Abstract
We investigate the antinociceptive effect of intrathecal and intraperitoneal tempol administration in a rat model of chronic constriction injury (CCI)-induced neuropathic pain and explore the underlying antinociceptive mechanisms of tempol. Rats were randomly assigned to four groups (n = 8 per group): sham group, CCI group, Tem1 group (intrathecal injection of tempol), and Tem2 group (intraperitoneal injection of tempol). Neuropathic pain was induced by CCI of the sciatic nerve. Tempol was intrathecally or intraperitoneally administered daily for 7 days beginning on postoperative day one. The mechanical withdrawal threshold and thermal withdrawal latency were tested on preoperative day 3 and postoperative days 1, 3, 5, 7, 10, 14, and 21. Structural changes were examined by hematoxylin and eosin staining, toluidine blue staining, and electron microscopy. Malondialdehyde (MDA) and superoxide dismutase (SOD) levels were determined using the thiobarbituric acid and nitroblue tetrazolium methods, respectively. Nerve growth factor (NGF) expression levels were determined by immunohistochemistry and Western blot. Intrathecal, but not intraperitoneal, injection of tempol produced a persistent antinociceptive effect. Intraperitoneal injection of tempol did not result in high enough concentration of tempol in the cerebrospinal fluid. Intrathecal, but not intraperitoneal, injection of tempol inhibited CCI-induced structural damage in the spinal cord reduced MDA levels, and increased SOD activities in the spinal cord. Furthermore, intrathecal, but not intraperitoneal, injection of tempol further downregulated the expression of NGF in the spinal cord following CCI, and this effect was blocked by p38MAPK inhibitor. Intrathecal injection of tempol produces antinociceptive effects and reduces CCI-induced structural damage in the spinal cord by increasing SOD activities and downregulating the expression of NGF via the p38MAPK pathway. Intraperitoneal administration of tempol does not exhibit antinociceptive effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuropathic pain is a type of abnormal pain that is caused by central or peripheral nerve injury. The most common clinical symptoms of neuropathic pain include allodynia, hyperalgesia, spontaneous pain, and paraesthesia (Costigan et al. 2009; Zhao et al. 2015). Epidemiological studies have shown that neuropathic pain occurs in approximately 4–6 % of the general population, 22 % of patients with chronic pain, and 74 % of patients with moderate or severe pain (Bouhassira et al. 2008; Ohayon and Stingl 2012; Torrance et al. 2006). Neuropathic pain is one of the most intractable types of chronic pain and it causes physiological, psychological, and social problems that impair the quality of life of affected patients (Attal et al. 2011; Smith and Torrance 2012). It has been reported that that patients with neuropathic pain have a lower quality of life than those with cancer, diabetes, chronic heart failure, or stroke (Doth et al. 2010; Dworkin et al. 2010; Smith et al. 2007). Although diverse pharmacological agents, such as serotonin reuptake inhibitors and calcium channel blockers, are available for the treatment of neuropathic pain, many patients have neuropathic pain that is refractory to these treatments (Dworkin et al. 2010). Therefore, identification of novel pharmacological agents is needed for the treatment of neuropathic pain.
The mechanisms underlying neuropathic pain are complex and not clearly understood. One mechanism with reported involvement in the pathogenesis of neuropathic pain involves the promotion of neuropathic pain by reactive oxygen species (ROS) (Janes et al. 2012; Khalil et al. 1999). In a mouse model of capsaicin-induced hyperalgesia, ROS was mainly synthesized by mitochondria in the neurons of the dorsal horn of the spinal cord (Schwartz et al. 2008). Spinal cord injury induces the release of ROS from neurons and subsequently triggers activation of postsynaptic neurons and glial cells, thus contributing to neuropathic pain (Gwak et al. 2012). Gao et al. reported that phenyl N-tert-butylnitrone (PBN), a ROS scavenger, reduced hyperalgesia. The reduction of hyperalgesia was accompanied by inhibition of N-methyl-d-aspartate (NMDA) receptors in the dorsal horn, suggesting that ROS contributes to neuropathic pain via activation of NMDA receptors, a key step in central sensitization (Gao et al. 2007). Additionally, Gwak et al. found that ROS played an important role in neuropathic pain via activation of CaMKII in remote segments following spinal cord injury (SCI) in rats (Gwak et al. 2013). Another study found evidence that inhibition of ROS-induced p38MAPK and ERK activation in microglia contributed to the analgesic effect of acupuncture (Choi et al. 2012). Furthermore, the antioxidant activity of the stress-responsive antioxidant protein Sestrin 2 has been reported to control ROS-dependent neuropathic pain signaling following peripheral nerve injury (Kallenborn-Gerhardt et al. 2013a). Therefore, inhibition of ROS is a promising potential therapeutic strategy for the treatment of neuropathic pain.
Tempol (4-hydroxy-2,2,6,6-tetramethylpiperidine-1-oxyl) is a prototype nitroxide antioxidant that is characterized by a low molecular weight and good membrane permeability (Mitchell et al. 1991). Tempol has diverse biological functions, including the removal of ROS and inhibition of lipid peroxidation, that contribute to the inhibition of oxidative injury in cerebrovascular endothelial and neuronal cells, alleviation of inflammation, and reduction of brain edema (Xiong et al. 2009). We previously demonstrated that tempol promotes the recovery of neuronal function in ischemic and hypoxic brain tissues (Cao et al. 2014). However, it remained unclear whether tempol could have an antinociceptive effect in a rat model of SCI.
We have previously investigated the antinociceptive effects of HBO treatment at various stages following CCI in rats, and found that early HBO treatment beginning on postoperative day 1 produced persistent antinociceptive effects (Zhao et al. 2014a, 2015). In addition, several studies have shown that early treatment promotes recovery of pathological pain (Beaudry et al. 2007; Liu et al. 2014; Matsuo et al. 2014). In this study, we investigated the early antinociceptive effects of intrathecal and intraperitoneal tempol administration in a chronic constriction injury (CCI) model of neuropathic pain in rats. To test the early antinociceptive effect of tempol, tempol administration was initiated 1 day after CCI. We studied the antinociceptive mechanisms of tempol and investigated whether tempol has different antinociceptive effects that depend on the administrative route.
