Abstract
Tumours secrete several pro-angiogenic factors, among which vascular endothelial growth factor (VEGF) and its receptor (VEGF-R) are the most extensively studied but not in ovarian cancer cells. The study was designed to investigate the effect of bisphenol A (BPA) (environmental oestrogen) and of 17β-estradiol (E2) (endogenous estrogen) on the gene (real-time PCR) and protein (Western blotting) expression of VEGF-R2 and VEGF-A in human non-cancer (HOSEpiC) and ovarian cancer cell lines (SKOV-3 and OVCAR-3). In addition, VEGF-A levels were measured in culture supernatants using a colorimetric assay. Cells were exposed to BPA (1, 40 and 100 nM) or 17β-estradiol (0.1, 10 and 40 nM) for 3 to 48 h. Since differential expression levels of basal oestrogen receptor (ERα and ERβ) between non-cancer and cancer cell lines may affect the response to oestrogens, receptor expression was measured both at the gene and protein levels. Basal ERβ expression was similar in all cell lines, and ERα expression was significantly higher in the SKOV-3 cell line. Basal VEGF-R2 expression was higher in cancer than non-cancer cell lines, and in contrast, VEGF-A expression was significantly lower in both SKOV-3 and OVCAR-3 cancer cell lines. Exposure of non-cancer cells to BPA and E2 was associated with a significant increase in VEGF-R2 expression but had no effect on VEGF-A expression or secretion. In contrast, exposure of cancer cells to BPA, but not E2, increased VEGF-R2 and VEGF-A expression and secretion. In conclusion, (1) BPA and E2 regulated VEGF-R2 and VEGF-A expression differently in non-cancer and cancer cells, and (2) BPA has a direct stimulatory effect on VEGF-R2 and VEGF-A expression in both, while E2 appears to be uninvolved in the regulation of VEGF-R2 and VEGF-A expression in cancer cells.

A schematic representation showing BPA and E2 action on VEGF-R2 and VEGF-A expression in non-cancer (HOSEpiC) and cancer cells (SKOV-3, OVCAR-3)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bisphenol A (BPA), a key component of polycarbonate plastic, is present in a multitude of products, including the interior coatings of food cans and milk containers and dental sealants (Welshons et al. 2006). Biomonitoring studies found BPA in the serum, milk, saliva and urine of humans in nanomolar concentrations (Vandenberg et al. 2010). Our previous data indicate that BPA, at concentrations in the range of those found in human blood samples, up-regulates genes responsible for inducing cell proliferation and down-regulates those involved in the inhibition of cell proliferation in OVCAR-3 cells (Ptak et al. 2011). In addition, we previously demonstrated that BPA is associated with a decrease in the expression and activity of the executioner caspase-3 by the ERK1/2 signal transduction pathway in OVCAR-3 cells (Ptak et al. 2013). Moreover, we observed that BPA induced the activity and expression of MMP-2, MMP-9 and N-cadherin, leading to enhanced migration of OVCAR-3 cells (Ptak et al. 2014). The stimulatory effects of BPA on cell migration were similar to those of 17β-estradiol in OVCAR-3 cells (Ptak et al. 2014).
Angiogenesis is a complex process regulated by numerous endogenous pro-angiogenic and anti-angiogenic factors (Ferrara and Kerbel 2005) that play a crucial role in physiological and pathological conditions. Vascular endothelial growth factor-A (VEGF-A commonly called VEGF) is the predominant VEGF species expressed by tumour cells (Dvorak 2002). VEGF-A acts through its tyrosine kinase receptors, VEGF-R1 (Flt-1) and VEGF-R2 (Flk-1/KDR) (Ferrara 1999; Neufeld et al. 1999), with VEGF-R2 being the major mediator of angiogenesis in solid tumours. VEGF-A is up-regulated in most solid tumours, including ovarian cancers, and correlates with tumour progression and poor prognosis (Siddiqui et al. 2010; Yu et al. 2013).
Several studies have shown a significant increase in serum VEGF-A levels in patients with ovarian cancer compared to healthy individuals (Paley et al. 1997; Yamamoto et al. 1997; Kraft et al. 1999). In addition, the expression of VEGF-A and VEGF-R2 in ovarian carcinomas are higher than that in benign or normal ovarian tissue (Chen et al. 2004). While VEGF-R2 expression in ovarian cancer cells has been reported (Chen et al. 2004; Nishida et al. 2004; Abu-Jawdeh et al. 1996), its functional significance is not known.
