Abstract
The menisci of the knee are two crescent shaped cartilage shock absorbers sitting between the femur and the tibia, which act as load sharers and shock absorbers. Loss of a meniscus leads to a significant increase in the risk of developing arthritis in the knee. Replacement of a missing meniscus with allograft tissue can reduce symptoms and may potentially reduce the risk of future arthritis. Meniscal allograft transplantation is a complex surgical procedure with many outstanding issues, including ‘what techniques should be used for processing and storing grafts?’, ‘how should the allografts be sized?’ and ‘what surgical implantation techniques might be most appropriate?’ Further clinical research is needed and close collaboration between the users (surgeons) and the suppliers (tissue banks) is essential. This review explores the above subject in detail.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
What are the menisci?
The menisci of the knee are two crescent shaped elastic cartilages that sit inside the knee between the surfaces of the femur and the tibia (Fig. 1). In the past it was presumed that the menisci were of no functional importance and that they were merely vestigial remnants of a muscle within the knee. However, from the 1970s onwards interest in the menisci grew and their true importance began to be appreciated. It is now understood that they have a number of roles within the knee; foremost, they are load sharers and shock absorbers (Fig. 2), however, they are also secondary stabilisers of the knee joint plus they play a part in proprioception, lubrication of the joint surfaces and nutrition of the articular cartilage layer covering the ends of the bones.
Meniscal tears and meniscectomy
Meniscal tears (Fig. 3) are very common, with an incidence of approximately 61 per 100,000 population per year (Baker et al. 1985). In younger patients they tend to occur through sports injuries, such as when twisting on a bent knee, from football or rugby tackles or from skiing injuries. In older patients the meniscal cartilages may degenerate and become less elastic, and tears may occur with minimal trauma or even spontaneously. Meniscal tears tend to cause pain, swelling, clicking, giving way and locking of the knee joint.
In the past the treatment of choice for symptomatic meniscal tears was to perform an open total meniscectomy, i.e. the knee joint was opened up through a large incision and the damaged meniscal cartilage was removed in its entirety.
The true consequences of meniscectomy are now fully appreciated (McDermott and Amis 2006). Without the menisci in place the joint contact surface areas decrease and the peak contact pressures increase significantly, by somewhere in the region of 235% (Baratz et al. 1986). Excessive stress on the articular surfaces of the femur and the tibia causes damage to the articular cartilage, leading to wear and tear and secondary osteoarthritis. The risk of arthritis developing in a knee is increased 14-fold by a point 21 years after total meniscectomy (Roos et al. 1998).
Thus, significant effort has been focussed over more recent years on meniscal preservation whenever feasible. Meniscal repair techniques have evolved greatly, with modern repair devices allowing highly effective repair of many meniscal tears arthroscopically, with minimally invasive keyhole surgery. One device, of a number available is the Smith and Nephew Ultra-Fast-Fix (Warwick, UK) which consists of two tiny plastic anchors with sutures attached that are connect by a slip knot, allowing tears to be repaired arthroscopically with very strong and effective sutures (Fig. 4). The success rate for meniscal repair using such techniques has been reported to be as high as approximately 90% (Kotsovolos et al. 2006), although clearly success rates will vary depending on the threshold employed by the individual surgeon when determining which meniscal tears to resect and in which they might attempt a repair.
However, the menisci have a very poor blood supply, with only the outer peripheral one-third of the tissue being vascularised. Tears in this ‘red zone’ may potentially heal, sometimes even on their own without surgical repair. Tears in the inner avascular ‘white zone’ are extremely unlikely to heal, with or without surgical suturing. In addition, only certain morphologies of tear are actually repairable; vertical circumferential tears lend themselves nicely to repair, whereas radial tears, flap tears, complex tears and degenerate tears tend to be irreparable. In my own practise, approximately 25% of meniscal tears in patients under the age of 40 are found to be suitable and appropriate for meniscal repair at arthroscopy.
