Abstract
Background
The majority of youth with mental health needs do not receive therapy services to treat their disorder, and unmet need is particularly high among racial and ethnic minorities and economically disadvantaged families in the population at large. Investigating whether these patterns emerge within systems of care can reveal opportunities to expand therapy access and utilization.
Objective
This study examines multilevel predictors of receipt of therapy within the Children’s Mental Health Initiative (CMHI), the largest federally-funded effort in the United States to serve youth with significant emotional or behavioral disturbance, to determine whether disparities in therapy use persist within this specialized population that has been connected to a service array.
Method
Using data from 1604 youth aged 10–17 in 33 CMHI-funded system of care sites, the relationship between youth, family and site-level variables and the receipt of outpatient therapy in the first 6 months of service were examined using a multilevel model.
Results
Youth who were African American, had caregivers with less education, were in families at or below the poverty level, or lived in sites that served a higher rate of families below the poverty level were less likely to receive needed therapy services after controlling for age, gender, and symptomatology.
Conclusions
Despite the CMHI’s success in connecting the majority of enrolled youth to therapy services, treatment disparities persist along racial and socioeconomic lines. These findings identify youth and communities that may require additional strategies and attention to better connect youth to needed therapy services.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite advances in empirically supported mental health interventions and efforts to expand access to mental health care, the majority of youth with diagnosable mental health disorders do not receive mental health services to treat their disorder (Angold et al. 1998; Flisher et al. 1997; Horwitz et al. 2003; Kataoka et al. 2002). In a nationally representative sample, only 36% of youth with mental disorders and 50% of youth with severe levels of impairment received mental health treatment services for their symptoms (Merikangas et al. 2011). The Comprehensive Community Mental Health Services for Children and Their Families Program, also called the Children’s Mental Health Initiative (CMHI), is the largest federally-funded national effort to address this treatment gap. The CMHI seeks to provide community-based child and adolescent mental health services to youth with significant emotional or behavioral disturbance and is based on the system of care model (Huang et al. 2005; Stroul and Friedman 1986). The system of care approach strives to ensure access to community-based services and supports that are culturally competent, family and youth driven, and individualized to the strengths and needs of each family. In order to reduce barriers to care, the model calls for interagency collaboration between all child and family-serving agencies from the public, private, and faith-based sectors and wraparound service planning that creates a coordinated network of services and supports. Upon enrollment to the CMHI, the model dictates that each youth is connected to a care coordinator who helps organize wraparound services that incorporate formal and informal supports. From its inception in 1993, the CMHI has funded systems of care in 173 sites across the country. The CMHI has been successful in enrolling populations with mental health needs, including those that have often been underserved, such as families living below the federal poverty line and racial and ethnic minorities (CMHS 2016; Miech et al. 2008). Evaluations of the CMHI have found positive outcomes for youth receiving services, including significant improvements in behavioral and emotional symptoms, reductions in suicidal ideation and attempts, increases in school attendance, and reductions in hospitalization and arrest costs (CMHS 2016). These successes have led to continued federal funding and dissemination through System of Care Expansion and Sustainability Grants and Cooperative Agreements, with the goal of bringing the system of care model to scale. However, it is not clear whether the model as currently implemented is sufficient to overcome long-standing patterns of treatment disparities observed in mental health care. As the system of care model is expanded and disseminated, it is important to continue evaluating the experiences of youth within care. This study examines whether mental health treatment disparities that are well-documented in the population at large are reproduced within youth enrolled in the CMHI, with a focus on the receipt of therapy services. Unlike most prior studies, we examine this question in a multilevel context, enabling the investigation not only of individual and family characteristics but also of site-level factors that may impact access to and engagement with mental health services.
Youth within systems of care are a unique sample in which to examine receipt of therapy. By virtue of their enrollment in CMHI, they have already been identified as having emotional and behavioral health needs and are connected to at least one element of the local system of care. Thus, they have already overcome two potential barriers to receiving needed care—recognition as requiring additional services and connection to a service array. Highlighting groups that are less likely to receive needed therapy services even after being enrolled in a system of care can help to identify gaps within the service model, inform efforts to improve utilization of therapy, and point towards potential structural barriers and inefficiencies that limit the potential of the CMHI as it is scaled up.
Underserved Populations in the United States
Racial and Ethnic Minorities
Extensive research has found that race and ethnicity are associated with the use of mental health services in the United States, with greater unmet need among Latinx (used as a gender-neutral and non-binary alternative to Latino or Latina) and African-Americans in the population at large (Smedley et al. 2002; Snowden and Yamada 2005). While racial and ethnic disparities in mental health service use have been found to be smaller within high-poverty neighborhoods and Medicaid-enrolled populations (Chow et al. 2003; Snowden and Thomas 2000), they have emerged in high-poverty samples as well (Thompson 2005). These differences have also been found within youth already connected to a public sector of care (e.g., alcohol and drug abuse, child welfare, juvenile justice, mental health, and public school special education services; Garland et al. 2005; Hurlburt et al. 2004).
Families with Lower Socioeconomic Status
In addition to race and ethnicity, family socioeconomic status is a well-studied predictor of unmet need. In nationally representative and unselected samples, economic disadvantage has been linked to greater unmet mental health needs in children (Cohen and Hesselbart 1993; Cunningham and Freiman 1996; Flisher et al. 1997; Haines et al. 2002; Kataoka et al. 2002), though not in all samples (Zimmerman 2005; Thompson 2005). Beyond poverty, a caregiver’s ability to navigate the system and advocate for their child may also be an important predictor of service use. There is some evidence that children with more educated parents are more likely to receive specialty mental health services (Farmer et al. 1999), though not all work has not found this effect (Thompson 2005; Zimmerman 2005).
Underserved Localities
Geographically, demand for and supply of health care services are not distributed equally, creating the potential for community factors to shape individual access to and engagement in mental health care (Johnson et al. 2017; Probst et al. 2004). There is a shortage of mental health care providers in many U.S. counties, particularly those that are rural or have low per-capita income (Thomas et al. 2009). Investigations of access to primary health care have found that racial segregation and higher concentrations of minorities are associated with worse access to a usual source of health care for African Americans (Caldwell et al. 2017). Similarly, higher concentrations of community poverty and “neighborhood disadvantage” (a composite scale of community poverty, community unemployment, and community education level) are negatively associated with having a usual source of health care and receiving recommended prevention services, even when including individual level disadvantage in the model (Kirby and Kaneda 2005; Litaker et al. 2005). Thus, there is reason to believe that access to mental health services may also be impacted by locality factors such as economic and racial/ethnic makeup.
