Abstract
Mesenchymal stem cells (MSC) have emerged as a new therapeutic tool for a number of clinical applications, because they have multipotency and paracrine effects via various factors. In the present study, we investigated the effects of adipose-derived MSC (Ad-MSC) transplantation via intrathecal injection through the cisterna magna on cell proliferation and differentiation of endogenous stem cells in the hippocampal dentate gyrus (DG) using Ki-67 (a marker for proliferating cells), and doublecortin (DCX, a marker for neuroblasts). The transplanted Ad-MSC were detected in the meninges, not in the hippocampal parenchyma. However, the number of Ki-67-immunoreactive cells was significantly increased by 83% in the DG 2 days after single Ad-MSC injection, and by 67% at 23 days after repeated Ad-MSC treatment compared with that in the vehicle-treated group after Ad-MSC transplantation. On the other hand, the number of DCX-immunoreactive cells in the DG was not changed at 2 days after single Ad-MSC injection; however, it was significantly increased by 62% 9 days after single Ad-MSC injection. At 23 days after repeated Ad-MSC application, the number of DCX-immunoreactive cells was much more increased (223% of the vehicle-treated group). At this time point, DCX protein levels were also significantly increased compared with those in the vehicle-treated group. These results suggest that the intrathecal injection of Ad-MSC could enhance endogenous cell proliferation, and the repeated Ad-MSC injection could be more efficient for an enhancement of endogenous cell proliferation and differentiation in the brain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mesenchymal stem cells (MSC), also termed multipotent mesenchymal stromal cells, are a phenotypically and functionally heterogeneous cell population which has been traditionally isolated from the bone marrow (Horwitz et al. 2005; Dominici et al. 2006; Yang et al. 2009). Recent reports have detailed the isolation of cells with MSC characteristics from a variety of tissues including cord blood, peripheral blood, fetal liver and lung, adipose tissue, skeletal muscle, amniotic fluid, and synovium (Erices et al. 2000; Campagnoli et al. 2001; Liu et al. 2009).
MSC have emerged as a new cell source of therapy, because they possess multipotency and can be easily expanded in culture (Erices et al. 2000; Caterson et al. 2001; Ito et al. 2001; Cheng et al. 2003; Pavlichenko et al. 2008; Komatsu et al. 2010). Indeed, these cells have differential capacities as well as paracrine effects via the secretion of growth factors, cytokines, antifibrotic, or angiogenic mediators (Kinnaird et al. 2004a; Gnecchi et al. 2008). It has been reported that exogenous cell transplantation enhances endogenous cell proliferation and neurogenesis as well as repairing process in the CNS (Mahmood et al. 2004; Madhavan et al. 2009; van Velthoven et al. 2010).
There are some distinct regions of active proliferation in adult mammalian brains, which are known to continuously generate neurons throughout life (Picard-Riera et al. 2004). The hippocampal dentate gyrus (DG) is one of the neurogenic sites in the adult brain (Gould et al. 1997; Kempermann et al. 1997). Newly generated cells in the subgranular zone (SGZ) of the DG can proliferate, migrate, and differentiate finally into neurons termed granule cells, which extend axonal and dendritic projections and establish new synaptic connections to the existing hippocampal circuitry (Ramirez-Amaya et al. 2006; Kee et al. 2007).
Neurogenesis is a dynamic process that is positively and negatively regulated by environmental, endocrine, and pharmacological stimuli (Bain et al. 2004; Terada et al. 2008; Veena et al. 2009). Secretive properties of MSC may be mainly influenced by local microenvironments (Kinnaird et al. 2004a). Recent reports have revealed that MSC undergoing hypoxia environment or gene manipulation in vitro can produce several cytokines such as insulin-like growth factor-1, vascular endothelial growth factor, and hepatocyte growth factor, which are capable of promoting the survival of surrounding cells via paracrine mechanisms (Kinnaird et al. 2004a; Dominici et al. 2006).
It has been attempted to deliver drug and cells to the CNS by intrathecal route (Hylden and Wilcox 1980; Taiwo et al. 2005). The intrathecal application improves the transplant of MSC in some neurodegenerative diseases (Habisch et al. 2007; Morita et al. 2008), because the application avoids some brain damage produced by a needle or cannula, which is known to induce expression of stem cell factors (Sun et al. 2004). In addition, the intrathecal injection of bone marrow stromal cells shows some therapeutic benefit without any marked adverse effect in clinical trial (Saito et al. 2008).
Stem cell therapy is one of major topic in the veterinary field (Fortier and Travis 2011). Experimental and clinical stem cell trials on various diseases such as diabetes, arthritis, and spinal cord injury have been increased in the veterinary field using MSCs (Minguell et al. 2010; Fortier and Travis 2011; Lee et al. 2011; Zhu et al. 2011). Recently, some benefit and therapeutic effects of adipose tissue derived-MSC (Ad-MSC) from the dog have been reported (Neupane et al. 2008; Vieira et al. 2010). In the present study, therefore, we investigated the effects of intrathecal Ad-MSC transplantation on cell proliferation and neuroblast differentiation in the SGZ of the DG of normal rats.