Materials and Methods
Animals
The Animal Ethics Committee of Guangzhou Women and Children’s Medical Center (Guangzhou, China) approved all experimental protocols. All procedures were conducted in accordance with the National Institutes of Health Guidelines for the Care and Use of Laboratory Animals and the Animal Welfare Act. Thirty-two adult Sprague–Dawley rats (male, weighing 250–280 g, 8–10 weeks old) were used in this study. The animals were obtained from the Animal Care Center of Guangzhou Women and Children’s Medical Center. Animals were housed individually in plastic boxes at room temperature (23–25 °C) with a 12 h light/dark cycle. Animals were fed standard rat chow and water ad libitum. The animals were randomly assigned to four groups (n = 8 for each group): sham group, CCI group, Tem1 group (intrathecal injection of tempol for 7 days beginning 1 day after CCI), and Tem2 group (intraperitoneal injection of tempol for 7 days beginning 1 day after CCI). To test whether tempol produced antinociceptive effect as an oxidant, the animals were randomly assigned to three groups (n = 8 for each group): CCI group, Tem1 group, and positive control group (PC group, Animals in the PC group received intraperitoneal administration of the SOD (4000 U/kg/day, Sigma-Aldrich, St. Louis, MO, US)for 7 days beginning 1 day after CCI).
Induction of Neuropathic Pain
The CCI model of the sciatic nerve was used to create neuropathic pain as previously described (Bennett and Xie 1988). Briefly, rats (n = 8 per group) were anesthetized with an intraperitoneal injection of sodium pentobarbital (40 mg/kg). The left biceps femoris of each rat was bluntly dissected to expose the sciatic nerve. For the CCI, Tem1, and tem2 groups, four 4–0 chromic catgut sutures were loosely tied around the trunk of the sciatic nerve at 1 mm intervals. An appropriate amount of constriction was applied by tightening the sutures to cause a mild shaking of the left leg without inducing a blockade of the nerve or blocking the blood supply. The wound was then sutured in layers. For the sham group, an identical dissection was performed, but the sciatic nerve was not ligated.
Intrathecal Catheter Insertion
An intrathecal catheter was inserted as previously described (Sakura et al. 2005). Briefly, all rats were anesthetized by an intraperitoneal injection of sodium pentobarbital (40 mg/kg). Rats were placed in a prone position and a longitudinal skin incision (2 cm long) was made at the L4–L5 intervertebral space in the midline of the back. After the fascia was cut open, the L4–L5 interspinous space was exposed by blunt dissection of the muscles around the spinous process. The ligamentumflavum was exposed after removal of part of the spinous process of the L4 and L5 vertebra. A heat-connected polyethylene catheter (PE-10, Ningbo Anlai Company, China) was inserted into the subarachnoid space by passing through the ligamentumflavum and the dura at the L4–L5 intervertebral space. The insertion of the catheter into the subarachnoid space was verified by the appearance of side tail swing or hind leg twitch. The catheter was advanced by 2 cm in the caudal direction. The success of catheter insertion was verified by cautious aspiration of cerebrospinal fluid (CSF). The catheter was then flushed with normal saline (10 μl) to prevent thrombus formation. The distal end of the catheter was closed by heating to prevent CSF leakage. The catheter was then fixed subcutaneously. Next, the incision was sutured and the rat was given an intramuscular injection of penicillin to prevent infection (Huabei Pharmaceutical Co., Ltd., China). One day after catheter insertion, lidocaine (1 %, 20 μl) was injected through the catheter. Rats showing obvious hind limb paralysis (lidocaine-positive) in both hind limbs within 30 s after lidocaine injection were included in the study. Rats that exhibited obvious limb paralysis or movement disorders after catheter insertion and lidocaine-negative rats or rats showing unilateral limb paralysis were excluded from the study. A total of 10 rats were excluded, including 2 rats in the control group, 2 rats in the CCI group, 3 rats in the Temp1 group, and 2 rats in the Temp2 groups.
Drug Administration
Rats received both intrathecal and intraperitoneal injections of saline solution (Baxter, Deerfield, IL, USA) or tempol (a gift from the Department of Cell Biology, School of Medicine, New York University, USA) daily for 7 days, starting 1 day after CCI. For the sham and CCI groups, rats received intrathecal injections of 20 μl saline and intraperitoneal injections of 20 μl saline. For the Tem1 group, rats received intrathecal injections of 20 μl tempol (30 μg) and intraperitoneal injections of 20 μl saline. For the Tem2 group, rats received intrathecal injections of 20 μl saline and intraperitoneal injections of 20 μl tempol (30 μg) (Cao et al. 2014; Liu et al. 2013).
To test whether p38MAPK mediates tempol-induced downregulation of NGF, rats in the CCI, Tem1, and Tem2 groups received intrathecal injection of SB203580 (2 μg), a specific inhibitor of p38MAPK, daily for 7 days, starting 1 day after CCI. The expression of NGF was tested on the 21st day using Western blot.
Neurobehavioral Tests
Mechanical withdrawal threshold (MWT) and thermal withdrawal latency (TWL) tests were performed on preoperative day 3 and postoperative days 1, 3, 5, 7, 10, 14, and 21, as previously described (Zhao et al. 2013). The MWT test was carried out to assess the response of the paw to a mechanical stimulus. The rats were placed in a Plexiglas chamber, and the MWT test was performed by stimulating the plantar surface of the left hind paw using Von Frey filaments (Stoelting Company, Wood Dale, IL, USA). Each Von Frey filament was held for approximately 3–5 s. Each trial started with the application of a 0.6-g Von Frey force following the up-and-down procedure. A positive response was defined as a quick withdrawal of the hind paw upon stimulation. When a positive response occurred, a filament with a lower force was applied. If a negative response occurred, a filament with a greater force was applied. This protocol was continued until the least force necessary to cause withdrawal was identified. The MWT test was performed ten times, and the paw withdrawal threshold was defined as the Von Frey force that caused withdrawal 50 % of the time.
To examine TWL, a BME-410C full-automatic plantar analgesia tester (Youer Equipment Scientific Co., Ltd., Shanghai, China) was used to measure the sensitivity of the paw to thermal stimuli. The thermal withdrawal latency test was performed by placing the rats on the surface of a 3-mm-thick glass plate that was covered with the same Plexiglas chamber that was used for the MWT tests. The radiant heat source was positioned at a fixed distance below the glass plate. Heat stimuli were directed at the exposure site on the left hind paw. TWL was defined as the elapsed time (in seconds) between the delivery of the thermal stimulus and the withdrawal of the paw from the heat source. Each test session calculated the mean latency from the delivery of five thermal stimuli at 5-min intervals. A cut-off time of 30 s was set to avoid tissue damage.