Use of Therapy Services Within the CMHI
Race and Ethnicity
There is some extant research investigating whether these disparities are reproduced within the CMHI, particularly in regards to racial and ethnic minority status. Popescu et al. (2015) found that in 55 sites funded from 2002 to 2006 (phases 4 and 5), African American youth had lower odds of using individual, family, or group psychotherapy and those who did receive therapy used fewer days than non-Hispanic White youth. Additionally, among those who received therapy, Latinx youth received fewer days of individual, family, and group therapy than non-Hispanic White youth. These disparities were more modest than those reported in the general population (Kataoka et al. 2002), but still significant. The current study will confirm whether this finding emerges in later phases of the CMHI. Importantly, it will do so using a multilevel model that can distinguish racial and socio-economic effects from other youth, family, and site characteristics.
Socioeconomic Status
Family socioeconomic status has been examined to a limited extent within the CMHI, but has not been previously investigated as a predictor of youth therapy across multiple CMHI sites. In a study of grant communities funded in 1997–2000, it was found that families living below the poverty threshold received fewer support and treatment services overall, but there was no significant difference for outpatient mental health services (Gyamfi 2004). In one CMHI-funded system of care implemented in Chicago Public Schools, a non-linear relationship was found between caregiver education and days of community mental health service. Youth with the highest and lowest-educated caregivers received more days of services than youth of caregivers with a moderate (high school diploma or GED) level of education (Burnett-Zeigler and Lyons 2010). As the system of care model attempts to make services more cohesive and navigable for families and enable access irrespective of income, it is important to examine current differences in therapeutic care related to family socioeconomic status across CMHI sites. Investigating the extent to which youth receipt of therapy is related to caregiver poverty level or education may help to identify structural factors that limit access to therapy services. This study will expand our current understanding of treatment disparities by investigating family poverty level and caregiver education as predictors of therapy across CMHI sites, which has not previously been looked at. We hypothesize that youth living in families below the poverty line and youth with caregivers with less education will be less likely to receive needed therapy services.
Site Factors
With system of care sites spread across the country, there is a unique opportunity to examine site-level factors that impact youth contact with therapy services. Though there is reason to believe that access may vary across geographic locations, previous studies have not investigated site characteristics that predict receipt of therapy services. Implementation of the system of care model has varied between sites (Brannan et al. 2012; Vinson et al. 2001), and communities have different availability of services and resources. System of care sites that serve higher rates of disadvantaged populations may encounter greater limitations in terms of community resources and available mental health care providers. Based on previous work suggesting that health care in general may vary according to community-level poverty and the density of minority populations (e.g., Caldwell et al. 2017; Kirby and Kaneda 2005; Litaker et al. 2005), we will examine both economic makeup (the percent of the youth enrolled in the site who are at or below the poverty level) and racial/ethnic makeup (the percent of the youth enrolled who are white) as potential predictors of receipt of therapy services. We hypothesize that youth in sites that serve a higher proportion of families living below the poverty level will be less likely to receive therapy services, and youth in sites with a higher proportion of white enrollees will be more likely to receive therapy services.
Isolating the Effects of Race, Socioeconomic Status, and Site
Several additional factors stand as potential confounds for isolating the effects of race, poverty level, caregiver education, and site on youth receipt of therapy. While all youth within the CMHI have identified mental health needs, level and type of symptomatology may still reflect varying intensity of need and impact the receipt of therapy. While level of symptomatology has been found to predict use of mental health services outside of the CMHI (Burns et al. 1995; Farmer et al. 1999), a previous study of 89 youth in a single system of care site found that child dysfunction did not predict receipt of family or individual therapy (Graves et al. 2009). This may be explained by the restricted range of symptomatology experienced by youth within the CMHI, as all youth have identified mental health needs. In addition to the severity, the manifestation of youth problems may shape whether or not they receive services. In general populations, youth with externalizing problems may be more likely to receive services than youth with internalizing problems (Thompson 2005; Thompson and May 2006). This has been found to be especially true for minority and immigrant populations as compared to non-Hispanic Whites (Gudiño et al. 2008, 2009). Thus, controlling for level of youth symptomatology, including both internalizing and externalizing problems, is important for investigating gaps in the provision of therapy services that are not explained by intensity of need. We will also control for youth demographics that have been inconsistently linked to receipt of mental health services. In nationally representative or unselected samples, there is conflicting evidence on the relationship between gender and receipt of mental health services (Zimmerman 2005; Cohen and Hesselbart 1993; Flisher et al. 1997; Verhulst and van der Ende 1997). There is some evidence that girls may be less likely to be perceived as needing mental health intervention (Thompson 2005) or use mental health services, but more likely to receive high-intensity treatment once identified (Farmer et al. 1999). Youth age has also been inconsistently linked to mental health service receipt, with effects found primarily in samples with broader age ranges, particularly youth under six and transition-aged children (Kataoka et al. 2002; Pottick et al. 2007). We will include gender and age in our models as demographic controls.
Current Study
As the largest federally funded initiative to serve youth with serious emotional or behavioral disturbance, the CMHI is in a unique position to address the treatment gap in adolescent mental health care. However, it is not yet clear the extent to which the CMHI and the system of care model are currently meeting their potential to address long-standing service disparities in access to therapy. Stubborn patterns of service access and use may be still be at play among youth enrolled in CMHI, despite the unique efforts taken to connect these youth to needed services. This study seeks to replicate and extend previous investigations of therapy in systems of care that identified racial and ethnic disparities in earlier phases of CMHI. In addition to race and ethnicity, we will examine socioeconomic factors (family poverty and caregiver education) that have not yet been examined as predictors of therapy across CMHI sites. Further, this study moves beyond the individual level to incorporate novel potential site-level predictors of therapy utilization. As the CMHI model is expanded and disseminated, it is important to evaluate the ways in which it is and is not sufficient to overcome stubborn treatment inequalities. We hypothesize that race, socioeconomic status, and site-level characteristics will significantly predict the receipt of therapy when controlling for symptomatology, such that (1) non-Hispanic White youth will be more likely to receive therapy than African American or Latinx youth; (2) youth in families who are living in poverty will be less likely to receive therapy; (3) youth of caregivers who have less education will be less likely to receive therapy; (4) youth living in sites where the CMHI serves more families at or below the poverty line will be less likely to receive therapy; and (5) youth in sites where there is a higher percentage of white enrollees will be more likely to receive therapy. As there is less conclusive evidence on the relationships between age and gender and therapy utilization, we do not include them in our hypotheses but will control for these demographic variables. Similarly, though all youth within this sample have mental health needs, these analyses will control for youth problem behaviors as it may reflect intensity of need. To account for the dependencies created by the nested structure of the data and to investigate multilevel characteristics simultaneously, we will utilize a hierarchical model to predict the receipt of therapy.
