Abstract
Blood samples collected from deceased tissue donors for mandatory transfusion microbiology testing may be taken either at the time of tissue donation, or residual samples may be retrieved from hospital laboratories where they were originally used for ante-mortem tests. In the latter case, sample labelling may not conform to the required standard, which stipulates that three independent identifiers be provided. If no alternative adequately labelled sample is available for testing the donated tissues may have to be discarded, which can adversely affect tissue sufficiency. An alternative method to ensure that the blood sample to be tested is from the intended deceased donor is to confirm the identity of the blood sample by Deoxyribonucleic Nucleic Acid (DNA) Short Tandem Repeats (STR) analysis, then comparing the DNA profile with the DNA from the donated tissues. If the two DNA profiles are identical, probability calculations can demonstrate the chance of the two samples of DNA being from the same or different individuals. The authors have used this approach to salvage deceased tissue donations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Deceased tissue donations provide valuable allografts for transplantation including bone, skin, tendons, corneas and heart valves. In the UK all donors are required to be tested according to the standards set out in the Department of Health Guidance document (MSBT 2000) as well as the Orange Guide (Rules and Guidance for Pharmaceutical Manufacturers and Distributors 2007). Compliance with guidance means that samples must be appropriately labelled. The specification for blood sample labelling in NHSBT Tissue Services is described in the UK Blood Services Guidance (Guidelines for the UK Blood Transfusion Services, 7th Edition, 2005). The regulatory environment is increasing in stringency with the Directive regarding human tissue and cells for human application (Directive 2004/23/EC) which, together with the daughter technical Directives (Commission Directive 2006/86/EC; Commission Directive 2006/17/EC), lays out statutory requirements for tissue and cell banking, including testing and labelling. When deceased donor blood samples are not available or are inappropriately labelled then tissue is lost; this can especially be the case when ante-mortem samples from deceased donors are obtained from diagnostic testing laboratories. These samples may be of a higher analyte quality than post-mortem samples with regard to haemolysis or inhibitors (Padley et al. 2005), but may be labelled with less than the three required donor identifiers, e.g. name, date of birth and hospital number. Despite Guidelines from the British Committee for Standards in Haematology (BSH Guidelines 2004) and other standards (EFI 2003; ISCT and EBMT (JACIE) 2002) we find that temporary serum archives from hospital chemical pathology or haematology or other testing laboratories may only be stored with two identifiers. An alternative means of identifying these samples to meet the requirements of the Directive 2006/17/EC is needed to avoid loss of tissue which may otherwise meet requirements.
In 1985 Jeffreys and co-workers described the technique of DNA ‘fingerprinting’ or ‘profiling’ (Jeffreys et al. 1985). Their technique was based on the fact that many non-coding portions of genes (introns) contain stretches of DNA of varying lengths made up of particular repeated sequences of base pairs. There are two types of these repeating sequences of DNA, longer ones called Variable Number Tandem Repeats (VNTRs) and very short ones called Short Tandem Repeats (STRs). The early work on DNA profiling was done using VNTR analysis. Currently, DNA profiling is most commonly performed by STR analysis.
STRs (or microsatellites) differ from VNTRs (minisatellites) in having smaller repeat units and the total size of an STR is also smaller. STRs consist of tandem repeats of a basic sequence motif of 2–5 nucleotides that are repeated variable numbers of times. For example, the 16 bp sequence “gatagatagatagata” would represent four copies of the tetramer “gata”. The small size of STRs means that the polymerase chain reaction (PCR) can be used to amplify very small amounts (less than 1 ng) of DNA. It also permits analysis of partially degraded DNA that has been broken into short pieces. STRs exhibit size polymorphisms because of the different number of copies of the repeat element that occur in different individuals. There are many thousands of STR loci throughout the genome. The more loci that are investigated, the less chance that two unrelated individuals will have the same STR analysis profile. DNA profiling techniques are used to determine whether DNA samples are likely to come from the same person, related people or non-related people and are used in forensic investigations and in disputed paternity testing (Butler 2006). STR analysis is used within the NHS Blood and Transplant (NHSBT) to confirm the identity of cord blood stem cell units and their link to the mother’s sample and the relevant medical history prior to issue for clinical transplantation (Armitage et al. 1999; Davey et al. 2004)
Materials and methods
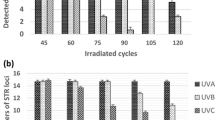
In a pilot study, we investigated the applicability of STR analysis for sample and donor identity confirmation on blood and bone marrow (extracted from the long bones donated as bone graft for transplant) samples from five deceased tissue donors. The blood or bone marrow sample taken by the staff performing the tissue procurement (therefore meeting the identification requirements) was obtained up to a maximum of 48 h post-mortem. The type of sample obtained for identity matching depended on the type of donor. Where the donor was a multi-organ donor or where a post-mortem examination had been undertaken, the sample was usually bone marrow rather than blood because in these circumstances it can be to difficult to obtain an adequate sample of blood. As detailed in Table 4, the STR analysis would also confirmed the sex of the donor thereby providing another identifier for the primary sample. DNA was extracted from the blood and bone marrow samples of each donor using a modified salting out technique for the blood and a commercial DNA extraction (Tepnel—USA) for the bone marrow. Polymerase chain reaction (PCR) was carried out using primers for 1 sex linked and 6 autosomal STR loci to amplify the DNA. The STR loci and their chromosomal location are shown in Table 1.