Materials and Methods
Experimental Animals
Twelve-week-old male Wistar rats were purchased from Orient Bio Inc. (Seongnam, South Korea). They were housed in a conventional state under adequate temperature (23°C) and humidity (60%) vehicle with a 12-h light/12-h dark cycle, and free access to food and water. The procedures for handling and caring for the animals adhered to the guidelines that are in compliance with the current international laws and policies (NIH Guide for the Care and Use of Laboratory Animals, NIH Publication No. 85-23, 1985, revised 1996). All of the experiments were conducted to minimize the number of animals used and the suffering caused by the procedures used in the present study, and they were approved by the Institutional Animal Care and Use Committee (IACUC) at Seoul National University.
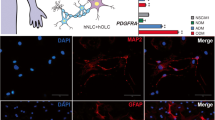
Cell Preparation
Canine Ad-MSC (RNLBio, Seoul Korea) was maintained in Dulbecco’s Minimum Essential Medium (DMEM: Hyclone, VT, USA) supplemented with 10% fetal bovine serum (Hyclone), and penicillin (100 U/ml), streptomycin (100 μg/ml). All the cell cultures were maintained at 37°C in a humidified 5% CO2/air atmosphere. For the labeling of the Ad-MSC, CM-DiI (Invitrogen, Carlsbad, CA, USA) was used before their injection, which is a lipophilic fluorescent dye that binds irreversibly to the cell membrane and is not transferable to other cells. Images of CM-DiI-labeled Ad-MSC was taken through an inverted fluorescence microscope (IX 71, Olympus, Japan) equipped with a digital camera (DP71, Olympus) (Supplementary Fig. 1).
Surgical Procedure for Cell Transplantation
The animals were divided into four groups; single vehicle-treated group (vehicle-group, n = 30), single Ad-MSCs-treated group (Ad-MSC group, n = 30), four times (once a week) vehicle-treated group (Four vehicle-group, n = 10), and four times (once a week) Ad-MSC-treated group (Four Ad-MSC-group, n = 10). The animals that received a single injection were sacrificed at 2, 9, and 23 days after the single injection, and the animals that received four times injection a week were sacrificed at 2 days after the last injection. The Ad-MSC (2 × 106) suspended in 5 μl phosphate-buffered saline (PBS) were transplanted intrathecally into the cisterna magna. Same volume of vehicle (PBS) was injected in the same way of Ad-MSC treatment. The technique of intrathecal injection was used by previously reported (Habisch et al. 2007). In brief, the back around the site of intrathecal injection was shaved, wiped with alcohol, and allowed to dry. A needle (gauge 30, Hamilton, Point Style 4) was positioned over the midline of the atlanto-occipital membrane to form an angle of 60 degrees with the horizontal line. There were no obvious behavioral sequelae (e.g., locomotor, feeding, or drinking) due to chronic intrathecal injections at either volume used.
Tissue Processing for Histology
The animals in each group were sacrificed at 2, 9, and 23 days after the last injection. For histology, the animals (n = 5 each group) were anesthetized with 1 g/kg urethane (Sigma, St. Louis, MO). They were, then, perfused transcardially with 0.1 M PBS (pH 7.4) followed by 4% paraformaldehyde in 0.1 M phosphate-buffer (PB, pH 7.4). The brains were removed and postfixed in the same fixative for 6 h. The brain tissues were cryoprotected by infiltration with 30% sucrose overnight. Thereafter, frozen tissues were serially sectioned on a cryostat (Leica, Wetzlar, Germany) into 30 μm coronal sections, and then, the sections were collected into six-well plates containing PBS.
Migration of Ad-MSC into the Brain Parenchyma
To identify migration of transplanted Ad-MSC into hippocampal parenchyma, ten sections per animals were selected from the corresponding area (Bregma −3 ~−4.08 mm of rat brain atlas) (Paxinos and Watson 2005). The sections were mounted on gelatin-coated slides with 4,6-diamidino-2-phenylindole, dihydrochloride (DAPI, a cell marker) containing mount medium (Vector) to identify the nuclei of the cells, and we examined under LSM 510 META NLO confocal microscope (Carl Zeiss, Göttingen, Germany). A series of high magnification images was collected at 0.7 μm intervals with excitation by 488, 770 nm lasers and bright field light to create a stack in the Z axis.
Immunohistochemistry
To obtain the accurate data for Ki-67 (a marker for proliferating cells) and DCX (a marker of neuroblasts) immunoreaction, the sections from vehicle- and Ad-MSC-groups were used at designated times under the same conditions. The sections were sequentially treated with 0.3% hydrogen peroxide (H2O2) in PBS for 30 min and 10% normal horse serum in 0.05 M PBS for 30 min. They were then incubated with diluted rabbit anti-Ki67 antibody (1:1,000, Abcam, Cambridge, UK) or goat anti-DCX antibody (1:50, Santa Cruz Biotechnology, Santa Cruz, CA) overnight at 4°C and subsequently exposed to biotinylated rabbit anti-goat IgG (diluted 1:200, Vector, Burlingame, CA) for anti-DCX and goat anti-rabbit IgG (diluted 1:200, Vector) for anti-Ki-67. The sections were, then, exposed to streptavidin peroxidase complex (diluted 1:200, Vector), and visualized with reaction to 3,3′-diaminobenzidine tetrachloride (Sigma) in 0.1 M Tris–HCl buffer (pH 7.2) and mounted on gelatin-coated slides. A negative vehicle test was carried out using pre-immune serum instead of primary antibody to establish the specificity of the immunostaining.