Method
Data
The data examined in this study were collected as part of the longitudinal outcome study of the National Evaluation of the CMHI. Confidentiality and patient protection in the data collection process were managed by SAMHSA and individual funded sites and varied across location, but all youth and caregivers provided informed consent/assent before participating in data collection. Prior to conducting analyses, we obtained an exemption from the Institutional Review Board at University of Illinois at Urbana-Champaign for these secondary analyses as the data were pre-existing and de-identified.
Youth enrolled in CMHI-funded systems of care were eligible for the longitudinal outcome study if they had a caregiver or legal custodian who would grant consent and was capable of completing a data collection interview, did not have a sibling who was already enrolled in the outcome study, were enrolled or enrolling in system of care services at the time of the baseline outcome study interview, and were between 5 and 17.5 years of age at the time of the baseline interview. In addition, some sites had sampling schemes to select a subset of youth for the longitudinal outcome study.
Data were drawn from sites funded in 2008, 2009, and 2010 and come from 47 system of care sites across the country. The sample was reduced to youth who were age 10–17 at the time of the enrollment, to focus on adolescents under the age of majority. This narrowed the data to 39 communities. Six communities were dropped because they had fewer than ten youth with sufficient data in these age ranges, leaving a total of 33 communities represented in the sample.
A total of 9083 youth aged 10 to 17 were enrolled in the system of care. Out of these youth, 3607 participated in the longitudinal outcome study. Common reasons for not participating in the longitudinal outcome study included missing the 30 day baseline data collection window (28.2%), failure to collect consent from the caregiver or independent youth (27.1%), delay in local evaluation procedures (11.9%), ineligibility because a sibling was enrolled in the study (6.2%), or ineligibility because the youth was not selected through the site’s sampling scheme (4.2%). Out of the 3607 youth enrolled in system of care services and in the longitudinal outcome study, 1604 completed the measures required for this study at intake and 6 months and are included in our analyses. The majority of the 2003 youth who are enrolled in the longitudinal outcome study but not in our sample were lost to follow-up at 6 months and therefore did not have data on service usage (1700 youth).
Participants
Participants in our sample were predominately male (60%) with a mean age of 14 (SD = 2.15). Youth were predominately White (43%), African American (24%), or Hispanic/Latinx (20%). In regards to family characteristics, 51% of caregivers had a high school degree or less and 73% were near or below the poverty level. Characteristics of our sample as compared to other youth aged 10–17 who were enrolled in system of care services but are not in our sample are presented in Table 1. Our sample is slightly younger (mean difference of 2.3 months) and reflects a slightly different racial makeup (7% more White youth) than those enrolled in the longitudinal outcome study but not in our sample. Youth in our sample had significantly higher total problem, externalizing, and internalizing scores at baseline (1.8 points, 1.4 points, and 1.6 points higher, respectively) as compared to youth enrolled in the longitudinal outcome study but not in our sample.
The CMHI is intended to serve youth with serious emotional and behavioral disturbance, which is reflected in our sample. Ninety three percent of the youth had a DSM or ICD diagnosis at the time of intake, as indicated on their Enrollment and Demographic Information Form (EDIF) completed at the baseline interview. Diagnoses came from a qualified professional (e.g., licensed clinical social worker, psychiatrist, mental health assessment specialist staff) either prior to intake or at intake if needed; 40% of youth in the sample received a diagnostic evaluation as part of their intake into the system of care. The most common diagnoses were mood disorders (49%), attention deficit hyperactivity disorder (40%), oppositional defiant disorder (22%), substance use disorder (12%), anxiety disorders (10.7%), and PTSD and acute stress disorder (9%). The majority of youth had diagnoses in two or more categories (67%). Caregivers reported high rates of problem behaviors on the CBCL; the mean total problems T score was 69.6 (SD = 9.9), which is considered to be in the clinical range (cutoff = 63). The mean externalizing score was 69.3 (SD = 10.6) and the mean internalizing score was 66.2 (SD = 10.5).
Measures
Demographic information (race/ethnicity, age, gender, poverty level, and caregiver education) was collected at intake using the Enrollment and Demographic Information Form (EDIF) and the Caregiver Information Questionnaire, Revised (CIQ-R). These measures were designed for the National Evaluation to capture uniform demographic information about youth and caregivers from all sites. Race/ethnicity categories in the EDIF included American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian, White, Hispanic, and Multiracial. Due to insufficient number and distribution, some categories could not be adequately investigated in a multilevel analysis and we therefore collapsed race/ethnicity into four categories (non-Hispanic White, Black/African American, Latinx/Hispanic, and Multiracial/Other) for the analysis. We use Black and African American interchangeably in discussing this sample. Caregiver education was collected as a four-level categorical variable based on caregiver report. Poverty level was used in this analysis instead of family income because it is adjusted for family size and location and thus better reflects need across a national sample. Poverty level was calculated using thresholds provided by the Department of Health and Human Services (HHS). Families above the poverty line had incomes more than 1.5 times the poverty threshold; families at/near the poverty line had incomes 1–1.5 times the threshold.
Service use was assessed using the Multi-Sector Service Contact (MSSC-R), a caregiver-report measure created by Macro International, Inc. to investigate the types and frequencies of services received by children and families in the National Evaluation. A dichotomous variable indicating whether the youth had received therapy in the first 6 months of enrollment in the system of care was created using three items (family therapy, group therapy, and individual therapy). Previous work with similar measures suggests that caregiver report of child service use is reasonably consistent with provider report (Ascher et al. 1996; Hoagwood et al. 2000).