Determination of Tempol Concentration in Cerebrospinal Fluid (CSF) and Whole Blood
Tempol concentrations were measured using electron paramagnetic resonance (EPR) spectrometry as previously reported (Hahn et al. 1992). Briefly, cerebrospinal fluid (0.1 ml) and whole blood samples were obtained at 20, 40, 60, 80, 100, and 120 min after intrathecal or intraperitoneal injection of tempol (30 μg). The sample was mixed with 0.2 ml of preservative-free heparin. Then, the samples were mixed with the oxidizing agent potassium ferricyanide and stored on ice for a short time. Samples were then placed vertically into the EPR cavity. EPR spectra were recorded on a Varian E4 X-band spectrophotometer. A standard curve was generated by determining the EPR signal of varying concentrations of an aqueous Tempol solution, and used for determining the tempol concentrations in the CSF and blood.
Tissue Preparation
After completion of the behavioral tests on postoperative day 21, the rats (n = 8 per group) were anesthetized by intraperitoneal injection of sodium pentobarbital (40 mg/kg). Four rats in each group were transcardially perfused with 200 ml of normal saline. The spinal cord between the L4–L5 segment and the cauda equina was removed and was used for the toluidine blue and hematoxylin and eosin (HE) staining, transmission electron microscopy (TEM), and immunohistochemistry. The other four rats in each group were used for the measurement of malondialdehyde (MDA) levels and superoxide dismutase (SOD) activities and Western blot.
Toluidine Blue and Hematoxylin and Eosin (HE) Staining
After removal, the spinal cord between the L4–L5 segment and cauda equina was fixed in 4 % paraformaldehyde for 4 h and embedded in paraffin. Transverse sections (4-µm thick) were obtained from paraffin-embedded tissue blocks. Sections were washed in xylene to remove the paraffin and rehydrated with serial dilutions of alcohol followed by a wash in phosphate buffered saline (PBS) solution. For HE staining, sections were stained with hematoxylin and eosin. For toluidine blue staining, sections were immersed in toluidine blue solution for 5 min. Slides were then rinsed well in water, dehydrated, cleared, and mounted. Histological images were recorded under a light microscope (Fluo View 1000; Olympus Co.; Tokyo, Japan).
Transmission Electron Microscopy (TEM)
For TEM examination, white matter (1 mm) from the dorsal horn of the spinal cord was removed and fixed with 2.5 % glutaraldehyde for 24 h. After three 10-min washes with 0.1 M PBS, tissues were postfixed in 1 % OsO4 for 1 h, dehydrated in a graded series of acetone (50, 70, 90, and 100 % for 10 min each), embedded in a 1:1 mixture of Epon812 and acetone for 2–3 h, and finally embedded in Epon812 for 2 h. Ultrathin sections were cut, stained with lead citrate and uranyl acetate, and viewed and imaged with a scanning electron microscope.
The ultrastructure damage score was determined as previously reported(Zhao et al. 2014b). Fifteen slices in each group were selected for examination of the cauda equine fibers. Fibers that had locally disintegrated myelin lamellae and intracellular edema were considered damaged. The total ultrastructure damage score was determined as follows: “1” normal, no disintegrated myelin lamellae and intracellular edema; “2” mild injury, <20 % damaged fibers per region; “3” moderate injury, <50 % damaged fibers per region; “4” severe injury, <80 % damaged fibers per region; and “5” ultra-severe injury, >80 % damaged fibers per region. Evaluation of all tissue sections was done by the same examiner, who was blinded to the experimental conditions.
Determination of Malondialdehyde (MDA) Levels and Superoxide Dismutase (SOD) Activities
MDA levels and SOD activities in the spinal cord and plasma were measured using the thiobarbituric acid and nitroblue tetrazolium methods, respectively, as previously reported (Zhao et al. 2014a). To determine MDA levels and SOD activities in the spinal cord and plasma, spinal cord specimens and plasma were homogenized in ice-cold lysis buffer. Samples were centrifuged at 600×g for 15 min at 4 °C and the supernatant was collected. MDA levels in the spinal cord and plasma were determined using Type 532 spectrometry (S0131, Beyotime Co. Ltd., Haimen, China). Blood SOD activity was evaluated using commercial kits (S0109, Beyotime Co. Ltd.) according to the manufacturer’s instructions. Standard curves were plotted according to the absorption values of the standard samples and were used to determine the MDA levels and SOD activities of the spinal cord and plasma samples.
Immunohistochemistry
Immunohistochemistry to detect the expression of NGF in the spinal cord was performed as previously described (Zhao et al. 2014b). Briefly, the spinal cord between the L4 and L5 segments was removed, fixed in 4 % paraformaldehyde for 24 h, dehydrated in 30 % sucrose in PBS at 4 °C for 24 h, and embedded in paraffin. Transverse spinal cord sections (5-µm thick) were obtained from paraffin-embedded tissue blocks. Endogenous peroxidase activity was blocked by 3 % H2O2 at room temperature for 10 min. Sections were incubated in 5 % normal goat serum for 20 min to block nonspecific protein binding sites. Sections were then incubated with primary antibodies against NGF (polyclonal rabbit anti-rat NGF, 1:100 dilution, Wuhan Boster Bio-Engineering Co., Wuhan, China) for 3 h at 37 °C. After the primary antibody was washed off, sections were incubated with goat anti-rabbit biotin-conjugated secondary antibodies (1:1000 dilution, Wuhan Boster Bio-Engineering Co.) for 30 min at 37 °C. Sections were then incubated with streptavidin horseradish peroxidase for 30 min at 37 °C. DAB (3, 3-diaminobenzidine) substrate was then applied to the sections followed by counterstaining with hematoxylin. The integral optical density (IOD) of NGF-positive cells in each spinal dorsal horn was examined by observers blind to the experimental conditions, using a confocal microscope (FluoView 1000; Olympus Co., Tokyo, Japan). The images were processed using an Image-Pro Plus image 6.0 analysis system. Ten sections that were not damaged, folded, or torn were selected from each group for the analysis.