In order to quantitatively analyze Ki-67- and DCX-immunoreactive cell numbers, 15 sections per each animal were selected corresponding to Bregma −3 ~ −4.08 mm of rat brain atlas (Paxinos and Watson 2005). Images of all Ki-67 and DCX-immunoreactive structures were taken from three layers (molecular, granule cell, and polymorphic layers) through a light microscope (Olympus, Japan) equipped with a digital camera (DP71, Olympus, Japan) connected to a PC monitor. The number of DCX- and Ki-67 positive cells in the SGZ was counted by Optimas 6.5 software (CyberMetrics, Scottsdale, AZ). Cell counts were obtained by averaging the counts from the sections taken from each animal: A ratio of the count was calibrated as percent.
Western Blot Analysis
To confirm changes in the DCX levels in the DG of rats, five animals in each group were sacrificed and used for western blot analysis. After sacrificing them and removing the hippocampus, it was serially and transversely cut into 400 μm thickness on a vibratome (Leica, Wetzlar, Germany), and the DG was dissected with a surgical blade. The tissues were homogenized in 50 mM PBS (pH 7.4) containing 0.1 mM ethylene glycol bis(2-aminoethyl ether)-N,N,N′,N′ tetraacetic acid (EGTA) (pH 8.0), 0.2% nonidet P-40, 10 mM ethylenediamine tetraacetic acid (EDTA) (pH 8.0), 15 mM sodium pyrophosphate, 100 mM β-glycerophosphate, 50 mM NaF, 150 mM NaCl, 2 mM sodium orthovanadate, 1 mM phenylmethylsulfonyl fluoride (PMSF), and 1 mM dithiothreitol (DTT). After centrifugation, the protein level was determined in supernatants using a Micro BCA protein assay kit with bovine serum albumin as the standard (Pierce Chemical, Rockford, IL). Aliquots containing 50 μg of total protein were boiled in loading buffer containing 150 mM Tris (pH 6.8), 3 mM DTT, 6% SDS, 0.3% bromophenol blue, and 30% glycerol. Then, each aliquot was loaded onto a 10% polyacrylamide gel. After electrophoresis, the gels were transferred to nitrocellulose transfer membranes (Pall Crop, East Hills, NY). To reduce background staining, the membranes were incubated with 5% non-fat dry milk in PBS containing 0.1% Tween 20 for 45 min. The membranes were, then, incubated with goat anti-DCX antibody (1:100) or mouse anti-beta actin antibody (1:2,000, Sigma), and peroxidase-conjugated rabbit anti-goat IgG (Sigma) for DCX or peroxidase-conjugated goat anti-mouse IgG (Sigma) for beta actin and an ECL kit (Pierce Chemical). The result of the western blot analysis was scanned, and densitometric analysis for the quantification of the bands was done using Scion Image software (Scion Corp., Frederick, MD), which was employed to count relative optical density (ROD). DCX protein levels were normalized by the corresponding beta-actin protein level: A ratio of the ROD was calibrated as %, with 2d-vehicle-treated group designated as 100%.
Statistical Analysis
Data are expressed as the mean ± SEM. Differences among the means were statistically analyzed by one-way ANOVA followed by Duncan’s new multiple range method. Differences among the means were statistically analyzed by two-way ANOVA with treatment times and days as the two factors to elucidate differences between the 2d Ad-MSC and 4 Ad-MSC groups. Statistical significance was considered at P < 0.05.
Results
Migration of Ad-MSC into the Brain Parenchyma
To investigate the migration of transplanted Ad-MSC into the brain parenchyma, we examined the brain tissue directly under a fluorescence microscope (Supplementary Fig. 2). No CM-DiI-labeled Ad-MSC were observed in the brain parenchyma and the ventricular system in the brain after Ad-MSC. However, abundant CM-DiI-labeled Ad-MSC were observed in the subarachnoid region in the diencephalon, midbrain, cerebellum, medulla oblongata, and spinal cord (Supplementary Fig. 2 and Fig. 1).
