Abstract
The present study examined predictors of youth client retention in therapy in a large community-based sample. We used several conceptualizations of retention, including (a) “intake retention” (i.e., returned to treatment after intake session); (b) “mutual termination” (i.e., termination agreed upon by family and therapist), (c) “mean treatment duration” (i.e., completing the mean number of sessions in the agency), and (d) “total treatment duration” (i.e., total number of sessions). Archival data from over 400 children and adolescents who sought treatment at a large public mental health clinic were analyzed using regression analyses. Although different predictors were identified across the various conceptualizations, a few robust predictors emerged including ethnicity and client symptom severity. Clinical implications and future research directions are discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Epidemiological studies estimate that 10–20% of children have mental health problems involving functional impairment (United States Public Health Service 1999). Fortunately, a body of research has accumulated demonstrating the potency of several treatment approaches with youth, referred to as evidence-based or empirically-supported treatments (hereafter, EBTs; e.g., Chorpita and Southam-Gerow 2006; McMahon et al. 2006; Weisz et al. 2006). However, for any treatment to be effective, it is likely that clients must attend therapy sessions and follow treatment recommendations. Indeed, some research has suggested that dropping out of therapy early leads to an attenuation of outcomes (e.g., Boggs et al. 2004; Prinz and Miller 1994). Unfortunately, studies have shown that client attrition is commonplace, with between 40 and 60% of clients ceasing treatment before termination is recommended (Baekeland and Lundwall 1975; Wierzbicki and Pekarik 1993). Accordingly, researchers have sought to identify risk factors for attrition so that clients at risk for early termination can be identified early in the therapy process. Such factors can guide research in the development and implementation of strategies for enhancing therapy attendance (e.g., Nock and Kazdin 2005).
Several related constructs have been discussed within the spectrum of therapy adherence (e.g., Meichenbaum and Turk 1987), including therapy initiation (i.e., the process of calling a mental health provider, scheduling an appointment, and attending at least one session), attrition/retention, and adherence to therapy recommendations, often operationalized as homework compliance. The focus of the present investigation, attrition/retention, has been defined in a variety of ways in the literature: (1) the client discontinuing therapy before the therapist feels the client is ready for treatment termination (Garcia and Weisz 2002; Klein et al. 2003); (2) the client missing a scheduled session (Wierzbicki and Pekarik 1993); (3) the client failing to attend a specific number of sessions (i.e., Kazdin and Mazurick 1994; Kendall and Sugarman 1997; Siqueland et al. 2002); and (4) a combination of the criteria listed above (Kazdin et al. 1997; see Kazdin 1996; Wierzbicki and Pekarik 1993 for reviews of these operational definitions). Use of the term “treatment completion” is typical of the study of retention/attrition within research projects investigating the efficacy of manualized treatment approaches.Footnote 1 As these various definitions imply, defining the end of treatment is not a simple task, a point we return to later.
The lion’s share of research on attrition with child and adolescent research-clinic based samples has occurred in randomized clinical trial (RCT studies) and most of this has focused on youth with externalizing behavior problems, though a few studies of children with internalizing disorders have been conducted. Even fewer studies have occurred in non-research clinical service settings like community mental health centers or private practice settings where treatment endpoints are rarely predetermined. We reviewed studies completed since the Wierzbicki and Pekarik (1993) review. Table 1 presents a summary of the significant findings from those studies, including counts of the number of studies identifying the predictors as significant. For the review, we also divided studies into two categories, depending on whether they were conducted in a research-oriented clinic (e.g., during an efficacy trial) or in a community clinic setting (i.e., mental health center). The most commonly cited factors in research clinic studies were: socioeconomic status, race/ethnicity, severity of presenting problem, parent stress, and single parent status whereas for community clinic studies, the most common factors were: ethnicity, problem severity, and child age.
The literature on attrition in child/adolescent mental health treatment has several limitations. First, there is a paucity of studies on children. In the most recent meta-analysis of 125 studies of psychotherapy attrition only 16 studies involved a child population (Wierzbicki and Pekarik 1993). Since that review, the number of child and adolescent studies in community mental health centers and similar settings remains low.
Another limitation of the literature is that the large majority of attrition research has been conducted as part of RCTs where treatment is manualized and has a finite endpoint, and thus treatment completion can be objectively defined at the outset of the study. However, outside of the RCT context, treatment duration is rarely pre-determined, complicating the study of attrition. In addition, there is reason to be cautious in generalizing data from RCTs to community mental health settings. Differences between youth seen in these two settings have been demonstrated across multiple studies (Hammen et al. 1999; Southam-Gerow et al. 2003, 2008b). Furthermore, differences between the procedures (e.g., monetary incentives, reminder phone calls) at the two settings cloud generalizability of findings (Weisz et al. 2003). Thus, studying attrition outside of research settings may be important.
Another limitation to attrition research is a lack of a guiding theoretical framework, despite the presence of theoretical models that purport to explain health care utilization. For example, the Health Belief Model (HBM; Becker et al. 1972, 1978; Friedman and Litt 1987; LaGreca and Bearman 2003) hypothesizes that adherence is related to the patient’s or family’s perceptions of the following: (a) severity of the disease or complications related to the disease, (b) the benefits of recommended regimens, (c) their susceptibility to the specific disease or condition, and (d) perceived barriers and costs associated with the prescribed course of treatment. Additionally, some versions of this model include information about the patient’s relationship with their health care provider and individual beliefs about health (Bauman 2000).
Researchers have also discussed an ecological framework for understanding mental health care (e.g., Bronfenbrenner 1979; Schoenwald and Hoagwood 2001; Southam-Gerow et al. 2006). Such a framework may be applicable to an understanding of attrition and retention. The ecological model depicts the multi-layer and dynamic context of mental health service delivery that involves several relevant levels of factors to consider in treatment development, delivery, and relevant to the current project, attrition. The context includes: (a) client-level factors (e.g., symptoms, functioning), (b) provider-level factors (e.g., level of professional experience, attitudes), (c) intervention-specific characteristics (e.g., therapeutic modality), (d) service delivery characteristics (e.g., frequency of sessions, location of care), (e) organizational influences (e.g., culture and climate), and (f) environmental factors (e.g., service system financing policies). All of these may influence attrition.
