Abstract
The Saint Louis hospital tissue bank provides skin allografts to pediatric and adult burn units in the Paris area. The aim of this study was to analyze our activity during the last 11 years focusing on the reasons for skin discard. Skin is procured solely from the back of the body, which is divided into 10 zones that are harvested and processed separately. This retrospective study included all skin donors harvested between June 2002 and June 2013, representing a total of 336 donors and 2770 zones. The donors were multiorgan heart-beating donors in 91 % of cases (n = 307). The main reason for discarding harvested skin was microbial contamination, detected in 99 donors (29 %). Most contaminants were of low pathogenicity. Other reasons for discard included positive serologic tests for 2 donors [17 zones (0.61 %)], unsuitable physical skin characteristics for 3 zones (0.11 %), the donor’s medical history for 53 zones (1.91 %), and technical issues with processing or distribution for 61 zones (2.2 %). In our experience, microbial contamination continues to be the main reason for discarding potential skin allografts. However, discards are limited by separate harvesting and processing of multiple zones in each donor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Some patients with extensive burns do not have sufficient healthy skin for autologous coverage. Skin allografts are the best and most common alternative for temporary burn coverage. However, allograft availability is sometimes limited by a lack of donors and the risk of disease transmission. Tissue banks use a variety of selection criteria and processing methods to ensure that allografts are free of microbial contamination, without severely restricting their production. Differences among tissue banks include the type of donors [multi-organ heart-beating donors (MOHBDs) vs non-heart-beating donors (NHBDs)], the procurement method, the decontamination process, microbiological screening, and storage conditions (Kearney 2005).
The Saint Louis hospital tissue bank provides skin allografts to more than half of Paris-area burns centers, including a pediatric burns unit. In this retrospective study, we analyzed our activity over the last 11 years, focusing on the reasons for skin discard, and especially microbial contamination.
Materials and methods
Donors’ characteristics
We reviewed all the files of skin donors procured in our tissue bank between June 2002 and June 2013. The following data were collected: age, gender, weight, height, cause of death and type of donor, procurement date and site, operating team, time between death and clamping, time between procurement and cryopreservation, harvested skin area and microbiological findings. The donors’ total body surface area was calculated according to Dubois formula.
Procurement of skin allograft
Skin is procured in aseptic conditions. For MOHBDs, procurement takes place in the operating room, usually after organ and soft-tissue retrieval, and before bone procurement. For NHBDs, skin is harvested in a specific tissue-recovery room (mortuary) within 24 h post mortem, only if the body was refrigerated within 6 h following death, in keeping with French regulations.
The donor is positioned in the ventral position. After hair removal, four successive washes are done, three with povidone-iodine (one with a foaming 4 % solution and two with a 10 % solution) and the last with 70 % ethanol. After sterile draping, the back of the trunk and lower limbs is divided into ten zones, numbered 1–10, grossly defined by the harvesting team (Table 1). The legs (zones 9 and 10) are not sampled in female donors. Skin strips 0.3–0.5 mm thick are harvested with an electric dermatome (B Braun Medical, Boulogne, France). Immediately after removal, the skin strips (2–5 per zone) from each zone are placed separately in sterile containers in sterile Ringer’s lactate (Fresenius Kabi, Sèvres, France), supplemented with 320 mg/l gentamicin (Panpharma, Fougères, France), 500 mg/l vancomycin (Merck Génériques, Lyon, France) and 600 mg/l clindamycin (Pfizer, Paris, France). The allografts are transported to the tissue bank on crushed ice.
Processing of skin allografts
After arrival in the tissue bank, the allografts are kept at +2 to +8 °C until processing. Processing is done in aseptic conditions (ISO 5 in ISO 7 environment according to international standard ISO 14644), on average within 36 h after procurement.
The 10 zones are processed and evaluated separately. The allografts are removed from the transport solution and incubated for 2 h at room temperature with continuous agitation (GFL, Burgwedel, Germany) in cryoprotectant solution consisting of RPMI culture medium (Invitrogen, Lifetechnologies, Cergy Pontoise, France) and 15 % glycerol (Braun Medical, Boulogne, France), supplemented with 0.7 % human albumin (LFB, Les Ulis, France) and antibiotics, as mentioned above. The skin strips are then examined macroscopically. Their edges are regularized, and the total surface area harvested from each zone is recorded. The skin strips from each zone are transferred to sterile sealed pouches (Maco Biotech Freezing, MacoPharma, Tourcoing, France).