Fluorescence detection of CM-DiI-labeled Ad-MSC in the cerebellum (a–h) and the medulla oblongata (i–p) 23 days after Ad-MSC transplantation. Low magnification photos of the engrafted CM-DiI-labeled Ad-MSC (red, a, i), the cerebellum and medulla oblongata (bright field, b, j). High magnification photos of box in panel c (d–g) and k (l–o): DAPI-(a marker for nucleus) stained cells (blue, d, l), CM-DiI-labeled Ad-MSC (red, e, m) and brain structures (bright field, f, n). Three dimensional orthogonal views (h, p) of white box in panel c and k show double-labeled Ad-MSC with DAPI. Green line (x axis) and red line (y axis), and the blue line represents the position of the central panel image in the z stack (h and p). Bar = 350 μm (a–c), 25 μm (d–h), 500 μm (i–k), 20 μm (l–p) (Color figure online)
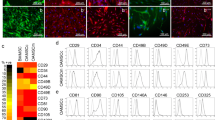
Effects of Ad-MSC Transplantation on Cell Proliferation
In the vehicle-groups, a few Ki-67-immunoreactive cells were detected in the SGZ of the DG (Fig. 2a, c, e, g). The number of Ki-67-immunoreactive cells was not changed after 9 and 23 days after the vehicle injection (Figs. 2c, e, g, 3).
Immunohistochemical staining for Ki-67 in the vehicle- (a, c, e, g) and Ad-MSC-groups (b, d, f, h). In the vehicle-group, Ki-67-immunoreactive cells are detected in the SGZ of the DG (a, b). Ki-67-immunoreactive cells are increased 2 days after Ad-MSC transplantation (b, h). Arrows indicate Ki-67-immunoreactive cells (a–h). GCL granule cell layer; ML molecular layer; PoL polymorphic layer. Bar 200 μm
Relative number of Ki-67-immunoreactive cells in the DG of the vehicle- and Ad-MSC-group (n = 5 per group; *P < 0.05, significantly different from the corresponding vehicle-group, # P < 0.05, significantly different from the 2d-Ad-MSC-group, † P < 0.05, significantly different from the 23d single-Ad-MSC-group). Data are expressed as the means ± SEM
In the single-Ad-MSC-group, the number of Ki-67-immunoreactive cells was significantly increased by 83% 2 days after MSC injection compared with that in the vehicle-group in the SGZ (Figs. 2b, 3). However, in this group, the number of Ki-67-immunoreactive cells was similar to that in the vehicle-group 9 and 23 days after Ad-MSC injection (Figs. 2d, f, 3).
Twenty-three days after Ad-MSC transplantation, in the four Ad-MSC-groups, Ki-67-immunoreactive cells were also observed in the SGZ of the DG (Fig. 2h). The number of Ki-67-immunoreactive cells was similar to that in the 2d-Ad-MSC-group, and the number of the cells was increased by 67% compared with that in the vehicle-group (Fig. 3).
Effects of Ad-MSC Transplantation on Neuroblasts
In the vehicle-groups, many doublecortin (DCX)-immunoreactive neuroblasts were easily detected in the SGZ of the DG (Fig. 4a, b, e, f, i, j, m, n). They had well-developed processes which extended into the molecular layer. In the vehicle-groups, the number of DCX-immunoreactive cells was not changed 9 and 23 days after the vehicle injection (Figs. 4e, f, i, j, m, n, 5).
Immunohistochemistry for DCX in the vehicle- (a, b, e, f, i, j, m, n) and Ad-MSC-groups (c, d, g, h, k, l, o, p). In the vehicle-groups, DCX-immunoreactive cells are not changed with time. DCX-immunoreactive cells at 2 days after Ad-MSC transplantation is similar to the vehicle-group; however, DCX-immunoreactive cells are markedly increased 9 and 23 days after Ad-MSC injection. GCL, granule cell layer; ML, molecular layer; PoL, polymorphic layer. Bar = 200 μm (a, c, e, g, i, k, m, o), 50 μm (b, d, f, h, j, l, n, p)
Relative number of DCX-immunoreactive neuroblasts in the DG of the vehicle- and Ad-MSC-groups (n = 5 per group; *P < 0.05, significantly different from the vehicle-group at the same time point, # P < 0.05, significantly different from the 2d-Ad-MSC-group, † P < 0.05, significantly different from the 23d single-Ad-MSC-group). Data are expressed as the means ± SEM
In the single-Ad-MSC-group, DCX-immunoreactive cells were also observed in the SGZ (Fig. 4c, d, g, h, k, l). Two days after single Ad-MSC transplantation, the number of DCX-immunoreactive cells was similar to that in the vehicle-group (Figs. 4c, d, 5); however, DCX-immunoreactive cells were significantly increased (162 and 147% of the vehicle-group, respectively) 9 and 23 days after single Ad-MSC injection (Figs. 4g, h, k, l, 5). Twenty-three days in the four Ad-MSC-group, a distinctive increase of DCX-immunoreactive cells, which had strong DCX immunoreactivity in their somata and processes, was observed in the SGZ of the DG (Fig. 4o, p): the number of DCX-immunoreactive cells was markedly increased (223% of the vehicle-group) compared with that in the single-Ad-MSC-group (Fig. 5).
