Abstract
Lysophosphatidic acid (LPA; monoacyl-glycerol-3-phosphate) is a lipid mediator that functions as a mitogen and motility factor for many cell types. LPA signals through six specific G protein-coupled receptors, named LPA1–6, which trigger both overlapping and distinct signaling pathways. LPA is produced from extracellular lysophosphatidylcholine by a secreted lysophospholipase D, named autotaxin (ATX), originally identified as an “autocrine motility factor” for tumor cells. ATX–LPA signaling is vital for embryonic development and promotes tumor formation, angiogenesis, and experimental metastasis in mice. Elevated expression of ATX and/or aberrant expression of LPA receptors are found in several human malignancies, while loss of LPA6 function has been implicated in bladder cancer. In this review, we summarize our present understanding of ATX and LPA receptor signaling in cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
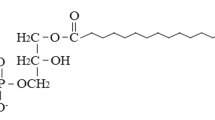
The impact of the tumor microenvironment on tumor progression is mediated, in large part, by growth factors, motility factors, and proangiogenic factors that are produced by the tumor cells themselves as well as the surrounding stroma. One such factor is lysophosphatidic acid (LPA; monoacyl-glycerol-3-phosphate), a multifunctional lipid mediator best known for its ability to stimulate proliferation, migration, and survival of many cell types, both normal and malignant. However, the list of biological responses to LPA is quite diverse, as it ranges from growth factor-like activities to neurite remodeling and modulation of ion channel activity [1, 2]. Bioactive LPA is produced extracellularly from lysophosphatidylcholine (an abundant plasma lipid) by a secreted lysophopholipase D (lysoPLD) [3, 4], known as autotaxin (ATX), named after its first discovered activity as an “autocrine motility factor” for melanoma cells [5]. LPA acts through six known G protein-coupled receptors (GPCRs), termed LPA1–6, which are differentially expressed and show both overlapping and distinct signaling properties [1, 6]. A schematic representation of the ATX–LPA receptor signaling axis is shown in Fig. 1.
Autotaxin–LPA receptor signaling. Autotaxin is a secreted lysophospholipase D that hydrolyzes extracellular lysophosphatidylcholine (an abundant plasma phospholipid) into bioactive LPA. LPA acts through specific G protein-coupled receptors and stimulates cell proliferation, migration, and survival. ATX is a multidomain enzyme; the colors refer to the specific domains (for structural details, see references [24, 25])
Increasing evidence points to an important role for ATX and LPA receptor signaling in cancer [7], as will be discussed below. In brief, (1) elevated or aberrant expression of ATX and LPA receptors is found in several human malignancies; (2) overexpression of ATX or individual LPA receptors promotes tumor formation and metastasis in mouse models, whereas knockdown has the opposite effect; and (3) LPA2 knockout mice show reduced colon carcinogenesis. Moreover, loss of function of LPA6 has been implicated in bladder cancer development, suggesting that LPA6 is a candidate tumor suppressor. In this review, we summarize the evidence for a role of ATX–LPA signaling in cancer and also discuss recent developments in targeting ATX by pharmacological inhibitors.
2 LPA receptor signaling
LPA receptors can be divided in two subfamilies. The classical LPA1–3 receptors belong to the so-called endothelial differentiation gene (Edg) family, whereas three additional LPA receptors (LPA4–6) are more closely related to the purinergic receptor family [1, 6]. Depending on receptor subtype, LPA stimulation results in (1) activation of the mitogenic Gαi-linked Ras-Raf-MEK-ERK pathway [8, 9]; (2) Gαi-mediated activation of phosphoinositide 3-kinase-beta [10], which promotes cell survival and many other cellular functions; (3) cytoskeletal remodeling, cell migration and invasion via the Gα12/13-linked RhoA pathway acting in concert with the Gαi-mediated Rac activation pathway [11–13]; and (4) Gαq-linked activation of phospholipase C with consequent production of second messengers [14, 15]. In addition, LPA stimulation often leads to changes in cAMP levels via either Gαi or G(βγ) subunits (for review, see [1, 2]). LPA stimulation also promotes the production of growth factors and cytokines via multiple pathways [16]. For a given LPA receptor, the net outcome of these synergizing signaling pathways strongly depends on cellular context. For example, depending on the cell system used, LPA4 receptor signaling may either enhance [17] or inhibit [18] tumor cell migration and invasiveness.