Cryopreservation takes place at a rate of −1 to −2 °C per minute between +10 and −40 °C, as described in detail elsewhere (Gaucher et al. 2012). Thereafter, the temperature is reduced at a rate of −5 °C per minute down to −150 °C (Freezal, Air Liquide Santé, Puteaux, France). At the end of the rate-controlled freezing process, the pouches are immediately transferred to the vapor phase of a liquid nitrogen container (Espace 330, Air Liquide Santé, Puteaux, France) and held between −150 and −170 °C until their distribution.
Evaluation of microbial contamination
Viral contamination is assessed by serological testing of the donor. In keeping with French law (Decree N°2010—1625, 23 December 2010), MOHBDs are systematically screened for HIV, HTLV, syphilis, HCV, HBV, EBV, CMV and toxoplasmosis. EBV, CMV and toxoplasmosis serologic testing is not obligatory for NHBDs but is available for most such donors. In 2011, molecular biology tests for HIV, HBV and HCV nucleic acids were added to serological tests.
Microbiological sampling is done during skin processing: for each zone, skin remnants from strip regularization are sampled (about 1 cm2 per strip) and transferred to a recipient containing 13 ml of Schaedler broth (Biomérieux SA, Craponne, France) for bacteriological and mycological testing. The samples are incubated at 37 °C in these recipients for 2 or 10 days (the incubation period was extended in 2009) and then sonicated for 20 min at 35 kHz (Fisher scientific, Singen, Germany) at the end of the incubation period. The liquid medium is then homogenized and seeded into Chocolate agar + PolyViteX (Biomérieux SA, Craponne, France) for aerobic culture, Columbia agar + 5 % sheep blood (Biomérieux SA, Craponne, France) for anaerobic culture, and Sabouraud chloramphenicol gentamicin agar (Bio-Rad Inc, Hercules, USA) for fungal culture. The bacterial media are incubated at 37 °C for 8 days and the fungal medium at 30 °C for 11 days. As a second control at the end of the culture period (21 days), direct microscopic examination of the Schaedler broth kept at 37 °C is performed. Positive results are verified by further culture with the Bact/Alert® system (Biomérieux SA, Craponne, France). When microbiological growth is detected, species identification and antibiotic sensitivity testing are performed at the microbiology department of Saint Louis hospital.
Statistical methods
Statistics and graphical presentations were produced using GraphPad Prism version 5.00 for Windows (GraphPad Software, La Jolla California, USA). The Chi square test was used to identify associations between the rate of microbial contamination and the different body areas, causes of death, procurement sites, and operating teams.
Student’s t test was used to identify relationships between microbial contamination and donor age and gender. Student’s t test was also used to determine if the length of stay in an intensive care unit and other times before procurement differed between contaminated and uncontaminated donors. Significance was assumed at p < 0.05.
Results
Donor characteristics
Among a total of 1585 deceased donors harvested at Saint Louis hospital between June 2002 and June 2013, 340 donors (7 %) underwent skin harvesting. Four donors were excluded after procurement, as examination of their complete records in the tissue bank showed a missing HIV serology, a positive HBV serology, a case of hemochromatosis, or excessively thin harvested skin. On average, the bank collected skin from 42 donors per year, but the number of donors doubled between 2006 (27 donors) and 2010 (58 donors). Skin procured from a single donor was distributed to 1–4 recipients (mean 1.45 recipients).
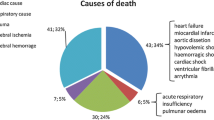
The 336 donors included in this study consisted of 137 females (41 %) and 199 males (59 %), with ages ranging from 15 to 82 years (mean 50 years), and a median body surface area of 1.88 m2 (range 1.22–2.56 m2); 307 donors (91 %) were MOHBDs and 29 (9 %) NHBDs. Stroke was the main cause of death (56 %), followed by cardiac arrest (21 %) (Table 2).