Recent evidence revealed that oestrogen may play an important role in angiogenesis. Oestrogen up-regulates VEGF-A in breast (Higgins et al. 2006; Garvin et al. 2006) and endometrial tissues (Fujimoto et al. 1999). In addition, BPA (which has oestrogenic activity) up-regulates VEGF-A expression in reproductive tissues, such as the rat uterus and vagina (Long et al. 2001), swine ovary (Grasselli et al. 2010), and MELN breast cancer cells (Buteau-Lozano et al. 2008).
To our knowledge, even though VEGF and its receptor (VEGF-R) are the most extensively studied pro-angiogenic factors, there are no reports on the effects of xenoestrogens and even 17β-estradiol on VEGF-A expression in ovarian cancer cells. Therefore, the present study was performed to investigate the effects of BPA (a representative environmental oestrogen) and of E2 (an endogenous oestrogen) on VEGF-A secretion and on VEGF-A and VEGF-R2 mRNA and protein levels in two human epithelial ovarian cancer cell lines (OVCAR-3 and SKOV-3) and the non-cancer epithelial ovarian cell line, the human ovarian surface epithelial cells (HOSEpiC).
Materials and methods
Cell culture and treatments
HOSEpiC were purchased from ScienCell Research Laboratories (Carlsbad, CA, USA) and maintained in OEpiCM medium as recommended by the manufacturer. HOSEpiC from ScienCell Research Laboratories are isolated from human ovarian tissue and are recommended and used as normal epithelial cells (Guo et al. 2011; Li et al. 2014). HOSEpiC cells were used at passage 2–3 in all experiments.
The OVCAR-3 and SKOV-3 human ovarian epithelial carcinoma cell lines were obtained from the American Type Culture Collection (Manassas, VA, USA). OVCAR-3 cells were routinely cultured in RPMI 1640 medium (PAA Laboratories GmbH, Cölbe, Germany), and SKOV-3 cells were propagated in McCoy’s 5A modified medium (Sigma Chemical Co., St. Louis, MO, USA). Both cell lines were supplemented with 50 U/ml penicillin, 50 μg/ml streptomycin, and 10 % v/v heat-inactivated foetal bovine serum (FBS) (PAA Laboratories GmbH). All cultures were maintained in a humidified incubator with 5 % CO2 at 37 °C. The propagation medium was replaced with medium without serum 24 h before each experiment. The experiments were performed in serum-free medium.
BPA (AccuStandard Inc., New Haven, CT, USA) and E2 (Sigma) were dissolved in absolute ethanol. The final concentration of ethanol in the medium was 0.1 %. The cells were exposed to vehicle (0.1 %), BPA (1, 40 and 100 nM) or E2 (0.1, 1 and 40 nM) for 3, 24 and 48 h.
Real-time PCR analysis
The expression of the ERα, ERβ, VEGF-R2 and VEGF-A genes was evaluated by real-time polymerase chain reaction (PCR). Total RNA isolation and cDNA synthesis were performed using the TaqMan Gene Expression Cells-to-CT kit (Applied Biosystems, Foster City, CA, USA) according to the manufacturer’s protocol. The lysis solution contained DNase I to remove genomic DNA during cell lysis. The resulting pre-amplified cDNA preparations were analysed by real-time PCR in a StepOnePlus real-time PCR system (Applied Biosystems) using TaqMan Gene Expression Assays, and TaqMan Gene Expression Master Mix containing ROX (Applied Biosystems) according to the manufacturer’s instructions. The PCR conditions were as follows: incubation for 2 min at 50 °C, then 10 min at 95 °C, followed by 40 cycles (denaturation step, 15 s at 95 °C; annealing/elongation step, 60 s at 60 °C). Duplicate control samples prepared for each gene without cDNA showed no DNA contamination. The expression of ERα (ESR1; Hs00174860_m1), ERβ (ESR2; Hs01100353_m1), VEGF-R2 (KDR; Hs00911700_m1) and VEGF-A (Hs00900055_m1) was normalised to that of GADPH (4310554E). Relative expression was quantified using the 2−ΔΔCt method (Livak and Schmittgen 2001). The qPCR amplification efficiency of all of the examined genes was within the range of 90–110 %.