There therefore exist a significant number of patients who present with a meniscal tear that is irreparable and who require a partial or sub-total meniscectomy. These patients normally do well post-operatively in the short-term, but are at risk of developing increasing wear and tear and symptoms in the future. In addition, there is a significant number of patients who have undergone meniscectomy in the past, and who later present with painful knees with varying degrees of established articular cartilage wear and arthritis. For these patients options are limited and treatment is difficult.
The history and results of meniscal transplantation
In the past, various tissues have been used in an attempt to replace missing meniscal tissue, including autologous tissues such as patellar, Achilles or semitendinosus tendon autograft (Johnson and Feagin 2000; Kohn 1993; Kohn et al. 1992), fat pad autograft (Kohn et al. 1997) and autologous rib perichondral grafts (Bruns et al. 1998), as well as synthetic silastic (Kenny et al. 1983), carbon fibre (Veth et al. 1983), Dacron (Sommerlath and Gillquist 1992) and Teflon (Messner 1994) prostheses. These various innovations have, unfortunately, met fairly universally with poor results.
From this position, the concept of replacing missing meniscal tissue with donor allograft tissue was first brought to the fore by Milachowski, a German surgeon, in 1989. He presented the first reported series of patients receiving meniscal allograft transplantations (Milachowski et al. 1989). Since then, meniscal allograft transplantation has been the focus of much interest and research, with over 4,000 transplants having been performed to-date in the US (personal communication, Kevin Stone, San Francisco, US). In Europe Professor Rene Verdonk, of Gent, Belgium, has performed over 100 meniscal transplants (Verdonk et al. 2006). Within the UK, there is at present only a small number of surgeons currently offering this procedure, although interest in the UK is certainly growing (see www.meniscalstudygroup.co.uk) and these numbers are slowly increasing.
On September 5th, 1998 an expert group of Orthopaedic Surgeons met in Copenhagen, Denmark, to discuss the subject of meniscal transplantation (Backer 1999). The group included Professor Marlowe Goble (USA), Professor Dieter Kohn (Germany), Professor René Verdonk (Belgium) and Professor Karola Messner (Sweden). The group came to a consensus opinion regarding the aims of meniscal transplantation, which are:
-
to reduce the pain experienced by some patients following meniscus resection,
-
to restore optimally the mechanical properties of the knee joint after meniscus resection,
-
to prevent the degenerative changes of cartilage and the changes in subchondral bone following meniscus resection, and
-
to avoid or reduce the risk of arthrosis (arthritis) following meniscal resection.
The indications for meniscal transplantation laid out by this group are quite specific. The patient must have undergone a previous meniscectomy and must be presenting with significant knee symptoms but without them having yet developed significant arthritis. If significant degeneration of the articular cartilage is already present then there is concern that any graft that might be implanted would be subjected to excessive stresses, including abrasive wear from the roughened articular surfaces, potentially leading to early failure of the graft. Some US centres do still advocate the technique of meniscal transplantation in patients whose knees already have significant established arthritis, for what is acknowledged will be only temporary pain relief, with a view to potentially delaying the time when joint replacement will become necessary (Stone and Walgenbach 2000). However, this practise is considered contentious by some surgeons.
The reported results of meniscal transplantation are generally very good. Cameron and Saha (Cameron and Saha 1997) reported the results of 67 meniscal allografts in 63 patients at a mean follow-up of 31 months (range 1–5 years). In five cases, the procedure was combined with an anterior cruciate ligament reconstruction, and in four cases the meniscal transplantation was combined with an upper tibial or lower femoral realignment osteotomy. There was a 90.5% good or excellent outcome in the isolated meniscal transplantation group, an 80% good or excellent outcome after transplantation combined with anterior cruciate ligament reconstruction, and 85.3% good or excellent results after transplantation combined with realignment osteotomy. In six cases, a traumatic tear of the posterior horn of the graft was observed.
