Abstract
Purpose of Review
To reduce pain, improve function and possibly mitigate the risk for development of osteoarthritis in patients with functionally deficient meniscus pathology, meniscal allograft transplantation (MAT) can be used to restore native joint biomechanics and increase knee joint longevity. This review explores the senior author’s preferred bridge-in-slot technique and recently published long-term clinical and radiographic outcomes following MAT.
Recent Findings
Recent literature demonstrates MAT to be a safe and largely successful procedure for patients with functional meniscus deficiency. A majority of patients reach established minimal clinically important difference (MCID) values. Graft survivorship is approximately 80% at 10 years, significantly delaying and in some cases, preventing the need for future joint reconstruction procedures in these young patients. Return to sport rates are over 70%, revealing meniscal allografts can withstand high impact activities. Cartilage damage at the time of MAT increases the risk for graft and clinical failure, though this may be mitigated with a concomitant cartilage restoration procedure.
Summary
Meniscal allograft transplantation can provide a durable and effective long-term solution to meniscal deficiency in symptomatic patients who wish to decrease the risk of symptomatic progression and possibly further osteoarthritis and continue activities of daily life and sports with less pain and more function. By restoring more normal joint biomechanics, MAT can mitigate the potential need for future knee arthroplasty in this young active patient population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Proper management of meniscal tears to the meniscus are essential to improving knee joint longevity. Treatment for meniscal pathology can consist of repair or partial to total meniscectomy, which can leave patients with a functionally deficient meniscus. Studies have shown that functionally deficient menisci cause severe increases in tibiofemoral contact pressures, which can lead symptom onset, reduced function and potentially, a rapid progression of osteoarthritis [1]. This can result in loss of function of the joint and may ultimately necessitate partial or total knee arthroplasty.
In cases of irreparable tears involving the majority of the meniscus or in patients with a prior total or subtotal meniscectomy, MAT has been shown to restore native knee biomechanics, reduce symptoms, improve function and to possibly prevent the progression of early osteoarthritis. Recent data demonstrate overall success of MAT in young patients with failure rates as low as 14% at 10 years [2] and systematic reviews have revealed significant increases in PRO scores across three separate MAT techniques. This paper will review the senior author’s indications and preferred technique for MAT before exploring the clinical and radiographic outcomes currently reported in the literature. Understanding proper patient selection, along with the risks and benefits of MAT will contribute to informed decisions regarding treatment for patients with a functionally deficient meniscus.
Preoperative Assessment
Patient History
A thorough history is essential in the evaluation of patients with meniscal insufficiency, as other factors may contribute to pain and functional limitations. History should include previous injuries to the affected extremity, prior treatments, response to prior treatments, comorbidities, activity level, and functional goals. Patients with meniscal deficiency often report a history of a knee injury with subsequent arthroscopic surgery involving meniscus repair and/or meniscectomy. There is often a period of symptom improvement following the initial surgery, followed by return of joint line pain and intermittent activity-related effusions. Less obvious stories can include attritional failure of a prior ACL reconstruction due to removal of a bucket handle medial meniscus tear at the time of the original reconstruction.
Physical Examination
Following a detailed history, physical examination should assess standing limb alignment, hip and knee range of motion, joint line tenderness, ligament stability, and gait. Careful inspection of surgical incisions can help elucidate prior surgeries including ligament reconstructions and attempted meniscus repair. Patients with meniscal deficiency often have preserved knee range of motion and can have the presence of an intra-articular effusion depending on recent activity level. Palpation will often reveal tenderness along the affected joint line or femoral condyle. Care should be taken to assess for associated pathologies such as ligamentous instability and limb malalignment.
Secondary indications may include the role of the medial meniscus as a secondary restraint to anterior tibial translation. The multiply failed ACL reconstruction patient may benefit from concomitant medial meniscus transplantation if meniscal deficiency was deemed to be associated with their failure. These patients will also typically have a more significant exam with a Grade 3 Lachman and Grade 3 Pivot shift.
Imaging
Radiographic assessment should routinely include a weightbearing anteroposterior (AP) view of both knees in full extension, a posteroanterior 45° flexion weightbearing view, and a non-weightbearing 30° flexion lateral view. Limb alignment should be assessed using a standing long-leg mechanical axis view. Magnetic resonance imaging (MRI) should be obtained preoperatively to assess the extent of previous meniscectomy, the degree of subchondral edema, and the presence of other pathologies including ligament insufficiency and chondral damage. Correlation of imaging findings with previous operative notes and intraoperative photos is crucial in the preoperative assessment of patients who are being considered for MAT.
Accurate radiographic measurements are needed for sizing of the meniscal allograft. Sizing is typically performed with tibial plateau length and width measurements from a standard AP and lateral radiograph with magnification markers placed at the joint line on the patient’s skin [3]. Appropriate sizing of the meniscal allograft is essential for a successful surgical outcome, as biomechanical studies have shown that oversized grafts lead to greater contact stresses to the articular surface and undersized grafts lead to increased contact stresses on the allograft [4,5,6]. A size mismatch of ≤ 10% is recommended for proper allograft function and normal joint contact-stresses [4,5,6]. MRI can also be utilized to size meniscus if calibrated X-rays are not available.