From a similar perspective, Anderson and Newman (1973) suggested that health care utilization is accounted for by several dimensions: (a) societal determinants (norms, technology), (b) health services system factors (resources, organization), and (c) individual determinants (predisposition of the individual to use services, enabling factors, and illness level). Although health care utilization is related to adherence in that it describes how likely an individual is to use services, the two constructs are not synonymous.
In this study, we draw on these health care utilization models to frame our study of predictors of attrition/retention using archival records from a large publicly-funded community mental health center. Because of the varied conceptualizations of attrition in the literature and because we were studying a population rarely examined, we operationalized attrition in several ways, following the work of Lau and Weisz (2003). First, we examined predictors of “intake retention”: individuals who attend at least one appointment after the intake visit. We also examined predictors of two different conceptualizations of treatment “completion”: “mutual termination”: individuals who ceased treatment with consent of the therapist and “mean treatment duration”: individuals who attended at least the mean number of treatment sessions for the sample before terminating. Finally, we examined for predictors of total treatment duration (i.e., total number of sessions the client attended).
To create a pool of potential predictors, we adopted elements of the ecological and Health Belief models. Because our study occurred in the context of a single agency and single mental health system and because provider level variables were not available, we focused on child and family factors. Thus, our application of the ecological model was limited. Our focus included child/adolescent-level factors (e.g., symptoms, age, ethnicity) and family-level factors (e.g., family stress, SES). Consistent with past research, we expected that retention would be predicted best by younger, non-minority youth with lower levels of symptoms whose family situation afforded psychosocial advantage (e.g., higher income, fewer family stressors).
Methods
Participants
Data for this study were collected from archival medical records for child clients who received traditional outpatient therapy services at a community mental health clinic that provides therapy and assessment services to children, families, and adults residing in a large metropolitan county in central Virginia. All closed cases who received services between July 1995 and May 2005 were potentially eligible. Inclusion in the study required all of the following criteria: (1) client was 18-years-old or younger at the time of the intake session; (2) client attended at least one complete intake session; (3) therapy (not assessment) was recommended for the client; (4) the client received services through the outpatient services reporting unit at clinic; and (5) a record of scheduled and attended sessions was available. The first episode of care that met the above criteria was used for all of the participants. Clients with missing information on any of these variables were excluded from the sample. Once the sample was obtained,Footnote 2 clients were excluded if they had a primary Axis I diagnosis of an eating disorder, enuresis/encopresis, a psychotic/thought disorder, or a missing diagnosis (n = 14) because such cases occurred in low frequency. Because the vast majority of the clients at the clinic were either Caucasian or African-American (more than 95% of all eligible cases), youth from other ethnic groups were not included in the study.Footnote 3 In short, the sample obtained is representative of the youth receiving outpatient services from the agency during the 10-year span, with as close to that entire population represented as was possible (i.e., the only youth missing were those for whom there was no record of their having attended a session at the agency; it is possible that some youth received treatment at the agency, the records for which were missing).
The sample consisted of 447 children (49.2% male) with a mean age at the date of their first visit of 11.87 (range 2.92–17.92). The majority of the sample was white (71.2%); 28.8% were African-American. The median family yearly income was $17,160. Using US Census archival poverty level tables, 41.5% of the sample was below the poverty level.Footnote 4
Independent Variables
The initial pool of predictors included child-sociodemographic (i.e., age, ethnicity, gender), child-clinical (e.g., diagnoses, functional impairment rating), and parent/family-related (e.g., income, psychosocial stressors, insurance status) variables.
Child: Sociodemographic
Gender and ethnicity were collected in a form completed at intake. Age was calculated using the client’s date of birth and the date of their first face-to-face visit at clinic.
Child: Clinical
Several indices of child clinical severity were available including primary DSM Axis I diagnoses, number of DSM Axis I diagnoses, DSM Axis V score (i.e., GAF), and number of hospital admissions. Primary DSM Axis I diagnoses were separated into four groups: (a) internalizing disorders (i.e., anxiety and depressive disorders), (b) disruptive behavior disorders (i.e., ADHD, conduct disorder, and oppositional defiant disorder), (c) adjustment disorders, and (d) relational problems (i.e., V codes, American Psychiatric Association 2000). We also coded presence (or not) of concurrent psychiatric care from the record of sessions attended. If a client attended one session with a psychiatrist they were considered to have received, and followed through with, a psychiatric referral. However, we only analyzed this variable for the mutual termination definition; for the other definitions, the IV would be confounded with psychiatric visits.
Another child-related factor was the presence or not of a DSM Axis III code for medical problems. DSM Axis III diagnoses are used to report current general medical conditions that could be relevant to conceptualizing or treating mental health problems (American Psychiatric Association 2000).
Parent/Family
Insurance information, annual income, family size, referral source, and psychosocial stressors (i.e., DSM Axis IV) were the parent/family related variables available in the agency database. The first three were collected in a form completed at intake. We coded insurance status into two groups: public or private insurance. Referral source, collected at the time of the intake, was coded as follows: public (e.g., court/legal system, school referral, community provider) or private (e.g., self/parent, friend). Annual income was provided as a raw figure by the family. Family size was separated into two groups (0–4 people and more than 4 people living in the home) because evidence has suggested that a family size greater than 4 is associated with attrition (Pumariega et al. 1998). Psychosocial stressors were also collected through the use of the DSM’s Axis IV. The DSM Axis IV is reserved for recording environmental or psychosocial factors that may impact the accurate diagnosis and/or treatment prognosis for the presenting mental health problem (American Psychiatric Association 2000). Stressors recorded on Axis IV can be independent of or a consequence of an individual’s presenting problem. Severe environmental and psychosocial problems that are the main focus of intervention can be coded on Axis I. The DSM-IV-TR classifies Axis IV problems into the following categories: (a) problems with primary support group, (b) problems with social environment, (c) educational problems, (d) occupational problems, (e) housing problems, (f) economic problems, (g) problems with access to health care, (h) problems related to legal system/crime, and (i) other psychological and environmental problems. Because there was a high prevalence of problems in primary support group (67.4%), participants in this group were compared to all others for data analyses.
Dependent Variables
As noted, we applied several conceptualizations of retention: “intake retention”, “mutual termination”, “mean treatment duration”, and “total treatment duration”. Coding of “intake retention” was based on whether the client attended appointments following the intake session. Those who attended one appointment (i.e., intake only) were coded as “drop-outs”, those who attended more than one appointment were coded as “retained”.