Among MOHBDs, the median length of stay in an intensive care unit was 2 days (range 1–17 days). Among hospitalized NHBDs, the pre-mortem hospital stay ranged from 1 to 21 days (median 1 day). The processing times were as follows: for MOHBDs, the median time between death and clamping (i.e. warm ischemia) was 11 h 45 min (range 2 h–39 h 37 min), and the median time between clamping and cryopreservation was 18 h 20 min (range 7 h 30 min–47 h 35 min). For NHBDs, the median time between death and cryopreservation was 36 h 27 min (range 12 h 53 min–53 h 12 min).
Characteristics of harvested skin
Skin procurement was performed by five different surgical teams in 30 different hospitals; our tissue bank’s team performed 279 (83 %) of the 336 procurements.
The total area of harvested skin was 753,234 cm2, corresponding to a total of 2770 zones. The median surface area per donor was 2235.5 cm2 (range 594–5894 cm2). The harvested skin surface area correlated with the total body surface area (r2 = 0.2675, p < 0.0001).
The maximum possible number of zones, i.e. 8 in women and 10 in men, was harvested in respectively 67 % (n = 97) and 50 % (n = 100) of donors.
As the zones were grossly defined, the surface area procured per zone varied slightly according to the harvesting team. The harvested surface area also differed according to the zone; the average areas were as follows: shoulders (zones 1 and 2) 304.8 cm2; lower back (zones 3 and 4) 268.3 cm2, thighs (zones 7 and 8) 284.7 cm2, buttocks (zones 5 and 6) 239.5 cm2, and legs (zones 9 and 10) 232.3 cm2.
Serology
All the donors were seronegative for HIV, HTLV and syphilis (TPHA and/or VDRL). One donor (0.3 %) was HCV-seropositive therefore excluded. HBV surface antigen (HBsAg) was not detected in any of the 336 donors, ruling out active infection. One donor (0.3 %) was positive for anti-HBV core and surface antibodies.
As it is required by law for MOHBDs, donors were tested for EBV, CMV and toxoplasmosis. Results of those tests are presented here for documentation though not used to rule out skin donors. Of the 319 (95 %) donors screened for both CMV and EBV, 175 (58 %) were positive for CMV and 306 (95 %) for EBV. The CMV and EBV serologies were not available for 17 (5 %) NHBDs.
Of the 320 donors screened for toxoplasmosis, 86 (27 %) were negative and 234 (73 %) were positive; 163 positive donors (70 %) had evidence of past infection (positive IgG and negative IgM), while 12 (5 %) had evidence of recent infection (positive IgG and IgM). The remaining 59 donors (25 %) were positive for IgG but their IgM status was not determined, meaning that the timing of infection could not be estimated.
Reasons for skin discard
A total of 307 zones (11 %) from 151 donors (45 %) were discarded, including 134 zones (5 %) from 52 donors (15 %) for reasons other than microbial contamination (Table 3).
Microbiological results
Microbial contamination was detected in 99 donors (29 %). No significant statistical relationship was found between donor gender, age or cause of death and the presence of contamination, or between the same parameters and the percentage of contamination. The length of stay in an intensive care unit was significantly longer in contaminated versus uncontaminated donors (mean 4.4 and 2.3 days respectively, p < 0.0001). The other studied parameters (hospital of procurement, operating team, time between death and clamping, and time between procurement and cryopreservation) were not related to microbial contamination.
273 of the 2770 harvested zones (69,260 of 753,234 cm2) were contaminated, representing 32 % of the surface area harvested from the 99 positive donors, and 9.2 % of the area harvested from all donors.
The microbial contaminants were mostly bacteria (Table 4). In the 190 zones with solely bacterial contamination, the bacteria were mostly of low pathogenicity. Staphylococcus aureus was never detected (Table 5). Nine zones (4.7 %) were contaminated with multiple bacteria (intestinal flora in 4 cases, skin flora in 1 case, and a mix of the two in 4 cases). In addition, 15 contaminated zones (7.9 %) were discarded for other reasons before the microbiological results became available. No correlation was found between the type of contaminant and the harvested zone.