3 LPA production by autotaxin, a secreted lysoPLD
LPA is produced by autotaxin (ATX or ENPP2), a member of the ectonucleotide pyrophosphatase/phosphodiesterase (ENPP) family. The ENPP family consists of seven structurally related ectoenzymes that hydrolyze pyrophosphate and phosphodiester bonds in nucleotides and their derivatives [19]. ATX hydrolyzes LPC into LPA (plus free choline) and is the only lysoPLD in the ENPP family. ATX is synthesized as a preproenzyme, processed by a furin-type protease and secreted along the classical secretory route as a glycosylated protein into the extracellular milieu (reviewed in [20]). ATX is widely expressed and present in plasma. The origin of plasma ATX remains to be determined, but likely sources are the lymphatic high endothelial venules [21] and adipose tissue, which express and secrete ATX at high levels. Indeed, adipose-specific deletion of Enpp2 leads to reduced plasma LPA levels [22].
ATX is a multidomain protein consisting of two N-terminal somatomedin B (SMB)-like domains, a central catalytic phosphodiesterase domain, and an N-terminal nuclease-like domain [19, 20]. Although ATX is capable of hydrolyzing nucleotides in vitro, the apparent affinity of ATX for LPC is some 10-fold higher than for nucleotides [23] and, furthermore, extracellular nucleotide levels are normally very low. Therefore, all biological effects of ATX are thought to be attributable to LPA production and subsequent receptor stimulation [20]. Formally, however, additional noncatalytic functions of ATX cannot be excluded at present. Recent structural studies [24, 25] have revealed how the different domains of ATX are organized and interact (Fig. 1) and shed light on what makes ATX a unique lysoPLD, namely a deep hydrophobic lipid-binding pocket in the catalytic domain. The ATX structure further suggests that the SMB domains could be involved in regulating catalytic activity [25].
3.1 ATX interaction with the cell surface
To ensure efficient delivery of LPA to its receptors, ATX must communicate with target cells in a locally restricted manner. One mechanism by which ATX interacts with target cells is via integrins. ATX binds to activated lymphocytes via α4β1 integrins [21] and to activated platelets via integrin β3 [26]. The SMB domains of ATX appear to be the primary mediators of integrin β3 binding [25]. Injection of enzymatically inactive (“dominant negative”) ATX in mice attenuates the homing of T cells to secondary lymphoid organs, presumably by competing with endogenous ATX for binding to integrins [21]. Since ATX is abundantly expressed in lymphatic high endothelial venules (HEVs), this suggests a model in which secretion of ATX by HEVs promotes the entry of lymphocytes into lymphoid organs. In this model, ATX is secreted into the lumen of HEVs and binds to adherent lymphocytes through activated integrins. Subsequently, the lymphocyte-bound ATX may produce a high local concentration of LPA to activate LPA receptors on the lymphocytes and promote their transendothelial migration [21]. In support of this scenario, LPA induces invasion of T lymphoma cells across a monolayer of normal fibroblasts [12]. Thus, ATX/LPA could use a similar strategy to stimulate the extravasation of circulating tumor cells, a hallmark of the metastatic cascade.
Since ATX is a heparin-binding protein (as it can be purified using heparin affinity chromatography), binding to heparan sulfate proteoglycans (HSPs) on the cell surface could be an alternative or additional way by which ATX ensures local delivery of LPA to its cognate receptors. Thus, diverse scenarios for localized LPA production and signaling can be envisioned in which ATX is recruited to target cells via specific cell surface molecules such as integrins and HSPs.
4 ATX and LPA receptors in embryonic development
Gene targeting studies in mice have revealed a vital role for ATX during embryogenesis, as Enpp2 knockout causes embryonic lethality at midgestation (around E9.5) due to severe vascular defects in both yolk sac and the embryo proper [27, 28]. The vascular network normally present in the yolk sac is completely absent and replaced by blood patches, while blood vessels in the embryo are enlarged; furthermore, the neural tube is malformed [27, 29]. Heterozygous Enpp2(+/−) mice show half-normal plasma LPA levels, consistent with ATX being the major LPA-producing enzyme in the circulation. The phenotype of Enpp2-knockout mice is strongly reminiscent of that of the Gα13 knockout, suggesting that the observed defects in ATX-null embryos can be explained by loss of migratory G13-RhoA signaling through multiple LPA receptors [27, 30].