“Mutual termination” was coded based on the therapist’s indication of reason for termination on a forced choice section of the termination summary. Among several options listed, therapists are required to indicate if the termination was with or without their agreement. Unfortunately, some of the options did not offer a clear indication of whether termination was with therapist agreement; participants with such termination reasons were not included in these analyses, eliminating less than 40% of the sample (n = 168). Because this definition led to the exclusion of a large number of youth from the related analyses, we planned to conduct analyses to compare those youth who were and were not included in the analyses to determine if there were systematic differences between the groups.
“Mean treatment duration” was defined by comparing the number of sessions attended by the individual to the mean number of sessions attended by the sample. The mean number of therapy sessions attended was 8.52; a cut-point of eight sessions was used because it better represented the distribution of the sample (median = 5, mode = 1). Clients who attended eight or fewer sessions were placed in the “less than mean duration” group; those who attended more than eight sessions were coded as “at least mean duration”.
Total treatment duration (i.e., total number of sessions). We also examined for predictors of retention using the simple method of predicting total numbers of sessions. Note that because one of our possible predictors (concurrent psychiatric care) was confounded with three of our definitions (intake retention, mean treatment duration, and total treatment duration), we only included that variable in the mutual agreement analyses.
Results
Analytic Plan
Our aims were to identify predictors for the four conceptualizations of retention outlined earlier: (a) intake retention, (b) mutual termination, (c) mean treatment duration, and (d) treatment duration. For the first three conceptualizations, we used logistic regression analyses whereas for the latter, we used a hierarchical regression analysis. Before conducting our regression analyses, however, we conducted preliminary analyses to reduce our pool of predictors.
Preliminary Analyses
We conducted several sets of analyses (t-tests, chi-square tests, correlational analyses) to reduce the pool of predictors to be used in four sets of planned regression analyses. These preliminary analyses were conducted separately for each conceptualization of attrition/retention. Predictors that were present for at least 50% of the sample and that were significant at the p ≤ .10 level were retained for subsequent regression analyses.
Retention Categories
For three of the four conceptualizations (i.e., intake retention, mutual termination, and mean treatment duration), the sample was divided into one of two categories: retain or dropped out. Using the “intake retention” conceptualization for all 448 participants, 83.0% (n = 372) were retained versus 17.0% (n = 76) that were not retained.
As noted earlier, for the “mutual termination” definition, we were only able to code 280 of the records into one of the two relevant categories of “mutual” or “unilateral” termination. Because of the large number of excluded participants, we conducted a preliminary set of analyses on the sample before conducting the analyses to identify our pool of predictors. Specifically, we compared the group of youth for whom it could be determined whether “mutual termination” had occurred or not to those for whom it could not be determined, conducting t-tests and chi-square tests for all variables we used in the study (i.e., child and family predictor variables). All of these tests revealed non-significant differences, suggesting that the data were not missing for any systematic difference that we could test. Fully 61.4% (n = 172) terminated therapy services in mutual agreement with their service provider, 38.6% (n = 108) terminated services without agreement of their service provider.Footnote 5 Based on the “mean treatment duration” definition, four of the records did not have adequate data to determine the total number of treatment sessions attended. As a result, analyses using this definition used 444 participants. From this sample, 33.8% (n = 150) attended at least the mean number of sessions for the agency versus 66.2% (n = 294) who did attended fewer.
Intake Retention
Preliminary analyses for “intake retention” were conducted using the entire sample (N = 448). There were four significant predictors: income (t [93.1Footnote 6] = 2.43, p < .03, d = −.31), Axis III diagnosis (χ2[1] = 4.12, p < .05), primary Axis I adjustment disorder diagnosis at intake (χ2[1] = 3.37, p < .07), and total number of Axis I diagnoses (t [420] = 1.96, p < .05, d = .24).
Mutual Termination
Preliminary analyses for “mutual termination” were conducted for the sample of 280 participants for whom mutual termination status could be coded. There were six retained predictors: age (t [278] = −2.00, p < .05, d = −.25), gender (χ2[1] = 4.21, p < .04), Axis III diagnosis (χ2[1] = 4.12, p < .04), primary Axis I adjustment disorder diagnosis at intake (χ2[1] = 2.77, p < .10), primary relational problems diagnosis at intake (χ2[1] = 2.82, p < .09), and Axis V score (t [261] = 2.20, p < .03, d = .28).
Mean Treatment Duration
Preliminary analyses for “mean treatment duration” were conducted using a sample of 444; as noted, data from four of the original participants were incomplete with regard to total number of sessions attended. Significant predictors were: age (t [442] = 2.45, p < .02, d = .24), ethnicity (χ2[1] = 10.95, p < .009), at least one previous psychiatric hospitalization (χ2[1] = 4.95, p < .03), primary Axis I disruptive behavior disorder diagnosis (χ2[1] = 5.19, p < .02), primary Axis I adjustment disorder diagnosis (χ2[1] = 6.11, p < .01), and Axis V score (t [418] = 2.14, p < .03, d = .23).
Total Treatment Duration
Preliminary analyses for “treatment duration” were conducted for the sample of 444 participants for whom the total number of sessions could be calculated. We used t-tests and correlational analyses for these preliminary tests. In the end, seven variables were retained for the total treatment duration regression analysis: age (r [n = 444] = −.14, p < .003), ethnicity (t [442] = 2.83, p < .005, d = .31), presence of Axis IV stressors (t [416] = 2.43, p < .02, d = .26), at least one previous psychiatric hospital admission (t [441] = 2.43, p < .02, d = −.27), primary Axis I adjustment disorder diagnosis (t [418] = 2.61, p < .009, d = .30), primary Axis I relational problems(t [23.88Footnote 7] = 2.16, p < .04, d = .35), and GAF score (r [n = 420] = −.10, p < .04).
Logistic and Hierarchical Regression Analyses
Examining Assumptions
Prior to performing all logistic and hierarchical regression analyses, data were checked for violations of any assumptions. Outliers were examined by visual inspection for all variables. To reduce multicollinearity, theoretically redundant variables were not included in the analyses. For example, only the continuous measure of age was included. Further, correlations between the variables included in the logistic regression analyses were below the accepted “moderate” level of .30 (Cohen 1988) (range −.006 to .232), thus no predictors were deleted because of high inter-correlation. The between-subjects design and collection of data at one time-point support the assumption of independent error.