Stollsteimer et al. (2000) published the results of 23 meniscal allograft transplants into 22 patients at a 1- to 5-year follow-up. Cryopreserved grafts were inserted using an arthroscopically-assisted technique with bone plugs attached to the anterior and posterior horns, secured to tibial bone tunnels. The mean age of the patients was 31 years (range, 20–42 years), and 12 grafts were lateral and 11 medial. The mean time interval between previous meniscectomy and subsequent meniscal transplantation was 45 months (range 3 months–15 year), and the mean post-transplantation follow-up was 40 months. Pain was assessed with a 4-point graded scale. 5 patients reported an improvement of 2 grades, 13 improved by 1 grade, 3 showed no improvement and 1 had a worsening of pain by 1 grade. Magnetic resonance imaging evaluation showed that there was a mean decrease in size of the graft of 62% (range 31–100%), compared to the corresponding normal meniscus in the opposite knee.
Rath et al. (2001) reported the outcome after meniscal transplantation of 22 deep frozen or cryopreserved grafts in 18 patients, with a mean follow-up of 5 years. They observed a decrease in pain, with a significant increase in function, although function did still remain limited. Eight of the grafts tore, necessitating 6 partial and 2 total meniscectomies.
Verdonk et al. (2006) published the results of their first 100 meniscal transplantation procedures using viable (fresh) allografts. There were 39 medial and 61 lateral meniscal transplantations, and the outcomes were evaluated after a mean of 7.2 years. About 28% of the medial and 16% of the lateral grafts failed, with failure being defined as moderate occasional or persistent pain or poor function. The mean cumulative graft survival time was 11.6 years. The survival rates for the medial and lateral allografts at 10 years were 74.2 and 69.8%, respectively.
Full analysis of the true effectiveness of meniscal transplantation is, however, extremely difficult as to-date no prospective randomised controlled clinical trials have been undertaken. Indeed, given the good results published to-date, it now seems relatively unlikely that any such trials would be feasible, given that patients tend to present with significant symptoms, often specifically requesting the procedure having researched the subject themselves on the internet, and thus they are unlikely to take well to being randomised into an arm of a trial where they receive no treatment. In addition, many meniscal transplantation procedures are performed in conjunction with other concomitant procedures, such as reconstruction of torn anterior cruciate ligaments or realignment osteotomies of the bones for malalignment of the joint, making evaluation solely of the meniscal transplant procedure very difficult. Furthermore, the numbers of patients actually receiving these procedures is small, making it near impossible to get good power in comparative studies.
The main issues of contention
To complicate a complex field even further, there are a number of specific issues within the field of meniscal transplantation where there is considerable lack of clarity, difference of opinion and debate. These include:
-
How should meniscal allografts be processed and stored?
-
What surgical techniques should be used to implant the graft?
-
How should the donor allografts be appropriately size matched to the recipient patient’s knee?
How should meniscal allografts be processed and stored?
There are different options available for the type of meniscal allograft that might be used, in terms of how the graft is processed, sterilised and stored. Different types of processing complicate comparison of outcomes between different clinical series. Some surgeons have chosen to use fresh ‘viable’ allografts. For example, in Gent, Belgium, the orthopaedic team harvest meniscal allografts themselves, in theatre in a sterile fashion, from local donors (Verdonk et al. 2006). The grafts are then kept bathed in a culture medium consisting of the intended recipient’s serum plus a cocktail of antimicrobials. The graft is kept for a maximum of 2 weeks before surgical implantation (Fig. 5). However, in other areas such as in some centres in the US, some grafts are harvested from newly deceased donors outside of the standard sterile operating theatre environment, which increases potential concerns over the risks of contamination.
The use of fresh allografts does raise a number of important concerns, particularly relating to screening against microbial disease transmission. Testing the deceased donor for blood borne viruses, awaiting bacterial culture results and the result of other donor health checks such as information from the general practitioner of the donor or the results of any post-mortem if such is undertaken can take weeks or even months to become available. This is one argument that supports the use of stored banks of frozen allografts, where plenty of time is available to complete a full screening and testing process. Furthermore, the use of banks of frozen allografts allows an opportunity for the grafts to be sized, so that the surgeon can choose a size-matched graft from a selection of available sizes and shapes.
In the past, some attempts were made to use freeze-dried, or lyophilised allografts. However, the clinical results from the use of these grafts were poor (Milachowski et al. 1989), with significant post-implantation shrinkage observed. The use of lyophilised grafts has, as a result, been abandoned.