Youth mental health problems at intake were assessed using the Child Behavior Checklist (CBCL 6–18; Achenbach 1991), a standardized caregiver-report measure of emotional and behavioral problems. The CBCL has demonstrated good internal consistency, test–retest reliability, construct validity, and criterion-related validity (Achenbach and Rescorla 2001). T-scores based on population norms were used for the total problems, externalizing, and internalizing scales because they adjust for age and gender.
Level two variables were created by aggregating all available data on youth enrolled in CMHI at each site. Site-level poverty was calculated as the percent of youth enrolled in the site whose families were at or below the poverty level. Percent white was calculated as the percent of youth enrolled in the site who identified as non-Hispanic White. These aggregated variables are not just reflective of the youth in the analytic sample (N = 1604), but of all youth enrolled in CMHI with available data (N = 3607).
Analysis
Before conducting hierarchical analyses to test our main hypotheses, we conducted descriptive analyses to look at the univariate relationships between our predictors of interest and receipt of therapy in a single-level context. For race, family poverty, and caregiver education, we calculated the percent of youth who received therapy for each category and tested mean differences using a one-way ANOVA. For the site-level predictors, we calculated the percent of youth in each site who received therapy and correlated this with the site characteristics across the 33 sites.
To address our main hypotheses, a multilevel logistic regression with community as the clustering variable was used to examine predictors of receipt of therapy services. The intraclass correlation coefficient (ICC) was calculated to estimate the percentage of total variability that can be accounted for by between-site differences. Continuous level one predictors (age, CBCL total problems, CBCL internalizing, and CBCL externalizing) were group-centered, in order to investigate the impact of these variables within each system of care.
Youth demographics (age and gender) and our level one predictors (race, caregiver education, poverty level, and CBCL total problems) were all entered in one step. Site-level poverty and percent white were added in a second step. As the only significant differences in caregiver education emerged at the cutpoint between “high school diploma or GED” and more education, this categorical variable was collapsed into these two categories. For the same reason, family poverty level was collapsed into “above the poverty level” and “at/near/below the poverty level”. During model refinement, the level two variables (site poverty and percent white) were removed from the final models when non-significant; all other variables remained in the final model. Analyses were run using the SAS software system version 9.4, using the PROC GLIMMIX procedure (SAS Institute Inc, Cary, North Carolina). Laplace’s method was used to approximate the marginal likelihood.
Results
Descriptives and Univariate Relationships
Overall, 72% of the sample received at least one session of therapy during the 6-month period. The most common therapy received was individual therapy (received by 68% of the sample); group therapy and family therapy were less common (20% and 24%, respectively). For those who received at least one session of any therapy, the median and modal number of total sessions was 24 (mean = 29.2). Most youth who received therapy received more than a few sessions; only 10.4% received fewer than five sessions.
There were statistically significant differences in problem behaviors across our predictors at baseline (see Table 2). Non-Hispanic White youth had, on average, higher total problem scores than African American youth (mean difference = 3.5 points) and Latinx youth (mean difference = 3.0 points). Youth of caregivers with a high school degree or less had slightly lower problem scores than those who had caregivers with more education (mean difference = 1.2 points). While these mean scores are all above the clinical cutoff of 63, this variability in problem behaviors within the clinical range may still reflect meaningful variation in intensity of need. Thus, total problem score was controlled for in all analyses.
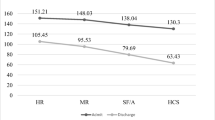
The univariate relationships between our predictors of interest and the receipt of therapy are presented in Table 3. The percent of youth who received therapy varied significantly by race. Post-hoc comparisons using the Tukey’s HSD test indicated that the only significant differences emerged between African-Americans and other groups, with a lower percentage of African-American youth receiving therapy (63.4%) as compared to White (74.3%) and Latinx (79.7%) youth. Similarly, a smaller percentage of youth in families living at or below the poverty line received therapy (69.6%) as compared to those living above the poverty line (80.1%). A smaller percentage of youth with caregivers with a high school degree or less education received therapy (69.2%) as compared to youth with caregivers with more education (75.9%). Youth who received therapy had, on average, higher CBCL total problem scores than youth who did not receive therapy (mean difference = 1.84, F = 11.2, p < .05). At the site level, there was a significant negative correlation between the percent of youth in the site who were below the poverty level and the percent of sample youth who received therapy (r = − .42, p < .05). There was not a significant correlation for percent white.
Multilevel Model
The intraclass correlation coefficient (ICC) calculated using the null model was .18, suggesting that 18% of the variation in whether a youth receives therapy was at the site level. Consistent with our hypothesis, race remained a significant predictor in the multilevel logistic regression after accounting for the variability explained by age, gender, caregiver education, poverty level, CBCL total problems, and site-level poverty (Table 4). Black youth were less likely to receive therapy than White youth; the odds that a Black youth received therapy were .71 times the odds of a White youth. Also consistent with our hypotheses, in regards to family characteristics, caregiver education and poverty level were both significantly predictive of receipt of therapy. Youth with caregivers who had attained a high school degree or less were less likely to receive therapy than youth with caregivers who had education beyond a high school degree (OR = .76). Youth in families near or below the poverty level were less likely to receive therapy than those above the poverty level (OR = .73).
At the site level, consistent with our hypothesis, aggregated poverty status did significantly predict receipt of therapy. Youth living in communities where the system of care served more families below the poverty line were less likely to receive therapy (OR = .77 where the poverty rate of families in the system of care was 10% higher than the full sample average). The percent of SOC enrollees who were white was not a significant predictor of receipt of therapy.
In addition to the total problems scale on the CBCL, a post-hoc model was run to investigate any unique impacts of the internalizing and externalizing subscales. These subscales were significantly correlated (r = 0.53) and did not uniquely predict receipt of therapy overall (i.e., one was not significantly predictive above and beyond the other).
To ensure that the unequal distribution of Latinx youth did not create model estimation problems, the analysis was re-run in a single-level regression using just the two communities that contained the plurality of Latinx youth. Race did not reach significance in this model.
While most youth who received therapy were in treatment for a substantial number of sessions (mean = 29), some youth received very few sessions (10.4% received fewer than five sessions). In order to examine the effect that this minority had on the results, all analyses were run a second time excluding youth who received fewer than five sessions of therapy. No substantive differences emerged in the results.