Missing Data
For the following regression analyses, we used listwise deletion as the primary means to handle missing data. The number of excluded participants, of course, varied by definition: Intake Retention (n = 91), Mutual Termination (n = 28), Mean Duration (n = 26), and Total Duration (n = 28). Preliminarily, we conducted t- and chi-square tests to determine if participants who were excluded from each regression analysis differed from those included on any of the variables we had available. We conducted these analyses for each definition separately.
For Intake Retention, three statistically significant differences emerged: families with lower incomes, families with public (vs. private) insurance, and families who terminated after the first session were more likely to have been excluded from the analysis because of missing data. The latter finding is logical—if a client did not attend treatment after the first session, some of the data for the study would not yet have been collected.
For Mutual Termination, no statistically significant differences were in evidence between the groups. For Mean Duration, one statistically significant difference emerged: families with lower incomes were more likely to have been excluded from the analysis because of missing data. For Total Duration, two statistically significant differences emerged: male youth clients and families with lower incomes were more likely to have been excluded from the analysis because of missing data. We discuss the implications of these findings later.
Sequential Logistic Regression Analyses
Logistic regression analyses were conducted to determine which variables best predicted attrition as defined in the three ways described above. We only conducted these analyses if preliminary analyses for the attrition category resulted in the retention of at least 2 predictors. Using this criterion, three separate sequential logistic regression analyses were conducted.
For the three logistic regression analyses, predictors were entered in blocks across several steps, using order of temporal precedence as the method for creating and entering the blocks. Temporal precedence was used given the lack of a clear pattern in past research that would dictate which variables were causally more relevant. Child sociodemographic (e.g., ethnicity, age) and other (Axis III) predictors were entered first, followed by parent/family factors (e.g., income, family size, Axis IV) in the second step, and child diagnosis/symptom severity data (e.g., Axis I diagnoses, Axis V, concurrent psychiatric care, hospital admissions) in the last step.
Intake Retention Logistic Regression Analysis
A total of 357 cases were used to conduct a three-step (child sociodemographic/other variables, parent/family factors, child symptom severity) sequential logistic regression analysis for “intake retention”. To reflect the actual distribution of cases, a cut-value of .83 was used for the analyses. Results of the logistic regression model suggested that Steps 1 (i.e., child sociodemographic/other) and 2 (i.e., parent/family) and the overall model were statistically significant, full model: χ2 (1) = 11.38, p = .02. The model correctly predicted 69.7% of cases overall; 40.0% of those who were not retained after intake and 74.6% of those who were retained. Prediction of those who were not retained was increased to 50.0% by increasing the cut-value to .84, with small decreases in the overall and retention prediction levels 65.3 and 67.8% respectively. None of the individual predictors were statistically significant at the p ≤ .05 level (see Table 2).
Mutual Termination Logistic Regression Analysis
A total of 261 cases were used to conduct a two-step (child sociodemographic/other variables, child symptom severity) sequential logistic regression analysis for “mutual termination”. To reflect the actual distribution of cases, a cut-value of .61 was used for the analyses. The first step (i.e., child sociodemographic/other) and the overall model were statistically significant. The full model was able to distinguish between those who did and did not terminate through mutual agreement “mutual termination”, χ 2 (6) = 15.98, p ≤ .02. The model correctly predicted 60.9% of cases overall; 10.3% of those whose therapist disagreed with termination and 96.1% of those whose therapist agreed with their decision to terminate therapy. The predictive value of the model was modestly increased to 61.7% overall, 18.7% for disagreement, and 91.6% for agreement when using a cut value of .56. No individual predictors were significant at the p ≤ .05 level (see Table 3).
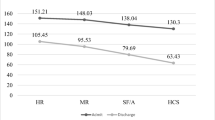
Mean Treatment Duration Logistic Regression Analysis
A total of 420 cases were used to conduct a two-step (child sociodemographic/other variables, child symptom severity) sequential logistic regression analysis for “mean treatment duration”. To reflect the actual distribution of cases, a cut-value of .34 was used for the analyses. The overall model was able to distinguish between “mean treatment duration”, χ 2 (7) = 25.51, p ≤ .001. Both individual steps (i.e., child sociodemographic/other variables, and child symptom severity) of the model were statistically significant at the p ≤ .05 level. The overall model correctly predicted 63.8% of cases overall; 66.0% of those who terminated before the mean number of sessions and 59.3% of those who completed at least the mean number of sessions. Ethnicity was the only statistically significant individual predictor (see Table 4). Results indicated that the odds that African-American youth would end treatment before reaching the mean number were twice those for Caucasian youth.
Total Treatment Duration Hierarchical Regression Analysis
A total of 418 cases were used to conduct a three-step (child sociodemographic/other variables, parent/family factors, child symptom severity) hierarchical regression analysis for “total treatment duration”. All three steps were significant at the p ≤ .05 level. The full model explained about 4% of the variance. As reflected in Table 5, there were three statistically significant individual predictors: child ethnicity, presence of an Axis IV stressor, and Axis I adjustment disorder diagnosis. Results suggest that African-American youth and youth with adjustment disorder diagnoses had fewer sessions total than Caucasian youth and youth without adjustment disorders, respectively. In addition, youth with at least one Axis IV stressor had more sessions than youth without an Axis IV stressor.
Discussion
This study explored whether various sociodemographic, family/ecological, and child symptom/diagnostic factors were associated with retention among youth clients seeking outpatient psychotherapy services at a publicly-funded community mental health center. To evaluate predictors, we used four different approaches, three categorical and one continuous. Using the “intake retention” definition (i.e., families returned to treatment after the intake session) yielded the highest percentage of individuals retained (83.0%), followed by “mutual termination” (i.e., therapist and family agreed to terminate) at 61.1%; only about 1/3 of families attended at least the mean number of treatment sessions for the agency. A fourth approach identified predictors of the total number of sessions attended by youth. Although predictors of retention varied depending on the definition used, a few consistent predictors emerged, including ethnicity and adjustment disorder diagnosis at intake.