Indications & Contraindications
The ideal candidate for meniscal allograft transplantation is a patient under the age of 50 with a history of subtotal or total meniscectomy who has a chief complaint of pain localized to the meniscal deficient compartment. Patients should have localized pain that limits their desired activities, ideally with a body mass index (BMI) less than 35 kg/m2, normal or correctable coronal and sagittal alignment, normal or correctable ligamentous stability, normal or correctable articular cartilage, and the ability to comply with postoperative rehabilitation protocols and restrictions.
Contraindications to MAT include patients with asymptomatic meniscal deficiency, skeletally immature patients, Kellgren-Lawrence grade 3 or 4 arthritis, uncorrected ligamentous instability or malalignment, irreparable chondral lesions, history of knee infections, immunodeficiency, or inflammatory arthritis. All previous operative notes, intraoperative photos, and imaging studies should be carefully reviewed to assess for arthritic changes. Patients with correctable malalignment, focal chondral defects, or ligamentous instability should have these issues addressed concomitantly or via staged procedures to ensure optimal outcomes following MAT [7].
Bridge-in-Slot Technique
The author’s preferred technique is the Bridge-in-Slot technique, which allows for retention of the natural shape and anatomy of the meniscal allograft [8]. This technique requires careful selection of donor tissue that will match the size of the patient’s native meniscus.
Positioning
After induction of anesthesia, the patient is positioned supine on a standard operating table that allows the knee to bend freely with removal or lowering of the lower limb extension board and pad. Exam under anesthesia is performed to assess baseline range of motion and rule out concomitant ligamentous laxity with the Lachman and Pivot Shift tests. A tourniquet is placed on the operative leg at the level of the proximal thigh and then the operative thigh is placed in a leg holder. The non-operative leg is placed in a well-leg holder. The foot of the bed is lowered, and the patient’s operative leg is then prepped and draped in sterile fashion. The posteromedial and posterolateral corners of the knee joint must be freely accessible.
Diagnostic Arthroscopy
Standard inferomedial and inferolateral portals are established. A diagnostic arthroscopy is performed to examine the entire joint for cartilage damage, ligamentous pathology, and to confirm meniscus deficiency. Commonly, cartilage damage will be found in the same compartment as the deficient meniscus. If this damage is over Outerbridge grade III in nature, concomitant cartilage restoration procedures should be considered, typically after the meniscus transplant is complete.
Intra-articular Preparation, Arthrotomy, and Slot Preparation
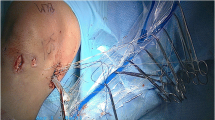
After completion of diagnostic arthroscopy, preparation of the meniscus implantation site can begin. The remnant of remaining meniscus is debrided peripherally to a vascular edge, ideally leaving 1 to 2 mm of peripheral rim intact (Fig. 1). The anterior and posterior roots should be debrided with a shaver so the original positions can still be noticed for placement of the new meniscus.
After localization with a spinal needle, a 2 cm mini-arthrotomy is made extending from the inferior pole of the patella through the patellar tendon in line with the insertion sites of the anterior and posterior roots of the involved meniscus. A line connecting the center of the anterior and posterior horns should be made using electrocautery. This will act as a guide for creating the bone bridge slot. Preparation of the tibial slot is started arthroscopically with a 4 mm bone cutting shaver, making a reference slot so that the shaft of the shaver is flush with the articular surface and also matches the native tibial slope/anatomy. A hooked depth gauge is used to measure the length of the slot along the sagittal plane. A hooked drill guide is placed hooking the posterior tibia at the posterior horn of the meniscus and a guide wire is advanced to the posterior tibial cortex without penetrating the cortex. An 8 mm cannulated reamer is placed over the guide wire and advanced to the posterior tibial cortex. If appropriate care can be taken, the posterior cortex can be removed to make sure the transplant does not bottom out. An 8 mm wide x 10 mm deep box-cutter is used to deepen the bone slot and a rasp then is used to refine the slot in preparation for graft insertion to ensure smooth graft passage (Fig. 2). A hooked ACL drill guide is used to pass a 2.4 mm guide pin through the center of the tibial slot to the ipsilateral posterior aspect of the tibia. This is followed by a 4 mm cannulated reamer to create a tunnel suitable for a transosseous passing stitch.
A posterior 2 cm incision is made on the inner or outer side of the joint in line with the involved compartment, approximately one third above and two thirds below the joint line. Dissection is carried down to the level of the ipsilateral gastrocnemius muscle, which is then elevated off the posterior capsule. A Henning retractor is placed anterior to the gastrocnemius to protect neurovascular structures and allow safe placement of meniscocapsular sutures.