Effects of Ad-MSC Transplantation on DCX Protein Levels
We found that the results of western blot analysis in the DG of the vehicle- and Ad-MSC-groups were similar to the pattern of immunohistochemical change: DCX protein levels in the homogenates were not changed 2 days after Ad-MSC transplantation; however, DCX protein levels at 9 and 23 days after Ad-MSC-injection were significantly increased (163 and 160% of the vehicle-group, respectively) compared with the vehicle-group (Fig. 6). In addition, DCX protein levels in the four Ad-MSC-group were much more increased (257% of the vehicle-group) compared with that in the single Ad-MSC-group (Fig. 6).
Western blot analysis of DCX in the DG of the vehicle- and Ad-MSC-groups. Relative optical density (ROD) as % of immunoblot band is also represented (n = 5 per group; *P < 0.05, significantly different from the corresponding vehicle-group, # P < 0.05, significantly different from the 2d-Ad-MSC-group, † P < 0.05, significantly different from the 23d single-Ad-MSC-group). The bars indicate the means ± SEM
Discussion
In this study, we investigated the changes in cell proliferation and neuroblast differentiation in the rat DG after the intrathecal Ad-MSC transplantation. We did not find any Ad-MSC in the parenchyma of the hippocampus and in the ventricle around the hippocampus after the intrathecal transplantation via the cisterna magna. However, we found abundant Ad-MSC in the subarachnoid space in the diencephalon, midbrain, medulla oblongata, and spinal cord. This finding is not consistent with previous studies that intrathecally transplanted various stem cells migrated into the parenchyma in some CNS disease models, such as animal models of amyotrophic lateral sclerosis, traumatic brain, and ischemic spinal cord injury (Lepore et al. 2005; Habisch et al. 2007; Liu et al. 2008; Kim et al. 2010). The difference in the distribution and migration of the transplanted stem cells may be associated with conditions of the brain, e.g., intact or damaged brain because the migration of transplanted stem cells is influenced by various factors, such as cell death and inflammatory cytokines under a disease condition (Sugaya 2003; Nervi et al. 2006; Newby 2006). However, under the normal condition, transplanted stem cells have a limited and non-targeted migration as well as differentiation in the brain and other tissue organs (Shear et al. 2004; Canola et al. 2007; Guzman et al. 2008).
Adult neurogenesis continues in the DG of the adult (Kuhn et al. 1996; Ramirez-Amaya et al. 2006). Ki-67 is an endogenous marker for cell proliferation in the initial phase of adult neurogenesis because Ki-67 is expressed during mitosis in all mammalian species from rodents to humans (Kee et al. 2002; Lagace et al. 2010). In the present study, we observed many Ki-67 positive cells in the DG of the vehicle-treated group. A significant increase in the number of Ki-67-immunoreactive cells was found 2 days after the single Ad-MSC treatment and 23 days after the repeated Ad-MSC treatment. It was reported that MSC transplantation into an injured region induced by an ischemia enhanced endogenous cell proliferation and repair processing (van Velthoven et al. 2010).
The DCX is expressed in migrating neuroblasts and immature neurons during development. Hence, DCX can be employed to label the cell bodies, processes and growth cones of newborn neurons (Nacher et al. 2001; Couillard-Despres et al. 2005). Therefore, an increase of DCX-immunoreactive cells may reflect that newly generated cells differentiate into neuroblasts. In the present study, we found that significant increases in DCX-immunoreactive cells and protein levels were also observed in the DG 9 days after the single Ad-MSC transplantation and 23 days after the repeated Ad-MSC transplantation compared withthose in the vehicle-group. We also observed that DCX-immunoreactive cells and protein levels in the four Ad-MSC- group were higher than those in the single-Ad-MSC-group. These results are consistent with previous articles that reported that repeated MSC injection was much more effective than single MSC injection in some brain and heart disease models (Poh et al. 2007; Diederichsen et al. 2008; van Velthoven et al. 2010).
In the present study, the number of Ki-67-immunoreactive cells was significantly increased 2 days after the single Ad-MSC administration, but DCX-immunoreactive cells were increased much later after the Ad-MSC administration. This delayed increase of the DCX-immunoreactive cells may be related with the different expression time points of the protein during neurogenesis: Ki-67 is expressed in neural precursor cells during mitosis; however, DCX is shortly expressed after exiting the cell cycle, and the expression continues for 2–3 weeks (Scholzen and Gerdes 2000; Kee et al. 2002; Couillard-Despres et al. 2005).
On the other hand, we found that increases in Ki-67-immunoreactive cells and DCX-immunoreactive neuroblasts in the DG after the intrathecal Ad-MSC administration, although the Ad-MSC did not migrate into the hippocampal parenchyma. This effect may be associated with the paracrine effect of the Ad-MSC, which migrated into the meninges of the brain after the transplantation. It was reported that intrathecal stem cell transplantation led to an increase of pre-symptomatic motor performance in the ALS mice with a limited migration of transplanted stem cells into the brain parenchyma and a very low survival rate (Habisch et al. 2007; Kim et al. 2010). In addition, emerging evidences suggest that MSC regulates the survival, migration, and differentiation of endogenous stem cells through the production of growth factors, chemokines, and extracellular matrix molecules (Kinnaird et al. 2004a, b; Prockop 2007).