Western Blot
Spinal cord tissues were homogenized in lysis buffer on ice. Proteins were resolved by SDS-PAGE and transferred onto polyvinylidene fluoride membranes by electroblotting. Membranes were incubated with primary antibodies against NGF (rabbit anti-rat NGF, dilution 1:200, Santa Cruz, Dallas, TX, USA) and p38 MAPK (rabbit anti-rat p38MAPK, dilution 1:1000, Santa Cruz, Dallas, TX, USA) at 4 °C overnight. β-actin was used as a loading control. Membranes were then incubated with horseradish peroxidase-linked goat anti-rabbit secondary antibodies (dilution 1:1000, Santa Cruz) at room temperature for 2 h. Bands were visualized using a chemiluminescence detection system.
Statistical Analysis
Analyses were performed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA). Numerical data are presented as the mean and standard deviation. One-way analysis of variance (ANOVA) was used to compare differences among groups, followed by the least significant difference test. p < 0.05 was considered statistically significant.
Results
Intrathecal Injection of Tempol Produces Persistent Antinociceptive Effects in CCI Rats
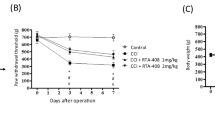
There were no significant differences in the preoperative MWT and TWL among the sham, CCI, Tem1, and Tem2 groups. Compared with the sham group, the MWT and TWL significantly decreased during postoperative days 1 through 21 in the CCI group (Fig. 1a and b), suggesting that CCI induced persistent mechanical and thermal algesia in rats. Compared with the CCI group, the MWT and TWL were significantly higher on postoperative days 5 through 21 in the Tem1 group, suggesting that intrathecal tempol injection produced a persistent antinociceptive effect. However, there were no significant differences in the MWT and TWL on postoperative days 1 through 21 in the CCI or Tem2 groups, suggesting that intraperitoneal tempol injection did not produce an antinociceptive effect (Fig. 1a and b). Similarly, intraperitoneal injection of SOD produced similar antinociceptive effects as intrathecal injection of tempol (Fig. 1c, d), suggesting that tempol exerted its antinociceptive effects as an antioxidants.
The effect of tempol on the MWT (a) and the TWL (b) in rats in the sham, CCI, Tem1 (intrathecal injection of tempol daily for 7 days beginning 1 day after CCI), and Tem2 (intraperitoneal injection of tempol daily for 7 days beginning 1 day after CCI) groups. MWT and TWL tests were performed on preoperative day 3 and postoperative days 1, 3, 5, 7, 10, 14, and 21. C,D. The effect of tempol on the MWT (c) and the TWL (d) in rats in the CCI, Tem1 (intrathecal injection of tempol daily for 7 days beginning 1 day after CCI), and PC (intraperitoneal administration of the SOD for 7 days beginning 1 day after CCI) groups. MWT and TWL tests were performed on preoperative day 1 and postoperative days 1, 3, 5, and 7. n = 8. ns not significant, # p < 0.05 versus sham, *p < 0.05 versus CCI
Intraperitoneal Injection of Tempol Results in a Low Concentration in the Cerebrospinal Fluid (CSF)
The peak concentration of tempol in the CSF occurred within 20 min after intrathecal injection of tempol, which was significantly higher than that after intraperitoneal injection of tempol (Fig. 2a). The concentrations of tempol in the blood were not detectable after intrathecal injection of tempol (Fig. 2b). The concentration of tempol in the blood reached peak at approximately 40 min after intraperitoneal injection of tempol (Fig. 2b).
The time course of tempol concentration in the cerebrospinal fluid (a) and whole blood (b). Rats in the Tem1 and Tem2 group received, respectively, i.t. and i.p. injections of tempol (30 μg), and at various times after injection. Tempol concentration was determined with EPR spectroscopy. *p < 0.05 versus Tem2. n = 4
Intrathecal Injection of Tempol Reduces CCI-Induced Structural Damage in the Spinal Cord
Figure 3a shows normal white matter histology in the dorsal horn of the spinal cord in the sham group. No obvious edema was observed (Fig. 3a). CCI induced severe white matter damage in the dorsal horn of the spinal cord, including extensive edema, vacuolar degeneration, and proliferation of meningeal cells (Fig. 3b). In the Tem1 group, reduced edema, decreased proliferation of meningeal cells, and no obvious vacuolar degeneration were found, suggesting that intrathecal tempol injection reduced the CCI-induced white matter damage in the dorsal horn of the spinal cord (Fig. 3c). Contrastingly, no obvious reduction of CCI-induced white matter damage was observed following intraperitoneal tempol injection (Fig. 3d).
No obvious edema or demyelination in the nerve fibers of the cauda equina in the sham group could be visualized by toluidine blue staining (Fig. 4a). In the CCI group, obvious edema in the nerve fibers and local axonal degeneration were observed, and the structure of the cauda equina was loose (Fig. 4b). In the Tem1 group, no obvious axonal degeneration or mild edema in the nerve fibers was found, suggesting that the intrathecal injection of tempol reduced the CCI-induced damage of the cauda equina (Fig. 4c). However, intraperitoneal injection of tempol caused no obvious improvement in CCI-induced damage of the cauda equina (Fig. 4d).
Representative electron microscopic findings in the sham, CCI, Tem1, and Tem2 groups are shown in Fig. 5. In the sham group, the normal ultrastructure of the spinal cord, with intact axons and myelin lamellae of myelinated fibers, was seen. In the CCI group, severe edema, disintegrated myelin lamellae of the myelinated fibers, and obvious interstitial edema were seen. The unmyelinated fibers showed unclear boundaries (Fig. 5b). In the Tem1 group, the CCI-induced ultrastructural damage was milder when compared with the CCI group. Local edema and disintegration of myelin lamellae in the myelinated fibers were still seen, but to a lesser extent than in the CCI group (Fig. 5c). Unmyelinated fibers showed mild swelling. However, in the Tem2 group, intraperitoneal injection of tempol did not result in an obvious improvement in CCI-induced ultrastructural damage (Fig. 5d). The ultrastructure damage scores in the cauda equina were significantly higher in the CCI group when compared with the sham group (p < 0.05, Fig. 5e). Intrathecal tempol injection significantly reduced the CCI-induced increase in ultrastructure damage scores in the cauda equina (p < 0.05, Fig. 5e). There were no significant differences in the ultrastructure damage scores between the CCI and Tem2 groups, suggesting that intraperitoneal tempol injection did not significantly reduce the CCI-induced increase in the ultrastructure damage scores in the cauda equine (p > 0.05, Fig. 5e).