Allograft Preparation
The meniscal allograft consists of a tibial bone bridge connecting the anterior and posterior horns of the donor meniscus. The attachment sites of the meniscus at the anterior and posterior horn are identified and the rest of the meniscus is elevated off the bone block (Fig. 3A). Bone anterior to the anterior meniscal attachment is left for graft integrity while bone posterior to the posterior attachment is removed to facilitate anatomic positioning of the posterior root. A sagittal saw is used to prepare the graft’s bone bridge which should have width of 7 mm and a height of 10 mm. Care should be taken to avoid the native insertions of the meniscus to retain graft integrity (Fig. 3B). The bone bridge should be trimmed to a width 1 mm less than the width of the prepared tibial slot to facilitate graft passage and minimize the risk of bone bridge fracture due to forceful insertion. Sizing is checked with a meniscal sizing block (Fig. 3C). An 0 PDS suture is used to pass a vertical mattress suture at the junction of the posterior third of the meniscal graft for graft passage into the joint (Fig. 3D). A small tape suture is wrapped around the bone block and used to facilitate a transosseous passing stitch.
Lateral Meniscal Allograft preparation. A Meniscus on bone block. B Meniscus allograft is cut to the proper height of 10 mm and removed from the bone block. C Meniscal sizing block is used to ensure proper bone width for easy insertion into the slot. D Passing suture is placed at the junction of the posterior third of the meniscus graft
Allograft Insertion and Fixation
Under arthroscopic visualization through the ipsilateral portal, a zone-specific, inside-out meniscal repair cannula is inserted through the contralateral portal for vertical mattress suture placement. First, a flexible nitinol suture-passing wire is passed through the meniscus repair canula and exits the posterior arthrotomy. The allograft passing suture is passed through the nitinol loop and this is used to bring the graft into the joint through the anterior incision. The bone bridge is manually reduced into the tibial bone slot with care taken to avoid fracture of the bone bridge (Fig. 4). The knee is taken through a full range of motion to confirm proper size and placement of the graft. A single 4.75 mm biocomposite anchor is fixed to the anterior tibia to secure the transosseous suture. Alternatively, an anchor can be placed adjacent to the bone block on the far side to secure the graft in place within the slot. Finally, 8–10 vertical mattress sutures are used to secure the meniscal allograft to the capsule utilizing standard inside-out technique (Fig. 5).
Post Operative Rehab
Patients are placed in a hinged knee brace locked in extension while sleeping, standing, or walking for 3 weeks. Motion is allowed from 0 to 90 for the first 6 weeks.. Heel-touch weight bearing is maintained for the first 6 weeks and can increase 25% per week after 6 weeks. Full range of motion is expected by 8–12 weeks and gentle stationary biking can begin as soon as 8 weeks. High impact activities should be avoided for at least 6 months post-operatively and return to sport is not advisable until physician clearance.
Outcomes
Literature regarding MAT consists largely of level IV evidence studies with heterogenous patient populations and variability in techniques and concomitant procedures. Additionally, many of the studies that report on outcomes after MAT contain patients who had concomitant procedures including cartilage restoration, limb realignment, or ligamentous reconstruction, which limits the ability to interpret outcomes with respect to the contribution of the MAT. Additionally, as the medial and lateral meniscus have different contributions to knee stability, shock absorption, and protection of articular cartilage, MAT procedures to the medial and lateral compartments are substantially different. Though overall evidence regarding outcomes of MAT in appropriately indicated patients is favorable, it is important to take these factors into account and to not overgeneralize findings.
Patient Reported Outcomes
Recent studies benefit from the collection of patient reported outcome scores (PROs) and defining clinically significant outcomes (CSOs) [9, 10•, 11••, 12, 13•, 14•, 15•, 16••]. This allows surgeons to better understand the potential clinical benefit patients may experience after MAT. In the lone randomized controlled trial to date, Smith et al. reports on one-year outcomes for 16 patients who underwent MAT and 20 patients treated nonoperatively with physical therapy at a mean age of 28 for meniscal deficiency [9]. MAT patients reported higher Knee injury and Osteoarthritis Outcome Score (KOOS) composite (p = 0.03), pain (p = 0.02), and activities of daily life (p = 0.005) subscores at study end, with KOOS Quality of Life (p = 0.058) and sports (p = 0.098) subscores trending higher in MAT patients but not reaching statistical significance.