The two main processing/storage techniques most widely used in current practise seem to be cryopreservation and fresh-freezing. Cryopreservation involves controlled rate freezing of the tissue down to very low temperatures, in the region of −196°C, with the graft bathed in a cryoprotectant of glycerol or dimethyl sulphoxide that protects cells from rupture and death from water crystal formation. However, even with optimal conditions, only approximately 10% of meniscal cells remain metabolically active although overall biosynthetic activity of the tissue persists at approximately 50%, showing that those surviving cells that are viable compensate by increasing their metabolic activity (Arnoczky et al. 1988). The unfortunate reality of real clinical practise is that the strict protocols for the thawing of a cryopreserved graft may well not be followed closely. In addition, the meniscal cells that do remain viable tend to be those in closest contact with the cryoprotectant, towards the surface layers of the graft. However, this is the very part of the graft that is the first to become populated by the ingrowth of cells from the recipient. It is the deeper layers of the tissue that is undoubtedly the region that is the last to be repopulated with host cells, and yet this is the area where the donor cells are least likely to survive the cryopreservation process. There is also no convincing evidence that the cryopreservation process maintains the mechanical integrity of the matrix of the meniscal graft tissue any better than fresh-freezing. Only clinical studies can elucidate which of these factors may be of importance, but to-date there are no such studies within the published literature.
With fresh-freezing, meniscal tissue is harvested from donors, washed thoroughly and then packaged and frozen at −80°C. Prior to freezing, various options exist for sterilisation, including chemical decontamination with, for example, ethanol and/or antibiotics, or sterilisation with gamma irradiation. Concerns do exist, however, with the use of irradiation, as although irradiation can cause cross-linking of collagen, in higher doses it causes dose-dependent scission and structural breakdown, reducing mechanical integrity of the tissue (Cheung et al. 1990). The International Atomic Energy Agency adopted 2.5 Mrad as the standard irradiation dose for medical products sufficient to eradicate virus particles. However, the process of irradiating the tissue can give variable doses to different portions of the graft, particularly when associated tissues such as tibial plateau bone are still attached to the meniscal graft. Studies have demonstrated that with doses above 2.5 Mrad, significant tissue weakening occurs (Cheung et al. 1990), however, there is evidence that virus particles may not necessarily be inactivated by these lower ‘tissue friendly’ doses, particularly for tissue such as bone.
A previously unpublished questionnaire study demonstrated what appeared to be a quite alarming lack of knowledge or even interest amongst orthopaedic surgeons regarding the details and science behind the different types of graft available, and it would appear that there is a significant need for further informed debate and education in this whole aspect of the use of allografts in reconstructive surgery of the knee. In addition, there is a need to investigate further the in vivo relevance of the laboratory based biomechanical studies that do exist within the literature, through rigorous clinical studies.
What surgical techniques should be used to implant the graft?
The mechanical function of the menisci is entirely dependent on the ultrastructural arrangement of the tissue. The menisci consist predominantly of circumferentially orientated type-I collagen fibres, running in continuity from bone, to insertional ligament, to meniscal tissue, back to insertional ligament and through to bone. As the axially directed forces bear down through the knee there is a tendency for the meniscal tissue to be extruded peripherally. Tension develops along the circumferential collagen fibres and these are referred to as ‘hoop stresses’ (Jones et al. 1996), (Fig. 6). The forces involved are very large and any interruption in the continuity of the collagen fibre to bone construct will defunction the tissue.
Biomechanical studies have confirmed the importance of maintaining the integrity of the interface between the meniscus and the bone of the allograft tibial plateau. It has been demonstrated that contact pressures within the joint after meniscectomy can be restored by meniscal transplantation techniques that include the use of a bone block of allograft tibial plateau attached to the meniscal graft. However, when meniscal tissue is implanted by suturing techniques alone, without any direct bony fixation, contact pressures are restored to a significantly lower degree, demonstrating that appropriate function is probably not so well re-established (McDermott et al. 2008).