The phenotype of individual LPA receptor knockouts is much less severe than that of the Enpp2 knockout. Thus far, LPA receptor-knockout studies in mice have uncovered normal physiological roles for LPA signaling in such diverse processes as neurogenesis [31] and bone formation [32] (LPA1), embryo implantation (LPA3) [33], and formation of blood and lymphatic vessels (LPA4) [34]. Lpa 2 -knockout mice show no abnormalities [35], while the LPA5- and LPA6-deficient phenotypes remain to be described.
5 ATX–LPA receptor signaling in cancer
Since the discovery of ATX as an autocrine motility factor for melanoma cells, many subsequent studies have implicated a role for ATX–LPA signaling in tumor formation and metastasis.
5.1 Studies in vitro
High expression of ATX is found in a number of tumor cell types, including neuroblastoma [36], hepatocellular carcinoma [37], breast cancer [38], renal cell carcinoma [39], glioblastoma [40], non-small cell lung cancer (NSCLC) [41], B cell lymphomas [42, 43], and thyroid carcinoma [44]. Expression of ATX is found both in the tumor core as well as in the invasive cells of glioblastomas [40], and in NSCLC, the highest expression is detected in poorly differentiated tumors [41]. This argues that ATX is able to augment cellular characteristics necessary for tumor aggressiveness.
ATX expression is regulated by various growth factors, cytokines, and (proto-)oncogenes, which will differ per cell type and thus cause diverse outcomes. For example, EGF, bFGF, TGFβ, and other factors induce up- or downregulation of ATX mRNA depending on cell type [44, 45]. v-Jun-transformed fibroblasts show strongly upregulated ATX expression [46], while ATX is upregulated in Wilms’ tumors harboring oncogenic β-catenin mutations [47] and in mammary epithelial cells stimulated by Wnt-1 [48]. Downregulation of ATX is observed following retinoic acid treatment of Wilms’ tumor cells and N-Myc-overexpressing neuroblastoma cells [49, 50].
In Hodgkin lymphoma cells, Epstein–Barr virus infection leads to strong induction of ATX expression, with subsequent generation of LPA and enhanced cell growth and survival [42]. Specific downregulation of ATX decreased LPA levels and reduced cell growth and viability in these cells. Furthermore, ATX expression is strongly induced upon forced expression of integrin α6β4 in MDA-MB-435 tumor cells, an effect mediated by the transcription factor NFAT1 [51]. This provides a possible explanation for the stimulatory effect of integrin α6β4 on tumor cell migration and invasion.
5.2 Insights from mouse studies
5.2.1 Xenograft models
The first evidence for a tumorigenic role of ATX in vivo came from studies using ATX-overexpressing, Ras-transformed NIH3T3 cells. ATX overexpression resulted in increased tumor growth, aggressiveness, and angiogenesis, whereas the inactive mutant ATX(T210A) did not [45, 52].
Subsequent studies have shown a role for both ATX and LPA receptor signaling in tumor progression and metastasis. LPA1 overexpression in MDA-MB-231 breast cancer cells promotes increased skeletal tumor growth and tumor-induced bone destruction in xenografted mice. The tumor cells do not express ATX, but they stimulate the production of LPA by activated platelets, thereby promoting tumor cell proliferation and cytokine-mediated bone destruction [53]. Silencing or pharmacological inhibition of LPA1 reduced both tumor growth and bone metastasis progression [54]. Furthermore, ATX overexpression in mammary carcinoma cells promotes metastasis to bone, while silencing of endogenous ATX expression inhibited metastasis, with little effect on primary tumor growth [55].
