Abstract
Sex steroid exposure constitutes a risk factor for breast cancer, but little is known about the effects of sex steroids on the normal breast, largely because of the lack of convenient models. We have developed a method of culturing normal breast tissue ex vivo. We have applied this method to investigate the effects of estradiol and progesterone on the key angiogenic mediator, vascular endothelial growth factor (VEGF), in the breast. Whole breast tissue was obtained from routine reduction mammoplasty. Tissue biopsies were cultured in vitro for 1–3 weeks, and the expression of luminal cytokeratin 18 was determined by immunohistochemistry. As an application, tissue biopsies were treated in vitro for 1 week with or without estradiol or estradiol and progesterone. Estrogen receptor, progesterone receptor, and Ki–67 were analyzed, and VEGF levels were examined by quantitative immunoassay and immunohistochemistry. Whole breast tissue was cultured ex vivo for 1 week with preserved morphology. Increased detachment of the luminal epithelium was observed after 2 weeks. Estradiol increased extracellular levels of VEGF in normal breast tissue biopsy medium. The addition of progesterone had neither stimulatory nor inhibitory effects on secreted VEGF. The method of whole breast tissue culturing thus provide a means by which to explore the biology of normal breast tissue. Our results suggest that estradiol exerts pro-angiogenic effects in normal breast by increasing levels of biologically active VEGF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development, proliferation, and differentiation of normal breast tissue are processes dependent on sex steroids (Anderson et al. 1998). Epidemiological evidence suggests that cumulative exposure to sex steroids constitutes a risk factor for the development of breast cancer (Rossouw et al. 2002; Beral 2003). The mechanisms underlying this increased risk are still largely unknown, one reason being the lack of applicable models for investigations into the biology of the normal breast. The adult female breast consists of a branching network of ducts lined by a double layer of epithelial cells, luminal glandular cells, and basal myoepithelial cells (Russo and Russo 1998). The epithelial bilayer is embedded in a stroma of fibroblasts, extracellular matrix, and adipose tissue, components that together create a unique environment difficult to reproduce in cell culture in vitro. A whole-tissue model preserving the multicellular structure and function of breast tissue would be highly advantageous for research on the normal breast.
Sex steroids have been demonstrated to affect a number of biological processes associated with tumor initiation and progression in the breast, including angiogenesis (Dickson and Lippman 1987; Goldfine et al. 1992; Clarke et al. 1997; Hyder and Stancel 2000). Vascular endothelial growth factor (VEGF) is a key mediator of tumor angiogenesis, including neovascularization in human breast cancer (Folkman 1995). Increased VEGF mRNA expression has been demonstrated in breast cancer tissue compared with that in normal breast tissue (Yoshiji et al. 1996), and high tissue VEGF levels appear to correlate with poor prognosis in breast cancer patients (Linderholm et al. 1998, 2000).
Both estrogen and progesterone have been shown to increase VEGF in a number of human breast cancer cell lines (Hyder et al. 1998, 2001; Ruohola et al. 1999; Soares et al. 2002; Garvin and Dabrosin 2003), and an estrogen responsive element has been identified in the promoter region of the gene for VEGF (Hyder et al. 2000). Using microdialysis, we have previously demonstrated increased extracellular VEGF levels during the luteal phase in human breast tissue in vivo (Dabrosin 2003). It is unclear, however, whether estradiol alone is responsible for increased VEGF or if progesterone also exerts regulatory effects on extracellular levels of VEGF in the normal breast. In this study, we have developed a method of culturing normal breast tissue ex vivo. With this method, whole breast tissue has been cultured for 1–3 weeks, and immunohistochemical staining for the luminal epithelial marker cytokeratin (CK) 18 has been performed. Furthermore, the effects of estradiol and progesterone on VEGF in the breast have been investigated as an application of whole-tissue culturing.
