Abstract
Proteins of Bcl-2 family are crucial regulators of intrinsic (mitochondrial) pathway of apoptosis that is implicated among the mechanisms of ischemic neuronal death. Initiation of mitochondrial apoptosis depends on changes of equilibrium between anti-apoptotic and pro-apoptotic proteins of Bcl-2 family as well as on translocation of pro-apoptotic proteins of Bcl-2 family to mitochondria. The aim of this work was to study the effect of transient global brain ischemia on expression and intracellular distribution of proteins of Bcl-2 family in relation to the ischemia-induced changes of ERK and Akt kinase pathways as well as disturbances in ubiquitin proteasome system. Using four vessel occlusion model of transient global brain ischemia, we have shown that both ischemia in duration of 15 min and the same ischemia followed by 1, 3, 24, and 72 h of reperfusion did not affect the levels of either pro-apoptotic (Bad, PUMA, Bim, Bax, Noxa) or anti-apoptotic (Bcl-2, Bcl-xl, Mcl-1) proteins of Bcl-2 family in total cell extracts from rat hippocampus. However, significantly elevated level of Bad protein in the mitochondria isolated from rat hippocampus was observed already 1 h after ischemia and remained elevated 3 and 24 h after ischemia. We did not observe significant changes of the levels of Puma, Bax, Bcl-2, and Bcl-xl in the mitochondria after ischemia and ischemia followed by reperfusion. Our results might indicate possible involvement of Bad translocation to mitochondria in the mechanisms of neuronal death following transient global brain ischemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Proteins of Bcl-2 family are crucial regulators of intrinsic (mitochondrial) pathway of apoptosis that is induced by global brain ischemia as documented in several previous studies (Chen et al. 1998; Krajewski et al. 1999; Perez-Pinzon et al. 1999; Sugawara et al. 1999; Cao et al. 2002; Tanaka et al. 2004; Hetz et al. 2005; Endo et al. 2006a; Miyawaki et al. 2008; Racay et al. 2009) and is often implicated among the mechanisms of delayed neuronal death induced by transient global brain ischemia (Nakka et al. 2008; Niizuma et al. 2010). In addition to mitochondrial apoptosis, proteins of Bcl-2 family play an important role in regulation of other cellular pathways with a strong impact on cell survival like autophagy (Rodriguez et al. 2011), ER stress (Rodriguez et al. 2011), ER calcium handling (Szegezdi et al. 2009; Bonneau et al. 2013), energetic metabolism (Hardwick et al. 2012), and cell cycle progression (Galluzzi et al. 2012). Initiation of mitochondrial apoptosis depends on changes of either equilibrium or protein–protein interactions between anti-apoptotic and pro-apoptotic proteins of Bcl-2 family as well as on translocation of pro-apoptotic proteins of Bcl-2 family to mitochondria (Taylor et al. 2008; Youle and Strasser 2008). The central mechanisms to modulate proteins of Bcl-2 family at the levels of protein stability, intracellular localization, and protein–protein interactions involve pathways regulated by Akt (Duronio 2008) and extracellular signal-regulated (ERK) kinases as well as by ubiquitin–proteasome system (UPS) (Fennell et al. 2008; Balmanno and Cook 2009). Transient global brain ischemia (TGBI) represents a form of severe metabolic stress that has strong impact on post-translational modifications of proteins (Lipton 1999) resulting in activation or inhibition of ERK (Sawe et al. 2008) and Akt kinase (Endo et al. 2006b) pathways. In addition, inhibition of 26S proteasome (Kamikubo and Hayashi 1996; Asai et al. 2002; Ge et al. 2007) and depletion of free ubiquitin in pyramidal neurons of hippocampus (Kato et al. 1993; Morimoto et al. 1996) observed after transient global brain ischemia have been considered to be main mechanisms responsible for ischemia-induced dysfunction of UPS.
Therefore, the aim of this work was to study the effect of transient global brain ischemia on expression and intracellular distribution of selected proteins of Bcl-2 family in relation to the ischemia-induced changes of ERK and Akt kinase pathways as well as disturbances in UPS.
We have focused our interest on Bax that together with Bak and Bok belongs to the group of pro-apoptotic pore-forming proteins of Bcl-2 family responsible for permeabilization of outer mitochondrial membrane and release of pro-apoptotic molecules from mitochondrial intermembrane space to cytosol (Youle and Strasser 2008). Bax is widely expressed in the brain (Krajewski et al. 1995a) while Bok is present only in ischemia-resistant CA3 neurons (Lein et al. 2004). Full-length Bak is present only in non-neuronal cells in brain, whereas neurons express an unusual BH3-only splice variant of Bak which has anti-apoptotic activity (Sun et al. 2001). Function of Bax is suppressed by phosphorylation with Akt kinase (Tsuruta et al. 2002; Gardai et al. 2004). Translocation of Bax to mitochondria and consequent pore formation is inhibited by anti-apoptotic proteins of Bcl-2 family. Among them, Bcl-xl is the main anti-apoptotic protein expressed in CNS (Krajewski et al. 1994). Deletion of Bcl-x gene by homology recombination was associated with massive death of neuronal cells (Motoyama et al. 1995) whereas deletion of other genes coding for anti-apoptotic proteins of Bcl-2 family had not any impact on survival of neuronal cells (Youle and Strasser 2008). Despite low expression of Bcl-2 and Mcl-1 (Krajewski et al. 1995b) as well as Bim (Inta et al. 2006) in CNS, we have focused our interest on these proteins as well. Bim is pro-apoptotic protein of Bcl-2 family that is controlled by ERK at transcription level (Balmanno and Cook 2009). In addition, its intracellular localization is regulated by crosstalk between ERK and UPS (Balmanno and Cook 2009). Stability of Mcl-1 is controlled by both Akt and ERK pathways (Balmanno and Cook 2009) whereas stability of Noxa depends on activity of 26S proteasome and interaction with Mcl-1 (Craxton et al. 2012). Finally, we have examined expression and intracellular localization of Bad and PUMA. Intracellular localization of Bad is controlled by ERK and Akt kinases, while its stability depends on activity of UPS (Balmanno and Cook 2009). Stability of PUMA does not depend on activity of UPS (Fennell et al. 2008) but it is considered to be an important mediator of the vulnerability of CA1 hippocampal neurons to proteasome inhibition in vivo (Tsuchiya et al. 2011).