The PCR products were analysed using a 3,100 automated genetic analyser (ABI Warrington, UK) and the STR profiles for the blood and marrow samples were compared for identity. Probability calculations were used to estimate the chances of the two samples belonging to different individuals using published frequencies (www.promega.com).
The probability calculations are based on the allele frequencies for each STR locus for a representative human population. Allele frequency is defined as the number of copies of the allele in a population divided by the total number of all alleles in a population.
If two alleles at one locus have frequencies of p and q in a population, the probability (P) of an individual having both alleles at that locus is given by the equation:
The probability (P) of an individual being homozygous for an allele with a frequency of p is given by the equation P = p2.
For this study STRs at seven loci on different chromosomes were used. The alleles at the seven different loci are inherited independently. Therefore, the probability for the combined genotype can be determined by multiplying the individual probabilities. The probability (P) for a DNA profile is the product of the probability (P 1, P 2 ... P n) for each individual locus, i.e.
The probability can be extremely small when all seven STR markers are included in the DNA profile. Table 2 shows the allele frequencies at two STR loci used in this study.
Example: If a person has the following genotype:
-
VWA31; 17,19
-
TH01; 6,9
-
The expected frequency of ‘17,19’ = 2pq = 2(0.283 × 0.092) = 0.0521
-
The expected frequency of ‘6,9’ = 2pq = 2(0.205 × 0.14) = 0.0574
-
The chance of observing these genotypes in an individual = 0.0521 × 0.0574 = 0.002989 or 1:335
When all seven loci (six autosomal and one x/y locus) are considered, the probability of two individuals having the same STR profile ranges between 1 and 100 million to one.
Results
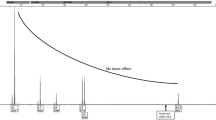
In this pilot study, DNA was successfully obtained from all of the five donors’ blood and bone marrow samples. All DNA samples were successfully amplified by PCR. There was 100% concordance between the STR profiles of the paired blood and bone marrow samples from each donor. One female and four male donors were correctly identified. An example of an STR readout is shown in Fig. 1.
Subsequent to validating this methodology, STR analysis has been used to confirm the identity of 11 inadequately labelled blood samples, or from surplus blood samples frozen as an archive from deceased tissue donors, by showing STR matching between surplus blood samples retrieved from hospital laboratories and either bone marrow taken from donated bone or a second blood sample not suitable for serological investigation taken during donation (Tables 3, 4).
The process of STR matching has been undertaken on 11 deceased tissue donors (Table 4) where the blood sample provided by a Hospital laboratory was only labelled with two identifiers. Matching for STR profiles has been used as a third point of identification between the blood sample and the donor’s bone marrow taken from a donated bone. The primary sample provided by the Hospital laboratory for mandatory microbiological markers was sampled up to a maximum of 24 h post-mortem, in keeping with the Guidelines for the UK Blood Transfusion Services.