There were no significant individual predictors of retention of youth after intake, though the overall model (including Axis III diagnosis, family income, total Axis I diagnoses, and Axis I adjustment disorder diagnosis) was able to correctly predict about 70% of cases. Analyses for families whose treatment ended in mutual agreement between therapist and family also failed to identify any significant individual predictors. However, the overall model (including gender, age, Axis III diagnosis, Axis V score, Axis I disruptive behavior disorder diagnosis, and Axis I anxiety or depressive disorder diagnosis) was significant and correctly predicted 64% of cases. For the two sets of analyses involving treatment duration, child ethnicity was a significant individual predictor. In addition, for the total treatment duration definition, a primary Axis I diagnosis of adjustment disorder and the presence of an Axis IV stressor was also a significant predictor.
On a positive note, more than 4/5 of children (83.0%) returned for at least one session after the initial intake/information gathering session and a majority of youth (61.4%) terminated at a time thought appropriate by the therapist. However, only about 1/3 of youth (33.8%) attended at least eight treatment sessions, including intake. Because the length of most evidence-based treatments exceeds eight sessions, these data raise concerns about the possibility of delivering such treatments to youth in the setting without some attention to factors that predict session attendance.
Variations in the definition of retention/attrition across studies make it difficult to compare these findings to the literature. Kazdin (1996) suggests that “dropping-out” of therapy has three components: (1) the client leaves therapy; (2) the client unilaterally makes the decision to leave; and (3) the treatment provider perceives the termination to be premature and has advised the client to continue, a definition most similar to the “mutual termination” definition. Based on this definition, the attrition rate among this sample (38.6%) is consistent with the 40–60% found in past research (Baekeland and Lundwall 1975; Wierzbicki and Pekarik 1993).
There were a few significant individual predictors across all analyses: child ethnicity, Axis I adjustment disorder diagnosis, and Axis IV stressors. These findings suggest good news and bad news. First, the good news. Children and adolescents with Axis I adjustment disorder diagnoses, and without Axis IV stressors at intake received fewer treatment sessions than children and adolescents without adjustment disorder diagnosis, and with the presence of at least one Axis IV stressor. This pattern of findings suggests that youth most in need of services (i.e., those with diagnoses other than adjustment disorder and those with psychosocial stressors) are receiving more services than those in less need. It makes sense that a child with Axis I diagnosis of adjustment disorder would receive a relatively fewer number of sessions, compared to youth with other Axis I diagnoses (APA 2000). Similarly, it might be expected that the presence of a least one Axis IV stressor would complicate treatment and thus require a larger number of sessions (Southam-Gerow et al. 2008b). In addition, although past hospital admission was not a significant individual predictor, it was present in two of the four models because it was related to retention in univariate analyses. And in both models, the direction of effect was in the expected direction: that is, youth with a history of at least one hospital admission received more treatment. The finding makes sense in the context of public mental health, wherein offering outpatient services to youth discharged from inpatient facilities is a major priority. However, this particular finding should be viewed with caution, because past hospital admission was not a statistically significant individual predictor. Together, these various findings suggest the good news that treatment allocation to families in this study appeared to occur in a logical way.
Now for the bad news. That Caucasian families were more likely to complete a higher number of sessions, though a common finding (e.g., Kazdin and Mazurick 1994; Nock and Kazdin 2001; Kendall and Sugarman 1997; McMiller and Weisz 1996; Siqueland et al. 2002; Zimmerman 2005; but see, Pina et al. 2003), raises concerns. First, considering that 75% of staff were Caucasian, one hypothesis for the finding is the lack of therapist–client cultural match—some have argued that such a match may be important to clients (see Sue 1998 for discussion). Additionally, though more speculative, it could be that the treatments offered at the clinic match cultural beliefs and preferences of Caucasian families better than those of the African-American families (Dwight-Johnson et al. 2000; Yeh et al. 2005). Finally, the finding highlights how little our current science guides us with regard to the importance of cultural and ethnic differences in therapy. In much of the literature, ethnic minority representation in samples continues to lag, despite calls for increased diversity (e.g., Mak et al. 2007). Thus, one relevant future direction would be to address the apparent difficulty in retaining African-American families in treatment, drawing on the growing literature on cultural adaptations for treatments (e.g., Lau 2006; Martinez and Eddy 2005; McClure et al. 2005).
Finally, a primary finding of the study is the overall lack of predictive variables. There were very few significant predictors. Furthermore, none of the four models was particularly potent at predicting attrition or retention. As an example, the logistic regression models all predicted fewer than 75% of cases correctly and the hierarchical regression model only accounted for 4% of the variance overall. Given the importance of treatment attendance for clients with mental health problems, the identification of variables that predict attendance would be highly useful.
Strength of this study include its focus on a public mental health clinic (contrasting it with the bulk of past studies on attrition and retention), the large sample size, the use of data collected over a period of 10 years, and the addition of diagnostic information as predictors. To date, there has been no investigation of retention and attrition among such a large and inclusive sample of children seeking services at a community mental health center.
Limitations and Future Directions
Our results should be considered in light of several limitations. First, although the database was rich and extensive, missing data were common. In particular, we found that missing data were more prevalent when the identified client was a male and from families with lower incomes and families with public insurance. Thus, the external validity of the findings should be assessed with these facts in mind.
Second, because of our use of archival data retrieved from a medical records review, a number of potentially relevant variables were not available to us. As noted earlier, some scientists have advocated for an ecological model when considering the effects of mental health treatments, with a focus on multiple levels, including the child, the family and the community as well as considering factors related to the agency, including the providers, characteristics of the agency itself, and aspects of the mental health system in which the agency operates (see Chorpita et al. 2002; Schoenwald and Hoagwood 2001; Southam-Gerow et al. 2006). Future work could include prospective investigations that build such an ecological model into the design, tapping factors related to retention and attrition across the multiple levels of family (e.g., expectations of therapy; Nock and Kazdin 2001), provider (e.g., ethnic match; Sue 1998), agency (e.g., organizational climate/culture; Glisson 2007) and system (e.g., payer policies; Schoenwald and Hoagwood 2001) levels. Additionally, given that there is little consensus about the most important predictors of attrition/retention, the use of qualitative research methods may help to generate fresh hypotheses.