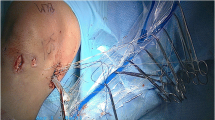
The actual surgical technique of implanting a meniscal allograft is highly demanding. The technique of suturing a graft in place without bone blocks is challenging enough. However, implanting a graft along with a block or plugs of bone is even more difficult (Fig. 7), and many surgeons favour the suturing-only technique, with encouraging surgical outcomes being reported in the literature (Verdonk et al. 2006) despite the published biomechanical studies. The surgeons who do advocate the suturing-only technique do emphasise the importance of a good intact peripheral meniscal rim, to which the allograft can be attached. Thankfully, most modern-day meniscectomies are as conservative as possible, and the peripheral meniscal rim can normally be preserved in most cases. An intact rim may significantly improve the biomechanical function of a sutured allograft, although this is an area that has not yet received appropriate attention by investigation with biomechanical studies.
Meniscal transplantation with bone block fixation—cadaveric specimens. a A drill guide is used to pass a guide wire horizontally from anterior to posterior, in line with the attachment points of the meniscal insertional ligaments, 7 mm distal to the level of the tibial joint line. b An 11 mm cannulated drill bit is then used over the guide wire to create an 11 mm diameter tunnel. c A 5–6 mm section of the osseochondral roof of the tunnel is removed using bone rongeurs. d Tibial plateau section with medial meniscus excised. A 2 cm × 2 cm block of bone is removed using a hacksaw, with the insertional ligament attachments kept intact, centrally. e The outline of the template is drawn on the graft bone block, and the bone block is trimmed to shape. f The tibial drill guide is passed over the bone block and a guide wire is drilled horizontally from anterior to posterior, in line with the attachment points of the insertional ligaments and 7 mm inferior to the level of the joint surface. g The bone block with the guide wire is then mounted in a special jig and a serrated corer is used to create a cylindrical plug of bone containing the insertional ligament attachments. h Meniscal allograft held on guide wire, about to be inserted into tibial tunnel. Note, LCL origin detached, and posterior meniscal suture in place, to pull graft posteriorly into compartment. i Meniscal allograft in place with LCL secured back into position
The operative techniques of meniscal transplantation are still evolving, with dedicated surgical instrumentation now being available commercially. However, debate around these issues still rages.
How should the donor allografts be appropriately size matched to the recipient patient’s knee?
If a meniscal graft is simply sutured into a knee, then there exists some degree of leeway for adjusting the fixation of the graft to accommodate for discrepancies in size matching between the new versus the original recipient’s meniscus. However, if a graft is inserted along with a continuous block of tibial plateau allograft bone, then accurate size matching becomes vital.
Cadaveric pressures studies have demonstrated that malpositioning of a meniscal insertion site on the tibial plateau by as little as 5 mm will significantly reduce the function of a graft (Sekaran et al. 2002). Dienst et al. (2007) showed that mismatch of graft sizing by as little as 10% leads to significant problems within the knee joint; if the graft is too large then it will not bear load and the forces on the articular cartilage will increase; if the graft is too small then the forces across the meniscus are increased and this can lead to failure of the graft.
If accurate size matching is going to be achieved then the only feasible way to achieve this is for grafts to be available from a bank with an inventory with a wide spectrum of sizes. This is in addition to the obvious requirement to match left versus right plus medial versus lateral.
Consideration must be given towards the methods employed for determining what graft sizes are required. The menisci are complex asymmetric structures that are difficult to define in simple terms. Various sizing and matching protocols have been suggested to try to match the age, sex, height and weight of the recipient and donor (Stone et al. 2007). However, most surgeons rely on radiological investigations, with either X-rays or MRI scans (Rath et al. 2001). Again, there is much debate as to which sizing methodologies might be most accurate and reliable and there appears to be little clear consensus of opinion.
Pollard et al. (1995) studied meniscal size by marking menisci with radiopaque tantalum powder-cyanoacrylic paint, and correlating their dimensions with specific bony landmarks on plain AP and lateral knee radiographs. They showed that the coronal and sagittal dimensions of the menisci could be determined from plain radiographs to within a mean error of 8.4% or less. Shaffer et al. (2000) also determined the accuracy of radiographic techniques for preoperative sizing of meniscal allografts and found that the mean difference between radiographic measurements and actual meniscal dimensions was 2.35 ± 1.79 mm. However, in a study examining the value of different radiographic measurement techniques, it was demonstrated that meniscal sizes can be predicted from measuring only the total bony plateau width (McDermott et al. 2004); the mean percentage error for calculating meniscal dimensions of width and height was 5.0% when using specific tibial dimensions, compared to 6.2% when relying on total plateau width only, which was not a significant difference.