Discussion
There are two steps involved in identity confirmation using STR analysis. The first step is the laboratory demonstration that STR profiles of sample from correctly labelled and inadequately labelled samples are identical. The second step requires application of statistical methodology to estimate the chance of two DNA samples, having the same STR profile, originating from two different individuals. In the cases used for the pilot study we were able to confirm that the blood samples were indeed most likely to have come from the presumptive donor with odds of up to 1:1 × 1014. The technique has since been applied to 11 cases of donor samples with inadequate labelling and STR confirmation ensured that the microbiological test results were indeed pertinent to the donor. This prevented the need to discard valuable tissue. The cost of these molecular techniques is significant and therefore we do not advocate the routine application of STR methodology to all deceased donor samples. However salvaging donations which would otherwise be discarded is clearly beneficial. This is especially so in the case of a deceased multi-tissue donor. In such cases the cost of the methodology in our service, (50% more than all the microbiology markers together—Hepatitis B anti-core and HBsAg, HTLV 1/2 antibody, HCV antibody, Syphilis Tp specific, HIV antigen and antibody and HCV and HCV RNA) is small in comparison with the disadvantage of losing large amounts of life saving and life enhancing donated tissues, wasting altruistic donations from a deceased donor, distressing their families and jeopardising tissue sufficiency. The technique is applicable whenever blood sample and donor identity require reconciliation and provides an aide to improving tissue sufficiency.
References
Armitage S, Warwick RM, Fehily D, Navarrete C, Contreras M (1999) Cord Blood Banking in London: the first 1000 collections. Bone Marrow Transplant 24(2):139–145
Butler JM (2006) Genetics and genomics of core short tandem repeat loci used in human identity testing. J Forensic Sci 51:253–265
British Committee for Standards in Haematology (BCSH) (2004) Guidelines for compatibility procedures in blood transfusion laboratories. Transfus Med 14:59–73
Commission Directive 2006/17/EC of 8 February 2006 implementing Directive 2004/23/EC of the European Parliament and of the Council as regards certain technical requirements for the donation, procurement and testing of human tissues and cells. Off J Eur Union L 38/40, 09/02/2006
Commission Directive 2006/86/EC of 24 October 2006 implementing Directive 2004/23/EC of the European Parliament and of the Council as regards traceability requirements, notification of serious adverse reactions and events, and certain technical requirements for the coding, processing, preservation, storage and distribution of human tissues and cells. Off J Eur Union L 294/32, 25/10/2006
Davey S, Armitage S, Rocha V, Garnier F, Brown J, Brown CJ, Warwick RM, Gluckman E, Contreras M, Navarrete CV (2004) the London Cord Blood experience—banking and transplantation outcome. Br J Haematol 125:358–365
Directive 2004/23/EC of the European Communities and of the Council of 31 March 2004 (2004) Setting standards of quality and safety for the donation, procurement, testing, processing, preservation, storage and distribution of human tissues and cells. Official J Eur Union. http://www.europa.eu.int/eur-lex/pri/en/oj/dat/2004/l_102/l_10220040407en00480058.pdf
European Federation for Immunogenetics (EFI) (2003) Standards for histocompatibility testing, version 5.3 approved by the Standards and Quality Assurance Committee 30th Jan 2003. www.efiweb.org
Guidelines for tissue banking in guidelines for blood transfusion services in the United Kingdom, 7th Edition (2005). The Stationary Office, London. Available at http://www.transfusionguidelines.org.uk
Jeffreys AJ, Wilson V, Thein SL (1985) Individual-specific “fingerprints” of human DNA. Nature 316:76–79
Joint Accreditation Committee of ISCT and EBMT (JACIE) (2002) Standards for haemopoietic progenitor cell collection processing and transplantation—Europe, March 2002. http://www.ebmt.org/8TransplantGuidelines/tguide3.html
MSBT Committee on Microbiological Safety of Blood and Tissues for Transplantation, Department of Health (2000) Guidance on the microbiological safety of human tissues and organs used in transplantation. NHS Executive
Orange Guide (2007) Rules and guidance for pharmaceutical manufacturers and distributors. ISBN/ISSN 9-78-085369719-0
Padley D, Ferguson M, Warwick RM, Womack C, Lucas SB, Saldanha J (2005) Challenges in the testing of non-heart beating cadavers for viral markers: implications for the safety of tissue donors. Cell Tissue Bank 6(3):171–179
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Warwick, R.M., Rushambuza, F.G., Brown, J. et al. Confirmation of cadaveric blood sample identity by DNA profiling using Short Tandem Repeat (STR) analysis. Cell Tissue Bank 9, 323–328 (2008). https://doi.org/10.1007/s10561-008-9071-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-008-9071-6