Western blot analysis
The expression of ERα, ERβ, VEGF-R2 and VEGF-A proteins was evaluated by Western blotting. Cells were washed with ice-cold PBS and lysed in ice-cold buffer (lysis buffer 50 mM Tris-HCl pH 7.5, 100 mM NaCl, 0.5 % sodium-deoxycholate, 0.5 % Nonidet NP-40 and 0.5 % SDS) supplemented with the protease inhibitor cocktail tablet (Roche Molecular Biochemicals, Mannheim, Germany). The protein concentration of the cell lysate was determined using the Bradford assay (Bio-Rad Protein Assay, Bio-Rad Laboratories, Munich, Germany). The cell lysate was boiled for 5 min in sample buffer (50 mM Tris-HCl pH 6.8, 12.5 % glycerol, 1 % sodium dodecylsulfate, 0.01 % bromophenol blue, 200 mM dithiothreitol). Protein (30 μg from each treatment group) was separated by 6 % and 10 % SDS-PAGE and transferred to PVDF membranes using a Bio-Rad Mini-Protean 3 apparatus (Bio-Rad Laboratories). The blots were blocked for 2 h with 5 % w/v BSA and 0.1 % v/v Tween 20 in 0.02-M Tris-buffered saline (TBS). The blots were incubated overnight at 4 °C with antibodies specific for ERα (sc-542), ERβ (sc-8974), Flk-1 (sc-101560) (also designated VEGF-R2) and VEGF-A (sc-152) (Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA). VEGF-R2 antibodies have good specific reactivity with three forms of VEGF-R2 including 150-kDa immature, 200-kDa intermediate glycosylated, and 230-kDa mature glycosylated proteins. To control for loading, the same membranes were immunoblotted for β-actin (antibody from Sigma Chemical Co.). After incubation with the primary antibodies, the membranes were washed three times and incubated for 1 h with a horseradish peroxidase-conjugated secondary antibodies for Flk-1 and VEGF-A (Santa Cruz Biotechnology) or β-actin (DakoCytomation (Glostrup, Denmark)). Immunopositive bands were visualised using Western Blotting Luminol Reagents (Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA) and quantified by densitometry (EasyDens, Cortex Nowa, Poland).
VEGF-A secretion
The secretion of VEGF-A was assessed using human VEGF-A ELISA (EIAab Science Co., Ltd, Wuhan, China) according to the manufacturer’s instructions. Serum-free supernatant was centrifuged, collected and stored at −70 °C. Absorbance was measured with an ELx800 microplate reader (BioTek Instruments, Winooski, VT, USA) using a 450-nm filter. Data were recorded and analysis was performed using the KC JUNIOR software (BioTek Instruments).
Statistical analysis
Data were expressed as means ± S.E.M. from four independent experiments performed in triplicates. Statistical analyses were performed using GraphPad Prism 5. Data were analysed by one-way analysis of variance (ANOVA) followed by Tukey’s honestly significant differences (HSD) multiple range test or two-way ANOVA followed by Tukey’s honestly significant differences (HSD) multiple range test when different times were compared. A P < 0.05 was considered statistically significant.
Results
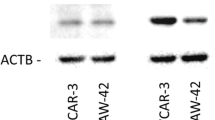
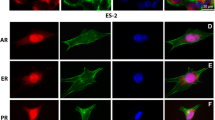
Basal ERα and ERβ gene and protein expression
For each transcript, the relative quantity (RQ) obtained in non-cancer human ovarian epithelial cells (HOSEpiC) was arbitrarily set as 1. Basal ERα transcript and protein levels were similar in HOSEpiC and OVCAR-3 cells, while there was an 8-fold increase in ERα transcript levels and a 2-fold increase in protein levels in SKOV-3 cells (Fig. 1a, b; P < 0.001). Both basal ERβ transcript levels and protein levels were similar in all three cell lines (Fig. 1c, d).
Basal VEGF-R2 and VEGF-A gene expression and VEGF-A secretion
Basal VEGF-R2 expression was higher in the cancer cells (2.9-fold and 3.6-fold in SKOV-3 cells at 3 h and 24 h, respectively, and 2.1-fold and 2.8-fold in OVCAR-3 cells at 3 h and 24 h, respectively) than in the non-cancer HOSEpiC cells (Fig. 2a; P < 0.001). By contrast, VEGF-A expression was significantly lower in the cancer cell lines (3.3-fold and 10-fold reductions in SKOV-3 cells at 3 h and 24 h, respectively, and 5-fold and 10-fold reductions in OVCAR-3 cells at 3 h and 24 h, respectively) than in the non-cancer HOSEpiC cells (Fig. 2b; P < 0.001). The VEGF-A secretion pattern correlated with the VEGF-A expression pattern as it was lower in the cancer cells (3-fold) than in the non-cancer cells (Fig. 2c; P < 0.001).
