporter 3. Toxicol Appl Pharmacol 277:259–269. https://doi.org/10.1016/j.taap.2014.03.025
Zhang LN et al (2013) Novel small-molecule PGC-1α transcriptional regulator with beneficial effects on diabetic db/db mice. Diabetes 62:1297–1307. https://doi.org/10.2337/db12-0703
Zhang J et al (2014) Bicyclol upregulates transcription factor Nrf2, HO-1 expression and protects rat brains against focal ischemia. Brain Res Bull 100:38–43. https://doi.org/10.1016/j.brainresbull.2013.11.001
Acknowledgements
This study was supported by the National Natural Science Foundation of China (21402241), the Natural Science Foundation of Jiangsu Province (BK20160032), the Six Talent Peaks Project of Jiangsu Province (T.P.), and the Program for Jiangsu Province “Shuang Chuang” Team.
Author information
Authors and Affiliations
Contributions
All authors listed contributed immensely to this study. YX and JAK performed the experiments and wrote the paper. WR, YW, SZ, and XS performed the animal experiments and analyzed the data. TP, JL, and LZ, as experts in molecular pharmacology, provided technical supports and designed the research.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Ethical Approval
All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Rights and permissions
About this article
Cite this article
Xu, Y., Kabba, J.A., Ruan, W. et al. The PGC-1α Activator ZLN005 Ameliorates Ischemia-Induced Neuronal Injury In Vitro and In Vivo. Cell Mol Neurobiol 38, 929–939 (2018). https://doi.org/10.1007/s10571-017-0567-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10571-017-0567-0