Materials and methods
Tissue preparation
Biopsies from human breast tissue were obtained from three healthy pre-menopausal women undergoing routine reduction mammoplasty. None of the patients had ongoing hormonal treatment. The breast tissue was transported to the laboratory in sterile physiologic saline solution (0.9% NaCl; B. Braun Medical, Bromma, Sweden) and processed under sterile conditions within 24 h. The tissue was first washed in sterile phosphate-buffered saline (PBS). An 8-mm biopsy punch (Kai Europe, Solingen, Germany) was then applied to produce multiple tissue biopsies consisting of epithelial areas, fibrous stroma, and adipose tissue. The biopsies were washed in PBS, placed individually in wells of a 12-well plate (Costar, Cambridge, Mass.), and submerged in medium as described below. Cell culture media and additives were obtained from GIBCO, Paisley, UK, if not otherwise stated.
In the first set of experiments, tissue biopsies from patient 1 were cultured in a modified mammary epithelium cell medium (Huss and Kratz 2001) consisting of the following: a 2:1 mixture of Dulbecco’s modified Eagle’s medium (DMEM) without phenol red and nutrient mixture F–12 (HAM) supplemented with 2% fetal bovine serum, hydrocortisone (0.3 μg/ml; Sigma, St. Louis, Mo.), insulin (4 μg/ml; Sigma), transferrin (4 μg/ml; Sigma), 3,3′,5–triiodothyronine (1 ng/ml; Sigma), cholera toxin (7 ng/ml; Sigma), epidermal growth factor (8 ng/ml; Sigma), and adenine (0.2 mg/ml; Sigma). Biopsies were incubated at 37°C in a humidified atmosphere containing 5% CO2, and the medium was changed every day. The biopsies were harvested after 1, 2, and 3 weeks. Upon harvesting, the biopsies were weighed (Mettler Toledo PG5002–S DeltaRange Balance; Mettler–Toledo, Stockholm, Sweden) and then directly fixed in 4% neutral buffered formaldehyde overnight. They were thereafter dehydrated through an ethanol–xylene series and embedded in paraffin for hematoxylin and eosin (H&E) staining and immunohistochemistry.
In order to conduct hormonal studies, a serum-free medium was used consisting of a 1:1 mixture of nutrient mixture F–12 (HAM) and DMEM without phenol red supplemented with transferrin (10 μg/ml; Sigma), insulin (1 μg/ml; Sigma), and bovine serum albumin (0.2 mg/ml; Sigma). Following a wash in PBS, the individual biopsies from patients 2 and 3 were placed in wells of a 12-well plate containing serum-free medium as described above with or without physiological levels of 10−9 M estradiol (17β–estradiol; E2; Sigma) or a combination of 10−9 M estradiol and 10−8 M progesterone (E2+P; Sigma). Biopsies in the control group were incubated in serum-free medium supplemented with ethanol solvent equivalent to that administered in the E2+P group (0.001%). The biopsies were treated for 7 days at 37°C in a humidified atmosphere containing 5% CO2, and the medium was changed every day. After the seventh day of incubation, the medium from each biopsy was collected and kept frozen until analysis. The tissue biopsies were weighed, formalin-fixed, and paraffin-embedded as described above.
Immunohistochemistry of tumor sections
Following the first set of experiments, biopsies after 1, 2, and 3 weeks in culture were sectioned, deparaffinized, and subjected to staining with anti-human cytokeratin 18 (monoclonal mouse anti-human CK 18; DakoCytomation, Glostrup, Denmark). Mayer’s hematoxylin was used for counter-staining. Negative controls (primary antibody omitted) did not stain.