Materials and Methods
Ischemia–Reperfusion
Animal studies were performed under a protocol approved by the State Veterinary and Food Department of Slovak Republic. A total of 50 adult male Wistar rats from the breeding house of the Institute of Experimental Pharmacology of Slovak Academy of Science (Dobra voda, Slovak Republic) were used. All animals were maintained on a 12/12-h light/dark cycle. Food and water were available ad libitum until the beginning of the experiment. Transient global cerebral ischemia was produced using the four-vessel occlusion model according to (Pulsinelli and Brierley 1979) with some modifications. Briefly, on day 1, both vertebral arteries were irreversibly occluded by coagulation through the alar foramina after anesthesia with 2 % halothane, 30 % O2, and 68 % N2O mixture. On day 2, both common carotid arteries were occluded for 15 min by small clips under anesthesia with 2 % halothane, 30 % O2, and 68 % N2O mixture. Two minutes before carotid occlusion, the halothane was removed from the mixture. Body temperature was maintained using a homoeothermic blanket. Global ischemia was followed by 1, 3, 24, and 72 h of reperfusion. After ischemia and particular time of reperfusion, animals were sacrificed by decapitation under deep anesthesia with 2 % halothane, 30 % O2, and 68 % N2O mixture. Both hippocampi were dissected and processed immediately. Control animals underwent the same procedure except of carotid occlusion.
Preparation of Protein Extracts and Isolation of Mitochondria
Protein extracts were prepared by homogenization of both hippocampi in homogenization buffer (10 mM Tris–HCl pH = 7.4, 1 mM EDTA, 0.24 M sucrose) using a Potter Teflon-glass homogenizer. Total cell extract were prepared by addition of appropriate volume of 6X RIPA buffer (6X phosphate buffered saline, 6 % (v/v) Nonidet P-40, 3 % (w/v) sodium deoxycholate, 0.6 % (w/v) sodium dodecyl sulfate (SDS)) to homogenate.
Mitochondria were isolated by differential centrifugation. Homogenate was first centrifuged at 400 g for 5 min and supernatant was then centrifuged at 12,000 g for 10 min. Resulting sediment was resuspended in homogenization buffer and centrifuged at 12,000 g for 10 min. Final sediment was first resuspended in homogenization buffer and proteins were solubilized by addition of appropriate volume of 6X RIPA buffer.
Cytoplasmic proteins were isolated by centrifugation of post-mitochondrial supernatant at 30,000 g for 60 min. The resulted supernatant was used for experiments without any further processing while sediment was discarded.
Protein concentrations were determined by protein Dc assay kit (Bio-Rad) using BSA as standard.
Quantitative Western Blot Analysis
Isolated proteins were separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE). After electrophoresis, separated proteins were transferred on nitrocellulose membranes using a semi-dry transfer protocol. The membranes were controlled for even load and possible transfer artefacts by staining with Ponceau Red solution. After blocking with BSA blocking buffer (50 mM Tris–Cl, pH 7.5, 150 mM NaCl, 0.05 % Tween 20, 2 % BSA), membranes were first incubated for 90 min with primary mouse monoclonal antibodies against ubiquitin (1:500, sc-8017), β-actin (1:2000, sc-47778), Bcl-2 (1:200, sc-7382), p-ERK (1:200, sc-7383), Bad (1.200, sc-8044) (all Santa Cruz Biotechnology), and Cox I (1 μg/ml, 459600, Invitrogen) or rabbit polyclonal antibodies raised against Bax (1:200, sc-493), Bcl-xl (1:200, sc-7195), Bim (1:200, sc-11425), PUMA (1:200, sc-28226), p-Akt (1:200, sc-100629), ERK (1:200, sc-93), Mcl-1 (1:200, sc-20679) (all Santa Cruz Biotechnology), Noxa (1:500, PRS2437), and Akt (1:1000, SAB4500802) (all Sigma-Aldrich) dissolved in BSA blocking solution. Membranes incubated with primary antibodies were washed using TBS-T solution (50 mM Tris–Cl, pH 7.5, 150 mM NaCl, 0.05 % Tween 20) and then incubated with secondary antibodies conjugated with horse radish peroxidase (1:5000, Santa Cruz). After extensive washing with TBS-T solution (4 times 15 min), membranes were incubated in SuperSignal West Pico Chemiluminescent Substrate (Thermo) solution for 3 min. After exposition of membranes on Chemidoc XRS (BioRad), the intensities of corresponding bands were quantified using Quantity One software (BioRad). Intensities of bands of interest were normalized by corresponding intensities of bands of either β-actin or Cox I.