VEGF-R2 and VEGF-A expression. Basal a VEGF-R2 mRNA, b VEGF-A mRNA, and c VEGF-A secretion in non-cancer HOSEpiC and cancer OVCAR-3 and SKOV-3 cell lines. Expression levels were normalised to those of GADPH. RQ relative quantity. HOSEpiC expression value = 1.0. ***P < 0.001 compared to HOSEpiC cells
Effect of BPA and E2 on VEGF-R2 mRNA and protein expression
In HOSEpiC cells, BPA exposure correlated with increased VEGF-R2 gene expression (by 1.5-, 2.0- and 1.7-fold at 3 h upon exposure to 1, 40 and 100 nM, respectively, and by 3.0-, 2.8- and 2.7-fold at 24 h upon exposure to 1, 40 and 100 nM, respectively) compared to the control (Fig. 3a; P < 0.05, P < 0.001). Exposure to E2 correlated with increased VEGF-R2 gene expression at 1 and 40 nM at 3 h (1.6-fold), and at all concentrations at 24 h (2-fold, 3.2-fold and 3.5-fold, respectively) (Fig. 3a; P < 0.05, P < 0.001).
Real-time PCR analysis of VEGF-R2 mRNA. Effect of BPA (1–100 nM) and E2 (0.1–40 nM) on VEGF-R2 expression in the non-cancer HOSEpiC cells (a) and cancer SKOV-3 (c) and OVCAR-3 (e) cells. VEGF-A mRNA expression after exposure to the test compounds for 3 or 24 h. Expression levels were normalised to those of GADPH and then to the control cells. RQ relative quantity. Control value = 1.0. b, d, f Immunoblot analysis of VEGF-R2 protein expression after exposure of the cells to the test compounds for 24 h. β-actin was used as a loading control. *P < 0.05 and ***P < 0.001 compared to control cells. Statistically significant differences between time-dependent experiments are indicated with different letters, and the same letters indicate no significant difference, with a<b<c<d, p < 0.05
In SKOV-3 and OVCAR-3 cells, neither BPA nor E2 had any effect on VEGF-R2 mRNA expression at 3 h. At 24 h, only BPA correlated with increased VEGF-R2 mRNA expression (at all concentrations tested) in SKOV-3 cells (2.5-fold, 2.3-fold and 1.8-fold upon exposure to 1, 40 and 100 nM, respectively) and in OVCAR-3 cells (1.6-fold, 1.7-fold and 1.6-fold upon exposure to 1, 40 and 100 nM, respectively) (Fig. 3b, c; P < 0.05, P < 0.001).
All glycosylated forms of VEGF-R2 protein were present in HOSEpiC cells as well as in SKOV-3 and OVCAR-3 cells. Western blot analysis reflected the real-time PCR analyses; in HOSEpiC cells, BPA and E2 stimulated VEGF-R2 protein expression (Fig. 3d), while in SKOV-3 and OVCAR-3 cells only BPA stimulated VEGF-R2 protein expression (Fig. 3e, f).
Effect of BPA and E2 on VEGF-A mRNA and protein expression
In the non-cancer cells, neither BPA nor E2 had any effect on VEGF-A gene expression (Fig. 4a), and protein expression (Fig. 4d).
Real-time PCR analysis of VEGF-A mRNA. Effect of BPA (1–100 nM) and E2 (0.1–40 nM) on VEGF-A expression in the non-cancer HOSEpiC cells (a) and cancer SKOV-3 (c) and OVCAR-3 (e) cells. VEGF-A expression after exposure to the test compounds for 3 or 24 h. Expression levels were normalised to those of GADPH and then to the control cells. RQ relative quantity. Control value = 1.0. b, d, f Immunoblot analysis of VEGF-A protein expression after exposure of the cells to the test compounds for 24 h. β-actin was used as a loading control. *P < 0.05 compared to control cells. Statistically significant differences between time-dependent experiments are indicated with different letters, and the same letters indicate no significant difference, with a<b<c<d, p < 0.05
In cancer cells, only BPA correlated with increased expression of VEGF-A mRNA at all concentrations tested, after 24 h of treatment (1.5-fold, 1.5-fold and 1.8-fold upon exposure to 1, 40 and 100 nM, respectively) in SKOV-3 cells, and at 3 h in OVCAR-3 cells (by 1.5-fold, 1.62-fold and 1.72-fold upon exposure to 1, 40 and 100 nM, respectively) (Fig. 4b, c; P < 0.05). VEGF-A protein expression was also slightly increased at 24 h (Fig. 4e, f) after BPA exposure. Exposure to E2 had no effect on VEGF-A gene or protein expression in any cancer cell tested (Fig. 4b, c, e, f).