It should be noted that the bacteriological tests were performed after treatment with the antibiotic cocktail, and that the latter comprised vancomycin and clindamycin (effective on gram-positive bacteria) and gentamicin (effective on gram-negative bacteria). All the isolated gram-positive cocci were sensitive to vancomycin and resistant to clindamycin. Likewise, all the isolated gram-positive bacilli were sensitive to vancomycin. Among the gram-negative bacilli, the A. baumannii, P. aeruginosa and K. pneumoniae isolates were resistant to gentamicin, whereas the E. cloacae, P. mirabilis, E. coli, E. aerogenes and M. morganii isolates were sensitive to gentamicin.
Fungal contamination was detected in 75 zones (27.5 %): 65 (86.7 %) of these zones yielded yeasts, 6 (8 %) filamentous fungi, and 4 (5.3 %) unidentified species. Candida albicans was the predominant yeast, being found in 62 (82.7 %) zones. Other isolated yeasts included C. parapsilosis (1 zone), C. glabrata (1 zone) and Trichosporon inkin (1 zone). The isolated filamentous fungi belonged to the genera Penicillium (2 zones), Rhizopus (1 zone) or Scapulariopsis (1 zone), or were unidentified (2 zones).
Interestingly, the rate of contamination varied significantly according to the zone (Chi square test p < 0.0001). The shoulders (zones 1 and 2) were the most frequently contaminated zone (11.5 and 14.2 %, respectively), and the legs (zones 9 and 10) were the least frequently contaminated zone (2.7 and 3.0 %, respectively) (Fig. 1).
Discussion
We report the skin donor harvesting and processing experience of Saint Louis Hospital tissue bank over an 11-year period. Unfortunately, tissue-bank practices and guidelines are extremely variable, making it difficult to compare the results published by different teams.
The number of skin donors sampled by our tissue bank increased markedly over the study period. MOHBDs represented the majority of our population of skin donors (91 vs 9 % NHBDs), reflecting the rise in the number of MOHBDs nationwide, as underlined in the annual report of The French Biomedical Authority (ABM: Agence de la biomédecine 2012). The temporal distribution of causes of death in our donor population is also similar to that reported by the ABM, with a higher proportion of stroke and a lower proportion of trauma over time. The same report states that organs and/or tissues were harvested from only 48 % of potential donors. In 2012, skin was collected from 185 donors in France (by our bank in 27.6 % of cases). This number is shockingly small by comparison with the 1589 MOHBDs and 4900 cornea donor harvested in the same year. Public awareness must be improved in order to increase the number of skin donors (Gaucher et al. 2013).
We harvest skin from the back of the body only, in order to preserve the deceased’s appearance for the family. For the same reason, skin is not removed from back of the legs (zones 9 and 10) of female donors. The average area of skin harvested per donor in our center (2235.5 cm2) is smaller than that reported by other authors (3500 cm2 for de Backere 1994; 3062 cm2 for Lindford et al. 2010). However, given the practical difficulties of turning the body and the accompanying risk of contamination and, most of all, the likely poorer acceptance of whole-body skin harvesting by the family, retrieval from only the back of the body may be more productive overall.
After procurement, the skin grafts are controlled morphologically and microbiologically, and only those considered suitable for transplantation are retained. Pre-procurement screening of MOHBDs markedly reduces the post-procurement discard rate (Beele et al. 2013; Van Geyt et al. 2010). Only 4.2 % of the skin zones we procured were discarded for reasons other than microbial contamination. Three zones were rejected upon physical assessment of the procured skin. In one donor, biopsy of a suspicious lesion revealed a benign skin growth in 5 of 8 retrieved zones, but the rest of the skin could be saved. This underlines the importance of recovery biopsies, as recommended by Singh et al. (2012). Moreover, histopathological examination of other organs retrieved first from MOHBDs can reveal abnormalities, as in the 3 cases we rejected for skin donation because of suspected renal carcinoma. Pouches that were discarded after distribution represented 17.9 % of all discarded skin and 2.0 % of all harvested skin. This proportion could be reduced through better control of transport conditions.
Only two (0.6 %) of the 336 donors were rejected because of seropositivity for pathogens (one for HCV, and one for dual anti-HBc and anti-HBs positivity). The second donor, rejected in 2007, would have qualified under current French guidelines, which accept donors with HBcAb and HBsAb in the absence of HBsAg and HBV nucleic acids. This rejection rate is lower than in previous reports (Pianigiani et al. 2006), probably because of the larger proportion of MOHBDs, who are serologically screened prior to skin procurement.