Representative electron microscopic images of myelinated and unmyelinated fibers in the cauda equina in in the sham (a), CCI (b), Tem1 (c), and Tem2 (d) groups. Arrows indicate locally disintegrated myelin lamellae and intracellular edema in myelinated fibers. Cauda equina fibers ultrastructure damage score in the sham, CCI, Tem1, and Tem2 groups (e). Magnification ×8000. n = 4
Intrathecal Injection of Tempol Reduces the CCI-Induced Increase in MDA Levels in the Spinal Cord
The MDA level in the spinal cord was significantly higher in the CCI group when compared with the sham group (p < 0.05, Fig. 6). Intrathecal tempol injection significantly reduced the CCI-induced increase in MDA levels in the spinal cord (p < 0.05, Fig. 6). There was no significant difference in MDA levels in the spinal cord between the CCI and Tem2 groups, suggesting that intraperitoneal tempol injection did not significantly reduce the CCI-induced increase in MDA levels in the spinal cord (p > 0.05, Fig. 6). Additionally, no significant differences were seen in the plasma MDA levels among the four groups (p > 0.05, Fig. 6).
Intrathecal Injection of Tempol Increases SOD Activities in the Spinal Cord
SOD activity in the spinal cord was not significantly different in the CCI and TEM2 groups when compared with the sham group (p < 0.05, Fig. 7). Compared with the CCI group, SOD activity was significantly higher in the Tem1 group (p < 0.05), suggesting that intrathecal tempol injection induced a significant increase in SOD activity in the spinal cord (p < 0.05, Fig. 7). In contrast, there was no significant difference in SOD activity between the sham, CCI, and Tem1 group’s plasma (p > 0.05, Fig. 7). Compared with the CCI group, SOD activity was significantly higher in the Tem2 group (p < 0.05, Fig. 7), suggesting that the intraperitoneal tempol injection induced an increase in SOD activity in the plasma.
Tempol Downregulates NGF Expression via the p38MAPK Signaling Pathway in the Spinal Cord
We examined NGF expression in the dorsal horn of the spinal cord using immunocytochemistry and Western blot analysis (Fig. 8). In the sham group, weak NGF immunoreactivity was observed in both the gray and white matter of the spinal cord (Fig. 7a). In contrast, strong NGF expression was upregulated in the CCI rats (Fig. 8b, e). NGF immunoreactivity was observed in the Tem1 group, and NGF-positive cells were significantly inhibited in the Tem1 group when compared with the CCI group (Fig. 8c and e). The significant decrease in the number of NGF-positive cells in the Tem1 group suggests that intrathecal tempol injection further downregulates NGF expression in CCI rats. However, intraperitoneal tempol injection did not decrease the expression of NGF (Fig. 8d and e).Consistent with these immunohistochemical findings, Western blot analysis indicated that intrathecal tempol injection (Tem1 group), but not the intraperitoneal injection of tempol (Tem2 group), inhibited CCI-induced increases in NGF expression in the spinal cord (Fig. 8f and g).
Spinal cord NGF expression in the sham, CCI, Tem1, and Tem2 groups (a–d). Representative immunocytochemical staining of spinal cord NGF in the sham (a), CCI (b), Tem1 (c), and Tem2 (d) groups. e The integral optical density of NGF-positive cells in the sham, CCI, Tem1, and Tem2 groups. f Western blot results showing the expression of NGF protein in the spinal cord of rats in the sham, CCI, Tem1, and Tem2 groups. The relative expression of NGF was normalized to the expression of β-actin. # p < 0.05 versus sham, *p < 0.05 versus CCI. n = 4
We further tested p38MAPK expression in the dorsal horn of the spinal cord using Western blot analysis. The expression of p38MAPK was upregulated in the CCI rats (Fig. 9a, b). Intrathecal tempol injection (Tem1 group) but not intraperitoneal injection of tempol (Tem2) inhibited CCI-induced upregulation of p38MAPK in the spinal cord (Fig. 9a, b). The p38MAPK inhibitor SB203580 inhibited tempol-induced downregulation of NGF in CCI rats (Fig. 9c, d).
p38MAPK mediated Tempol-induced downregulation of NGF in CCI rats. a Representative Western blot results showing the expression of p38MAPK in the spinal cord of rats in the sham, CCI, Tem1, and Tem2 groups. b The relative expression of p38MAPK was normalized to the expression of β-actin. # p < 0.05 versus sham, *p < 0.05 versus CCI. n = 4. c Representative Western blot results showing the expression of NGF in the spinal cord of rats in the sham, CCI, Tem1, and Tem2 groups after intrathecal injection of p38MAPK inhibitor SB203580. d The relative expression of NGF was normalized to the expression of β-actin. ns not significant
Discussion
We investigated the antinociceptive effects of intrathecal or intraperitoneal tempol injection on CCI-induced neuropathic pain in rats. We found that intrathecal tempol administration for 7 days beginning 1 day after CCI significantly increased the MWT and TWL on postoperative days 5 through 21 in CCI rats. This increase in the MWT and TWL suggested that the intrathecal injection of tempol produced a persistent antinociceptive effect. In contrast, intraperitoneal tempol administration for 7 days beginning 1 day after CCI did not reduce CCI-induced neuropathic pain on postoperative days 1 through 21. Supporting the results of the neurobehavioral tests, intrathecal tempol administration reduced CCI-induced structural damage in the spinal cord, while intraperitoneal administration did not. We also found that tempol produced a similar antinociceptive effect as the antioxidant SOD, suggesting that tempol produced antinociceptive effect as an antioxidant. Consistent with our results, (Tal 1996) Tal found that tempol, as an SOD mimetic, reduced thermal hyperalgesia in rats with chronic constriction nerve injury. Furthermore, we found that the intrathecal injection of tempol reduced the CCI-induced increase in MDA levels and increased SOD activity in the spinal cord. Once again, similar results were not seen in rats given an intraperitoneal administration of tempol. Finally, intrathecal tempol injection downregulated NGF expression in the spinal cord, but intraperitoneal injection did not. The specific p38MAPK inhibitor prevented tempol-induced downregulation of NGF in CCI rats. These results suggest that the intrathecal injection of tempol may inhibit CCI-induced neuropathic pain by increasing SOD activities and inhibiting NGF expression via the p38MAPK signaling pathway.