Effect of BPA and E2 on VEGF-A secretion
BPA increased VEGF-A secretion at all concentrations tested in both SKOV-3 cells (1797 ± 111 pg/ml, 1659 ± 169 pg/ml and 1658 ± 38 pg/ml at 1, 40 and 100 nM, respectively, vs. 1355 ± 16 pg/ml) and OVCAR-3 cells (1707 ± 151 pg/ml, 1875 ± 176 pg/ml,and 1797 ± 45 pg/ml at 1, 40 and 100 nM, respectively, vs. 1457 ± 14 pg/ml) (Fig. 5b, d; P < 0.05). However, E2 had no effect on VEGF-A secretion in either OVCAR-3 or SKOV-3 cells (Fig. 5b, d). In the non-cancer cells, neither BPA nor E2 had an effect on VEGF-A secretion (Fig. 5a).
Discussion
In this study, higher basal VEGF-R2 gene expression levels were detected in cancer cells than in the non-cancer HOSEpiC cells. In contrast, significantly less VEGF-A transcripts were detected in the cancer cell lines than in the non-cancer HOSEpiC cells. This observation is consistent with previously published data showing that VEGF-R2 is overexpressed in human bladder tumours, melanomas and breast cancer tissue (Wu et al. 2003; Straume and Akslen 2001; Speirs and Atkin 1999; Price et al. 2001; Kranz et al. 1999; Ryden et al. 2003; Nakopoulou et al. 2002). In addition, Spannuth et al. (2009) reported that VEGF-R2 expression, measured by immunofluorescence, was low or absent in the epithelial cells of normal ovaries but present in 75 % of invasive ovarian cancer samples analysed.
Our data showed that BPA significantly increased VEGF-R2 expression in both cancer and non-cancer cells despite the differences in basal VEGF-R2 expression between these cell types. This suggests a possible intensification of pro-angiogenic activity by creating more binding sites for VEGF. In support, a study addressing the effects of BPA on VEGF-R2 expression showed that 1 nM–1 μM BPA significantly stimulated VEGF-R2 mRNA expression in human umbilical vein endothelial cells (HUVEC) at 6 h (Andersson and Brittebo 2012). Moreover, whereas basal VEGF-A expression and secretion were lower in cancer cells, BPA increased VEGF-A expression and secretion in cancer but not in non-cancer cells (which were characterised by high VEGF-A expression and secretion). Our results concerning cancer cells are consistent with data showing that BPA (1 μM) stimulates VEGF-A mRNA expression at 6 h and secretion at 24 h in the breast cancer cell lines MCF-7 and MELN (Buteau-Lozano et al. 2008). In addition, Andersson and Brittebo (2012) reported increased VEGF-A gene expression in HUVEC exposed to 1 nM–1 μΜ BPA for 6 h. Our data showing the lack of effect of BPA on VEGF-A expression and secretion in non-cancer cells are supported by the observations of Romani et al. (2013) who showed unchanged VEGF-A levels in human luteal cells upon exposure to BPA. However, there are also data showing a stimulatory effect of BPA in doses of 1–10 μM on VEGF-A secretion in swine granulosa cells (Grasselli et al. 2010) and 37.5–150 mg/kg BPA on VEGF-A mRNA expression in rat uterus and vagina (Long et al. 2001).
In contrast, E2 stimulated VEGF-R2 expression only in non-cancer cells with low basal VEGF-R2 gene expression. To our knowledge, there is no information regarding the effect of E2 on VEGF-R2 expression in ovarian cancer cells. Studies of the effect of E2 on VEGF-R2 expression in breast cancer cells are ambiguous: Higgins et al. (2006) showed that E2 induces VEGF-R2 expression in ZR-75 breast cancer cells but decreases VEGF-R2 mRNA levels in MCF-7 cells (Higgins et al. 2008). There also is no information regarding the effect of E2 on VEGF-A expression and secretion in ovarian cancer cells. We showed that E2 does not alter VEGF-A expression levels and secretion in both cancer and non-cancer cell types, despite the high basal expression in non-cancer and low expression in cancer cells. There are data showing the action of E2 on VEGF-A expression in breast cancer cells. Stimulatory effects were described by Ruohola et al. (1999) and Buteau-Lozano et al. (2008) in MCF-7 breast cancer cells and by Stoner et al. (2004) in ZR-75 breast cancer cells. Stimulatory effects of E2 on VEGF have been observed in cell lines that predominantly expressed the oestrogen receptor alpha (ERα) (Al-Bader et al. 2011; Hevir et al. 2011). In human ovaries, ERβ is predominantly expressed in the granulosa cells, theca cells, surface epithelium and corpus luteum (Drummond and Fuller 2012). This should explain the discrepancy in our results and those previously published with breast cancer cells. Buteau-Lozano et al. (2008) showed unchanged VEGF-A levels in MDA-MB-231 cells upon exposure to E2. MDA-MB-231 cells express only ERβ and not ERα (Hevir et al. 2011).