Discussion
Despite advances in psychotherapy interventions for children and adolescents, there is an alarming treatment gap for youth with mental disorders (Merikangas et al. 2011). Importantly, our findings show that within the CMHI, an extraordinarily high percent of youth are connected to therapy services as compared to youth in the population at large. In our sample of youth in 33 sites, 72% of youth received at least one session of therapy during the first 6 months of enrollment in the CMHI. This is substantially higher than estimates found in the US population at large; for example, a national survey in 2002–2004 found that only 36% of youth with mental disorders received mental health treatment services for their symptoms (Merikangas et al. 2011). This overall rate of therapy suggests that the system of care model as implemented in the CMHI is successful in connecting enrolled youth to therapy at a substantially higher rate than in the general population.
In the context of this high rate of therapy utilization, receipt of therapy still varied based on race, family poverty, caregiver education, and site-level poverty after controlling for mental health problem behaviors. These results suggest that despite the success that CMHI has achieved in connecting youth to services, disparities persist in access to and engagement with therapy. These findings can provide information about populations that may be underserved and about potential structural barriers to care that persist within the CMHI.
As predicted in hypothesis 1, race was a significant predictor of therapy, such that African American youth were less likely than non-Hispanic White youth to receive therapy. While not unexpected as this matches a pattern commonly found in services research (e.g., Kataoka et al. 2002), this finding is disheartening as it suggests that racialized service differences still exist in federally-funded systems of care. This finding was largely consistent across nearly all sites; in all but 6 out of the 33 sites, a lower percentage of African American youth received therapy than White youth. The odds ratio for African American youth found in this study (.70) is similar to the odds ratio reported by Popescu et al. in phases 4 and 5 (2002–2006) of the CMHI (.73), suggesting consistency across funding years. As indicated by Popescu et al., these racial differences in service use within the CMHI are more modest than those that have been found in the general population. Nonetheless, these racial disparities are concerning, particularly in the context of a steep increase in suicidal behavior among African American youth over the past 20 years (Lindsey et al. 2017). Suicide rates for African American males in particular have increased at a rate outpacing other racial demographics; a 2015 study found that the rate of suicide among Black youth age 10–11 doubled from 1993 to 2012, resulting in the highest suicide rate among all youth racial and ethnic groups (Bridge et al. 2015). That Black youth are still less likely to receive therapy even when enrolled in a system of care is a critical disparity that must be overcome in order to address this trend.
In contrast to previous research conducted outside of the CMHI (Garland et al. 2005; Kataoka et al. 2002) and inconsistent with our hypothesis, Latinx youth were not less likely to receive therapy services as compared to non-Hispanic White youth. Further, estimates for Latinx youth were positive in all models, though these effects did not reach significance. This result should be interpreted with caution, however, as the plurality of Latinx youth (41%) came from two communities and the finding may not generalize across the sample as a whole. Studies of earlier stages of the CMHI also found that Latinx youth did not have lower odds of receiving therapy services as compared to non-Hispanic White youth (Popescu et al. 2015). Taken together with the results for African American youth, this finding suggests that the CMHI may be addressing service utilization in Latinx youth more successfully than in African American youth. Once identified as having a mental health need and connected to a system of care, Latinx youth are no less likely to be engaged in therapy services than non-Hispanic White youth.
Consistent with hypothesis 2, poverty level was significantly predictive of group therapy and therapy overall, such that youth in families above the poverty level were more likely to receive therapy. This may reflect limited capacity for low-resource, stressed families to navigate a complicated system and advocate for and attend additional services. Poverty has long been associated with transportation barriers (Sanchez 2008) that can limit access to healthcare (Syed et al. 2013). Families living in poverty may also have greater distrust of health care and other services (Canvin et al. 2007; Katapodi et al. 2010). This relationship could also reflect a difficulty in paying for these services or a lack of local providers who accept Medicaid.
As predicted in hypothesis 3, caregiver education was significantly predictive of therapy, such that youth of caregivers who had education beyond a high school degree were more likely to receive therapy. Notably, this cannot be explained by a relationship between caregiver education and poverty, as this finding emerged above and beyond the effect of poverty status. Caregivers with a higher level of education may be better able to navigate service systems and advocate for their child. Longitudinal evaluation of the CMHI suggests that sites have struggled to fully implement the principle of interagency collaboration (Brannan et al. 2012). Improving this may foster a more cohesive service array that is more easily navigable for caregivers. Additionally, previous literature has suggested that parents with more years of education may be more likely to identify that their child needs special health care services (Porterfield and McBride 2007). The system of care aims to create a service network that is family driven and youth guided, and therefore relies to some extent on caregiver’s perceptions of their child’s specific needs. Family and community education on symptoms of psychopathology and effective therapy interventions may be instrumental in improving utilization of potentially beneficial services.
Average rate of receipt of therapy varied significantly between sites; 18% of the variability in receipt of therapy was explained by the site. Consistent with hypothesis 4, site-level aggregated poverty (percent of CHMI-enrolled families living below the poverty line) was associated with receipt of therapy, over and above the impact of family poverty. This novel finding calls attention to the importance of aggregated disadvantage beyond the impact of individual financial constraints. Site differences in receipt of therapy may be related to availability of mental health community services, as poor communities are more likely to have a severe shortage of mental health care providers (Thomas et al. 2009). One of the goals of the CMHI is to increase and improve the array of services available to youth, but this is a challenging task. Brannan et al. (2012) found that nearly all sites in phases II, III, and IV reported difficulties in service capacity, but did not investigate site-level poverty or other site characteristics as possible correlates of service array deficits. Though the CMHI is a national initiative, this finding suggests that sites had varying levels of success with connecting youth to therapy services, and sites serving higher rates of families living in poverty may require additional attention and support to address this particular gap. Contrary to our hypothesis 5, the racial makeup of the sites, as measured by percent of enrollees who were White, was not a significant predictor of receipt of therapy. The role of race in predicting receipt of therapy is primarily at the individual level, and not a function of the aggregate community.