After hormone treatment as described above, analyses for Ki–67, estrogen receptor (ER), and progesterone receptor (PR) were conducted on sections from formalin-fixed paraffin-embedded biopsies. Ki–67 was stained by using the MIB–1 antibody (monoclonal mouse anti-human Ki–67 antigen, DakoCytomation). Staining for ER and PR was performed with monoclonal rabbit anti-human estrogen receptor alpha antibody (Lab Vision, Suffolk, UK) and monoclonal mouse anti-human progesterone receptor antibody (Novocastra Laboratories, Newcastle, UK). In addition, anti-human VEGF immunohistochemistry was performed (monoclonal mouse anti-human VEGF, R&D systems, Abingdon, UK). The anti-VEGF antibody is specific for both the 165 and 121 isoforms. Sections were counter-stained with Mayer’s hematoxylin. Negative controls (primary antibody omitted) did not show staining. In a blinded manner, all sections were first scanned to determine the range of intensity of the staining for VEGF. Thereafter, all sections were scored as weakly or strongly positive for VEGF. Ten high-power fields (×200) were examined in 3–5 sections from each group. Biopsy sections were also subjected to H&E staining. Envision detection (DakoCytomation) was used in all experiments.
Quantification of VEGF
Breast tissue media were analyzed for VEGF by using a commercial quantitative immunoassay kit for human VEGF (QuantGlo, human VEGF; R&D systems) without preparation. According to the manufacturer, the VEGF kit measures the VEGF 165 and 121 isoforms, and the minimum detectable dose is less than 1.76 pg/ml. The intra-assay and inter-assay precision for this kit is 3%–8%, which was confirmed in our laboratory.
Statistics
The values represent the mean±SEM. Statistical analyses were performed with ANOVA, Student’s t-test, or Fisher’s exact test where appropriate.
Results
Ex vivo breast tissue culture
Culturing of breast tissue was possible for up to 1 week with preserved morphology. At 1 week, the double-layer of basal and luminal epithelium was mainly preserved. The presence of luminal epithelium was confirmed by immunohistochemical staining of the luminal epithelial marker CK 18. At 2 weeks, the epithelium was reduced to a single layer, and increased epithelial detachment was observed. CK 18 staining revealed preferential detachment of the luminal epithelium, whereas the preserved single layer of epithelium did not stain. Sections from tissue biopsies treated for 3 weeks lacked an intact epithelium. In addition, increasing degeneration of the stroma could be observed after 2 and 3 weeks in culture. Representative tissue sections treated in vitro for 1–3 weeks are shown in Fig. 1.
H&E stained sections from tissue biopsies cultured in modified mammary epithelium cell medium for 1–3 weeks (arrows areas of increased epithelial detachment observed after 2–3 weeks of treatment). a–c Representative tissue sections incubated for 1, 2, and 3 weeks, respectively. Increased degeneration of the stroma is present after 2–3 weeks. d–f Tissue sections stained for the luminal epithelial marker cytokeratin 18 (CK 18). Luminal epithelial cells (brown) are preserved after 1 week in culture (d) but detach after 2 weeks, leaving a single layer of myoepithelial cells (e). After 3 weeks, the epithelium is no longer intact, and both luminal and myoepithelial cells can be observed in the lumen (f). ×100
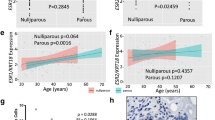
Estradiol increased extracellular VEGF
The breast tissue mass did not differ between treatment groups (0.50±0.04 g in controls, 0.49±0.03 g in E2, and 0.51±0.03 g in E2+P for patients 2 and 3; n=8−9). Significantly higher levels of VEGF were detected in breast culture medium after incubation with E2 or E2+P for 1 week. In patient 2, extracellular levels of VEGF were 273±70 pg/g tissue in controls, 676±69 pg/g tissue in the E2 group (P<0.01 compared with controls), and 573±52 pg/g tissue in the E2+P group (P<0.05 compared with controls; Fig. 2). Similar increases in VEGF after hormone treatment were observed in tissue medium from patient 3, although the absolute levels of extracellular VEGF were lower in all groups; 92±15 pg/g tissue in controls, 256±66 pg/g tissue in the E2 group (P<0.05 compared with controls), and 199±36 pg/g tissue in the E2+P group (P<0.05 compared with controls; Fig. 3). The addition of progesterone had neither a stimulatory nor an inhibitory effect on secreted VEGF as compared with estradiol treatment alone.