Statistical Analysis
All statistical analyses were done using GraphPad InStat V2.04a (GraphPad Software). For the comparison of ischemia-induced changes among all groups, a one-way ANOVA test was first carried out to test for differences among all experimental groups. Additionally, the unpaired Tukey’s test was used to determine differences between individual groups. Significance level was set at p < 0.05.
Results
Ischemia-induced disturbance of UPS are manifested by accumulation of ubiquitinylated proteins (Asai et al. 2002; Ge et al. 2007; Racay 2012) as well as depletion of free ubiquitin (Kato et al. 1993; Morimoto et al. 1996). The pattern of ubiquitinylated proteins in total cell extracts of samples derived from hippocampus of control animals and experimental animals subjected to 15 minutes of transient global brain ischemia and 1, 3, 24, or 72 h of reperfusion is shown in Fig. 1a. Massive accumulation of ubiquitinylated proteins was observed in hippocampus 1 and 3 h after ischemia (Fig. 1a). The quantitative analysis of the levels of ubiquitinylated proteins in hippocampal total cell extracts has revealed that ischemia did not significantly affect the levels of ubiquitinylated proteins (Fig. 1b). However, significant increase of ubiquitinylated protein levels to 310.2 % (p < 0.001), 329.3 % (p < 0.001), 193.9 % (p < 0.05), and 178.2 % (p < 0.05) of control was observed after 1, 3, 24, and 72 h of reperfusion, respectively (Fig. 1b). Accumulation of ubiquitinylated proteins was paralleled with the decrease of the level of free ubiquitin. As shown at Fig. 1c, significantly decreased level of free ubiquitin was documented 1 and 3 h after ischemia to 32.6 % (p < 0.001) and 36.6 % (p < 0.001) of control, respectively. Since UPS works often in hand with ERK and Akt kinase pathways, the time course of phosphorylation pattern representing active state of both kinases was investigated. Unlike accumulation of ubiquitinylated proteins, different time courses of the levels of phosphorylated forms of both ERK and Akt kinases were observed (Fig. 2a). We have observed transient decrease of Akt kinase phosphorylation at Ser472 after 15 min of ischemia (51.6 %, p < 0.01) that was followed with significant increase of p-Akt to 147.5 % (p < 0.01) after 3 h of reperfusion. Finally, p-Akt level has decreased to 54.7 % after 72 h of reperfusion (Fig. 2b). With respect of ERK, two isoforms of ERK, ERK1, and ERK2, and their phosphorylated forms were detected (Fig. 2a). Level of ERK1 phosphorylated at Tyr204 was significantly decreased to 46.6 % (p < 0.05) of control after ischemia. However, the level of ERK2 phosphorylated at Tyr204 was significantly decreased to 30.5 % (p < 0.001), 63.8 % (p < 0.01), and 48.1 % (p < 0.001) of control that was observed after 15 min of ischemia and ischemia followed with reperfusion in duration 24 and 72 h, respectively (Fig. 2c).
Effect of transient global brain ischemia on the levels of ubiquitinylated proteins and free ubiquitin. Rats were subjected to 15 min of transient global brain ischemia and 1, 3, 24, and 72 h of reperfusion. The patterns of protein ubiqitinylation were evaluated by Western blot analysis of total cell extracts prepared from the hippocampus of control and experimental rats, as described in Materials and Methods. The levels of ubiquitinylated proteins (a) and free ubiquitin (b) were evaluated by the Western blot analysis of cytoplasmic protein fraction prepared from the hippocampus of control and experimental rats, as described in Materials and Methods. c Quantification of the post-ischemic rise in ubiquitinylated proteins in the hippocampus. The data were normalized to β-actin level and expressed relative to controls. Data are presented as means ± SD (n = 5 per group). ***p < 0.001 (ANOVA, followed by Tukey’s test to determine differences between individual groups). d Quantification of ischemia-induced changes in free ubiquitin in the hippocampus. The data were normalized to β-actin level and expressed relative to control. Data are presented as means ± SD (n = 5 per group). *p < 0.05 (ANOVA, followed by Tukey’s test to determine differences between individual groups)
Effect of transient global brain ischemia on the level of phosphorylation of ERK and Akt kinase. a Rats were subjected to 15 min of transient global brain ischemia and 1, 3, 24, and 72 h of reperfusion. The patterns of ERK and Akt phosphorylation were evaluated by the Western blot analysis of total cell extracts prepared from the hippocampus of control and experimental rats, as described in Materials and Methods. b Quantification of ischemia-induced changes in Akt phosphorylation at in the hippocampus. The data were normalized to non-phosphorylated Akt level and expressed relative to control. Data are presented as means ± SD (n = 5 per group). *p < 0.05 (ANOVA, followed by Tukey’s test to determine differences between individual groups). c Quantification of ischemia-induced changes in ERK phosphorylation at in the hippocampus. The data normalized to the levels of non-phosphorylated isoforms ERK1 and ERK2 are expressed relative to control. Data are presented as means ± SD (n = 5 per group). *p < 0.05 (ANOVA, followed by Tukey’s test to determine differences between individual groups)
In order to study whether ischemia-induced changes observed at the level of UPS as well as at the level of ERK and Akt kinase pathways have impact on the levels of selected proteins of Bcl-2 family, we have performed the Western blot analysis of total cell extracts from hippocampi of control and experimental animals. All investigated proteins of Bcl-2 family have been already detected in total cell extracts from hippocampi of control animals. We have also detected Bcl-2 and Mcl-1 that are not abundantly expressed in CNS (Krajewski et al. 1995b) and weak signals were observed for all three isoforms of Bim (BimEL—extra-long, BimL—long, BimS—short isoform) that are also expressed at low levels in CNS (Inta et al. 2006). However, the levels of all investigated proteins of Bcl-2 family have not been significantly affected by ischemia and ischemia followed by reperfusion (Fig. 3).