Tempol has a small molecular weight and can easily cross the blood–brain barrier (Mitchell et al. 1991). Tempol has been reported to exhibit neuroprotective effects in a rat model of SCI (Patel et al. 2009; Xiong and Hall 2009). Consistent with these reports, we found that intrathecal tempol administration (30 μg) reduced CCI-induced neuropathic pain in rats. However, we found that intraperitoneal administration of tempol at an equal dose (30 μg) did not produce an antinociceptive effect in CCI rats. The contrast between these results is likely to be because the intraperitoneal injection of 30 μg tempol did not result in a spinal concentration high enough (>30 μg) to inhibit the CCI-induced neuropathic pain or reverse the CCI-induced structural damage in the spinal cord. Tempol is highly lipophilic and membrane-permeable, and intraperitoneally administrated tempol may be sequestered by many of the target organs, such as the brain (Kato et al. 2003), liver (Blonder et al. 2000), and kidney (Chatterjee et al. 2000), leading to a spinal concentration insufficient for pain inhibition. Intraperitoneal administration of tempol may be more appropriate to selectively target organs that are able to accumulate higher concentrations of the molecule. For instance, it has been reported that intraperitoneal administration of tempol effectively protects against ischemia–reperfusion injury in the kidney and liver.
In the present study, we found that the intrathecal injection of tempol reduced structural damage in the spinal cord. Histology showed that intrathecal tempol injection reduced CCI-induced white matter damage, including edema and vacuolar degeneration in the dorsal horn of the spinal cord. Examination of spinal cord tissue by electron microscopy showed that tempol reduced local edema and disintegration of the myelin lamellae in the myelinated fibers of the cauda equina. The reduction of CCI-induced damage in the cauda equina after intrathecal injection of tempol suggests that the intrathecal injection of tempol could be used to treat cauda equina syndrome after nerve injury.
ROS have been reported to contribute to the pathogenesis of neuropathic pain (Choi et al. 2012; Kallenborn-Gerhardt et al. 2013b). MDA is known to be a lipid peroxidation marker (Ohsawa et al. 2007). MDA is formed via degradation of polyunsaturated lipids by ROS and, thus, may reflect the level of oxidative stress. We found that CCI induced an increase in spinal cord MDA levels, suggesting that oxidative stress may contribute to neuropathic pain in CCI rats. The intrathecal injection of tempol reduced the CCI-induced increase in MDA levels, suggesting that tempol may exert antinociceptive effects via a reduction of oxidative stress in the spinal cord. It has been reported that tempol exerts anti-oxidative stress activities due to its ability to scavenge superoxide radicals (O2 −) by acting as a SOD mimetic (Wilcox 2010). In the present study, we found that the intrathecal administration of tempol increased SOD activity in the spinal cord. Our results, therefore, support the idea that tempol produces antinociceptive effects via increased SOD activity. Additionally, we found that the intraperitoneal injection of tempol increased SOD activity in the plasma, but that the increase in SOD activity in the plasma was not associated with the antinociceptive effects of tempol.
NGF, a prototypical neurotrophin, regulates the development and maintenance of the central and peripheral nervous system and has been reported to contribute to neuropathic pain (Dray 2008). NGF has been reported to upregulate many pain-related genes in the primary sensory neurons of dorsal root ganglion including voltage-gate sodium channels and TPV1 (Fang et al. 2005; Lindsay and Harmar 1989; Zhu and Oxford 2007). Upregulation of these ion channels may result in an increase in firing in the afferent neurons following neve injury, thus leading to neuropathic pain conditions (Siniscalco et al. 2011). Clinical and animal studies have shown that systemic NGF administration increases thermal and mechanical hyperalgesia (Cahill et al. 2003; Hayashida and Eisenach 2010; Petty et al. 1994). Additionally, Nitya et al. reported that atorvastatin attenuated neuropathic pain by inhibiting NGF in the sciatic nerve and spinal cord, suggesting that NGF inhibition may be a potential therapeutic strategy for the management of neuropathic pain (Pathak et al. 2013). We also investigated the effect of tempol on NGF expression in the spinal cord in CCI rats. CCI induced persistent mechanical and thermal algesia that was accompanied by severe structural damage in the spinal cord. The expression of NGF was significantly increased following CCI, suggesting that the upregulation of endogenous NGF expression may contribute to marked hypersensitivity to both mechanical and thermal stimuli after CCI. The intrathecal administration of tempol further decreased the post CCI expression of NGF, and inhibition of NGF expression was accompanied by decreased neuropathic pain and reduced structural damage. This result suggests that tempol may exert neuroprotective effects on the spinal neurons via downregulation of NGF expression.
In this study, we further found that the p38MARK inhibitor SB203580 blocked tempol-induced downregulation of NGF in CCI rats. Several studies have shown that NGF activates the p38MAPK signaling pathway, and subsequently increases the expression of TRPV1, leading to neuropathic pain (Ji et al. 2002; Julius and Basbaum 2001; Zhu and Oxford 2007). It has been reported that p38MAPK inhibition reduces neuropathic pain in animal models (Clark et al. 2007; Gwak and Hulsebosch 2007; Hains and Waxman 2006; Wen et al. 2007). Our findings that inhibition of p38MAPK blocked tempol-induced NGF in CCI rats suggest that the p38MAPK pathway mediates tempol-induced downregulation of NGF expression in neuropathic pain.
In summary, we investigated the antinociceptive effects of intrathecal or intraperitoneal tempol injection in a rat model of CCI-induced neuropathic pain. We found that intrathecal, but not intraperitoneal, tempol injection produced a persistent antinociceptive effect in CCI rats. The antinociceptive effect of the intrathecal tempol injection was accompanied by reduced structural damage and decreased MDA levels in the spinal cord. We also found that intrathecal tempol administration increased SOD activity and upregulated the expression of NGF in the spinal cord, suggesting that tempol might produce antinociceptive effects by increasing SOD activities or by upregulating the expression of NGF.
Conclusions
Intrathecal injection of tempol produces antinociceptive effects and reduces CCI-induced structural damage in the spinal cord by increasing SOD activities and upregulating the expression of NGF, and the mechanism is related to inhibiting p38MAPK. Intraperitoneal administration of tempol does not exhibit antinociceptive effects.