Extracellular VEGF after hormone exposure of breast tissue from patient 2. Tissue biopsies were cultured in the presence of estradiol (E2; 10−9 M), a combination of estradiol and progesterone (E2+P; 10−9 M and 10−8 M, respectively), or serum-free medium alone supplemented with hormone solvent (c). VEGF was measured by enzyme-linked immunosorbent assay (ELISA) after 7 days in culture (n=3−5 in each group, **P<0.01 as compared with control cells; *P<0.05 as compared with control cells)
Extracellular VEGF after hormone exposure of breast tissue from patient 3. Tissue biopsies were cultured as described in Fig. 2, and VEGF was measured by ELISA after 7 days in culture (n=4−5 in each group, *P<0.05 as compared with control cells)
Immunohistochemistry
No morphological differences were observed between biopsies taken from patient 1 and treated for 7 days with serum compared with biopsies taken from patient 2 and treated for 7 days without serum. Tissue sections from all treatment groups showed viability as shown by the staining of Ki–67, ER, and PR after 1 week in culture. Representative sections from each treatment group are shown in Figs. 4 and 5. Immunohistochemistry for VEGF revealed intracellular cytoplasmic staining in epithelial cells in tissue sections from all treatment groups, without detectable differences between groups. Representative tissue sections from all treatment groups are shown in Fig. 6. Necrosis was not observed in any group, and the distribution of epithelium, adipose, and connective tissue was similar in all treatment groups.
Immunohistochemistry for Ki–67 in breast tissue sections from patient 2 and after 7 days of treatment as described in Fig. 2. Viable dividing cells were identified in all treatment groups. Representative sections for controls, estradiol (E2), and estradiol + progesterone (E2+P) are shown in a–c, respectively. ×400
Immunohistochemical staining for estrogen receptor (ER) and progesterone receptor (PR) of breast tissue sections from patient 2 and after hormone treatment for 7 days as described in Fig. 2. Positive staining was observed in all treatment groups: controls, estradiol (E2), and estradiol + progesterone (E2+P). Staining for ER is shown in a–c and for PR in d–f. ×400
Immunohistochemistry for VEGF in breast tissue sections from patient 2. Tissue biopsies were treated for 7 days in culture as described in Fig. 2. No differences were observed in the distribution or intensity of staining in tissue sections from the treatment groups: controls, estradiol (E2), and estradiol + progesterone (E2+P), shown in a–c, respectively. ×400
Discussion
In this study, we demonstrate an ex vivo method allowing the culture of breast tissue, incorporating whole-tissue biopsies. Using this method, we show that estradiol increases secreted VEGF in breast tissue medium.
Cellular interactions between epithelial and stromal cells are key determinants in cytodifferentiation and organ morphogenesis (Cunha et al. 1985; Donjacour and Cunha 1991; Hom et al. 1998). Stromal cells are thought to play a central role in tumor growth and progression by providing a vascular network and extracellular signaling molecules (Picard et al. 1986; Grey et al. 1989; Camps et al. 1990; Hanahan and Folkman 1996); some evidence suggests that stromal alterations may precede malignant transformation of tumor cells (Moinfar et al. 2000). In a co-culture model of the breast, fibroblasts have been demonstrated to play a regulatory role in breast epithelial growth and differentiation (Shekhar et al. 2001). Likewise, interactions with endothelial cells have been shown to be essential for ductal-alveolar morphogenesis of preneoplastic human breast epithelial cells, a process stimulated by estrogen (Shekhar et al. 2000). Three-dimensional models have been constructed by culturing different cell types together as spheroids (Sutherland 1988; Carlsson and Nederman 1989). All of these co-culture models are however simplified compared with the three-dimensional structural and functional complexity of living tissue. The use of animal models, such as rodents or non-human primates, is limited in the context of human breast research because of important hormonal differences, differences in mammary development, differentiation, and tumorigenesis, and practical and economic reasons (Clarkson et al. 2004). Thus, there is a need for readily available techniques for studying the normal breast. Compared with other ex vivo culture methods, such as tissue slices (Hawkins et al. 1985), the whole breast tissue model may be applied to study the effects of exogenous substances for up to 1 week in culture. Investigations of the biology of the human breast may be conducted with preserved tissue architecture and without the use of an artificial extracellular matrix. The need for artificial constructions of cellular interactions is eliminated, and difficulties extrapolating results from non-human species are avoided. Our method is also relatively simple and inexpensive.