Effect of transient global brain ischemia on the total levels of selected proteins of Bcl-2 family. Rats were subjected to 15 min of transient global brain ischemia and 1, 3, 24, and 72 h of reperfusion. The pattern of protein expression was evaluated by the Western blot analysis of total cell extracts prepared from both hippocampi of control and experimental rats as described in Materials and Methods. β-actin served as loading control
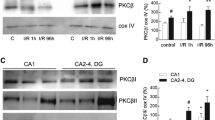
In addition to analysis of total cell extracts, we have determined the levels of selected proteins of Bcl-2 family in mitochondria isolated from hippocampi of control and experimental animals (Fig. 4a). We have observed that ischemia followed by reperfusion led to increase of Bad level in mitochondria, which was significant after 1 h (208.9 % of control, p < 0.01), 3 h (217.8 % of control, p < 0.01), and 24 h (209.3 % of control, p < 0.01) of reperfusion (Fig. 4b). We have also observed that ischemia followed by reperfusion led to increase of the level of PUMA protein in mitochondria; however, the changes were not statistically significant (Fig. 4c). The levels of other investigated proteins of Bcl-2 family in mitochondria were not significantly changed after ischemia and ischemia followed by reperfusion (Fig. 4a).
Effect of transient global brain ischemia on mitochondrial level of selected proteins of Bcl-2 family. a Rats were subjected to 15 min of transient global brain ischemia and 1, 3, 24, and 72 h of reperfusion. The mitochondrial level of selected proteins of Bcl-2 family was determined by the Western blot analysis of mitochondria isolated from control and experimental animals as described in Materials and Methods. b Quantification of the post-ischemic changes in Bad protein level in the hippocampal mitochondria. The data were normalized to COXI level and expressed as relative to controls. Data are presented as means ± SD (n = 5 per group). *p < 0.05, ***p < 0.001 (ANOVA, followed by Tukey’s test to determine differences between individual groups). c Quantification of the post-ischemic changes in PUMA protein level in the hippocampal mitochondria. The data were normalized to Cox I level and expressed relative to controls
Results presented in this study and in our other previous studies (Racay et al. 2007; Racay et al. 2009) indicate that majority of proteins of Bcl-2 family are already inserted in mitochondrial membrane in the cells of CNS. Therefore, we have investigated relative levels of selected proteins of Bcl-2 family in total cell extracts, mitochondria, and cytoplasm prepared from control rat hippocampi. As shown at Fig. 5, Bax, Bcl-xl, Bcl-2, PUMA, and Noxa were detected only in total cell extracts and mitochondria. Signals of these proteins correlate with that of cytochrome c oxidase subunit I (Cox I) used as mitochondrial marker. Bad was detected in all three fractions indicating significant amount of this protein in cytoplasm thus supporting suggestion that ischemia-induced initiation of apoptosis might be triggered by translocation of Bad to mitochondria.
Relative levels of selected proteins of Bcl-2 family in total cell extracts, mitochondria, and cytoplasm. The levels of selected proteins of Bcl-2 family were determined by the Western blot analysis of total cell extracts (TCE), mitochondria (MIT), and cytoplasm (CYT) prepared from control animals as described in Materials and Methods
Discussion
In this study, we have focused our interest on the effect of transient global brain ischemia on expression and intracellular distribution of selected proteins of Bcl-2 family in relation to the ischemia-induced changes of ERK and Akt kinase pathways as well as disturbances in UPS. We have shown that both ischemia in duration of 15 min and the same ischemia followed by 1, 3, 24, and 72 h of reperfusion did not affect the levels of either pro-apoptotic (Bad, PUMA, Bim, Bax, Noxa) or anti-apoptotic (Bcl-2, Bcl-xl, Mcl-1) proteins of Bcl-2 family in total cell extracts from rat hippocampus. However, significantly elevated level of Bad protein in the mitochondria isolated from rat hippocampus was observed already 1 h after ischemia and remained elevated 3 and 24 h after ischemia.
Despite relative strong impact of TGBI on UPS, ERK, and Akt kinase pathways, the total levels of investigated proteins of Bcl-2 family were not significantly affected by TGBI. It seems that systems controlling expression of proteins of Bcl-2 family are relative stable and short disturbances do not have significant impact on the levels of Bcl-2 family proteins. For example, expression of Bim was significantly elevated after focal brain ischemia in duration of 48 h (Inta et al. 2006) but not after 10 min of global brain ischemia (Sanderson et al. 2009).