Systematic reviews have also supported favorable clinical outcomes after MAT, often utilizing Lysholm and International Knee Documentation Committee (IKDC) PROs [10•, 11••, 16••]. In one review published in 2023, Leite et al. report on 24 studies with 328 patients to compare outcomes after bone plug, bone bridge, and soft tissue fixation MAT techniques [10•]. They noted improvements in Lysholm score (50.9–73.5 to 66–92.5), IKDC score (45.7–60.3 to 56.0–85.4), Tegner score (2.1–4.5 to 4.0–7.1), and VAS pain scale (4.6–6.8 to 0.9–3.6) after surgery across all techniques. Additionally, they commented on high levels of low-quality level IV evidence (58.3%). The MAT-specific one-year postoperative MCID values for Lysholm (12.3), IKDC (9.9), and KOOS subscores (Pain 9.09, Symptoms 9.7, Activities of Daily Living 9.5, Sport 13.3, and Quality of Life 14.6) were determined by Liu et al. in 2019 [12]. Su et al. performed a meta-analysis to evaluate for MCID achievement after MAT on 35 studies consisting of 1,658 patients [11••]. Using MAT-specific values, Su and colleagues found the mean improvement in Lysholm and IKDC scores across studies met MCID, while KOOS subscores were not evaluated. In the same study, AOSSM Outcomes Task Force MCID values established for all sports related knee injuries (Lysholm = 10.1, IKDC = 16.7, and VAS pain = 2.7) were also used as a measurement of treatment success. All 30 of the studies including Lysholm scores had mean pre- to post-operative score differences that met this definition of MCID achievement, while 75.0% (12 of 16) of studies including IKDC and 85.7% (12 of 14) of studies including the VAS pain scale had mean differences exceeding these MCID values. Similarly, a review by Ahmed et al. notes that the mean difference was greater than MAT-specific MCID values in five of five studies including Lysholm scores, and six of six studies including IKDC scores [13•]. The establishment of clinically significant outcomes (CSOs) such as MCID values allows for greater clinical utility in determining the effectiveness of surgeries such as MAT, and these results indicate that MAT provides the necessary improvement in function and quality of life that patients see clinical benefit.
Worker’s compensation status and body mass index (BMI) are two factors that may affect a patient’s ability to find meaningful clinical improvements after MAT. These variables were found to delay time to MCID and patient acceptable symptomatic state (PASS) achievement by Huddleston et al. in a 2022 case series of 80 patients who underwent MAT [14•]. They noted achievement of MCID of IKDC and all KOOS subscores at a range of 6.0 to 8.0 months and an overall MCID achievement of greater than 50% in their cohort. In a case series conducted by Wagner et al., worker’s compensation status, BMI, and age were associated with reduced odds of achieving MCID and PASS at 5 years follow-up after surgery [15•]. Higher preoperative PRO scores, concomitant bony surgery, and male sex were also associated with failure to achieve MCID, while lower preoperative PRO scores was correlated with failure to achieve PASS.
Additionally, revision MAT produces outcomes comparable to primary MAT. Wagner and colleagues performed a matched-cohort analysis of 16 revision MAT patients and 32 primary MAT age, sex, BMI, and concomitant procedure matched controls with a minimum of 5-year follow up [17]. There were no differences in MCID, PASS, or substantial clinical benefit (SCB) achievement among groups for IKDC, Lysholm, and KOOS subscores. Additionally, both primary and revision MAT patients had 5-year failure rates of 31%.
Graft Survivorship
While PROs can provide meaningful insight into the clinical impact of MAT, it is also necessary to evaluate graft survivorship and identify patients that may be at higher risk for failure. Graft failure is often defined as the need for revision MAT, graft removal, conversion to arthroplasty, or gross failure on second-look arthroscopy. Several recent studies have evaluated the long-term outcomes of MAT grafts.
Approximately 80% of patients are free of graft failure in published reports identifying the long-term success of MAT [2, 18•, 19•, 20]. Two recently published case series look at minimum 10 year outcomes of MAT [2, 18•]. In the largest series, Wagner and colleagues followed 174 patients who underwent bridge-in-slot MAT for a mean of 12.7 ± 2.7 years [18•]. Of these, 37% (65) underwent MAT-related reoperation at a mean of 6.6 ± 5.5 years. Overall, 23% (40) of patients met criteria for failure (defined as revision MAT or conversion to partial or total knee arthroplasty) at a mean of 7.3 ± 5.0 years. Survival rates were reported as 85% at 10 years and 72% at 15 years post-MAT. Grassi et al. followed 38 patients who underwent soft tissue fixation MAT for a minimum of 10 years[2]. Six patients required partial or total meniscectomy resulting in a 14% failure rate, while 27% required any reoperation. Grassi et al. also reported on the outcomes of soft tissue fixation MAT in 324 patients for a mean of 5.7 ± 3.0 years [19•]. Sixty-two (19%) patients required reoperation while 22 (6.8%) experienced a graft revision. No predictive factors for graft failure were identified. In Husen et al., graft failure was categorized into anatomic—tears covering greater than 20% of the allograft, peripheral tear, or dislocation of the graft from unstable fixation—and surgical failure—requiring revision or conversion to arthroplasty [20]. One hundred and fifty-seven patients were followed for a mean of 7 ± 3.5 years, with 14 (8.9%) experiencing surgical failure and 26 (16.6%) anatomic failure. An additional 13 (8.3%) experienced subjective failure with Lysholm scores less than 65. Pre-operative cartilage damage was found to be associated with all types of failure. Concomitant osteochondral allograft (OCA) transplantation and International Cartilage Regeneration & Joint Preservation Society (ICRS) grade were predictors of anatomic (HR 3.05 [95% CI: 1.34–6.92], HR 3.04 [95% CI: 1.31–7.11]) and surgical failure (HR 4.55 [95% CI: 1.46–14.17], HR 3.41 [95% CI: 1.05–11.01]).