In the present study, we have observed increased detachment of epithelial cells after 2–3 weeks in culture. A single layer of myoepithelial cells is preserved after 2 weeks, suggesting preferential loss of the luminal glandular cells and/or selective preservation of the basal myoepithelial cells under these culture conditions.
After 1 week in culture, the epithelium remains intact, under both serum-enriched and serum-free conditions. This observation is in agreement with a previous study in which a gelatin sponge was used for the in vitro culture of mammary gland tissue (Zhuang et al. 2003). In the sponge model, the morphology of breast tissue remains normal when cultured in medium with and without serum for 1 week (Zhuang et al. 2003). We show that estradiol increases secreted VEGF from breast tissue into the culture medium. In order to mimic physiologic conditions during the luteal phase of the menstrual cycle, the breast biopsies have been exposed to estradiol in combination with progesterone. The addition of progesterone neither a stimulatory nor an inhibitory effect on VEGF has secretion compared with estradiol exposure alone. Cross-talk between steroid hormones and polypeptide growth factors has been demonstrated previously (Ando’ et al. 1998); however, the addition of growth factors in serum-free medium was necessary for viability during the culture period, and all groups were treated in the same manner (Ando’ et al. 1998). Our results are in agreement with our previous in vivo findings demonstrating higher levels of extracellular VEGF in normal human breast tissue during the luteal phase than during the follicular phase (Dabrosin 2003). A wide inter-individual difference in extracellular VEGF has been found in vivo in the breast (Dabrosin 2003) similar to differences in the absolute levels of extracellular VEGF in tissue medium from patients 2 and 3 in the present study.
Although differences in extracellular VEGF have been observed, no difference in immunohistochemical staining for VEGF has been seen between treatment groups. This might be because immunohistochemistry is a semi-quantitative method and may lack the sensitivity necessary to detect differences between treatment groups. Furthermore, several isoforms of VEGF exist, and their activities are regulated at the post-translational level in the extracellular space (Ferrara and Davis–Smyth 1997; Neufeld et al. 1999). The longer VEGF isoforms (189 and 206) are mainly sequestered in the extracellular matrix and function as a reservoir for free VEGF. The shorter soluble isoforms (121 and 165) are considered the most biologically active and are not likely to be detected in the extracellular space by the immunostaining of tissue sections (Relf et al. 1997; Zhang et al. 2000). The results of the present study demonstrating differences in secreted VEGF without differences in the immunohistochemical staining are in agreement with our previous study (Garvin and Dabrosin 2003); variable levels of intratumoral secreted VEGF were detected in vivo, whereas immunohistochemical staining for VEGF showed no difference between treatment groups (Garvin and Dabrosin 2003). These findings demonstrate that it is critical to measure VEGF in the extracellular space, where its bioavailability is regulated and where it exerts its effects.
The culturing method for whole breast tissue presented in this study provides an additional means by which to explore the biology of normal breast tissue further. The method may be applied to investigate effects on normal human breast tissue and secreted extracellular proteins. The increase of VEGF levels by estradiol reported in the present study may be involved in the carcinogenic effects of sex steroids in the breast, although further studies are needed to elucidate the role of sex steroids in the regulation of angiogenesis.