The National Academy of Medicine (formerly the Institute of Medicine, IOM) defines a disparity as a difference in health care treatment that is not due to differences in health care needs or preferences of the patient (Smedley et al. 2002). However, disparities research is rarely able to control for patient preference (McGuire et al. 2006). The current study cannot disentangle the role of individual and family preference, accessibility (e.g., financial, transportation, or time constraints), availability of culturally appropriate care, discrimination, distrust of health care providers, and other possible factors in explaining the reported patterns of utilization. In future research, closer examination of these factors is needed to inform additional strategies to expand access to and use of therapy, particularly for the groups identified in this study. For example, if African American youth are less likely to be referred to needed therapy services, education of care coordinators and monitoring of racial differences in service referral would be a step towards addressing this disparity. If African American youth are just as likely to be referred to needed therapy services but less likely to use them, approaches that focus on reducing stigma towards therapy or improving the cultural competency of available services is warranted. Importantly, patient preference may still reflect current or past inadequacies in the system. Low expectations for treatment may stem from previous negative experiences with mental health care, cultural mistrust based in historical maltreatment, or lack of access to providers that belong to one’s race, gender, or religious background (Cooper-Patrick et al. 1997). Expanding multicultural education and training within systems of care may help to improve cultural competency of caseworkers, care coordinators, and local mental health service providers (Smith et al. 2006). Another factor that may influence the use of therapy services is the availability of African American therapists in the community. There is evidence that prospective clients often have a preference for a therapist of their own race/ethnicity (e.g., Cabral and Smith 2011) but relatively few psychologists, psychiatrists, social workers, and counseling professionals are African American (American Psychological Association 2014; Center for Mental Health Services 2004). CMHI sites have struggled with enacting the principle of cultural competence in particular (Brannan et al. 2012; Vinson et al. 2001). Further investigation of the strategies used by sites that have more successfully implemented this principle and possible co-occurring reductions in disparities may inform approaches for improving service provision to racial minorities.
There are several notable limitations of the current study. First, receipt of therapy and reports of youth problem behaviors in the previous 6 months were based on parent report, which may be biased by perceived stigma (e.g., certain groups of parents may be more reluctant to report use of therapy services or behavioral problems) or by memory, and may not align with youth perceptions. Previous work has found modest agreement between parent ratings on the Child Behavior Checklist and adolescent ratings on the Youth Self-Report (a corresponding measure; Achenbach and Rescorla 2001); youth-parent agreement is often found to be better for externalizing than internalizing symptoms (Youngstrom et al. 2000). Thus, adolescent internalizing symptomatology may be under-reported in this sample.
Second, in order to maintain a larger sample size, this analysis only uses data from baseline and 6 month interviews. It is possible that utilization rates would have changed over time and that findings may be different over the course of 12 or 18 months. Still, given that youth were enrolled in services due to acute need, receipt of services within the first 6 months is an important indicator of system responsiveness.
Third, because it utilizes a fully de-identified national data set, this study was unable to incorporate location-specific information about the communities such as indicators of the service array or community characteristics like urbanity or rurality. However, while the aggregated variables of site-level poverty and racial makeup cannot be interpreted as a reflection of the community as a whole, it does reflect an important characteristic of the population served by each system of care site.
Lastly and most importantly, the data do not allow for a more detailed analysis of the therapy that was received, and thus we cannot evaluate how well the therapy “matched” the youths’ specific needs, diagnosis, or preferences, or whether it was empirically based. While there is strong evidence of the efficacy of specific psychotherapies in clinical trials, there is less work on the effectiveness of therapy as it is actually received in real-world conditions, in community settings with diverse youth and high rates of comorbidity (Friedman and Hernandez 2002; Shirk 2001; Weisz and Hawley 1998; Chorpita et al. 2011). While there are now several interventions that have been empirically supported specifically with minority youth samples (Pina et al. 2019), the therapies that are delivered in real-world settings are not always evidence-based or culturally appropriate for a particular youth (Lilienfeld et al. 2012; Zaboski et al. 2017). Thus, we cannot make claims about the appropriateness of the therapy received in this study. In addition to quality of therapy services, youth may also have received an insufficient number of therapy sessions. This study uses a dichotomous measure of receipt of therapy, which speaks to whether or not a youth was connected to a mental health care service but does not speak to the sufficiency, frequency, or length of services. The majority of youth received more than a few sessions and the interpretation of the results were unchanged when analyses were re-run excluding youth who received fewer than five sessions. Nonetheless, this study primarily addresses access to care, and not quality or sufficiency of care. Finally, this study focuses specifically on the receipt of outpatient therapy and not medication, support services, or inpatient therapy.
Despite these limitations, this study investigates a critical element of child and adolescent mental health services with a unique national sample of youth that have already been identified as needing support and have been connected to a funded initiative with the express purpose of enabling access to needed services. It suggests that on its own and as currently implemented, the CMHI initiative is not sufficient to eliminate the differences in service use that emerge across race, poverty level, caregiver education, and site poverty. Further work is needed to identify the reasons that these differences persist within this system. Future work should focus on these groups to investigate possible reasons for the lower use of therapy, and sites should pay particular attention to these populations in order to attain the goal of serving all enrolled youth equally.
References
Achenbach, T. M. (1991). Manual for the child behavior checklist 14–18 and 1991 profile. Burlington, VT: University Associates in Psychiatry.
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school—Age forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth and Families.
American Psychological Association. (2014). Demographic characteristics of APA members by membership status, 2014. Retrieved May 15, 2018 from http://www.apa.org/workforce/publications/14-member/table-1.pdf.
Angold, A., Messer, S. C., Stangl, D., Farmer, E. M. Z., Costello, E. J., & Burns, B. J. (1998). Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health, 88(1), 75–80.
Ascher, B. H., Z. Farmer, E. M., Burns, B. J., & Angold, A. (1996). The child and adolescent services assessment (CASA): Description and psychometrics. Journal of Emotional and Behavioral Disorders, 4(1), 12–20.
Brannan, A. M., Brashears, F., Gyamfi, P., & Manteuffel, B. (2012). Implementation and development of federally-funded systems of care over time. American Journal of Community Psychology, 49(3–4), 467–482.
Bridge, J. A., Asti, L., Horowitz, L. M., Greenhouse, J. B., Fontanella, C. A., Sheftall, A. H., et al. (2015). Suicide trends among elementary school–aged children in the United States from 1993 to 2012. JAMA Pediatrics, 169, 673–677.
Burnett-Zeigler, I., & Lyons, J. S. (2010). Caregiver factors predicting service utilization among youth participating in a school-based mental health intervention. Journal of Child and Family Studies, 19(5), 572–578.
