Abstract
Tissue recovery personnel often find themselves in a situation in which, upon donor physical assessment, they discover an unusual or suspicious skin or tissue lesion. Because of the concern about the possibility of recovering tissues from a donor who may have an occult malignancy or infection, the Recovery Team may elect not to recover. Otherwise they may continue with the recovery, documenting their concern on the physical assessment form. At the time of evaluation of donor suitability the Medical Director must determine what the lesion is. This is inherently difficult and sometimes has led to the discard of recovered tissues. In order to optimize the gift of donation and avoid unnecessary deferral or discard of tissues we instituted a recovery biopsy procedure several years ago. Between January, 2005 and March, 2010, 561 biopsies were performed. In 552 donors (98.4%) there was no negative effect on medical suitability. Nine donors (1.6%) were found unsuitable based on the biopsy results. The recovery biopsy has allowed Recovery Teams to better manage their time by quickly identifying and biopsying suspicious lesions without trying to make a determination of donor eligibility and possibly ruling ineligible a qualified donor. The recovery biopsy has allowed the Medical Directors to make suitability decisions to accept or reject based on diagnostic certainty.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Like organ donation, tissue donor eligibility is, in part, determined by the review of the medical and behavioral history obtained by the Call Center Coordinator and by a physical assessment of the donor performed by the Tissue Recovery Team. The Recovery Team must have the ability to do a thorough examination and recognize then properly evaluate any abnormal findings. Their ability to evaluate abnormal findings is limited as most recovery technicians are not diagnosticians, and differentiating acceptable versus unacceptable lesions is exceedingly difficult on gross examination.
These factors can lead to “overcalling” suspicious physical assessment findings as possible cancer or infection, and can lead to an unnecessary rule out decision to not recover tissues from an otherwise normal, healthy donor. There is also the possibility that a donor actually does have an active occult malignancy or infection affecting the quality of the tissues and/or posing a risk of transmission to the recipient. Because of these limitations of the “standard physical assessment”, we instituted a policy of biopsying any abnormal or suspicious lesion(s) found at recovery. The Medical Director reviews the biopsy results to help determine if the recovered tissues are suitable or not for processing and eventual release for implantation. This practice has improved the safety of the implanted allograft while at the same time maximizing the gift of donation. It has improved the efficiency of the Recovery Teams by removing unnecessary conflicts and the stress of having to determine if a donor is eligible or not. The biopsy protocol has also aided continuing education programs. Biopsy results are reviewed by the Medical Director while making suitability decision.
Materials and methods
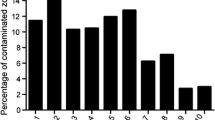
Supplies and training needs were evaluated to test use of recovery biopsy as a tool for diagnostic certainty for decisions made on skin lesions. A biopsy kit with appropriate instruments, containers, labels and instructions was developed, as was a training program for obtaining samples. A decision tree was also developed for lesions that qualify for biopsy versus those which are a rule out on observation. The program was initially launched in a local service area which resulted in increased efficiency in the recovery environment and increased certainty during donor suitability decision-making when a suspicious lesion was observed. The program was opened to national participation. A retrospective study was done on recovery biopsies from January, 2005 to March, 2010. All biopsy reports were collected and, based on their physical assessment description, grouped into categories typically used by recovery teams on the physical assessment form (i.e. grey–brown or blue–purple skin lesions, genital lesions, etc.). We looked for any effect that the pathology diagnosis had on donor suitability. We also looked for any effect the biopsy protocol had on overall efficiency.
Results
Between January, 2005 and March, 2010, 561 biopsies were performed. Acceptable biopsy results occurred for 552 donors (98.4%), which assisted with determining the donor to be suitable. Tissue from nine donors (1.6%) was discarded based on the biopsy results. Five cases were occult cancers and four cases were suggestive of an infectious granulomatous disease (see Table 1). The cases of cancer were of the breast, lymph node and skin (3).
Acceptable cases included a wide range of benign lesions (see Table 2).
Conclusion
The recovery biopsy has allowed Recovery Teams to better manage their time by quickly identifying and biopsying suspicious lesions without trying to make a determination of donor eligibility and possibly ruling a qualified donor as ineligible. At the quality assurance donor suitability evaluation step, the biopsy report eliminates the problem of trying to interpret findings on physical assessment. Identifying occult malignancy or a possible relevant infection eliminates the potential risk for transmission of disease. The recovery biopsy has elevated the standard of practice, becoming an integral part of our overall safety strategy, optimizing the gift of donation and avoiding unnecessary rejection of donated tissues.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Singh, S., Blevins, MB., Wakeman, M. et al. The utility of recovery biopsies in determining donor suitability. Cell Tissue Bank 13, 565–567 (2012). https://doi.org/10.1007/s10561-011-9272-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-011-9272-2