We found a bacterial contamination rate of 23.8 % after antibiotic treatment of the skin grafts. Rates of 5, 6, 15.7 and 16.7 % have been reported elsewhere (Ireland and Spelman 2005; Mathur et al. 2009; Neely et al. 2008; Obeng et al. 2001), although longer studies by the Siena and Helsinki skin banks gave similar contamination rates of 26.2 and 25 %, respectively (Lindford et al. 2010; Pianigiani et al. 2010). Discrepancies with other studies may be explained by differences in donor preparation before skin harvesting (May et al. 1991). However, in the study by Mathur et al. (2009), donors were scrubbed with povidone-iodine and ethanol, as in our center.
It is interesting to note that shoulder skin had the higher rate of microbial contamination, probably through contact with head hair, suggesting that more attention should be paid to draping the head and neck.
Until 2009, we incubated skin samples in enrichment broth for 2 days before culture. In 2009, the enrichment period was extended to 10 days, giving a total incubation period of 21 days. Although no significant change was seen in the positivity rate after this prolongation of the enrichment period, longer incubation can allow the detection of slow-growing bacteria (mostly commensal gram-positive bacilli) and samples with a low bioburden. Pirnay et al. (2012) reported a culture positivity rate of 29.7 % (after antibiotic treatment) with a 14-day culture period, as compared to 18.9 % with a 7-day period. It is noteworthy that bacteria can be sheltered from topical antibiotics within pores or hair follicles, and that Staphylococcus aureus and Propionibacterium acnes are known to form biofilms on skin (Achermann et al. 2014; Shin et al. 2013). Sample sonication before culture destroys these biofilms, releasing the bacteria and allowing their detection (Kobayashi et al. 2009; Portillo et al. 2014). To our knowledge, sonication was not used in studies with lower contamination rates.
All the gram-positive isolates in this study were sensitive to vancomycin, one of the antibiotics used in our cocktail, at a concentration 30–100 times the minimal bactericidal concentration for most contaminating bacteria (Pitt et al., 2014). Some gram-negative isolates were gentamicin-resistant, but most were susceptible.
It is therefore reasonable to question the conditions of skin allograft decontamination. There are two main issues. First, as mentioned above, bacteria can be sheltered deep within the skin. However, for technical reasons, it would be difficult to add a sonication phase before antibiotic treatment. Second, decontamination takes place at a low temperature (4 °C) in order to conserve the skin, but in vitro susceptibility tests show that the optimal temperature for antibiotic activity is 37 °C. Antibiotic cocktails are poorly active at 4 °C, even at high concentrations (Pitt et al. 2014). Our processing method includes 2 h of incubation at room temperature, which allows glycerol to penetrate into the skin but is not sufficient for the antibiotics to act. Extension of this incubation period at 37 °C would threaten skin quality. Another solution is to thaw contaminated skin grafts and to preserve them in glycerol after a second cycle of decontamination (Lomas et al. 2004; Verbeken et al. 2012).
Antifungal agents are not included in our antibiotic cocktail, and fungal contamination was detected in skin from 36 donors (10.7 %), predominantly due to Candida species. Mathur et al. (2009) reported similar results after fungal decontamination, whereas Pianigiani et al. (2010) reported a lower rate (5.3 %), even before treatment. In view of these paradoxical results, a study of the necessity and efficacy of antifungal treatment would be of interest.
Another important issue concerning microbiological analysis is the presence of residual antibiotics. In our center, samples are touch-dried of antibiotic solution before being submerged in culture medium, which further dilutes residual antibiotics. More efficient removal of decontaminating antibiotics might increase the sensitivity of subsequent microbiological tests.