The different effects of BPA and E2 observed in our study independent of the basal VEGF-R2/VEGF-A expression suggest that regulation of pro-angiogenic factors in ovarian cells is dependent on basal ERα/ERβ expression. A previous study indicated that BPA-induced VEGF-A expression is associated with an oestrogen-mimicking effect (Buteau-Lozano et al. 2008).
Our data showed a lack of difference in the basal ERβ gene and protein levels in cancer and non-cancer cells, and similar, low ERα gene and protein levels in non-cancer HOSEpiC and cancer OVCAR-3 cells, while significantly higher in SKOV-3. Surprisingly, we did not observe differences in E2 action in SKOV-3 and OVCAR-3 in addition to the significant differences in ERα gene and protein levels. Although both OVCAR-3 and SKOV-3 express ERα and ERβ, OVCAR-3 cells show lower ERα levels in comparison to SKOV-3. However, SKOV-3 carry an ERα exon 1 deletion mutation (Lau et al. 1999), which may explain the lack of differences in the response of OVCAR-3 and SKOV-3 to estradiol.
It has also been reported that BPA induces VEGF-R2 and VEGF-A expression in cells expressing ERβ but not ERα (HUVEC cells) (Andersson and Brittebo 2012). We showed that both ERβ mRNA and protein levels were similar in all tested cell lines and that BPA but not E2 induced VEGF-R2 and VEGF-A expression and VEGF-A secretion. In breast cancer cell lines MDA-MB-231 and T47D, which express only ERβ, previous data showed that VEGF levels were unchanged after treatment with E2. The heterodimerisation of ERα/ERβ may inhibit oestrogen-induced VEGF expression (Dadiani et al. 2009), which may explain the lack of E2 response in OVCAR-3 cells containing both ERα/ ERβ.
In conclusion, (1) BPA by increases VEGF-R2 receptor expression, especially in cancer cells, could creating more binding sites for VEGF-A, and (2) E2 appears to be uninvolved in the regulation of VEGF-R2 and VEGF-A expression in ovarian cancer cells.
References
Abu-Jawdeh GM, Faix JD, Niloff J, Tognazzi K, Manseau E, Dvorak HF, et al. Strong expression of vascular permeability factor (vascular endothelial growth factor) and its receptors in ovarian borderline and cancer neoplasms. Lab Investig. 1996;74:1105–15.
Al-Bader M, Ford C, Al-Ayadhy B, Francis I. Analysis of estrogen receptor isoforms and variants in breast cancer cell lines. Exp Ther Med. 2011;2:537–44.
Andersson H, Brittebo E. Proangiogenic effects of environmentally relevant levels of bisphenol A in human primary endothelial cells. Arch Toxicol. 2012;86:465–74.
Buteau-Lozano H, Velasco G, Cristofari M, Balaguer P, Perrot-Applanat M. Xenoestrogens modulate vascular endothelial growth factor secretion in breast cancer cells through an estrogen receptor-dependent mechanism. J Endocrinol. 2008;196:399–412.
Chen H, Ye D, Xie X, Chen B, Lu W. VEGF, VEGFRs expressions and activated STATs in ovarian epithelial carcinoma. Gynecol Oncol. 2004;94:630–5.
Dadiani M, Seger D, Kreizman T, Badikhi D, Margalit R, Eilam R, et al. Estrogen regulation of vascular endothelial growth factor in breast cancer in vitro and in vivo: the role of estrogen receptor alpha and c-Myc. 1. Endocr Relat Cancer. 2009;16:819–34.
Drummond AE, Fuller PJ. Activin and inhibin, estrogens and NFκB, play roles in ovarian tumourigenesis is there crosstalk? Mol Cell Endocrinol. 2012;359:85–91.
Dvorak HF. Vascular permeability factor/vascular endothelial growth factor: a critical cytokine in tumour angiogenesis and a potential target for diagnosis and therapy. J Clin Oncol. 2002;20:4368–80.