References
Anderson E, Clarke RB, Howell A (1998) Estrogen responsiveness and control of normal human breast proliferation. J Mammary Gland Biol Neoplasia 3:23–35
Ando’ S, Panno ML, Salerno M, Sisci D, Mauro L, Lanzino M, Surmacz E (1998) Role of IRS–1 signaling in insulin-induced modulation of estrogen receptors in breast cancer cells. Biochem Biophys Res Commun 253:315–319
Beral V (2003) Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet 362:419–427
Camps JL, Chang SM, Hsu TC, Freeman MR, Hong SJ, Zhau HE, Eschenbach AC von, Chung LW (1990) Fibroblast-mediated acceleration of human epithelial tumor growth in vivo. Proc Natl Acad Sci USA 87:75–79
Carlsson J, Nederman T (1989) Tumour spheroid technology in cancer therapy research. Eur J Cancer Clin Oncol 25:1127–1133
Clarke RB, Howell A, Anderson E (1997) Type I insulin-like growth factor receptor gene expression in normal human breast tissue treated with oestrogen and progesterone. Br J Cancer 75:251–257
Clarkson TB, Appt SE, Wood CE, Cline JM (2004) Lessons to be learned from animal studies on hormones and the breast. Maturitas 49:79–89
Cunha GR, Bigsby RM, Cooke PS, Sugimura Y (1985) Stromal-epithelial interactions in adult organs. Cell Differ 17:137–148
Dabrosin C (2003) Variability of vascular endothelial growth factor in normal human breast tissue in vivo during the menstrual cycle. J Clin Endocrinol Metab 88:2695–2698
Dickson RB, Lippman ME (1987) Estrogenic regulation of growth and polypeptide growth factor secretion in human breast carcinoma. Endocr Rev 8:29–43
Donjacour AA, Cunha GR (1991) Stromal regulation of epithelial function. Cancer Treat Res 53:335–364
Ferrara N, Davis–Smyth T (1997) The biology of vascular endothelial growth factor. Endocr Rev 18:4–25
Folkman J (1995) Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med 1:27–31
Garvin S, Dabrosin C (2003) Tamoxifen inhibits secretion of vascular endothelial growth factor in breast cancer in vivo. Cancer Res 63:8742–8748
Goldfine ID, Papa V, Vigneri R, Siiteri P, Rosenthal S (1992) Progestin regulation of insulin and insulin-like growth factor I receptors in cultured human breast cancer cells. Breast Cancer Res Treat 22:69–79
Grey AM, Schor AM, Rushton G, Ellis I, Schor SL (1989) Purification of the migration stimulating factor produced by fetal and breast cancer patient fibroblasts. Proc Natl Acad Sci USA 86:2438–2442
Hanahan D, Folkman J (1996) Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 86:353–364
Hawkins RA, Thomson ML, Killen E (1985) Oestrone sulphate, adipose tissue, and breast cancer. Breast Cancer Res Treat 6:75–87
Hom YK, Young P, Wiesen JF, Miettinen PJ, Derynck R, Werb Z, Cunha GR (1998) Uterine and vaginal organ growth requires epidermal growth factor receptor signaling from stroma. Endocrinology 139:913–921
Huss FRM, Kratz G (2001) Mammary epithelial cell and adipocyte co-culture in a 3-D matrix: the first step towards tissue-engineered human breast tissue. Cells Tissues Organs 169:361–367
Hyder SM, Stancel GM (2000) Regulation of VEGF in the reproductive tract by sex-steroid hormones. Histol Histopathol 15:325–334
Hyder SM, Murthy L, Stancel GM (1998) Progestin regulation of vascular endothelial growth factor in human breast cancer cells. Cancer Res 58:392–395
Hyder SM, Nawaz Z, Chiappetta C, Stancel GM (2000) Identification of functional estrogen response elements in the gene coding for the potent angiogenic factor vascular endothelial growth factor. Cancer Res 60:3183–3190
Hyder SM, Chiappetta C, Stancel GM (2001) Pharmacological and endogenous progestins induce vascular endothelial growth factor expression in human breast cancer cells. Int J Cancer 92:469–473
Linderholm B, Tavelin B, Grankvist K, Henriksson R (1998) Vascular endothelial growth factor is of high prognostic value in node-negative breast carcinoma. J Clin Oncol 16:3121–3128