Significant changes induced by TGBI were observed at the mitochondrial level of Bad. Impact of TGBI on translocation of Bad to mitochondria has already been subjected of previous studies with significantly different results. While some studies have documented ischemia-induced Bad translocation to mitochondria during early period of reperfusion (Abe et al. 2004; Miyawaki et al. 2008), the translocation of Bad to mitochondria during late period of reperfusion has been observed as well (Dłuzniewska et al. 2005). Finally, unchanged intracellular distribution of Bad after global brain ischemia was also documented (Sanderson et al. 2009). Our results are more consistent with the rapid post-ischemic translocation of Bad to mitochondria since significant increase of mitochondrial Bad level has been observed already 1 h after ischemia. Early translocation of Bad might be attributed to ischemia-induced inhibition of Akt kinase as the Akt-mediated phosphorylation of Bad was implicated to be the main mechanism responsible for inhibition of Bad translocation to mitochondria (Duronio 2008; Balmanno and Cook 2009). In addition to Bad, ischemia-induced translocation of PUMA to mitochondria has also been documented (Niizuma et al. 2009). In our experiments, we have also observed increased mitochondrial level of PUMA; however, the observed changes were not statistically significant. With respect to Bax, it is generally accepted that this protein is localized in cytoplasm and the signals responsible for mitochondrial apoptosis initiation are driving translocation of Bax to mitochondria (Lindsay et al. 2011). We have observed significantly increased mitochondrial level of Bax after TGBI in one of our previous study (Chomova et al. 2012). Similarly, enhanced expression of Bax after global brain ischemia has also been observed (Krajewski et al. 1995a). However, results presented in this study and in our other previous studies (Racay et al. 2007; Racay et al. 2009) are more consistent with a view that Bax is already inserted in the membrane of neural cell mitochondria but the formation of Bax pore is inhibited by interaction of Bax with Bcl-xl that is also located in mitochondrial membrane. Both Bax and Bcl-xl are the major proteins of Bcl-2 family expressed in CNS (Krajewski et al. 1994, 1995a). Results presented here might indicate that mitochondrial apoptosis after TGBI is initiated by translocation of Bad, and possibly PUMA, to mitochondria. Despite previously published importance of PUMA with respect to ischemia-induced mitochondrial apoptosis, our results are more in favor of Bad as apoptosis initiator. Unlike PUMA that was predominantly localized in mitochondria, significant amounts of Bad were found in cytoplasm of control animal supporting importance of ischemia-induced translocation of Bad to mitochondria. It is well known that Bad interacts strongly only with anti-apoptotic Bcl-xl but Bad does not bind other Bcl-2 family proteins including pro-apoptotic Bax (Yang et al. 1995). Interaction of Bad with Bcl-xl is associated with liberation of Bax from Bax/Bcl-xl heterodimers, consequent dimerization of Bax, formation of pore and cell death (Yang et al. 1995). The altered interaction Bad/Bcl-xl after TGBI has already been documented (Abe et al. 2004; Miyawaki et al. 2008). In addition to Bad, previous studies have documented translocation of p53 to mitochondria (Endo et al. 2006a; Racay et al. 2007; Racay et al. 2009). Thus, in cooperation with Bad, p53 might support liberation of Bax from inhibitory heterodimers with anti-apoptotic proteins of Bcl-2 family and consequent initiation of mitochondrial apoptosis.
The rapid translocation of Bad to mitochondria is not in accordance with the concept of delayed ischemic neuronal death that was observed a few days after initial ischemic insult (Kirino 2000) as well as with the concept of rapid execution of mitochondrial apoptosis after its initiation (Green 2005). It might well be that the delay between initial pro-apoptotic process represented by translocation of Bad to mitochondria and final execution of apoptosis is mediated by some unknown mechanism that has potential to slow down process of apoptosis. In accordance with this idea, significant delay between initiation of mitochondrial apoptosis and activation of caspase-activated DNAse, one of the main proteins involved in execution of mitochondrial apoptosis, after global brain ischemia has been documented previously (Tanaka et al. 2004). In addition, production of DNA fragments in CA1 layer of hippocampus was observed a few days after initial ischemia (Racay et al. 2009). On the other hand, broad spectrum caspase inhibitors reduced neuronal injury after focal but not after global brain ischemia in rats (Li et al. 2000) indicating caspase-independent mechanism of cell death after global brain ischemia. Proteins of Bcl-2 family can also regulate caspase-independent apoptosis that is characterized by slow kinetics. The ability of hippocampal neurons to die via caspase-independent apoptosis was documented after treatment of these neurones with ABT-737, antagonist of anti-apoptotic proteins Bcl-2, Bcl-xl, and Bcl-w (Young et al. 2010). Fast apoptotic neuronal death induced by ABT-737 was not prevented but it was significantly delayed by application of the broad spectrum caspase inhibitor zVADfmk (Young et al. 2010). Increased phosphorylation of Akt kinase observed in our experiments 3 h after reperfusion might represent one of the mechanisms responsible for delay of ischemic cell death. It is well known that Akt kinase pathway is controlling cellular mechanisms associated with cell survival (Aksamitiene et al. 2012). In hand with this, it has been documented that activation of the Akt kinase pathway mediates survival of vulnerable hippocampal neurons after transient global cerebral ischemia in rats (Endo et al. 2006b; Sanderson et al. 2009). In addition, enhanced activity of Akt kinase has been considered as one of the mechanisms involved in neuroprotective effects of ischemic preconditioning (García et al. 2004; Yin et al. 2005). In fact, it has been shown that ischemic preconditioning acts via PI3 K/Akt signaling to block the ischemia-induced neurodegenerative cascade involving mitochondrial translocation of Bad, interaction of Bad with Bcl-x(L), caspase activation, and neuronal death (Miyawaki et al. 2008). Thus, it seems that Akt kinase pathway is activated after ischemia; however, the ischemia-induced activation of Akt kinase is only able to delay cell death but is not able to protect vulnerable neurones from cell death.