Ferrara N. Role of vascular endothelial growth factor in the regulation of angiogenesis. Kidney Int. 1999;56:794–814.
Ferrara N, Kerbel RS. Angiogenesis as a therapeutic target. Nature. 2005;438:967–74.
Fujimoto J, Sakaguchi H, Hirose R, Wen H, Tamaya T. Angiogenesis in endometriosis and angiogenic factors. Gynecol Obstet Investig. 1999;48 Suppl 1:14–20.
Garvin S, Nilsson UW, Huss FR, Kratz G, Dabrosin C. Estradiol increases VEGF in human breast studied by whole-tissue culture. Cell Tissue Res. 2006;325:245–51.
Grasselli F, Baratta L, Baioni L, Bussolati S, Ramoni R, Grolli S, et al. Bisphenol A disrupts granulosa cell function. Domest Anim Endocrinol. 2010;39:34–9.
Guo AM, Liu X, Al-Wahab Z, Maddippati KR, Ali-Fehmi R, Scicli AG, et al. Role of 12-lipoxygenase in regulation of ovarian cancer cell proliferation and survival. Cancer Chemother Pharmacol. 2011;8:1273–83.
Hevir N, Trost N, Debeljak N, Rizner TL. Expression of estrogen and progesterone receptors and estrogen metabolizing enzymes in different breast cancer cell lines. Chem Biol Interact. 2011;191:206–16.
Higgins KJ, Liu S, Abdelrahim M, Yoon K, Vanderlaag K, Porter W, et al. Vascular endothelial growth factor receptor-2 expression is induced by 17beta-estradiol in ZR-75 breast cancer cells by estrogen receptor alpha/Sp proteins. Endocrinology. 2006;147:3285–95.
Higgins KJ, Liu S, Abdelrahim M, Vanderlaag K, Liu X, Porter W, et al. Vascular endothelial growth factor receptor-2 expression is down-regulated by 17beta-estradiol in MCF-7 breast cancer cells by estrogen receptor alpha/Sp proteins. Mol Endocrinol. 2008;22:388–402.
Kraft A, Weindel K, Ochs A, Marth C, Zmija J, Schumacher P, et al. Vascular endothelial growth factor in the sera and effusions of patients with cancer and noncancer disease. Cancer. 1999;85:178–87.
Kranz A, Mattfeldt T, Waltenberger J. Molecular mediators of tumour angiogenesis: enhanced expression and activation of vascular endothelial growth factor receptor KDR in primary breast cancer. Int J Cancer. 1999;84:293–8.
Lau KM, Mok SC, Ho SM. Expression of human estrogen receptor-alpha and -beta, progesterone receptor, and androgen receptor mRNA in normal and malignant ovarian epithelial cells. Proc Natl Acad Sci U S A. 1999;96:5722–7.
Li J, Cui G, Sun L, Wang SJ, Tian S, Guan Z, et al. ARHI overexpression induces epithelial ovarian cancer cell apoptosis and excessive autophagy. Int J Gynecol Cancer. 2014;24:437–43.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–8.
Long X, Burke KA, Bigsby RM, Nephew KP. Effects of the xenoestrogen bisphenol A on expression of vascular endothelial growth factor (VEGF) in the rat. Exp Biol Med (Maywood). 2001;226:477–83.
Nakopoulou L, Stefanaki K, Panayotopoulou E, Giannopoulou I, Athanassiadou P, Gakiopoulou-Givalou H, et al. Expression of the vascular endothelial growth factor receptor-2/Flk-1 in breast carcinomas: correlation with proliferation. Hum Pathol. 2002;33:863–70.
Neufeld G, Cohen T, Gengrinovitch S, Poltorak Z. Vascular endothelial growth factor (VEGF) and its receptors. FASEB J. 1999;13:9–22.
Nishida N, Yano H, Komai K, Nishida T, Kamura T, Kojiro M. Vascular endothelial growth factor C and vascular endothelial growth factor receptor 2 are related closely to the prognosis of patients with ovarian carcinoma. Cancer. 2004;101:1364–74.
Paley PJ, Staskus KA, Gebhard K, Mohanraj D, Twiggs LB, Carson LF, et al. Vascular endothelial growth factor expression in early stage ovarian carcinoma. Cancer. 1997;80:98–106.
Price DJ, Miralem T, Jiang S, Steinberg R, Avraham H. Role of vascular endothelial growth factor in the stimulation of cellular invasion and signaling of breast cancer cells. Cell Growth Differ. 2001;12:129–35.