As in other studies, donor parameters (age, gender and causes of death) did not influence the rate of skin graft contamination (Forsell and Liesman 2000; Lannau et al. 2015; May et al. 1985; Pianigiani et al. 2010; Schubert et al. 2012; Vehmeyer et al. 2002), and neither did the hospital where procurement took place, or the operating team. The number of NHBDs in our population was too small for statistical analysis of the possible relationship between the type of donor and the contamination rate, which has been reported elsewhere (Forsell and Liesman 2000; Pianigiani et al. 2010). Among MOHBDs, the stay in intensive care was significantly longer for donors with contaminated skin, but it did not influence the type of microbial contaminants (data not shown). This suggests that longer stays in the hospital environment may increase the skin bioburden and make the decontamination process less effective. The processing intervals (time between death and clamping, and time between clamping and cryopreservation) did not have a statistically significant impact on the contamination rate in our study, confirming the results of several previous studies (Deijkers et al. 1997; Forsell and Liesman 2000; Lannau et al. 2015; Schubert et al. 2012; Vehmeyer et al. 2002).
As we separately harvest 8 or 10 zones from each donor and only discard contaminated zones, we were able to use 68 % of the total surface area harvested from the 99 contaminated donors. This individual processing of different zones thus saved a considerable amount of skin (147,507 cm2) from being discarded.
In conclusion, microbial contamination continues to be the main cause of skin allograft discard after harvesting at the Saint Louis Hospital tissue bank. However, the separate harvesting and treatment of between 8 and 10 zones per donor reduces the surface area rejected because of microbial contamination. We encourage all tissue banks to share their procedures and experience, as this would help to compare different approaches and thereby increase the efficiency of donor skin procurement.
Abbreviations
- MOHBDs:
-
Multi-organ heart-beating donors
- NHBDs:
-
Non-heart-beating donors
References
Achermann Y, Goldstein EJC, Coenye T, Shirtliff ME (2014) Propionibacterium acnes: from commensal to opportunistic biofilm-associated implant pathogen. Clin Microbiol Rev 27:419–440
Agence de la biomédecine (2012). Annual report
Beele H, van Wijk MJ, Parker R, Sánchez-Ibáňez J, Brubaker SA, Wulff B, Richters CD, Cox M, Warwick RM, Eastlund T (2013) Report of the clinical donor case workshop of the European Association of Tissue Banks annual meeting 2012. Cell Tissue Bank 14:561–570
De Backere AC (1994) Euro Skin Bank: large scale skin-banking in Europe based on glycerol-preservation of donor skin. Burns J Int Soc Burn Inj 20(Suppl 1):S4–S9
Deijkers RL, Bloem RM, Petit PL, Brand R, Vehmeyer SB, Veen MR (1997) Contamination of bone allografts: analysis of incidence and predisposing factors. J Bone Joint Surg Br 79:161–166
Forsell JH, Liesman J (2000) Analysis of potential causes of positive microbiological cultures in tissue donors. Cell Tissue Bank 1:111–115
Gaucher S, Elie C, Vérola O, Jarraya M (2012) Viability of cryopreserved human skin allografts: effects of transport media and cryoprotectant. Cell Tissue Bank 13:147–155
Gaucher S, Duchange N, Jarraya M, Magne J, Rochet J-M, Stéphanazzi J, Hervé C, Moutel G (2013) Severe adult burn survivors. What information about skin allografts? Cell Tissue Bank 14:505–510
Ireland L, Spelman D (2005) Bacterial contamination of tissue allografts—experiences of the donor tissue bank of Victoria. Cell Tissue Bank 6:181–189
Kearney JN (2005) Guidelines on processing and clinical use of skin allografts. Clin Dermatol 23:357–364
Kobayashi H, Oethinger M, Tuohy MJ, Procop GW, Bauer TW (2009) Improved detection of biofilm-formative bacteria by vortexing and sonication: a pilot study. Clin Orthop 467:1360–1364
Lannau B, Van Geyt C, Van Maele G, Beele H (2015) Analysis of potential factors affecting microbiological cultures in tissue donors during procurement. Cell Tissue Bank 16:65–71