Recently published systematic reviews have also shown that high-grade preoperative cartilage defects are predictive for graft failure [16••, 21•, 22]. Wang et al. performed a best-evidence synthesis of 18 studies consisting of 1,920 patients at a mean follow-up of 6.0 years after surgery [22]. Their analysis determined there was strong evidence for the association of cartilage damage severity at the time of surgery and graft failure, while sex, knee compartment, laterality, concomitant anterior cruciate ligament (ACL) reconstruction or osteotomy had no association with failure. Additionally, conflicting evidence was found for an association with failure and older age and kissing cartilage lesions—lesions on both sides of a compartment. Kunze et al. evaluated 17 studies with 2,184 patients reporting an overall failure rate of 17.8% with 5- and 10-year failure rates of 10.9% and 22.7% respectively [21•]. Per quantitative random-effects analysis of International Cartilage Regeneration & Joint Preservation Society (ICRS) grade, knee compartment, and sex, only ICRS grade greater than 3a at the time of primary MAT correlated with a higher odds of graft failure (OR 5.32 [95% CI: 2.75 – 10.31]).
Concomitant procedures to address cartilage defects, malalignment, and ligament insufficiency are commonly performed with MAT and may influence graft survival. Lee et al. performed a systematic review of 24 studies and 1,882 patients to evaluate the effects of combined procedures on patients undergoing MAT [23]. The authors noted that there was insufficient evidence to draw conclusions regarding the effect of realignment, ligamentous, and cartilage procedures on graft survivorship. However, they did report no differences in IKDC, Lysholm, Tegner activity, or VAS pain scores across patients undergoing isolated and combined MAT surgeries. Wang and colleagues performed a systematic review and determined that treating cartilage defects at the time of MAT surgery may mitigate risk for graft failure [16••]. Of potential risk factors, only high-grade cartilage defects were predictive of MAT failure in the majority of studies (5 of 7) in which it was analyzed. In the two studies in which cartilage defects were not determined to be predictive, lesions were treated at the time of surgery. In four of the five studies where an association was present, cartilage lesions were left untreated. Saltzman et al. compared 69 patients who underwent concomitant cartilage restoration procedures with 22 patients who underwent MAT without cartilage defects with a minimum of 2 years of follow up [24]. There were no differences in revision MAT or conversion to arthroplasty rates between those with (15.2% and 3.1%, respectively) and without (10.0% and 5.0%, respectively) cartilage defects addressed at the time of MAT. Similarly, Grassi et al. found similar graft survival rates in patients who underwent MAT with and without concomitant cartilage restoration procedures [19•]. However, they did note a twice as high rate of clinical failure (defined by a Lysholm score of less than 65) in those who underwent concurrent cartilage restoration. Zaffagnini et al. followed eight patients who underwent combined MAT, ACL reconstruction, and varus-correcting high tibial osteotomy (HTO) for a mean of 5.1 years [25]. No patients experienced graft failure and improvements of IKDC (33.3 ± 20.7 to 78.3 ± 9.8), Lysholm (66.3 ± 18.5 to 85.1 ± 7.7), VAS pain (71.3 ± 20.3 to 25.0 ± 14.1), and WOMAC (42.3 ± 17.2 to 10.9 ± 12.0) were seen. Liu et al. evaluated 22 patients who underwent concomitant MAT and HTO at a mean of 9.3 ± 3.7 years after surgery [26]. They reported 9.1% (2) required further cartilage procedures including chondroplasty and OCA, while 4.5% (1) required conversion to arthroplasty at 7.8 years after surgery.
Return to Sport
Athletes are a population of specific importance when considering an MAT. These patients require musculoskeletal demands often not seen in typical everyday activities. Two recent systematic reviews evaluate return to play after MAT with variable results [13•, 27]. In the first, a review published in 2022, Ahmed and colleagues included 14 case series with 670 patients [13•]. Mean age at time of surgery varied from 12.6 to 45.3 years, mean follow-up varied from 2 to 9.3 years, and level of competition ranged from recreational to professional across studies. They noted only two studies with return to play rates of less than or equal to 50%, while the other twelve reported return to play rates ranging from 73.5% to 91.7%. Additionally, for patients that did return to sport, the reported rates of return to the same preinjury level of competition varied considerably ranging from 6.9% to 96.2%, and rates of return to higher levels of competition were greater than 0% in only two studies. A 77.4% return to play rate among 624 patients across 11 studies is noted in a 2020 systematic review by Hurley et al. [27]. In these patients, 68.6% (326 of 475) returned to the same or higher level of competition at a mean of 9.0 months. They highlighted variability across rehabilitation protocols and criteria to return to sport, citing time from surgery as the most common criteria used to guide return and 6 months (in 17 of 45 studies) as the most common timepoint for participation to begin. Interestingly, they also reported that 33.3% (16 of 48 studies) advised against a return to sport. Cvetanovich et al. followed 87 patients for a mean of 3.64 ± 0.88 years to evaluate return to sport rates [28]. Concomitant procedures were performed in 82.7% (72) of patients, with the most common being OCA transplantation (67.8%). In their cohort, 75.6% (62) were able to return to at least one sport at a mean of 12.58 ± 6.20 months after surgery, with 48.3% (30) returning to the same or higher level of play. Sport-specific analysis revealed highest return to sport rates in cycling (76.7%), golf (69.6%), light weight lifting (90.5%), yoga (80.9%), swimming (86.7%), hunting (83.3%), hiking (100%), and snow shoeing (100%). Allahabadi et al. looked exclusively at professional athletes undergoing OCA transplantation [29]. Three patients underwent concomitant OCA and lateral MAT, with two returning to a higher level of play at 9 and 12 months after surgery.