Ptak A, Wróbel A, Gregoraszczuk EL. Effect of bisphenol-A on the expression of selected genes involved in cell cycle and apoptosis in the OVCAR-3 cell line. Toxicol Lett. 2011;202:30–5.
Ptak A, Rak-Mardyła A, Gregoraszczuk EL. Cooperation of bisphenol A and leptin in inhibition of caspase-3 expression and activity in OVCAR-3 ovarian cancer cells. Toxicol In Vitro. 2013;27:1937–43.
Ptak A, Hoffmann M, Gruca I, Barć J. Bisphenol A induce ovarian cancer cell migration via the MAPK and PI3K/Akt signalling pathways. Toxicol Lett. 2014;229:357–65.
Romani F, Tropea A, Scarinci E, Dello Russo C, Lisi L, Catino S, et al. Endocrine disruptors and human corpus luteum: in vitro effects of phenols on luteal cells function. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2013;31:170–80.
Ruohola JK, Valve EM, Karkkainen MJ, Joukov V, Alitalo K, Härkönen PL. Vascular endothelial growth factors are differentially regulated by steroid hormones and antiestrogens in breast cancer cells. Mol Cell Endocrinol. 1999;149:29–40.
Ryden L, Linderholm B, Nielsen NH, Emdin S, Jonsson PE, Landberg G. Tumour specific VEGF-A and VEGFR2/KDR protein are co-expressed in breast cancer. Breast Cancer Res Treat. 2003;82:147–54.
Siddiqui GK, Elmasry K, Wong Te Fong AC, Perrett C, Morris R, Crow JC, et al. Prognostic significance of intratumoural vascular endothelial growth factor as a marker of tumour angiogenesis in epithelial ovarian cancer. Eur J Gynaecol Oncol. 2010;31:156–9.
Spannuth WA, Nick AM, Jennings NB, Armaiz-Pena GN, Mangala LS, Danes CG, et al. Functional significance of VEGF-R2 on ovarian cancer cells. Int J Cancer. 2009;124:1045–153.
Speirs V, Atkin SL. Production of VEGF and expression of the VEGF receptors Flt-1 and KDR in primary cultures of epithelial and stromal cells derived from breast tumours. Br J Cancer. 1999;80:898–903.
Stoner M, Wormke M, Saville B, Samudio I, Qin C, Abdelrahim M, et al. Estrogen regulation of vascular endothelial growth factor gene expression in ZR-75 breast cancer cells through interaction of estrogen receptor alpha and SP proteins. Oncogene. 2004;23:1052–63.
Straume O, Akslen LA. Expression of vascular endothelial growth factor, its receptors (FLT-1, KDR) and TSP-1 related to microvessel density and patient outcome in vertical growth phase melanomas. Am J Pathol. 2001;159:223–35.
Vandenberg LN, Chahoud I, Heindel JJ, Padmanabhan V, Paumgartten FJ, Schoenfelder G. Urinary, circulating, and tissue biomonitoring studies indicate widespread exposure to bisphenol A. Environ Health Perspect. 2010;118:1055–70.
Welshons WV, Nagel SC, vom Saal FS. Large effects from small exposures. III. Endocrine mechanisms mediating effects of bisphenol A at levels of human exposure. Endocrinology. 2006;147:S56–69.
Wu W, Shu X, Hovsepyan H, Mosteller RD, Broek D. VEGF receptor expression and signaling in human bladder tumours. Oncogene. 2003;22:3361–70.
Yamamoto S, Konishi I, Mandai M, Kuroda H, Komatsu T, Nanbu K, et al. Expression of vascular endothelial growth factor (VEGF) in epithelial ovarian neoplasms: correlation with clinicopathology and patient survival, and analysis of serum VEGF levels. Br J Cancer. 1997;76:1221–7.
Yu L, Deng L, Li J, Zhang Y, Hu L. The prognostic value of vascular endothelial growth factor in ovarian cancer: a systematic review and meta-analysis. Gynecol Oncol. 2013;128:391–6.
Acknowledgments
Thanks to Marta Hoffmann and Justyna Barć for excellent technical assistance. We also thank The Polish Committee for Scientific Research (from 2010 to 2013 as project 0050/B/P01/2010/38) for funding.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ptak, A., Gregoraszczuk, E.L. Effects of bisphenol A and 17β-estradiol on vascular endothelial growth factor A and its receptor expression in the non-cancer and cancer ovarian cell lines. Cell Biol Toxicol 31, 187–197 (2015). https://doi.org/10.1007/s10565-015-9303-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10565-015-9303-z