In conclusion, our results indicate that the intrathecal Ad-MSC administration could enhance endogenous cell proliferation in the DG. In addition, the repeated Ad-MSC injection could be more beneficial for the enhancement of endogenous stem cell proliferation in the DG.
References
Bain MJ, Dwyer SM, Rusak B (2004) Restraint stress affects hippocampal cell proliferation differently in rats and mice. Neurosci Lett 368:7–10
Campagnoli C, Roberts IA, Kumar S, Bennett PR, Bellantuono I, Fisk NM (2001) Identification of mesenchymal stem/progenitor cells in human first-trimester fetal blood, liver, and bone marrow. Blood 98:2396–2402
Canola K, Angenieux B, Tekaya M, Quiambao A, Naash MI, Munier FL, Schorderet DF, Arsenijevic Y (2007) Retinal stem cells transplanted into models of late stages of retinitis pigmentosa preferentially adopt a glial or a retinal ganglion cell fate. Invest Ophthalmol Vis Sci 48:446–454
Caterson EJ, Nesti LJ, Albert T, Danielson K, Tuan R (2001) Application of mesenchymal stem cells in the regeneration of musculoskeletal tissues. MedGenMed 3(1):E1
Cheng FJ, Zou P, Zhong ZD, Guo R, Xiao J (2003) The growth characteristics of mesenchymal stem/progenitor cells in human umbilical cord blood. Zhongguo Shi Yan Xue Ye Xue Za Zhi 11:565–568
Couillard-Despres S, Winner B, Schaubeck S, Aigner R, Vroemen M, Weidner N, Bogdahn U, Winkler J, Kuhn HG, Aigner L (2005) Doublecortin expression levels in adult brain reflect neurogenesis. Eur J Neurosci 21:1–14
Diederichsen AC, Møller JE, Thayssen P, Junker AB, Videbaek L, Saekmose SG, Barington T, Kristiansen M, Kassem M (2008) Effect of repeated intracoronary injection of bone marrow cells in patients with ischaemic heart failure the Danish stem cell study—congestive heart failure trial (DanCell-CHF). Eur J Heart Fail 10:661–667
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop D, Horwitz E (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for cellular therapy position statement. Cytotherapy 8:315–317
Erices A, Conget P, Minguell JJ (2000) Mesenchymal progenitor cells in human umbilical cord blood. Br J Haematol 109:235–242
Fortier LA, Travis AJ (2011) Stem cells in veterinary medicine. Stem Cell Res Ther 2:9
Gnecchi M, Zhang Z, Ni A, Dzau VJ (2008) Paracrine mechanisms in adult stem cell signaling and therapy. Circ Res 103:1204–1219
Gould E, McEwen BS, Tanapat P, Galea LA, Fuchs E (1997) Neurogenesis in the dentate gyrus of the adult tree shrew is regulated by psychosocial stress and NMDA receptor activation. J Neurosci 17:2492–2498
Guzman R, Bliss T, De Los Angeles A, Moseley M, Palmer T, Steinberg G (2008) Neural progenitor cells transplanted into the uninjured brain undergo targeted migration after stroke onset. J Neurosci Res 86:873–882
Habisch HJ, Janowski M, Binder D, Kuzma-Kozakiewicz M, Widmann A, Habich A, Schwalenstöcker B, Hermann A, Brenner R, Lukomska B, Domanska-Janik K, Ludolph AC, Storch A (2007) Intrathecal application of neuroectodermally converted stem cells into a mouse model of ALS: limited intraparenchymal migration and survival narrows therapeutic effects. J Neural Transm 114:1395–1406
Horwitz EM, Le Blanc K, Dominici M, Mueller I, Slaper-Cortenbach I, Marini FC, Deans RJ, Krause DS, Keating A (2005) Clarification of the nomenclature for MSC: The International Society for cellular therapy position statement. Cytotherapy 7:393–395
Hylden JL, Wilcox GL (1980) Intrathecal morphine in mice: a new technique. Eur J Pharmacol 67:313–316
Ito T, Suzuki A, Okabe M, Imai E, Hori M (2001) Application of bone marrow-derived stem cells in experimental nephrology. Exp Nephrol 9:444–450
Kee N, Sivalingam S, Boonstra R, Wojtowicz JM (2002) The utility of Ki-67 and BrdU as proliferative markers of adult neurogenesis. J Neurosci Methods 115:97–105
Kee N, Teixeira CM, Wang AH, Frankland PW (2007) Preferential incorporation of adult-generated granule cells into spatial memory networks in the dentate gyrus. Nat Neurosci 10:355–362
Kempermann G, Kuhn HG, Gage FH (1997) Genetic influence on neurogenesis in the dentate gyrus of adult mice. Proc Natl Acad Sci USA 94:10409–10414
Kim H, Kim HY, Choi MR, Hwang S, Nam KH, Kim HC, Han JS, Kim KS, Yoon HS, Kim SH (2010) Dose-dependent efficacy of ALS-human mesenchymal stem cells transplantation into cisterna magna in SOD1–G93A ALS mice. Neurosci Lett 468:190–194