References
Attal N, Lanteri-Minet M, Laurent B, Fermanian J, Bouhassira D (2011) The specific disease burden of neuropathic pain: results of a French nationwide survey. Pain 152:2836–2843. doi:10.1016/j.pain.2011.09.014
Beaudry F, Girard C, Vachon P (2007) Early dexamethasone treatment after implantation of a sciatic-nerve cuff decreases the concentration of substance P in the lumbar spinal cord of rats with neuropathic pain. Can J Vet Res 71:90–97
Bennett GJ, Xie YK (1988) A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain 33:87–107
Blonder JM, McCalden TA, Hsia CJ, Billings RE (2000) Polynitroxyl albumin plus tempol attenuates liver injury and inflammation after hepatic ischemia and reperfusion. Life Sci 67:3231–3239
Bouhassira D, Lanteri-Minet M, Attal N, Laurent B, Touboul C (2008) Prevalence of chronic pain with neuropathic characteristics in the general population. Pain 136:380–387. doi:10.1016/j.pain.2007.08.013
Cahill CM, Dray A, Coderre TJ (2003) Intrathecal nerve growth factor restores opioid effectiveness in an animal model of neuropathic pain. Neuropharmacology 45:543–552
Cao YY, Ding XD, Meng LX, Zhao BS (2014) Effects of tempol preconditioning on the expression level of HIF-α and VEGF after brain injure induced by cardiac arrest in rats. Guandong Med J 35:497–500
Chatterjee PK, Cuzzocrea S, Brown PA, Zacharowski K, Stewart KN, Mota-Filipe H, Thiemermann C (2000) Tempol, a membrane-permeable radical scavenger, reduces oxidant stress-mediated renal dysfunction and injury in the rat. Kidney Int 58:658–673. doi:10.1046/j.1523-1755.2000.00212.x
Choi DC, Lee JY, Lim EJ, Baik HH, Oh TH, Yune TY (2012) Inhibition of ROS-induced p38MAPK and ERK activation in microglia by acupuncture relieves neuropathic pain after spinal cord injury in rats. Exp Neurol 236:268–282. doi:10.1016/j.expneurol.2012.05.014
Clark AK et al (2007) Inhibition of spinal microglial cathepsin S for the reversal of neuropathic pain. Proc Natl Acad Sci USA 104:10655–10660. doi:10.1073/pnas.0610811104
Costigan M, Scholz J, Woolf CJ (2009) Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci 32:1–32. doi:10.1146/annurev.neuro.051508.135531
Doth AH, Hansson PT, Jensen MP, Taylor RS (2010) The burden of neuropathic pain: a systematic review and meta-analysis of health utilities. Pain 149:338–344. doi:10.1016/j.pain.2010.02.034
Dray A (2008) Neuropathic pain: emerging treatments. Br J Anaesth 101:48–58. doi:10.1093/bja/aen107
Dworkin RH et al (2010) Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc 85:S3–S14. doi:10.4065/mcp.2009.0649
Fang X, Djouhri L, McMullan S, Berry C, Okuse K, Waxman SG, Lawson SN (2005) trkA is expressed in nociceptive neurons and influences electrophysiological properties via Nav1.8 expression in rapidly conducting nociceptors. J Neurosci 25:4868–4878. doi:10.1523/jneurosci.0249-05.2005
Gao X, Kim HK, Chung JM, Chung K (2007) Reactive oxygen species (ROS) are involved in enhancement of NMDA-receptor phosphorylation in animal models of pain. Pain 131:262–271. doi:10.1016/j.pain.2007.01.011
Gwak YS, Hulsebosch CE (2007) Inhibition of neuronal p38-mapk activation attenuates below-level central neuropathic pain following spinal cord injury. J Neurotrauma 24:1259
Gwak YS, Kang J, Unabia GC, Hulsebosch CE (2012) Spatial and temporal activation of spinal glial cells: role of gliopathy in central neuropathic pain following spinal cord injury in rats. Exp Neurol 234:362–372. doi:10.1016/j.expneurol.2011.10.010
Gwak YS, Hassler SE, Hulsebosch CE (2013) Reactive oxygen species contribute to neuropathic pain and locomotor dysfunction via activation of CamKII in remote segments following spinal cord contusion injury in rats. Pain 154:1699–1708. doi:10.1016/j.pain.2013.05.018
Hahn SM et al (1992) Tempol, a stable free radical, is a novel murine radiation protector. Cancer Res 52:1750–1753
Hains BC, Waxman SG (2006) Activated microglia contribute to the maintenance of chronic pain after spinal cord injury. J Neurosci 26:4308–4317. doi:10.1523/jneurosci.0003-06.2006
Hayashida K, Eisenach JC (2010) Spinal alpha 2-adrenoceptor-mediated analgesia in neuropathic pain reflects brain-derived nerve growth factor and changes in spinal cholinergic neuronal function. Anesthesiology 113:406–412. doi:10.1097/ALN.0b013e3181de6d2c
Janes K, Neumann WL, Salvemini D (2012) Anti-superoxide and anti-peroxynitrite strategies in pain suppression. Biochim Biophys Acta 1822:815–821. doi:10.1016/j.bbadis.2011.12.008
Ji RR, Samad TA, Jin SX, Schmoll R, Woolf CJ (2002) p38 MAPK activation by NGF in primary sensory neurons after inflammation increases TRPV1 levels and maintains heat hyperalgesia. Neuron 36:57–68
Julius D, Basbaum AI (2001) Molecular mechanisms of nociception. Nature 413:203–210. doi:10.1038/35093019
Kallenborn-Gerhardt W et al (2013a) Antioxidant activity of sestrin 2 controls neuropathic pain after peripheral nerve injury. Antioxid Redox Signal 19:2013–2023. doi:10.1089/ars.2012.4958
Kallenborn-Gerhardt W, Schroder K, Geisslinger G, Schmidtko A (2013b) NOXious signaling in pain processing. Pharmacol Ther 137:309–317. doi:10.1016/j.pharmthera.2012.11.001
Kato N, Yanaka K, Hyodo K, Homma K, Nagase S, Nose T (2003) Stable nitroxide Tempol ameliorates brain injury by inhibiting lipid peroxidation in a rat model of transient focal cerebral ischemia. Brain Res 979:188–193
Khalil Z, Liu T, Helme RD (1999) Free radicals contribute to the reduction in peripheral vascular responses and the maintenance of thermal hyperalgesia in rats with chronic constriction injury. Pain 79:31–37
Lindsay RM, Harmar AJ (1989) Nerve growth factor regulates expression of neuropeptide genes in adult sensory neurons. Nature 337:362–364. doi:10.1038/337362a0