Some authors have suggested that MRI might be more accurate for sizing of meniscal allografts (Haut et al. 2000). Clinical practise, however, varies widely, with some surgeons requesting from their tissue bank several different parameters about the graft dimensions and donor characteristics, whilst other surgeons ignore graft size altogether. There is clearly, a significant need to clarify further this whole aspect of the use of meniscal allografts.
Specific adverse reactions
Thankfully, excluding the various potential surgical risks that exist in common with any major surgical procedure, significant problems specifically relating to the use of meniscal allograft tissues have remained rare.
One of the greatest concerns expressed by most patients is the potential risk of disease transmission from allograft tissue. In 1989, it was estimated that the risk of obtaining an allograft (bone) from an unrecognised HIV infected donor in the USA was approximately one in 1.6 million (Buck et al. 1989). Since that time, the HIV epidemic has grown worldwide, but also, the polymerase chain reaction test for HIV has become available, and tissue bank regulations in the US and Europe require careful donor selection to reduce the risk, so the estimated risk may, therefore, continue to be relatively remote. Nonetheless, transmission of disease has been well documented, although such events are rare (Eastlund and Strong 2003).
All tissue processed in the UK or imported into the UK is now subject to the safety requirements of the EC Tissues and Cells Directives, which have been transposed into UK law, and against which the Human Tissue Authority inspects tissue facilities. Allograft tissue must be provided through an accredited tissue bank. Criteria for safe processing and sterilisation techniques are carefully quality assured, and thankfully the incidence of contamination of graft tissue with subsequent infection in the patient is extremely rare.
Meniscal tissue itself is described as ‘immunopriviledged’, in that because the cells are embedded within dense mucopolysaccharide matrix they are protected from the immune response (Elves 1976). Although patients have been found to develop antibodies against human leucocyte antigens (HLA) from the donor meniscal tissue, evidence of clinical or histological signs of rejection are extremely rare, with only one report of a failed meniscal transplantation that may have been attributable to acute rejection having been reported in the literature (Hamlet et al. 1997).
The future of meniscal allograft transplantation
The use of allograft tissue for meniscal replacement is most probably the best surgical option currently available for that proportion of patients meeting the stringent selection criteria for that procedure. However, it undoubtedly represents just one temporary step in the evolution of a process that will inevitably develop into the use of tissue engineering techniques to grow new replacement host tissue for individual patients.
Collagen scaffolds, such as the Menaflex Collagen Meniscal Implant (ReGen Biologics, NJ, USA), which is made from processed bovine Achilles tendon, are already now available for replacing meniscal tissue after partial meniscectomy where the peripheral rim is still intact (Fig. 8). Studies have demonstrated biological compatibility, with ingrowth of host tissue into the scaffold. Clinical results to-date seem encouraging, with decreased pain, increased function and reduction in the number of subsequent surgical procedures being required (Rodkey et al. 2008).
In the future we will hopefully see the development of scaffolds that are seeded with the patient’s host cells in bioreactors that impose a suitable mechanical environment to induce appropriate cell types, thus building a new meniscus for the specific patient. However, in association with this, the challenge will be to incorporate bone substitute blocks firmly attached to the ends of the new meniscal tissue, to allow solid fixation into the recipient’s knee with a graft that exactly matches the dimensions of the missing meniscus. In addition, grafts may carry specific growth factors to encourage rapid biological incorporation of the graft to the recipient’s tissues.
In the present, however, meniscal allograft transplantation represents a highly encouraging addition to the armamentarium of the reconstructive knee surgeon, with the anticipation that demand for this procedure is likely to increase. The expert group at the 1998 Copenhagen meeting estimated that in Denmark (population 5 million) there were likely to be between 10 and 50 suitable candidates for meniscal transplantation a year (Backer 1999). Extrapolating these figures to the UK population, there may be a need for up to 100–500 such procedures in the United Kingdom each year.