Linderholm B, Grankvist K, Wilking N, Johansson M, Tavelin B, Henriksson R (2000) Correlation of vascular endothelial growth factor content with recurrences, survival, and first relapse site in primary node-positive breast carcinoma after adjuvant treatment. J Clin Oncol 18:1423–1431
Moinfar F, Man YG, Arnould L, Bratthauer GL, Ratschek M, Tavassoli FA (2000) Concurrent and independent genetic alterations in the stromal and epithelial cells of mammary carcinoma: implications for tumorigenesis. Cancer Res 60:2562–2566
Neufeld G, Cohen T, Gengrinovitch S, Poltorak Z (1999) Vascular endothelial growth factor (VEGF) and its receptors. FASEB J 13:9–22
Picard O, Rolland Y, Poupon MF (1986) Fibroblast-dependent tumorigenicity of cells in nude mice: implication for implantation of metastases. Cancer Res 46:3290–3294
Relf M, LeJeune S, Scott PA, Fox S, Smith K, Leek R, Moghaddam A, Whitehouse R, Bicknell R, Harris AL (1997) Expression of the angiogenic factors vascular endothelial cell growth factor, acidic and basic fibroblast growth factor, tumor growth factor beta-1, platelet-derived endothelial cell growth factor, placenta growth factor, and pleiotrophin in human primary breast cancer and its relation to angiogenesis. Cancer Res 57:963–969
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the women’s health initiative randomized controlled trial. JAMA 288:321–333
Ruohola JK, Valve EM, Karkkainen MJ, Joukov V, Alitalo K, Harkonen PL (1999) Vascular endothelial growth factors are differentially regulated by steroid hormones and antiestrogens in breast cancer cells. Mol Cell Endocrinol 149:29–40
Russo IH, Russo J (1998) Role of hormones in mammary cancer initiation and progression. J Mammary Gland Biol Neoplasia 3:49–61
Shekhar MP, Werdell J, Tait L (2000) Interaction with endothelial cells is a prerequisite for branching ductal-alveolar morphogenesis and hyperplasia of preneoplastic human breast epithelial cells: regulation by estrogen. Cancer Res 60:439–449
Shekhar MP, Werdell J, Santner SJ, Pauley RJ, Tait L (2001) Breast stroma plays a dominant regulatory role in breast epithelial growth and differentiation: implications for tumor development and progression. Cancer Res 61:1320–1326
Soares R, Reis–Filho JS, Gartner F, Schmitt FC (2002) Vascular endothelial growth factor, transforming growth factor-alpha, and estrogen receptors: possible cross-talks and interactions. Am J Pathol 160:381–382
Sutherland RM (1988) Cell and environment interactions in tumor microregions: the multicell spheroid model. Science 240:177–184
Yoshiji H, Gomez DE, Shibuya M, Thorgeirsson UP (1996) Expression of vascular endothelial growth factor, its receptor, and other angiogenic factors in human breast cancer. Cancer Res 56:2013–2016
Zhang HT, Scott PA, Morbidelli L, Peak S, Moore J, Turley H, Harris AL, Ziche M, Bicknell R (2000) The 121 amino acid isoform of vascular endothelial growth factor is more strongly tumorigenic than other splice variants in vivo. Br J Cancer 83:63–68
Zhuang YH, Saaristo R, Ylikomi T (2003) An in vitro long-term culture model for normal human mammary gland: expression and regulation of steroid receptors. Cell Tissue Res 311:217–226
Acknowledgements
The authors are grateful to Dr. Hans Olsson at the Department of Clinical Pathology and to the staff at the Laboratory for Experimental Plastic Surgery in Linköping for their expert assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by grants from the Swedish Cancer Society and Linköping University Hospital.
Rights and permissions
About this article
Cite this article
Garvin, S., Nilsson, U.W., Huss, F.R.M. et al. Estradiol increases VEGF in human breast studied by whole-tissue culture. Cell Tissue Res 325, 245–251 (2006). https://doi.org/10.1007/s00441-006-0159-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-006-0159-7