Liu HX, Zhang JJ, Zhang L, Liu H (2013) Effects of tempol on white matter lesions and cognitive impairment in a rat model of chronic cerebral hypoperfusion. Zhonghua yi xue za zhi 93:1330–1334
Liu X et al (2014) Early repeated administration of progesterone improves the recovery of neuropathic pain and modulates spinal 18 kDa-translocator protein (TSPO) expression. J Steroid Biochem Mol Biol 143:130–140. doi:10.1016/j.jsbmb.2014.02.017
Matsuo H et al (2014) Early transcutaneous electrical nerve stimulation reduces hyperalgesia and decreases activation of spinal glial cells in mice with neuropathic pain. Pain 155:1888–1901. doi:10.1016/j.pain.2014.06.022
Mitchell JB et al (1991) Inhibition of oxygen-dependent radiation-induced damage by the nitroxide superoxide dismutase mimic, tempol. Arch Biochem Biophys 289:62–70
Ohayon MM, Stingl JC (2012) Prevalence and comorbidity of chronic pain in the German general population. J Psychiatr Res 46:444–450. doi:10.1016/j.jpsychires.2012.01.001
Ohsawa I et al (2007) Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat Med 13:688–694. doi:10.1038/nm1577
Patel SP, Sullivan PG, Pandya JD, Rabchevsky AG (2009) Differential effects of the mitochondrial uncoupling agent, 2,4-dinitrophenol, or the nitroxide antioxidant, Tempol, on synaptic or nonsynaptic mitochondria after spinal cord injury. J Neurosci Res 87:130–140. doi:10.1002/jnr.21814
Pathak NN et al (2013) Antihyperalgesic and anti-inflammatory effects of atorvastatin in chronic constriction injury-induced neuropathic pain in rats. Inflammation 36:1468–1478. doi:10.1007/s10753-013-9688-x
Petty BG et al (1994) The effect of systemically administered recombinant human nerve growth factor in healthy human subjects. Ann Neurol 36:244–246. doi:10.1002/ana.410360221
Sakura S, Kirihara Y, Muguruma T, Kishimoto T, Saito Y (2005) The comparative neurotoxicity of intrathecal lidocaine and bupivacaine in rats. Anesth Analg 101:541–547. doi:10.1213/01.ANE.0000155960.61157.12
Schwartz ES, Lee I, Chung K, Chung JM (2008) Oxidative stress in the spinal cord is an important contributor in capsaicin-induced mechanical secondary hyperalgesia in mice. Pain 138:514–524. doi:10.1016/j.pain.2008.01.029
Siniscalco D, Giordano C, Rossi F, Maione S, de Novellis V (2011) Role of neurotrophins in neuropathic pain. Curr Neuropharmacol 9:523–529. doi:10.2174/157015911798376208
Smith BH, Torrance N (2012) Epidemiology of neuropathic pain and its impact on quality of life. Curr Pain Headache Rep 16:191–198. doi:10.1007/s11916-012-0256-0
Smith BH, Torrance N, Bennett MI, Lee AJ (2007) Health and quality of life associated with chronic pain of predominantly neuropathic origin in the community. Clin J Pain 23:143–149. doi:10.1097/01.ajp.0000210956.31997.89
Tal M (1996) A novel antioxidant alleviates heat hyperalgesia in rats with an experimental painful peripheral neuropathy. Neuroreport 7:1382–1384
Torrance N, Smith BH, Bennett MI, Lee AJ (2006) The epidemiology of chronic pain of predominantly neuropathic origin. Results from a general population survey. J Pain 7:281–289. doi:10.1016/j.jpain.2005.11.008
Wen YR et al (2007) Nerve conduction blockade in the sciatic nerve prevents but does not reverse the activation of p38 mitogen-activated protein kinase in spinal microglia in the rat spared nerve injury model. Anesthesiology 107:312–321. doi:10.1097/01.anes.0000270759.11086.e7
Wilcox CS (2010) Effects of tempol and redox-cycling nitroxides in models of oxidative stress. Pharmacol Ther 126:119–145. doi:10.1016/j.pharmthera.2010.01.003
Xiong Y, Hall ED (2009) Pharmacological evidence for a role of peroxynitrite in the pathophysiology of spinal cord injury. Exp Neurol 216:105–114. doi:10.1016/j.expneurol.2008.11.025
Xiong Y, Singh IN, Hall ED (2009) Tempol protection of spinal cord mitochondria from peroxynitrite-induced oxidative damage. Free Radic Res 43:604–612. doi:10.1080/10715760902977432
Zhao BS, Ding YY, Wang H, Han G, Meng LX (2013) Effects of hyperbaric oxygen postconditioning of microglia on activation in rats model of neuropathic pain. Int J Anesth Resus 34:546–548
Zhao BS, Meng LX, Ding YY, Cao YY (2014a) Hyperbaric oxygen treatment produces an antinociceptive response phase and inhibits astrocyte activation and inflammatory response in a rat model of neuropathic pain. J Mol Neurosci 53:251–261. doi:10.1007/s12031-013-0213-3
Zhao BS, Meng LX, Tan YH, Song XR (2014b) Effects hyperbaric oxygen treatment on expression of nerve growth factor in spinal cord of rats with neuropathic pain. Chin J Anesthesiol 34:800–803
Zhao BS, Song XR, Hu PY, Meng LX, Tan YH, She YJ, Ding YY (2015) Hyperbaric oxygen treatment at various stages following chronic constriction injury produces different antinociceptive effects via regulation of P2X4R expression and apoptosis. PLoS One 10:e0120122. doi:10.1371/journal.pone.0120122
Zhu W, Oxford GS (2007) Phosphoinositide-3-kinase and mitogen activated protein kinase signaling pathways mediate acute NGF sensitization of TRPV1. Mol Cell Neurosci 34:689–700. doi:10.1016/j.mcn.2007.01.005
Acknowledgments
This work was supported by the Medjaden Academy & Research Foundation for Young Scientists and BBraun Anesthesia Scientific Research Fund (Grant Nos. MJR20150037 and BBF 2012-012).We thank Dr. Lingxin Meng for supporting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhao, B., Pan, Y., Wang, Z. et al. Intrathecal Administration of Tempol Reduces Chronic Constriction Injury-Induced Neuropathic Pain in Rats by Increasing SOD Activity and Inhibiting NGF Expression. Cell Mol Neurobiol 36, 893–906 (2016). https://doi.org/10.1007/s10571-015-0274-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10571-015-0274-7