Kinnaird T, Stabile E, Burnett MS, Lee CW, Barr S, Fuchs S, Epstein SE (2004a) Marrow-derived stromal cells express genes encoding a broad spectrum of arteriogenic cytokines and promote in vitro and in vivo arteriogenesis through paracrine mechanisms. Circ Res 94:678–685
Kinnaird T, Stabile E, Burnett MS, Shou M, Lee CW, Barr S, Fuchs S, Epstein SE (2004b) Local delivery of marrow-derived stromal cells augments collateral perfusion through paracrine mechanisms. Circulation 109:1543–1549
Komatsu K, Honmou O, Suzuki J, Houkin K, Hamada H, Kocsis JD (2010) Therapeutic time window of mesenchymal stem cells derived from bone marrow after cerebral ischemia. Brain Res 1334:84–92
Kuhn HG, Dickinson-Anson H, Gage FH (1996) Neurogenesis in the dentate gyrus of the adult rat: age-related decrease of neuronal progenitor proliferation. J Neurosci 16:2027–2033
Lagace DC, Donovan MH, DeCarolis NA, Farnbauch LA, Malhotra S, Berton O, Nestler EJ, Krishnan V, Eisch AJ (2010) Adult hippocampal neurogenesis is functionally important for stress-induced social avoidance. Proc Natl Acad Sci USA 107:4436–4441
Lee JH, Chung WH, Kang EH, Chung DJ, Choi CB, Chang HS, Hwang SH, Han H, Choe BY, Kim HY (2011) Schwann cell-like remyelination following transplantation of human umbilical cord blood (hUCB)-derived mesenchymal stem cells in dogs with acute spinal cord injury. J Neurol Sci 300:86–96
Lepore AC, Bakshi A, Swanger SA, Rao MS, Fischer I (2005) Neural precursor cells can be delivered into the injured cervical spinal cord by intrathecal injection at the lumbar cord. Brain Res 1045:206–216
Liu W, Jiang X, Fu X, Cui S, Du M, Cai Y, Xu R (2008) Bone marrow stromal cells can be delivered to the site of traumatic brain injury via intrathecal transplantation in rabbits. Neurosci Lett 434:160–164
Liu Y, Liu T, Ma X, Fan X, Bao C, Cui Z (2009) Effects of encapsulated rabbit mesenchymal stem cells on ex vivo expansion of human umbilical cord blood hematopoietic stem/progenitor cells. J Microencapsul 26:130–142
Madhavan L, Daley BF, Paumier KL, Collier TJ (2009) Transplantation of subventricular zone neural precursors induces an endogenous precursor cell response in a rat model of Parkinson’s disease. J Comp Neurol 515:102–115
Mahmood A, Lu D, Chopp M (2004) Marrow stromal cell transplantation after traumatic brain injury promotes cellular proliferation within the brain. Neurosurgery 55:1185–1193
Minguell JJ, Florenzano FM, Ramírez MR, Martínez RF, Lasala GP (2010) Intracoronary infusion of a combination of bone marrow-derived stem cells in dogs. Exp Clin Cardiol 15:17–20
Morita E, Watanabe Y, Ishimoto M, Nakano T, Kitayama M, Yasui K, Fukada Y, Doi K, Karunaratne A, Murrell WG, Sutharsan R, Mackay-Sim A, Hata Y, Nakashima K (2008) A novel cell transplantation protocol and its application to an ALS mouse model. Exp Neurol 213:431–438
Nacher J, Crespo C, McEwen BS (2001) Doublecortin expression in the adult rat telencephalon. Eur J Neurosci 14:629–644
Nervi B, Link DC, DiPersio JF (2006) Cytokines and hematopoietic stem cell mobilization. J Cell Biochem 99:690–705
Neupane M, Chang CC, Kiupel M, Yuzbasiyan-Gurkan V (2008) Isolation and characterization of canine adipose-derived mesenchymal stem cells. Tissue Eng Part A 14:1007–1015
Newby AC (2006) Matrix metalloproteinases regulate migration, proliferation, and death of vascular smooth muscle cells by degrading matrix and non-matrix substrates. Cardiovasc Res 69:614–624
Pavlichenko N, Sokolova I, Vijde S, Shvedova E, Alexandrov G, Krouglyakov P, Fedotova O, Gilerovich EG, Polyntsev DG, Otellin VA (2008) Mesenchymal stem cells transplantation could be beneficial for treatment of experimental ischemic stroke in rats. Brain Res 1233:203–213
Paxinos G, Watson C (2005) The rat brain in stereotaxic coordinates, 5th edn. Elsevier Academic Press, Amsterdam
Picard-Riera N, Nait-Oumesmar B, Baron-Van Evercooren A (2004) Endogenous adult neural stem cells: limits and potential to repair the injured central nervous system. J Neurosci Res 76:223–231
Poh KK, Sperry E, Young RG, Freyman T, Barringhaus KG, Thompson CA (2007) Repeated direct endomyocardial transplantation of allogeneic mesenchymal stem cells: safety of a high dose, “off-the-shelf”, cellular cardiomyoplasty strategy. Int J Cardiol 117:360–364
Prockop DJ (2007) “Stemness” does not explain the repair of many tissues by mesenchymal stem/multipotent stromal cells (MSCs). Clin Pharmacol Ther 82:241–243