In 2002 National Health Service Blood and Transplant (NHSBT) Tissue Services (TS) and The British Association for Surgery of the Knee (BASK) developed a ‘User Group’ to facilitate professional interaction between the major provider, NHSBT TS, and the major clinical users of soft tissue allografts (tendon, ligament and meniscus) in the UK. The UK Meniscal Study Group is also represented on this User Group. At the time of writing, agreement has been reached on the establishment of a pilot project to collate usage and outcome data for soft tissue allograft surgery of the knee in the UK. It is hoped that collaborative initiatives such as this will help to promote appropriate practise and techniques and encourage further audit and research into this exciting field of surgery.
References
Arnoczky SP, McDevitt CA, Schmidt MB, Mow VC, Warren RF (1988) The effect of cryopreservation on canine menisci: a biochemical, morphologic, and biomechanical evaluation. J Orthop Res 6(1):1–12
Backer M (1999) Meniscus transplantation–consensus declaration [editorial]. Scand J of Med Sci Sports 9(3):131–133
Baker PE, Peckham AC, Pupparo F, Sanborn JC (1985) Review of meniscal injury and associated sports. Am J Sports Med 13:1–4
Baratz ME, Fu FH, Mengato R (1986) Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. Am J Sports Med 14:270–274
Bruns J, Kahrs J, Kampen J, Behrens P, Plitz W (1998) Autologous perichondral tissue for meniscal replacement. J Bone Joint Surg 80-B:918–923
Buck BE, Malinin TI, Brown MD (1989) Bone transplantation and human immunodeficiency virus. An estimate of risk of acquired immunodeficiency syndrome (AIDS). Clin Orthop Relat Res 240:129–136
Cameron JC, Saha S (1997) Meniscal allograft transplantation for unicompartmental arthritis of the knee. Clin Orthop Relat Res 337:164–171
Cheung DT, Perelman N, Tong D, Nimni ME (1990) The effect of gamma-irradiation on collagen molecules, isolated alpha-chains, and crosslinked native fibers. J Biomed Mater Res 24:581–589
Dienst M, Greis PE, Ellis BJ, Bachus KN, Burks RT (2007) Effect of lateral meniscal allograft sizing on contact mechanics of the lateral tibial plateau: an experimental study in human cadaveric knee joints. Am J Sports Med 35:34–42
Eastlund T, Strong DM (2003) Infectious disease transmissions through tissue transplantation. In: Phillips GO, Kearney JN, Strong DM, vonVersen R, Nather A (eds) Advances in tissue banking, vol 7. World Scientific, Singapore, pp 51–131
Elves MW (1976) Newer knowledge of the immunology of bone and cartilage. Clin Orthop Relat Res 120:232–259
Hamlet W, Liu SH, Yang R (1997) Destruction of a cyropreserved meniscal allograft: a case for acute rejection. Arthroscopy 13:517–521
Haut TL, Hull ML, Howell SM (2000) Use of roentgenography and magnetic resonance imaging to predict meniscal geometry determined with a three-dimensional coordinate digitizing system. J Orthop.Res 18:228–237
Johnson LL, Feagin JA Jr (2000) Autogenous tendon graft substitution for absent knee joint meniscus: a pilot study. Arthroscopy 16:191–196
Jones RS, Keene GC, Learmonth DJ, Bickerstaff D, Nawana NS, Costi JJ, Pearcy MJ (1996) Direct measurement of hoop strains in the intact and torn human meniscus. Clin Biomech 11:295–300
Kenny C, Krackow KA, McCarthy EF (1983) An evaluation of the effects of a silastic meniscus prothesis on post-meniscectomy osteoarthrosis. Trans Orthop Res Soc 8:335
Kohn D (1993) Autograft meniscus replacement: experimental and clinical results. Knee Surg Sports Traumatol Arthrosc 1:123–125
Kohn D, Wirth CJ, Reiss G, Plitz W, Maschek H, Erhardt W, Wulker N (1992) Medial meniscus replacement by a tendon autograft. Experiments in sheep. J Bone Joint Surg 74-B:910–917