Lindford AJ, Frey I, Vuola J, Koljonen V (2010) Evolving practice of the Helsinki Skin Bank. Int Wound J 7:277–281
Lomas RJ, Huang Q, Pegg DE, Kearney JN (2004) Application of a high-level peracetic acid disinfection protocol to re-process antibiotic disinfected skin allografts. Cell Tissue Bank 5:23–36
Mathur M, De A, Gore M (2009) Microbiological assessment of cadaver skin grafts received in a Skin Bank. Burns J Int Soc Burn Inj 35:104–106
May SR, Wainwright JF, DeClement FA (1985) Variables determining the amount of microbial contamination on cadaveric allograft skin used as a biological wound dressing. Burns Incl Therm Inj 11:242–251
May SR, Roberts DP, DeClement FA, Still JM (1991) Reduced bacteria on transplantable allograft skin after preparation with chlorhexidine gluconate, povidone-iodine, and isopropanol. J Burn Care Rehabil 12:224–228
Neely AN, Plessinger RT, Stamper B, Kagan RJ (2008) Can contamination of a patient’s allograft be traced back to the allograft donor? J Burn Care Res: Off Publ Am Burn Assoc 29:73–76
Obeng MK, McCauley RL, Barnett JR, Heggers JP, Sheridan K, Schutzler SS (2001) Cadaveric allograft discards as a result of positive skin cultures. Burns J Int Soc Burn Inj 27:267–271
Pianigiani E, Risulo M, Ierardi F, Sbano P, Andreassi L, Fimiani M, Caudai C, Valensin PE, Zazzi M (2006) Prevalence of skin allograft discards as a result of serological and molecular microbiological screening in a regional skin bank in Italy. Burns J Int. Soc Burn Inj 32:348–351
Pianigiani E, Ierardi F, Cuciti C, Brignali S, Oggioni M, Fimiani M (2010) Processing efficacy in relation to microbial contamination of skin allografts from 723 donors. Burns J Int Soc Burn Inj 36:347–351
Pirnay J-P, Verween G, Pascual B, Verbeken G, De Corte P, Rose T, Jennes S, Vanderkelen A, Marichal M, Heuninckx W et al (2012) Evaluation of a microbiological screening and acceptance procedure for cryopreserved skin allografts based on 14 day cultures. Cell Tissue Bank 13:287–295
Pitt TL, Tidey K, Roy A, Ancliff S, Lomas R, McDonald CP (2014) Activity of four antimicrobial cocktails for tissue allograft decontamination against bacteria and Candida spp. of known susceptibility at different temperatures. Cell Tissue Bank 15:119–125
Portillo ME, Salvadó M, Alier A, Martínez S, Sorli L, Horcajada JP, Puig L (2014) Advantages of sonication fluid culture for the diagnosis of prosthetic joint infection. J Infect 69:35–41
Schubert T, Bigaré E, Van Isacker T, Gigi J, Delloye C, Cornu O (2012) Analysis of predisposing factors for contamination of bone and tendon allografts. Cell Tissue Bank 13:421–429
Shin K, Yun Y, Yi S, Lee HG, Cho J-C, Suh K-D, Lee J, Park J (2013) Biofilm-forming ability of Staphylococcus aureus strains isolated from human skin. J Dermatol Sci 71:130–137
Singh S, Blevins M-B, Wakeman M, Bergevin M (2012) The utility of recovery biopsies in determining donor suitability. Cell Tissue Bank 13:565–567
Van Geyt C, Van Wijk M, Bokhorst A, Beele H (2010) Physical examination of the potential tissue donor, what do European tissue banks do? Clin Transplant 24:259–264
Vehmeyer S, Wolkenfelt J, Deijkers R, Petit P, Brand R, Bloem R (2002) Bacterial contamination in postmortem bone donors. Acta Orthop Scand 73:678–683
Verbeken G, Verween G, De Vos D, Pascual B, De Corte P, Richters C, De Coninck A, Roseeuw D, Ectors N, Rose T et al (2012) Glycerol treatment as recovery procedure for cryopreserved human skin allografts positive for bacteria and fungi. Cell Tissue Bank 13:1–7
Acknowledgments
The authors would like to thanks Dr. Jean-Luc Donay from the microbiology department of Saint Louis Hospital as well as Thierry Marchix, Chantal Schaffart, and all the members of the Tissue Bank technical team. Thanks to Dr. Sophie Olson for revising this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Sonia Gaucher and Zena Khaznadar have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Gaucher, S., Khaznadar, Z., Gourevitch, JC. et al. Skin donors and human skin allografts: evaluation of an 11-year practice and discard in a referral tissue bank. Cell Tissue Bank 17, 11–19 (2016). https://doi.org/10.1007/s10561-015-9528-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-015-9528-3