Forced overexpression of LPA1, LPA2, or LPA3 in ovarian cancer cells enhances tumor growth in nude mice, showing increased growth factor production, ascites formation, and organ invasion [56]. In another study, overexpressed LPA1, LPA2, and LPA4 were found to collaborate with c-Myc and Tbx2 (a transcriptional repressor of p19Arf) to transform mouse embryo fibroblasts (MEFs) both in vitro and in xenografts [57]. In this case, LPA-mediated cell transformation is mediated by the Gi-linked MAPK and PI3K pathways. Overexpression of individual LPA receptors in naïve MEFs had no transforming effect, indicating that LPA signaling needs to collaborate with other pro-oncogenic events to induce cell transformation [57].
5.2.2 Genetic models
Unfortunately, the embryonic lethality of ATX-deficient mice has hampered studies on the importance of ATX in cancer progression. However, important insights have been gained form studies in transgenic and LPA receptor-knockout mice. MMTV-driven overexpression of ATX or individual LPA receptors (LPA1–3) in mouse mammary gland leads to late-onset invasive and metastatic mammary carcinomas and cancer-associated inflammation [58]. The transgene expression influenced several signaling pathways, including PI3K-Akt and MAPK pathways, as well as Wnt pathway components and E-cadherin. The ATX and LPA receptor-driven tumors do not form a distinct cluster, as would be expected due to the fact that each of the receptors links to particular pathways and functional outcomes [58]. This reinforces the notion that transgenic overexpression of ATX and LPA receptors allows accumulation of secondary mutations leading to mammary cancers, possibly by increasing cell viability upon LPA signaling and thus increasing the likelihood of acquiring (pro-)oncogenic mutations.
Of the known LPA receptors, LPA2 has been implicated in intestinal cancer [59]. In a model of chemically induced colon carcinogenesis, LPA2-knockout mice (which show a wild-type phenotype) display a remarkably reduced tumor incidence and progression. This is accompanied by a decrease in both cell proliferation and chemokine expression, in particular the proinflammatory factors MCP-1 and MIF which are associated with colorectal cancer. Reduced colon tumorigenesis in the LPA2-null animals correlated with reduced infiltration by macrophages [59], a predominant stromal cell type known to contribute to tumor progression. Furthermore, LPA treatment increased tumor incidence in APCmin/+ mice, a model for spontaneous intestinal cancer [59]. Conversely, loss of LPA2 dramatically reduced tumor incidence in APCmin/+ mice, accompanied by reduced expression levels of cell cycle regulators such as KLF5, c-Myc, and cyclin D1 [60]. These studies show that LPA2, in combination with loss of the tumor suppressor APC, is capable of promoting tumorigenesis in the colon. It thus appears that, again, LPA signaling increases the susceptibility to accelerate cancer progression when other genetic factors are present. The results from the various in vivo studies are summarized in Table 1.
6 Clinical implications
To what extent do the findings obtained in mouse models bear relevance to the human disease? Cancer-specific gain-of-function mutations in ATX or LPA receptors have not been reported to date; in contrast, loss of function mutations have been reported for LPA6 in bladder cancer (see below). Analysis of multiple microarray datasets (www.oncomine.org) reveals strongly elevated ATX expression in certain human cancers, especially B cell lymphomas, renal carcinoma, liver cancer, and pancreatic cancer. Also, individual LPA receptors are found overexpressed in several cancers when compared to the corresponding normal tissues (www.oncomine.org, see also [7]).
In follicular lymphoma, serum ATX levels correlate with tumor burden and clinical course, suggesting that ATX may serve as a biomarker in follicular lymphoma [43]. Furthermore, an increase in serum ATX activity has been reported in pancreatic cancer patients [61] and ENPP2 is one of the genes in a 64-gene signature that predicts poor survival of patients with stage I NSCLC [62]. As a word of caution, it should be realized that high ATX expression by itself does not necessarily imply elevated LPA levels and enhanced receptor signaling, since substrate (LPC) availability and LPA degradation by cell-associated lipid phosphate phosphatases are additional determinants of bioactive LPA levels in the cellular microenvironment [20]. Ultimately, it is the LPA receptor expression profile on both the tumor and surrounding stromal cells that will determine the outcome of enhanced ATX expression. One area of future research is to establish to what extent aberrant ATX and/or LPA receptor expression patterns are associated with clinical outcome.