While these studies do indicate favorable outcomes for the athlete undergoing MAT, there are additional factors that must be considered for this specific population. Athletes are often measured on performance and return to play statistics do not wholly encompass the effect of this surgery on long-term career outcomes. Additionally, athletes may be more susceptible to further knee or lower extremity injury as a result of compensating for the allograft, underscoring the importance of proper sport-specific physical therapy and rehabilitation.
Radiographic Outcomes
Radiographs can be used as an easily accessible clinical tool to assess for progression of osteoarthritis following MAT. Studies evaluating long-term radiographic outcomes after MAT are limited, but have found slight increases in Kellgren-Lawrence (KL) grades [30,31,32]. Vundelinckz et al. followed 30 patients for a mean of 12 years and 8 months after MAT, noting increases in KL grade from 1.41 ± 0.56 pre-operatively to 1.97 ± 0.95 at 7.5 years postoperatively and 1.85 ± 1.13 at final follow up [31]. The final follow-up increase in KL grade did not reach statistical significance (p = 0.0522), but authors did note a loss of 6 patients from the previous follow-up time point. Similarly, Saltzman et al. found increases in KL grades from 0.7 ± 0.8 to 1.6 ± 1.9 in 40 patients at a mean of 5.7 ± 3.2 years following concomitant MAT and ACL reconstruction [30]. They noted no patients had a KL grade greater than 4 at any time point. Additionally, they found overall decreased medial and lateral joint space height across this period (5.2 ± 1.1 mm to 4.5 ± 0.8 mm and 5.7 ± 1.1 mm to 4.3 ± 0.9 mm, respectively). Interestingly, they noted no pre- to post-operative difference in joint space height of the same compartment the MAT was performed on. Leite and colleagues’ systematic review found that comparative joint space height was assessed in only four studies. In three studies using bone plug fixation, joint space height did not differ, ranging from 4.4 to 4.9 mm pre-operatively to 4.0 to 4.9 mm 2 to 6.5 years after surgery.
Conclusion
MAT is an effective procedure in reducing pain and restoring function in the meniscal deficient patient. With 10-year success rates around 80% and return to sport rates above 70%, MAT provides favorable long-term clinical outcomes in appropriately indicated patients. Preoperative cartilage damage presents a risk factor for poor outcomes, though addressing these lesions during primary MAT surgery may mitigate this risk.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mahmoud A, Young J, Bullock-Saxton J, Myers P. Meniscal Allograft Transplantation: The Effect of Cartilage Status on Survivorship and Clinical Outcome. Arthroscopy. 2018;34:1871-1876.e1.
Grassi A, Macchiarola L, Lucidi GA, Coco V, Romandini I, Filardo G, et al. Long-term Outcomes and Survivorship of Fresh-Frozen Meniscal Allograft Transplant With Soft Tissue Fixation: Minimum 10-Year Follow-up Study. Am J Sports Med. 2020;48:2360–9.
Haen TX, Boisrenoult P, Steltzlen C, Pujol N. Meniscal sizing before allograft: Comparison of three imaging techniques. Knee. 2018;25:841–8.
Dienst M, Greis PE, Ellis BJ, Bachus KN, Burks RT. Effect of lateral meniscal allograft sizing on contact mechanics of the lateral tibial plateau: an experimental study in human cadaveric knee joints. Am J Sports Med. 2007;35:34–42.
Khoshgoftar M, Vrancken ACT, van Tienen TG, Buma P, Janssen D, Verdonschot N. The sensitivity of cartilage contact pressures in the knee joint to the size and shape of an anatomically shaped meniscal implant. J Biomech. 2015;48:1427–35.
Samitier G, Alentorn-Geli E, Taylor DC, Rill B, Lock T, Moutzouros V, et al. Meniscal allograft transplantation. Part 1: systematic review of graft biology, graft shrinkage, graft extrusion, graft sizing, and graft fixation. Knee Surg Sports Traumatol Arthrosc. 2015;23:310–22.
Yanke AB, Chahla J, Cole BJ, Huddleston H. Medial Meniscus Transplantation and Bone-Tendon-Bone Anterior Cruciate Ligament Reconstruction. 2020. https://doi.org/10.5435/JAAOS-D-20-00363.
Cotter EJ, Frank RM, Waterman BR, Wang KC, Redondo ML, Cole BJ. Meniscal Allograft Transplantation With Concomitant Osteochondral Allograft Transplantation. Arthrosc Tech. 2017;6:e1573–80.