Finally, the operational definitions of retention may need fine tuning. The “true” end-point of therapy is difficult to operationalize because the delivery of therapeutic intervention necessarily varies by presenting problem, treatment progress, and a number of therapist-related factors. Although we drew on past work for our definitions, we also noted that the considerable heterogeneity in definitions across past work. Development of more widely accepted definitions, even those that differ across populations (i.e., private, specialty clinics versus public mental health clinics), would provide a uniform language for researchers and clinicians and would facilitate the application of research findings to the population for which they are relevant.
One last future direction concerns a potential way to improve research on attrition in community settings. As noted, studies like this one rarely occur in public mental health settings. Many agencies have limited research budgets and expertise; as a result, clinic databases are not always developed to “maximize the research yield.” One potentially promising way to improve this problem may be through community-university partnerships (e.g., Southam-Gerow 2005). Within a partnership, scientists and community partners can work together to (a) identify the problems and issues that are most pertinent to the agency and (b) develop methods to examine and solve those problems.
Implications for Community Mental Health
Continued research in this area will continue to be important, especially given the expected increase of mental health problems among children over the next 15 years (United States Public Health Service 2000). Development and dissemination of empirically-supported treatments are currently a major focus in the field of clinical psychology (e.g., Southam-Gerow et al. 2008a). For treatments to benefit children and their families, regular attendance for the recommended duration of treatment is paramount. Mental health agencies may need to consider adoption not only of evidence-based treatments but also interventions designed to improve engagement and decrease attrition. Examples include programs that include motivational enhancement components (e.g., Miller and Rollnick 2002; Nock and Kazdin 2001, 2005). Similarly, others interventions may be useful for specific populations, such as caregivers who are depressed (e.g., Chronis et al. 2006). The present study also suggests the potential importance culture and ethnicity, underscoring the relevance of cultural competence and cultural adaptation (Cunningham et al. 2002; Huey and Polo 2008; Lau 2006).
However, prescribing prevention interventions without clear risk variables represents an expensive endeavor to provide attrition prevention to all clients. These results do not offer strong support for the strength of any of the predictors tested. Agencies wishing to identify predictors of attrition may need to proactively collect data that could represent potentially robust predictors. Such a step would be especially important very early in treatment, ideally in the first meeting, or even over the telephone at the time of the initial call. In an interesting recent study, Lasalvia et al. (2007) found that consensus on treatment goals between patients and providers was a robust predictor of positive outcomes. The findings supported the notion that concerns beyond DSM’s Axis I are often critical to patients; with attention to these problems, engagement in treatment may follow. Given the present findings, inquiry about medical problems in the family, and psychosocial stressors in the family as potential predictors of attrition may be a good, though under-appreciated method for building engagement and understanding the problems facing the family.
Notes
In some cases, where the point of therapy initiation is defined as the first phone call to obtain mental health services, the construct of “preintake attrition” is examined. This refers to the phenomenon of an individual making an appointment with a mental health provider and failing to attend their first scheduled appointment (Masi et al. 2003; Sparks et al. 2003). Preintake attrition is distinct from therapy attrition in that there has not been any face-to-face contact between the mental health services provider and the client(s). This can be viewed as a related construct within the umbrella of therapy attrition.
Some individuals had more than one “episode of care”, that is, they received services from the clinic for more than one discrete time period. It should be noted that some information was archived so it cannot be determined whether a client received services prior to July 1995.
These data are similar to those found in the locality, as reported in 2000 Census data (http://www.dataplace.org/area_overview/Chesterfield%20County,%20VA), though the proportion of African-Americans in the clinic was larger than that found in the locality as a whole (17% in the population, 27% in the sample).
These estimates also take into account the number of individuals dependent on the income.
As noted earlier, a large number (n = 168) fell into an “other” category for which information about therapist’s perception of termination was not available. These participants were not included in subsequent analyses for the mutual termination conceptualization.
Preliminary analyses suggested that variances were unequal between groups—thus, the degrees of freedom were adjusted accordingly.
Preliminary analyses suggested that variances were unequal between groups—thus, the degrees of freedom were adjusted accordingly.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: Author.
Anderson, R., & Newman, J. F. (1973). Societal and individual determinants of medical care utilization in the United States. Milbank Memorial Fund Quarterly: Health and Society, 51, 95–124.
Attride-Stirling, J., Davis, H., Farrell, L., Groark, C., & Day, C. (2004). Factors influencing parental engagement in a community child and adolescent mental health service: A qualitative comparison of completers and non-completers. Clinical Child Psychology and Psychiatry, 9, 347–361. doi:10.1177/1359104504043918.
Baekeland, F., & Lundwall, L. (1975). Dropping out of treatment: A critical review. Psychological Bulletin, 82, 738–783. doi:10.1037/h0077132.
Bauman, L. J. (2000). A patient-centered approach to adherence: Risks for nonadherence. In D. Drotar (Ed.), Promoting adherence to medical treatment in chronic childhood illness (pp. 71–93). Mahwah, NJ: Lawrence Erlbaum Associates, Inc.
Becker, M. H., Drachman, R. H., & Kirscht, J. P. (1972). Predicting mothers’ compliance with pediatric regimens. Journal of Pediatrics, 81, 843–854.
Becker, M. H., Radius. S. M., Rosenstock, I. M., Drachman, R. H., Shuberth, K. C., & Teets, K. C. (1978). Compliance with a medical regimen for asthma: A test of the Health Belief Model. Public Health Reports, 93, 268–277.
Boggs, S. R., Eyberg, S. M., & Edwards, D. L. (2004). Outcomes of parent–child interaction therapy: A comparison of treatment completers and study dropouts one to three years later. Child & Family Behavior Therapy, 26, 1–22. doi:10.1300/J019v26n04_01.
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press.
Chorpita, B. F., & Southam-Gerow, M. A. (2006). Treatment of anxiety disorders in youth. In E. J. Mash & R. A. Barkley (Eds.), Treatment of childhood disorders (3rd ed., pp. 271–335). New York: Guilford Press.
Chorpita, B. F., Yim, L. M., Donkervoet, J. C., Arensdorf, A., Amundsen, M. J., McGee, C., et al. (2002). Toward large-scale implementation of empirically supported treatments for children: A review and observations by the Hawaii empirical basis to services task force. Clinical Psychology: Science and Practice, 9, 165–190.
Chronis, A. M., Gamble, S. A., Roberts, J. E., & Pelham, W. E. (2006). Cognitive-behavioral depression treatment for mothers of children with attention-deficit/hyperactivity disorder. Behavior Therapy, 37, 143–158. doi:10.1016/j.beth.2005.08.001.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). New Jersey: Lawrence Erlbaum.