In conclusion, our results have shown that global brain ischemia had not impact on expression of proteins of Bcl-2 family despite strong impact on mechanisms controlling expression of these proteins but was associated with significant changes in intracellular localization of Bad. Translocation of Bad to mitochondria that was observed in early periods of reperfusion might represent an important mechanism of mitochondrial apoptosis initiation associated with neuronal death induced by global brain ischemia.
Abbreviations
- ER:
-
Endoplasmic reticulum
- ERK:
-
Extracellular signal-regulated kinase
- TGBI:
-
Transient global brain ischemia
- UPS:
-
Ubiquitin-proteasome system
- Cox I:
-
Cytochrome c oxidase subunit I
- SDS–PAGE:
-
Sodium dodecyl sulfate–polyacrylamide gel electrophoresis
References
Abe T, Takagi N, Nakano M, Furuya M, Takeo S (2004) Altered Bad localization and interaction between Bad and Bcl-xL in the hippocampus after transient global ischemia. Brain Res 1009:159–168
Aksamitiene E, Kiyatkin A, Kholodenko BN (2012) Cross-talk between mitogenic Ras/MAPK and survival PI3K/Akt pathways: a fine balance. Biochem Soc Trans 40:139–146
Asai A, Tanahashi N, Qiu JH, Saito N, Chi S, Kawahara N, Tanaka K, Kirino T (2002) Selective proteasome dysfunction in the hippocampal CA1 region after transient forebrain ischemia. J Cereb Blood Flow Metab 22:705–710
Balmanno K, Cook SJ (2009) Tumour cell survival signalling by the ERK1/2 pathway. Cell Death Differ 16:368–377
Bonneau B, Prudent J, Popgeorgiev N, Gillet G (2013) Non-apoptotic roles of Bcl-2 family: the calcium connection. Biochim Biophys Acta 1833:1755–1765
Cao G, Luo Y, Nagayama T, Pei W, Stetler RA, Graham SH, Chen J (2002) Cloning and characterization of rat caspase-9: implications for a role in mediating caspase-3 activation and hippocampal cell death after transient cerebral ischemia. J Cereb Blood Flow Metab 22:534–546
Chen J, Nagayama T, Jin K, Stetler RA, Zhu RL, Graham SH, Simon RP (1998) Induction of caspase-3-like protease may mediate delayed neuronal death in the hippocampus after transient cerebral ischemia. J Neurosci 18:4914–4928
Chomova M, Tatarkova Z, Dobrota D, Racay P (2012) Ischemia-induced inhibition of mitochondrial complex I in rat brain: effect of permeabilization method and electron acceptor. Neurochem Res 37:965–976
Craxton A, Butterworth M, Harper N, Fairall L, Schwabe J, Ciechanover A, Cohen GM (2012) NOXA, a sensor of proteasome integrity, is degraded by 26S proteasomes by an ubiquitin-independent pathway that is blocked by MCL-1. Cell Death Differ 19:1424–1434
Dłuzniewska J, Beresewicz M, Wojewódzka U, Gajkowska B, Zabłocka B (2005) Transient cerebral ischemia induces delayed proapoptotic Bad translocation to mitochondria in CA1 sector of hippocampus. Brain Res Mol Brain Res 133:274–280
Duronio V (2008) The life of a cell: apoptosis regulation by the PI3K/PKB pathway. Biochem J 415:333–344
Endo H, Kamada H, Nito C, Nishi T, Chan PH (2006a) Mitochondrial translocation of p53 mediates release of cytochrome c and hippocampal CA1 neuronal death after transient global cerebral ischemia in rats. J Neurosci 26:7974–7983
Endo H, Nito C, Kamada H, Nishi T, Chan PH (2006b) Activation of the Akt/GSK3beta signaling pathway mediates survival of vulnerable hippocampal neurons after transient global cerebral ischemia in rats. J Cereb Blood Flow Metab 26:1479–1489
Fennell DA, Chacko A, Mutti L (2008) BCL-2 family regulation by the 20S proteasome inhibitor bortezomib. Oncogene 27:1189–1197
Galluzzi L, Kepp O, Trojel-Hansen C, Kroemer G (2012) Non-apoptotic functions of apoptosis-regulatory proteins. EMBO Rep 13:322–330
García L, Burda J, Hrehorovská M, Burda R, Martín ME, Salinas M (2004) Ischaemic preconditioning in the rat brain: effect on the activity of several initiation factors, Akt and extracellular signal-regulated protein kinase phosphorylation, and GRP78 and GADD34 expression. J Neurochem 88:136–147
Gardai SJ, Hildeman DA, Frankel SK, Whitlock BB, Frasch SC, Borregaard N, Marrack P, Bratton DL, Henson PM (2004) Phosphorylation of Bax Ser184 by Akt regulates its activity and apoptosis in neutrophils. J Biol Chem 279:21085–21095