Ramirez-Amaya V, Marrone DF, Gage FH, Worley PF, Barnes CA (2006) Integration of new neurons into functional neural networks. J Neurosci 26:12237–12241
Saito F, Nakatani T, Iwase M, Maeda Y, Hirakawa A, Murao Y, Suzuki Y, Onodera R, Fukushima M, Ide C (2008) Spinal cord injury treatment with intrathecal autologous bone marrow stromal cell transplantation: the first clinical trial case report. J Trauma 64:53–59
Scholzen T, Gerdes J (2000) The Ki-67 protein: from the known and the unknown. J Cell Physiol 182:311–322
Shear DA, Tate MC, Archer DR, Hoffman SW, Hulce VD, Laplaca MC, Stein DG (2004) Neural progenitor cell transplants promote long-term functional recovery after traumatic brain injury. Brain Res 1026:11–22
Sugaya K (2003) Neuroreplacement therapy and stem cell biology under disease conditions. Cell Mol Life Sci 60:1891–1902
Sun L, Lee J, Fine HA (2004) Neuronally expressed stem cell factor induces neural stem cell migration to areas of brain injury. J Clin Invest 113:1364–1374
Taiwo OB, Kovács KJ, Larson AA (2005) Chronic daily intrathecal injections of a large volume of fluid increase mast cells in the thalamus of mice. Brain Res 1056:76–84
Terada M, Kuzumaki N, Hareyama N, Imai S, Niikura K, Narita M, Yamazaki M, Suzuki T (2008) Suppression of enriched environment-induced neurogenesis in a rodent model of neuropathic pain. Neurosci Lett 440:314–318
van Velthoven CT, Kavelaars A, van Bel F, Heijnen CJ (2010) Repeated mesenchymal stem cell treatment after neonatal hypoxia-ischemia has distinct effects on formation and maturation of new neurons and oligodendrocytes leading to restoration of damage, corticospinal motor tract activity, and sensorimotor function. J Neurosci 30:9603–9611
Veena J, Srikumar BN, Raju TR, Shankaranarayana Rao BS (2009) Exposure to enriched environment restores the survival and differentiation of new born cells in the hippocampus and ameliorates depressive symptoms in chronically stressed rats. Neurosci Lett 455:178–182
Vieira NM, Brandalise V, Zucconi E, Secco M, Strauss BE, Zatz M (2010) Isolation, characterization, and differentiation potential of canine adipose-derived stem cells. Cell Transplant 19:279–289
Yang J, Wu H, Hu N, Gu X, Ding F (2009) Effects of bone marrow stromal cell-conditioned medium on primary cultures of peripheral nerve tissues and cells. Neurochem Res 34:1685–1694
Zhu S, Lu Y, Zhu J, Xu J, Huang H, Zhu M, Chen Y, Zhou Y, Fan X, Wang Z (2011) Effects of intrahepatic bone-derived mesenchymal stem cells autotransplantation on the diabetic beagle dogs. J Surg Res 168:213–223
Acknowledgments
The authors would like to thank Mr. Seok Han, Mr. Seung Uk Lee, and Ms. Hyun Sook Kim for their technical help and Seung-Hae Kwon of the Korean Basic Science Institute Chuncheon Center for technical assistance with the confocal image analyses (LSM 510 META NLO) in this study. This research was supported by the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2010-001058), and by a grant (2010K000823) from Brain Research Center of the 21st Century Frontier Research Program funded by the Ministry of Education, Science and Technology, the Republic of Korea.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Jung Hoon Choi and Jin Young Chung contributed equally to this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10571_2011_9729_MOESM1_ESM.tif
Supplementary Fig. 1. Fluorescence image of in vitro labeled of Ad-MSCs with CM-DiI. Scale Bar = 25 μm (A-C) (TIFF 3077 kb)
10571_2011_9729_MOESM2_ESM.tif
Supplementary Fig. 2. Immunofluorescence detection of CM-DiI-labeled Ad-MSCs in the hippocampus (A-C), diencephalon (D-E), midbrain (G-H) and spinal cord (J-L). Note that Ad-MSC (arrows) are observed in the meninges of the brain except for hippocampus. 3 V, third ventricle; CA, cerebral aqueduct; CC, central canal of the spinal cord. Scale Bar = 500 μm (A-I) 350 μm (J-L) (TIFF 12638 kb)
Rights and permissions
About this article
Cite this article
Choi, J.H., Chung, J.Y., Yoo, D.Y. et al. Cell Proliferation and Neuroblast Differentiation in the Rat Dentate Gyrus After Intrathecal Treatment with Adipose-Derived Mesenchymal Stem Cells. Cell Mol Neurobiol 31, 1271–1280 (2011). https://doi.org/10.1007/s10571-011-9729-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10571-011-9729-7