Burns, B. J., Costello, E. J., Angold, A., Tweed, D., Stangl, D., Farmer, E. M., et al. (1995). Children’s mental health service use across service sectors. Health Affairs (Project Hope), 14(3), 147–159.
Cabral, R. R., & Smith, T. B. (2011). Racial/ethnic matching of clients and therapists in mental health services: A meta-analytic review of preferences, perceptions, and outcomes. Journal of Counseling Psychology, 58(4), 537–554.
Caldwell, J. T., Ford, C. L., Wallace, S. P., Wang, M. C., & Takahashi, L. M. (2017). Racial and ethnic residential segregation and access to health care in rural areas. Health & Place, 43, 104–112.
Canvin, K., Jones, C., Marttila, A., Burstrom, B., & Whitehead, M. (2007). Can I risk using public services? Perceived consequences of seeking help and health care among households living in poverty: Qualitative study. Journal of Epidemiology and Community Health, 61(11), 984–989.
Center for Mental Health Services. (2004). Mental health, United States, 2004. In R. W. Manderscheid & J. T. Berry (Eds.), DHHS Publication No. (SMA) 06-4195. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Mental Health Services (CMHS), Substance Abuse and Mental Health Services Administration (SAMHSA), U.S. Department of Health and Human Services (DHHS). (2016). The comprehensive community mental health services for children with serious emotional disturbances program. Report to Congress, 2016.
Chorpita, B. F., Daleiden, E. L., Ebesutani, C., Young, J., Becker, K. D., Nakamura, B. J., et al. (2011). Evidence-based treatments for children and adolescents: An updated review of indicators of efficacy and effectiveness. Clinical Psychology: Science and Practice, 18(2), 154–172.
Chow, J., Jaffe, K., & Snowden, L. R. (2003). Mental health service use by racial and ethnic populations in poverty areas. American Journal of Public Health, 93, 792–797.
Cohen, P., & Hesselbart, C. S. (1993). Demographic factors in the use of children’s mental health services. American Journal of Public Health, 83(1), 49–52.
Cooper-Patrick, L., Powe, N. R., Jenckes, M. W., Gonzales, J. J., Levine, D. M., & Ford, D. E. (1997). Identification of patient attitudes and preferences regarding treatment of depression. Journal of General Internal Medicine, 12(7), 431–438.
Cunningham, P. J., & Freiman, M. (1996). Determinants of ambulatory mental health services use for school-age children and adolescents. Health Services Research, 31(4), 409–427.
Farmer, E. M. Z., Stangl, D. K., Burns, B. J., Costello, E. J., & Angold, A. (1999). Use, persistence, and intensity: Patterns of care for children’s mental health across one year. Community Mental Health Journal, 35(1), 31–46.
Flisher, A. J., Kramer, R. A., Grosser, R. C., Alegria, M., Bird, H. R., Bourdon, K. H., et al. (1997). Correlates of unmet need for mental health services by children and adolescents. Psychological Medicine, 27(5), 1145–1154.
Friedman, R. M., & Hernandez, M. (2002). The national evaluation of the comprehensive community mental health services for children and their families program: A commentary. Children’s Services, 5(1), 67–74.
Garland, A. F., Lau, A. S., Yeh, M., McCabe, K. M., Hough, R. L., & Landsverk, J. A. (2005). Racial and ethnic differences in utilization of mental health services among high-risk youths. The American Journal of Psychiatry, 162(7), 1336–1343.
Graves, K. N., Shelton, T. L., & Kaslow, N. J. (2009). Utilization of individual versus family therapy among adolescents with severe emotional disturbance. American Journal of Family Therapy, 37, 227–238.
Gudiño, O. G., Lau, A. S., & Hough, R. L. (2008). Immigrant status, mental health need, and mental health service utilization among high-risk Hispanic and Asian Pacific Islander youth. Child & Youth Care Forum, 37(3), 139–152.
Gudiño, O. G., Lau, A. S., Yeh, M., McCabe, K. M., & Hough, R. L. (2009). Understanding racial/ethnic disparities in youth mental health services: Do disparities vary by problem type? Journal of Emotional and Behavioral Disorders, 17(1), 3–16.
Gyamfi, P. (2004). Children with serious emotional disturbance: The impact of poverty and receipt of public assistance on behavior, functioning, and service use. Children and Youth Services Review, 26, 1129–1139.
Haines, M. M., McMunn, A., Nazroo, J. Y., & Kelly, Y. J. (2002). Social and demographic predictors of parental consultation for child psychological difficulties. Journal of Public Health, 24(4), 276–284.
Hoagwood, K., Horwitz, S., Stiffman, A., Weisz, J., Bean, D., Rae, D., et al. (2000). Concordance between parent reports of children’s mental health services and service records: The services assessment for children and adolescents (SACA). Journal of Child and Family Studies, 9(3), 315–331.
Horwitz, S. M., Gary, L. C., Briggs-Gowan, M. J., & Carter, A. S. (2003). Do needs drive services use in young children? Pediatrics, 112(6 Pt 1), 1373–1378.
Huang, L., Stroul, B., Friedman, R., Mrazek, P., Friesen, B., Pires, S., et al. (2005). Transforming mental health care for children and their families. American Psychologist, 60(6), 615–627.
Hurlburt, M. S., Leslie, L. K., Landsverk, J., Barth, R. P., Burns, B. J., Gibbons, R. D., et al. (2004). Contextual predictors of mental health service use among children open to child welfare. Archives of General Psychiatry, 61(12), 1217.
Johnson, W. C., LaForest, M., Lissenden, B., & Stern, S. (2017). Variation in mental illness and provision of public mental health services. Health Services and Outcomes Research Methodology, 17(1), 1–30.
Kataoka, S. H., Zhang, L., & Wells, K. B. (2002). Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. American Journal of Psychiatry, 159(9), 1548–1555.
Katapodi, M. C., Pierce, P. F., & Facione, N. C. (2010). Distrust, predisposition to use health services and breast cancer screening: Results from a multicultural community-based survey. International Journal of Nursing Studies, 47(8), 975–983.
Kirby, J. B., & Kaneda, T. (2005). Neighborhood socioeconomic disadvantage and access to health care. Journal of Health and Social Behavior, 46(1), 15–31.
Lilienfeld, S. O., Ammirati, R., & David, M. (2012). Distinguishing science from pseudoscience in school psychology: Science and scientific thinking as safeguards against human error. Journal of School Psychology, 50(1), 7–36.