Cunningham, P. B., Foster, S. L., & Henggeler, S. W. (2002). The elusive concept of cultural competence. Children’s Services, 5, 231–243. doi:10.1207/S15326918CS0503_7.
Dierker, L., Nargison, J., Wiseman, R., & Hoff, D. (2001). Factors predicting attrition within a community initiated system of care. Journal of Child and Family Studies, 10, 367–383. doi:10.1023/A:1012581027044.
Dwight-Johnson, M., Sherbourne, C. D., Liao, D., & Wells, K. B. (2000). Treatment preferences among depressed primary care patients. Journal of General Internal Medicine, 15, 527–534. doi:10.1046/j.1525-1497.2000.08035.x.
Farmer, E. M. Z., Stangl, D. K., Burns, B. J., Costello, E. J., & Angold, A. (1999). Use, persistence, and intensity: Patterns of care for children’s mental health services across one year. Community Mental Health Journal, 35, 31–46. doi:10.1023/A:1018743908617.
Friedman, I. M., & Litt, I. F. (1987). Adolescents’ compliance with therapeutic regimens: Psychological and social aspects and intervention. Journal of Adolescent Health Care, 8, 52–67.
Garcia, J. A., & Weisz, J. R. (2002). When youth mental health care stops: Therapeutic relationship problems and other reasons for ending youth outpatient treatment. Journal of Consulting and Clinical Psychology, 70, 439–443. doi:10.1037/0022-006X.70.2.439.
Glisson, C. (2007). Assessing and changing organizational culture and climate for effective services. Research on Social Work Practice, 17, 736–747. doi:10.1177/1049731507301659.
Hammen, C., Rudolph, K., Weisz, J., Rao, U., & Burge, D. (1999). The context of depression in clinic-referred youth: Neglected areas in treatment. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 64–71. doi:10.1097/00004583-199901000-00021.
Harpaz-Rotem, I., Leslie, D., & Rosenheck, R. A. (2004). Treatment retention among children entering a new episode of mental health care. Psychiatric Services (Washington, DC), 55, 1022–1028. doi:10.1176/appi.ps.55.9.1022.
Huey, S., & Polo, A. (2008). Evidence-based psychosocial treatments for ethnic minority youth: A review and meta-analysis. Journal of Clinical Child and Adolescent Psychology, 37, 262–301. doi:10.1080/15374410701820174.
Kazdin, A. E. (1996). Dropping out of child psychotherapy: Issues for research and implications for practice. Clinical Child Psychology and Psychiatry, 1, 133–156. doi:10.1177/1359104596011012.
Kazdin, A. E., Holland, L., & Crowley, M. (1997). Family experience of barriers to treatment and premature termination from child therapy. Journal of Clinical and Consulting Psychology, 65, 453–463. doi:10.1037/0022-006X.65.3.453.
Kazdin, A. E., & Mazurick, J. L. (1994). Dropping out of child psychotherapy: Distinguishing early and late dropouts over the course of treatment. Journal of Consulting and Clinical Psychology, 62, 1069–1074. doi:10.1037/0022-006X.62.5.1069.
Kazdin, A. E., Mazurick, J. L., & Bass, D. (1993). Risk for attrition in treatment of antisocial children and their families. Journal of Clinical Child Psychology, 22, 2–16.
Kazdin, A. E., & Wassell, G. (1998). Treatment completion and therapeutic change among children referred for outpatient therapy. Professional Psychology, Research and Practice, 29, 332–340. doi:10.1037/0735-7028.29.4.332.
Kendall, P. C., & Sugarman, A. (1997). Attrition in the treatment of childhood anxiety disorders. Journal of Consulting and Clinical Psychology, 65, 883–888. doi:10.1037/0022-006X.65.5.883.
Klein, E. B., Stone, W. N., Hicks, M. W., & Pritchard, I. L. (2003). Understanding dropouts. Journal of Mental Health Counseling, 25, 89–100.
LaGreca, A. M., & Bearman, K. J. (2003). Adherence to pediatric treatment regimens. In M. C. Roberts (Ed.), Handbook of pediatric psychology (3rd ed., pp. 119–140). New York: The Guilford Press.
Lasalvia, A., Bonetto, C., Tansella, M., Stefani, B., & Ruggeri, M. (2007). Does staff-patient agreement on needs for care predict better mental outcome? A 4-year follow-up in a community service. Psychological Medicine, 38, 123–133.
Lau, A. S. (2006). Making the case for selective and directed cultural adaptations of evidence-based treatments: Examples from parent training. Clinical Psychology: Science and Practice, 13, 295–310. doi:10.1111/j.1468-2850.2006.00042.x.
Lau, A. S., & Weisz, J. R. (2003). Reported maltreatment among clinic-referred children: Implications for presenting problems, treatment attrition, and long-term outcomes. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 1327–1334. doi:10.1097/01.CHI.0000085754.71002.14.
Mak, W. W. S., Law, R. W., Alvidrez, J., & Pérez-Stable, E. J. (2007). Gender and ethnic diversity in NIMH-funded clinical trials: Review of a decade of published research. Administration and Policy in Mental Health and Mental Health Services Research, 34, 497–503. doi:10.1007/s10488-007-0133-z.
Martinez, C. R., & Eddy, J. M. (2005). Effects of culturally adapted parent management training on Latino youth behavioral health outcomes. Journal of Consulting and Clinical Psychology, 73, 841–851. doi:10.1037/0022-006X.73.5.841.
Masi, M. V., Miller, R. B., & Olson, M. M. (2003). Differences in dropout rates among individual, couple, and family therapy clients. Contemporary Family Therapy, 25, 63–75.
McClure, E. B., Connell, A. M., & Zucker, M. (2005). The Adolescent Depression Empowerment Project (ADEPT): A culturally sensitive family treatment for depressed African American girls. In E. D. Hibbs & P. S. Jensen (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice (2nd ed., pp. 149–164). Washington, DC: American Psychological Association.
McMahon, R. J., Wells, K. C., & Kotler, J. S. (2006). Conduct problems. In E. J. Mash & R. A. Barkley (Eds.), Treatment of childhood disorders (3rd ed., pp. 137–268). New York: Guilford Press.