Ge P, Luo Y, Liu CL, Hu B (2007) Protein aggregation and proteasome dysfunction after brain ischemia. Stroke 38:3230–3236
Green DR (2005) Apoptotic pathways: ten minutes to dead. Cell 121:671–674
Hardwick JM, Chen YB, Jonas EA (2012) Multipolar functions of BCL-2 proteins link energetics to apoptosis. Trends Cell Biol 22:318–328
Hetz C, Vitte PA, Bombrun A, Rostovtseva TK, Montessuit S, Hiver A, Schwarz MK, Church DJ, Korsmeyer SJ, Martinou JC, Antonsson B (2005) Bax channel inhibitors prevent mitochondrion-mediated apoptosis and protect neurons in a model of global brain ischemia. J Biol Chem 280:42960–42970
Inta I, Paxian S, Maegele I, Zhang W, Pizzi M, Spano P, Sarnico I, Muhammad S, Herrmann O, Inta D, Baumann B, Liou HC, Schmid RM, Schwaninger M (2006) Bim and Noxa are candidates to mediate the deleterious effect of the NF-kappa B subunit RelA in cerebral ischemia. J Neurosci 26:12896–12903
Kamikubo T, Hayashi T (1996) Changes in proteasome activity following transient ischemia. Neurochem Int 28:209–212
Kato H, Chen T, Liu XH, Nakata N, Kogure K (1993) Immunohistochemical localization of ubiquitin in gerbil hippocampus with induced tolerance to ischemia. Brain Res 619:339–343
Kirino T (2000) Delayed neuronal death. Neuropathology 20:S95–S97
Krajewski S, Krajewska M, Shabaik A, Wang HG, Irie S, Fong L, Reed JC (1994) Immunohistochemical analysis of in vivo patterns of Bcl-X expression. Cancer Res 54:5501–5507
Krajewski S, Mai JK, Krajewska M, Sikorska M, Mossakowski MJ, Reed JC (1995a) Upregulation of bax protein levels in neurons following cerebral ischemia. J Neurosci 15:6364–6376
Krajewski S, Bodrug S, Krajewska M, Shabaik A, Gascoyne R, Berean K, Reed JC (1995b) Immunohistochemical analysis of Mcl-1 protein in human tissues. Differential regulation of Mcl-1 and Bcl-2 protein production suggests a unique role for Mcl-1 in control of programmed cell death in vivo. Am J Pathol 146:1309–1319
Krajewski S, Krajewska M, Ellerby LM, Welsh K, Xie Y, Deveraux OL, Salvesen GS, Bredesen DE, Rosenthal RE, Fiskum G, Reed JC (1999) Release of caspase-9 from mitochondria during neuronal apoptosis and cerebral ischemia. Proc Natl Acad Sci USA 96:5752–5757
Lein ES, Zhao X, Gage FH (2004) Defining a molecular atlas of the hippocampus using DNA microarrays and high-throughput in situ hybridization. J Neurosci 24:3879–3889
Li H, Colbourne F, Sun P, Zhao Z, Buchan AM (2000) Caspase inhibitors reduce neuronal injury after focal but not global cerebral ischemia in rats. Stroke 31:176–182
Lindsay J, Esposti MD, Gilmore AP (2011) Bcl-2 proteins and mitochondria–specificity in membrane targeting for death. Biochim Biophys Acta 1813:532–539
Lipton P (1999) Ischemic cell death in brain neurons. Physiol Rev 79:1431–1568
Miyawaki T, Mashiko T, Ofengeim D, Flannery RJ, Noh KM, Fujisawa S, Bonanni L, Bennett MV, Zukin RS, Jonas EA (2008) Ischemic preconditioning blocks BAD translocation, Bcl-xL cleavage, and large channel activity in mitochondria of postischemic hippocampal neurons. Proc Natl Acad Sci USA 105:4892–4897
Morimoto T, Ide T, Ihara Y, Tamura A, Kirino T (1996) Transient ischemia depletes free ubiquitin in the gerbil hippocampal CA1 neurons. Am J Pathol 148:249–257
Motoyama N, Wang F, Roth KA, Sawa H, Nakayama K, Negishi I, Senju S, Zhang Q, Fujii S (1995) Massive cell death of immature hematopoietic cells and neurons in Bcl-x-deficient mice. Science 267:1506–1510
Nakka VP, Gusain A, Mehta SL, Raghubir R (2008) Molecular mechanisms of apoptosis in cerebral ischemia: multiple neuroprotective opportunities. Mol Neurobiol 37:7–38
Niizuma K, Endo H, Nito C, Myer DJ, Chan PH (2009) Potential role of PUMA in delayed death of hippocampal CA1 neurons after transient global cerebral ischemia. Stroke 40:618–625
Niizuma K, Yoshioka H, Chen H, Kim GS, Jung JE, Katsu M, Okami N, Chan PH (2010) Mitochondrial and apoptotic neuronal death signaling pathways in cerebral ischemia. Biochim Biophys Acta 1802:92–99