Lindsey, M. A., Brown, D. R., & Cunningham, M. (2017). Boys do(n’t) cry: Addressing the unmet mental health needs of African American boys. American Journal of Orthopsychiatry, 87(4), 377.
Litaker, D., Koroukian, S. M., & Love, T. E. (2005). Context and healthcare access: Looking beyond the individual. Medical Care, 43(6), 531–540.
McGuire, T. G., Alegria, M., Cook, B. L., Wells, K. B., & Zaslavsky, A. M. (2006). Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Services Research, 41(5), 1979–2005.
Merikangas, K. R., He, J., Burstein, M., Swendsen, J., Avenevoli, S., Case, B., et al. (2011). Service utilization for lifetime mental disorders in U. S. adolescents: Results of the National Comorbidity Survey–Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 50(1), 32–45.
Miech, R., Azur, M., Dusablon, T., Jowers, K., Goldstein, A., Stuart, E., et al. (2008). The potential to reduce mental health disparities through the comprehensive community mental health services for children and their families program. Journal of Behavioral Health Services & Research, 35(3), 253–264.
Pina, A. A., Polo, A. J., & Huey, S. J. (2019). Evidence-based psychosocial interventions for ethnic minority youth: The 10-year update. Journal of Clinical Child & Adolescent Psychology, 48(2), 1–24.
Popescu, I., Xu, H., Krivelyova, A., & Ettner, S. (2015). Disparities in receipt of specialty services among children with mental health need enrolled in the CMHI. Psychiatric Services, 66(3), 242–248.
Porterfield, S. L., & McBride, T. D. (2007). The effect of poverty and caregiver education on perceived need and access to health services among children with special health care needs. American Journal of Public Health, 97(2), 323–329.
Pottick, K. J., Bilder, S., Vander Stoep, A., Warner, L. A., & Alvarez, M. F. (2007). US patterns of mental health service utilization for transition-age youth and young adults. Journal of Behavioral Health Services and Research, 35(4), 373–389.
Probst, J. C., Moore, C. G., Glover, S. H., & Samuels, M. E. (2004). Person and place: The compounding effects of race/ethnicity and rurality on health. American Journal of Public Health, 94(10), 1695–1703.
Sanchez, T. W. (2008). Poverty, policy, and public transportation. Transportation Research Part A: Policy and Practice, 42(5), 833–841.
Shirk, S. R. (2001). The road to effective child psychological services: Treatment processes and outcome research. In J. H. Hughes, A. M. LaGreca, & J. C. Conoley (Eds.), Handbook of psychological services for children and adolescents (pp. 43–59). New York: Oxford University Press.
Smedley, B. D., Stith, A. Y., & Nelson, A. R. (2002). Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press.
Smith, T. B., Constantine, M. G., Dunn, T. W., Dinehart, J. M., & Montoya, J. A. (2006). Multicultural education in the mental health professions: A meta-analytic review. Journal of Counseling Psychology, 53(1), 132–145.
Snowden, L. R., & Thomas, K. (2000). Medicaid and African American outpatient mental health treatment. Mental Health Services Research, 2(2), 115–120.
Snowden, L. R., & Yamada, A. (2005). Cultural differences in access to care. Annual Review of Clinical Psychology, 1, 143–166.
Stroul, B., & Friedman, R. (1986, revised edition). A system of care for severely emotionally disturbed children and youth. Washington, DC: CASSP Technical Assistance Center.
Syed, S., Gerber, B., & Sharp, L. (2013). Traveling towards disease: Transportation barriers to health care access. Journal of Community Health, 38(5), 976–993.
Thomas, K. C., Ellis, A. R., Konrad, T. R., Holzer, C. E., & Morrissey, J. P. (2009). County-level estimates of mental health professional shortage in the United States. Psychiatric Services, 60(10), 1323–1328.
Thompson, R. (2005). The course and correlates of mental health care received by young children: Descriptive data from a longitudinal urban high-risk sample. Children and Youth Services Review, 27(1), 39–50.
Thompson, R., & May, M. A. (2006). Caregivers’ perceptions of child mental health needs and service utilization: An urban 8-year old sample. Journal of Behavioral Health Services and Research, 33(4), 474–482.
Verhulst, F., & van der Ende, J. (1997). Factors associated with child mental health service use in the community. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 901–909.
Vinson, N. B., Brannan, A. M., Baughman, L. N., Wilce, M., & Gawron, T. (2001). The system-of-care model: Implementation in twenty-seven communities. Journal of Emotional and Behavioral Disorders, 9(1), 30–42.
Weisz, J. R., & Hawley, K. M. (1998). Finding, evaluating, refining, and applying empirically supported treatments for children and adolescents. Journal of Clinical Child Psychology, 27, 206–216.
Youngstrom, E., Loeber, R., & Stouthamer-Loeber, M. (2000). Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. Journal of Consulting and Clinical Psychology, 68(6), 1038–1050.
Zaboski, B. A., Schrack, A. P., Joyce-Beaulieu, D., & MacInnes, J. W. (2017). Broadening our understanding of evidence-based practice: Effective and discredited interventions. Contemporary School Psychology, 21(3), 287–297.
Zimmerman, F. J. (2005). Social and economic determinants of disparities in professional help-seeking for child mental health problems: Evidence from a national sample. Health Services Research, 40(5I), 1514–1533.
Funding
This study was supported by a subcontract to a cooperative agreement between the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Illinois Department of Health Services (IDHS). The conclusions are solely the responsibility of the authors and do not necessarily represent the official views of either IDHS or SAMHSA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors Aber and Allen have received SAMHSA funding, through the Illinois Department of Human Services Division of Mental Health, to conduct evaluation of a local system of care initiative (State-assigned Grant #D7333). Author Fitts declares that she has no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Thank you to Kirstin Painter, Ph.D., Public Health Analyst at the Center for Mental Health Services (SAMHSA) for her assistance with accessing the CMHI data.
Rights and permissions
About this article
Cite this article
Fitts, J.J., Aber, M.S. & Allen, N.E. Individual, Family, and Site Predictors of Youth Receipt of Therapy in Systems of Care. Child Youth Care Forum 48, 737–755 (2019). https://doi.org/10.1007/s10566-019-09504-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10566-019-09504-w