McMiller, W. P., & Weisz, J. R. (1996). Help-seeking preceding mental health clinic intake among African-American, Latino, and Caucasian youths. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 1086–1094. doi:10.1097/00004583-199608000-00020.
Meichenbaum, D., & Turk, D. C. (1987). Facilitating treatment adherence: A practitioner’s guidebook. New York: Plenum Press.
Miller, W. R., & Rollnick, S. (2002). Motivational interviewing: Preparing people for change. New York: Guilford.
Nock, M. K., & Kazdin, A. E. (2001). Parent expectancies for child therapy: Assessment and relation to participation in treatment. Journal of Child and Family Studies, 10, 155–180. doi:10.1023/A:1016699424731.
Nock, M. K., & Kazdin, A. E. (2005). Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology, 73, 872–879. doi:10.1037/0022-006X.73.5.872.
Pina, A. A., Silverman, W. K., Weems, C. F., Kurtines, W. M., & Goldman, M. L. (2003). A comparison of completers and noncompleters of exposure-based cognitive and behavioral treatment for phobic and anxiety disorders in youth. Journal of Consulting and Clinical Psychology, 71, 701–705. doi:10.1037/0022-006X.71.4.701.
Prinz, R., & Miller, G. (1994). Family-based treatment for childhood antisocial behaviour: Experimental influences on dropout and engagement. Journal of Consulting and Clinical Psychology, 62, 645–650.
Pumariega, A. J., Glover, S., Holzer, C. E., & Nguyen, H. (1998). Utilization of mental health services in a tri-ethnic sample of adolescents. Community Mental Health Journal, 34, 145–156.
Schoenwald, S. K., & Hoagwood, K. (2001). Effectiveness, transportability, and dissemination of interventions: What matters when? Psychiatric Services (Washington, DC), 52, 1190–1197. doi:10.1176/appi.ps.52.9.1190.
Siqueland, L., Crits-Cristoph, P., Gallop, R., Barber, J. P., Griffin, M. L., Thase, M. E., et al. (2002). Retention in psychosocial treatment of cocaine dependence: Predictors and impact on outcome. The American Journal on Addictions, 11, 24–40. doi:10.1080/10550490252801611.
Southam-Gerow, M. A. (2005, Summer). Using partnerships to adapt evidence-based mental health treatments for use outside labs. Report on Emotional & Behavioral Disorders in Youth, 5, 58–60, 77–79.
Southam-Gerow, M. A., Austin, A. A., & Marder, A. M. (2008a). Transportability and dissemination of psychological treatments: Research models and methods. In D. McKay (Ed.), Handbook of research methods in abnormal and clinical psychology (pp. 203–224). Newbury Park, CA: Sage.
Southam-Gerow, M. A., Chorpita, B. F., Miller, L. M., & Gleacher, A. A. (2008b). Are children with anxiety disorders privately-referred to a university clinic like those referred from the public mental health system? Administration and Policy in Mental Health and Mental Health Services Research, 35, 168–180. doi:10.1007/s10488-007-0154-7.
Southam-Gerow, M. A., Ringeisen, H. L., & Sherrill, J. T. (2006). Introduction to special issue: Integrating interventions and services research: Progress and prospects. Clinical Psychology: Science and Practice, 13, 1–8. doi:10.1111/j.1468-2850.2006.00001.x.
Southam-Gerow, M. A., Weisz, J. R., & Kendall, P. C. (2003). Youth with anxiety disorders in research and service clinics: Examining client differences and similarities. Journal of Clinical Child and Adolescent Psychology, 32, 375–385. doi:10.1207/S15374424JCCP3203_06.
Sparks, W. A., Daniels, J. A., & Johnson, E. (2003). Relationship of referral source, race, and wait time on preintake attrition. Professional Psychology: Research and Practice, 5, 514–518.
Sue, S. (1998). In search of cultural competence in psychotherapy and counseling. The American Psychologist, 53, 440–448. doi:10.1037/0003-066X.53.4.440.
United States Public Health Service. (1999). Mental health: A report of the surgeon general. Washington, DC: United States Public Health Service.
United States Public Health Service. (2000). Report of the surgeon general’s conference on children’s mental health: A national action agenda. Washington, DC: United States Public Health Service.
Weisz, J. R., McCarty, C. A., & Valeri, S. M. (2006). Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin, 132, 132–149. doi:10.1037/0033-2909.132.1.132.
Weisz, J. R., Southam-Gerow, M. A., Gordis, E. B., & Connor-Smith, J. K. (2003). Primary and secondary control enhancement training for youth depression: Applying the deployment-focused model of treatment development and testing. In A. E. Kazdin & J. R. Weisz (Eds.), Evidence-based treatments for children and adolescents (pp. 165–183). New York: Guilford.
Werba, B. E., Eyberg, S. M., & Boggs, S. R. (2006). Predicting outcome in parent–child interaction therapy: Success and attrition. Behavior Modification, 30, 618–646. doi:10.1177/0145445504272977.
Wierzbicki, M., & Pekarik, G. (1993). A meta-analysis of psychotherapy dropout. Professional Psychology, Research and Practice, 24, 190–195. doi:10.1037/0735-7028.24.2.190.
Yeh, M., McCabe, K., Hough, R. L., Lau, A., Fakhry, F., & Garland, A. (2005). Why bother with beliefs? Examining relationships between race/ethnicity, parental beliefs about causes of child problems, and mental health service use. Journal of Consulting and Clinical Psychology, 73, 800–807. doi:10.1037/0022-006X.73.5.800.
Zimmerman, F. J. (2005). Social and economic determinants of disparities in professional help-seeking for child mental health problems: Evidence from a national sample. Health Services Research, 40(5 Pt 1), 1514–1533. doi:10.1111/j.1475-6773.2005.00411.x.
Acknowledgments
Preparation of this article was supported in part through a grant from the National Institute of Mental Health Grant K23 MH69421. Portions of this manuscript were submitted in partial fulfillment of a Master’s in Science degree by Lauren M. Miller.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miller, L.M., Southam-Gerow, M.A. & Allin, R.B. Who Stays in Treatment? Child and Family Predictors of Youth Client Retention in a Public Mental Health Agency. Child Youth Care Forum 37, 153–170 (2008). https://doi.org/10.1007/s10566-008-9058-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10566-008-9058-2