Kohn D, Rudert M, Wirth CJ, Plitz W, Reiss G, Maschek H (1997) Medial meniscus replacement by a fat pad autograft. An experimental study in sheep. Int Orthop 21:232–238
Kotsovolos ES, Hantes ME, Mastrokalos DS, Lorbach O, Paessler HH (2006) Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthroscopy 22:3–9
McDermott ID, Amis AA (2006) The consequences of meniscectomy. J Bone Joint Surg 88-B:1549–1556
McDermott ID, Sharifi F, Bull AM, Gupte CM, Thomas RW, Amis AA (2004) An anatomical study of meniscal allograft sizing. Knee Surg Sports Traumatol Arthrosc 12:130–135
McDermott ID, Lie DT, Edwards A, Bull AMJ, Amis AA (2008) The effects of lateral meniscal allograft transplantation techniques on tibio-femoral contact pressures. Knee Surg Sports Traumatol Arthrosc 16:553–560
Messner K (1994) Meniscal substitution with a Teflon-periosteal composite graft: a rabbit experiment. Biomaterials 15:223–230
Milachowski KA, Weismeier K, Wirth CJ (1989) Homologous meniscus transplantation. Experimental and clinical results. Int Orthop 13:1–11
Pollard ME, Kang Q, Berg EE (1995) Radiographic sizing for meniscal transplantation. Arthroscopy 11:684–687
Rath E, Richmond JC, Yassir W, Albright JD, Gundogan F (2001) Meniscal allograft transplantation. Two- to eight-year results. Am J Sports Med 29:410–414
Rodkey WG, DeHaven KE, Montgomery WH III, Baker CL Jr, Beck CL Jr, Hormel SE, Steadman JR, Cole BJ, Briggs KK (2008) Comparison of the collagen meniscus implant with partial meniscectomy. A prospective randomized trial. J Bone Joint Surg 90-Am:1413–1426
Roos H, Lauren M, Adalberth T, Roos EM, Jonsson K, Lohmander LS (1998) Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum 41:687–693
Sekaran SV, Hull ML, Howell SM (2002) Nonanatomic location of the posterior horn of a medial meniscal autograft implanted in a cadaveric knee adversely affects the pressure distribution on the tibial plateau. Am J Sports Med 30:74–82
Shaffer B, Kennedy S, Klimkiewicz J, Yao L (2000) Preoperative sizing of meniscal allografts in meniscus transplantation. Am J Sports Med 28:524–533
Sommerlath K, Gillquist J (1992) The effect of a meniscal prosthesis on knee biomechanics and cartilage. An experimental study in rabbits. Am J Sports Med 20:73–81
Stollsteimer GT, Shelton WR, Dukes A, Bomboy AL (2000) Meniscal allograft transplantation: a 1- to 5-year follow-up of 22 patients. Arthroscopy 16:343–347
Stone KR and Walgenbach A (2000) Surgical technique of meniscal replacement in arthritic knees. Presented at ESKKA 9th congress, 16–20 September 2000, London, UK
Stone KR, Freyer A, Turek T, Walgenbach AW, Wadhwa S, Crues J (2007) Meniscal sizing based on gender, height and weight. Arthroscopy 23:503–508
Verdonk PC, Demurie A, Almqvist KF, Veys EM, Verbruggen G, Verdonk R (2006) Transplantation of viable meniscal allograft. Surgical technique. J Bone Joint Surg 88-Am(Suppl 1 Pt 1):109–118
Veth RP, den-Heeten GJ, Jansen HW, Nielsen HK (1983) An experimental study of reconstructive procedures in lesions of the meniscus. Use of synovial flaps and carbon fiber implants for artificially made lesions in the meniscus of the rabbit. Clin Orthop Relat Res 181:250–254
Acknowledgment
The author wishes to thank Dr Ruth Warwick (NHSBT TS) for her advice and assistance with the preparation of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McDermott, I.D. What tissue bankers should know about the use of allograft meniscus in orthopaedics. Cell Tissue Bank 11, 75–85 (2010). https://doi.org/10.1007/s10561-009-9127-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-009-9127-2