Perez-Pinzon MA, Xu GP, Born J, Lorenyo J, Busto R, Rosenthal M, Sick TJ (1999) Cytochrome C is released from mitochondria into the cytosol after cerebral anoxia or ischemia. J Cereb Blood Flow Metab 19:39–43
Pulsinelli WA, Brierley JB (1979) A new model of bilateral hemispheric ischemia in the unanesthetized rat. Stroke 10:267–272
Racay P (2012) Ischaemia-induced protein ubiquitinylation is differentially accompanied with heat-shock protein 70 expression after naïve and preconditioned ischaemia. Cell Mol Neurobiol 32:107–119
Racay P, Tatarkova Z, Drgova A, Kaplan P, Dobrota D (2007) Effect of ischemic preconditioning on mitochondrial dysfunction and mitochondrial p53 translocation after transient global cerebral ischemia in rats. Neurochem Res 32:1823–1832
Racay P, Chomova M, Tatarkova Z, Kaplan P, Hatok J, Dobrota D (2009) Ischemia-induced mitochondrial apoptosis is significantly attenuated by ischemic preconditioning. Cell Mol Neurobiol 29:901–908
Rodriguez D, Rojas-Rivera D, Hetz C (2011) Integrating stress signals at the endoplasmic reticulum: the BCL-2 protein family rheostat. Biochim Biophys Acta 1813:564–574
Sanderson TH, Kumar R, Murariu-Dobrin AC, Page AB, Krause GS, Sullivan JM (2009) Insulin activates the PI3K-Akt survival pathway in vulnerable neurons following global brain ischemia. Neurol Res 31:947–958
Sawe N, Steinberg G, Zhao H (2008) Dual roles of the MAPK/ERK1/2 cell signaling pathway after stroke. J Neurosci Res 86:1659–1669
Sugawara T, Fujimura M, Morita-Fujimura Y, Kawase M, Chan PH (1999) Mitochondrial release of cytochrome c corresponds to the selective vulnerability of hippocampal CA1 neurons in rats after transient global cerebral ischemia. J Neurosci 19:1–6
Sun YF, Yu LY, Saarma M, Timmusk T, Arumae U (2001) Neuron-specific Bcl-2 homology 3 domain-only splice variant of Bak is anti-apoptotic in neurons, but pro-apoptotic in non-neuronal cells. J Biol Chem 276:16240–16270
Szegezdi E, Macdonald DC, Ní Chonghaile T, Gupta S, Samali A (2009) Bcl-2 family on guard at the ER. Am J Physiol Cell Physiol 296:C941–C953
Tanaka H, Yokota H, Jover T, Cappuccio I, Calderone A, Simionescu M, Bennett MV, Zukin RS (2004) Ischemic preconditioning: neuronal survival in the face of caspase-3 activation. J Neurosci 24:2750–2759
Taylor RC, Cullen SP, Martin SJ (2008) Apoptosis: controlled demolition at the cellular level. Nat Rev Mol Cell Biol 9:231–241
Tsuchiya T, Bonner HP, Engel T, Woods I, Matsushima S, Ward MW, Taki W, Henshall DC, Concannon CG, Prehn JH (2011) Bcl-2 homology domain 3-only proteins Puma and Bim mediate the vulnerability of CA1 hippocampal neurons to proteasome inhibition in vivo. Eur J Neurosci 33:401–408
Tsuruta F, Masuyama N, Gotoh Y (2002) The phosphatidylinositol 3-kinase (PI3 K)-Akt pathway suppresses Bax translocation to mitochondria. J Biol Chem 277:14040–14047
Yang E, Zha J, Jockel J, Boise LH, Thompson CB, Korsmeyer SJ (1995) Bad, a heterodimeric partner for Bcl-XL and Bcl-2, displaces Bax and promotes cell death. Cell 80:285–291
Yin XH, Zhang QG, Miao B, Zhang GY (2005) Neuroprotective effects of preconditioning ischaemia on ischaemic brain injury through inhibition of mixed-lineage kinase 3 via NMDA receptor-mediated Akt1 activation. J Neurochem 93:1021–1029
Youle RJ, Strasser A (2008) The BCL-2 protein family: opposing activities that mediate cell death. Nat Rev Mol Cell Biol 9:47–59
Young KW, Piñón LG, Dhiraj D, Twiddy D, Macfarlane M, Hickman J, Nicotera P (2010) Mitochondrial fragmentation and neuronal cell death in response to the Bcl-2/Bcl-x(L)/Bcl-w antagonist ABT-737. Neuropharmacology 58:1258–1267
Acknowledgments
This work was supported by the Agency for Support of Science and Development of Slovak Republic (Grant APVV-0245-11 to P.R.).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pilchova, I., Klacanova, K., Chomova, M. et al. Possible Contribution of Proteins of Bcl-2 Family in Neuronal Death Following Transient Global Brain Ischemia. Cell Mol Neurobiol 35, 23–31 (2015). https://doi.org/10.1007/s10571-014-0104-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10571-014-0104-3