Smith NA, Parsons N, Wright D, Hutchinson C, Metcalfe A, Thompson P, et al. A pilot randomized trial of meniscal allograft transplantation versus personalized physiotherapy for patients with a symptomatic meniscal deficient knee compartment. Bone Joint J. 2018;100-B:56–63.
• Leite CBG, Merkely G, Zgoda M, Farina EM, Görtz S, Howard J, et al. Systematic Review of Clinical Results After Medial Meniscus Allograft Transplantation Reveals Improved Patient Reported Outcomes at Greater Than 5 Years Follow-Up. Arthroscopy. 2023;39:802–11. ()
•• Su L, Garcia-Mansilla I, Kelley B, Arshi A, Fabricant PD, Sherman SL, et al. Clinical Outcomes of Meniscal Allograft Transplantation With Respect to the Minimal Clinically Important Difference. Am J Sports Med. 2022;50:3440–6. ()
Liu JN, Gowd AK, Redondo ML, Christian DR, Cabarcas BC, Yanke AB, et al. Establishing Clinically Significant Outcomes After Meniscal Allograft Transplantation. Orthop J Sports Med. 2019;7:2325967118818462.
• Ahmed AF, Rinaldi J, Noorzad AS, Zikria BA. Return to Sports Following Meniscal Allograft Transplantation Is Possible but Remains Questionable: A Systematic Review. Arthroscopy. 2022;38:1351–61. (Systematic review noting a majority of patients return to sport after MAT in 12 of 14 studies)
• Huddleston HP, Polce EM, Gilat R, Mehta N, Alzein M, Dandu N, et al. Time to Achieving Clinically Significant Outcomes After Meniscal Allograft Transplantation. Cartilage. 2022;13:19476035221102570. (Retrospective case series that determined worker's compensation and BMI were found to delay MAT-specific MCID and PASS achievement)
• Wagner KR, Kaiser JT, Knapik DM, Condron NB, Gilat R, Meeker ZD, et al. Patient-Specific Variables Associated with Failure to Achieve Clinically Significant Outcomes After Meniscal Allograft Transplantation at Minimum 5 Year Follow-Up. Arthroscopy. 2023;39:2327–38. (Retrospective case series that found that worker's compensation, BMI, and age were found to affect MAT-specific MCID and PASS at 5-years after surgery)
•• Wang Z, Credille K, Swindell H, McCormick JR, Darbandi A, Alzein M, et al. Concomitant Treatment of High-Grade Cartilage Lesions Mitigates Risk of Meniscal Allograft Transplant Failure. Arthroscopy. 2023;S0749–8063(23):00940–4. (Systematic review that found concomitant treatment of high-grade cartilage lesions reduces graft failure after MAT)
Wagner KR, Horner NS, Gilat R, Kaiser JT, Meeker ZD, Swindell HW, et al. Revision and Primary Meniscal Allograft Transplantations Provide Clinical Benefit at Mid-Term Follow-Up: A Matched-Cohort Analysis of Patient-Reported Outcomes, Reoperations, and Failures. Arthroscopy. 2024;40:412-421.e1.
• Wagner KR, Kaiser JT, Hevesi M, Cotter EJ, Gilat R, Meeker ZD, et al. Minimum 10-Year Clinical Outcomes and Survivorship of Meniscal Allograft Transplantation With Fresh-Frozen Allografts Using the Bridge-in-Slot Technique. Am J Sports Med. 2023;51:2954–63. (Retrospective case series reporting an 85% survival rate 10-years after MAT)
• Grassi A, Di Paolo S, Coco V, Romandini I, Filardo G, Lucidi GA, et al. Survivorship and Reoperation of 324 Consecutive Isolated or Combined Arthroscopic Meniscal Allograft Transplants Using Soft Tissue Fixation. Am J Sports Med. 2023;51:119–28. (Retrospective case series that found a higher rate of PRO failure in patients who underwent concomitant operation during MAT)
Husen M, Poudel K, Wang A, Saul D, Stuart MJ, Levy BA, et al. Survivorship of 157 Arthroscopic Meniscal Allograft Transplants Using Bone Fixation at a Mean of 7 Years and Prognostic Factors Analysis. Am J Sports Med. 2024;52:96–108.
• Kunze KN, Ramkumar PN, Manzi JE, Wright-Chisem J, Nwachukwu BU, Williams RJ. Risk Factors for Failure After Osteochondral Allograft Transplantation of the Knee: A Systematic Review and Exploratory Meta-analysis. Am J Sports Med. 2023;51:1356–67. (Systematic review finding that high grade cartilage damage at the time of primary MAT was correlated with higher odds of graft failure)
Wang D-Y, Lee CA, Li Y-Z, Zhang B, Li N, Jiang D, et al. Prognostic Factors to Determine Survivorship of Meniscal Allograft Transplant: A Systematic Review. Orthop J Sports Med. 2021;9:23259671211007216.
Lee B-S, Kim H-J, Lee C-R, Bin S-I, Lee D-H, Kim N-J, et al. Clinical Outcomes of Meniscal Allograft Transplantation With or Without Other Procedures: A Systematic Review and Meta-analysis. Am J Sports Med. 2018;46:3047–56.
Saltzman BM, Meyer MA, Leroux TS, Gilelis ME, Debot M, Yanke AB, et al. The Influence of Full-Thickness Chondral Defects on Outcomes Following Meniscal Allograft Transplantation: A Comparative Study. Arthroscopy. 2018;34:519–29.
Zaffagnini S, Romandini I, Filardo G, Dal Fabbro G, Grassi A. Meniscal allograft transplantation, anterior cruciate ligament reconstruction, and valgus high tibial osteotomy for meniscal-deficient, unstable, and varus knees: surgical technique and clinical outcomes. Int Orthop. 2023;47:2523–35.
Liu JN, Agarwalla A, Garcia GH, Christian DR, Gowd AK, Yanke AB, et al. Return to Sport and Work After High Tibial Osteotomy With Concomitant Medial Meniscal Allograft Transplant. Arthroscopy. 2019;35:3090–6.
Hurley ET, Davey MS, Jamal MS, Manjunath AK, Kingery MT, Alaia MJ, et al. High rate of return-to-play following meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2020;28:3561–8.
Cvetanovich GL, Christian DR, Garcia GH, Liu JN, Redondo ML, Yanke AB, et al. Return to Sport and Patient Satisfaction After Meniscal Allograft Transplantation. Arthroscopy. 2020;36:2456–63.
Allahabadi S, Quigley R, Frazier L, Joyce K, Cole BJ. Outcomes and Return to Sport After Knee Osteochondral Allograft Transplant in Professional Athletes. Orthop J Sports Med. 2024;12:23259671241226736.
Saltzman BM, Meyer MA, Weber AE, Poland SG, Yanke AB, Cole BJ. Prospective Clinical and Radiographic Outcomes After Concomitant Anterior Cruciate Ligament Reconstruction and Meniscal Allograft Transplantation at a Mean 5-Year Follow-up. Am J Sports Med. 2017;45:550–62.
Vundelinckx B, Vanlauwe J, Bellemans J. Long-term Subjective, Clinical, and Radiographic Outcome Evaluation of Meniscal Allograft Transplantation in the Knee. Am J Sports Med. 2014;42:1592–9.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502.
Author information
Authors and Affiliations
Contributions
A.P., E.H., and S.B. wrote the main manuscript text. All authors made substantial contributions to and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Boden reports other from Medtronic, personal fees from SeaSpine, other from Wolters Kluwer Health - Lippincott Williams & Wilkins, outside the submitted work. Dr. Yanke reports personal fees from Allosource, grants from Arthrex Inc., personal fees and other from JRF Ortho, grants from Organogenesis, other from Patient IQ, other from Sparta Biomedical, personal fees from Stryker, grants and other from Icarus Medical, outside the submitted work. Dr. Cole reports grants, personal fees and other from Arthrex Inc., personal fees from Elsevier Publishing, personal fees and other from Operative Techniques in Sports Medicine, other from Ossio, other from Bandgrip Inc., grants from Aesculap/B.Braun, other from JRF Ortho, grants from National Institutes of Health (NIAMS & NICHD), other from Smith & Nephew, outside the submitted work.
Disclosures
Andrew R Phillips BA and Erik C Haneberg BS declare no competing interests.
Stephanie A Boden MD has the following to disclose: Eastern Orthopedic Association: Board or committee member; Medtronic: IP royalties; SeaSpine: Paid consultant; Spine: Editorial or governing board; Wolters Kluwer Health—Lippincott Williams & Wilkins: Publishing royalties, financial or material support.
Adam B Yanke MD, PhD has the following to disclose: AlloSource: Paid consultant; Arthrex, Inc: Research support; Icarus Medical: Stock or stock Options; JRF Ortho: Paid consultant; Organogenesis: Research support; Patient IQ: Unpaid consultant; PatientIQ: Stock or stock Options; Sparta Biomedical: Stock or stock Options; Unpaid consultant; Stryker: Paid consultant; Paid presenter or speaker.
Brian J Cole MD, MBA has the following to disclose: Aesculap/B.Braun: Research support; American Journal of Sports Medicine: Editorial or governing board; Arthrex, Inc: IP royalties; Paid consultant; Research support; Arthroscopy Association of North America: Board or committee member; Bandgrip Inc: Stock or stock Options; Elsevier Publishing: IP royalties.
Journal of the American Academy of Orthopaedic Surgeons: Editorial or governing board; JRF Ortho: Other financial or material support; National Institutes of Health (NIAMS & NICHD): Research support; Operative Techniques in Sports Medicine: Publishing royalties, financial or material support; Ossio: Stock or stock Options.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Phillips, A.R., Haneberg, E.C., Boden, S.A. et al. Long-Term Clinical and Radiographic Outcomes of Meniscus Allograft Transplant. Curr Rev Musculoskelet Med 17, 343–352 (2024). https://doi.org/10.1007/s12178-024-09904-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-024-09904-z