6.1 LPA6: a candidate tumor suppressor in bladder cancer
The LPA6 receptor, previously known as orphan receptor P2Y5 (or 6H1), deserves special mention because it has been associated with familial bladder cancer [63] as well as genetic hair growth abnormalities [64]. LPA6/P2Y5 is known to couple to the Gα13-RhoA signaling pathway, which regulates the actin cytoskeleton, but it does not mediate changes in cytosolic calcium or cAMP [65]. P2RY5 is an inducible gene: its expression is rapidly induced upon T cell activation [66] and in LPA-stimulated fibroblasts [16].
The LPA6-encoding gene, P2RY5, is located inside the retinoblastoma tumor suppressor gene RB1 (intron 17) in the reverse orientation. In bladder cancer, a segment around RB1 is characterized by a loss of polymorphism associated with the initial expansion of neoplasia [63, 67]. This segment contains several so-called forerunner genes that may contribute to such expansion, and P2RY5 is one of these genes. Homozygous mutational inactivation of P2RY5 precedes the loss of RB during tumor development, while nucleotide substitutions in P2RY5 represent a cancer-predisposing factor, particularly in combination with tobacco smoking [63, 67]. Reintroduction of P2RY5 into bladder cancer cells that lacked it resulted in cell cycle arrest and apoptosis, consistent with P2RY5 being a candidate tumor suppressor. One family with an inherited risk of cancer, including breast, colon, lung, prostate, and uterus, carried a germline mutation in P2RY5. The most frequent polymorphism results in a W307C mutation in the LPA6 cytoplasmic tail. This could affect LPA6 interaction with G proteins [63, 67] and hence compromise LPA signaling, but this needs to be tested. Interestingly, a single nucleotide polymorphism within the same genomic locus that is predicted to downregulate P2RY5 expression is a potential risk factor for developing invasive ovarian cancer [68].
Loss of P2RY5 function has also been implicated in genetic hair growth disorders [64]. LPA6/P2Y5 is detected in the inner root sheath of hair follicles. However, human hair follicles do not express ATX but, instead, an LPA-producing phospholipase A1 encoded by LIPH [69]; mutations in LIPH induce the same abnormal hair growth phenotype as mutations in LPA6. This raises the question of whether LPA6 in other tissues, such as bladder epithelium, is normally stimulated via ATX- or LIPH-mediated LPA production. Given the very restricted tissue distribution of LIPH, however, ATX is the more attractive candidate.
In conclusion, LPA 6 /P2RY5 provides a new paradigm for cancer development and may represent an early detection and risk marker in bladder cancer [70]. It is now important that the biological function and signaling properties of LPA6 and its mutant versions be elucidated in further detail.
7 ATX as a drug target
As a secreted phosphodiesterase, ATX is an attractive and easily “druggable” therapeutic target. Several ATX inhibitors have been based on the seminal finding that LPA and sphingosine 1-phosphate (S1P) inhibits ATX activity against nucleotides and artificial substrates (Ki about 100 nM) [23]. Several LPA analogs have been described as ATX inhibitors, some with an effect on melanoma cell metastasis [71, 72] and breast tumor growth in mice [73]. Yet, the potency of LPA analogs is rather low (and even very poor when tested in ATX-mediated LPC hydrolysis assays), and it is not clear whether the reported in vivo effects are attributable to ATX inhibition. Most LPA-based ATX inhibitors lack an in vivo pharmacodynamic proof of principle in that they have not been shown to lower circulating LPA levels. Furthermore, there are concerns about their potential agonistic effect on LPA receptors. FTY720, a structural analog of sphingosine, is an immunomodulator for patients with relapsing multiple sclerosis. The active form, FTY720-phosphate (FTY-P) is an S1P mimetic and acts on S1P receptors with high potency. At higher concentrations, FTY-P (like S1P) is a competitive inhibitor of ATX and reduces plasma LPA levels when injected into mice [74]. It remains to be seen, however, whether ATX inhibition underlies the reported anticancer effects of high doses FTY720 [74]. Lipid phosphonate analogs that inhibit ATX activity against artificial substrates show a reducing effect on plasma LPA levels and B16 melanoma metastasis; however, their potency is relatively low [75].
Nonlipid, small-molecule inhibitors clearly hold more promise. High-throughput screening identified thiazolidinedione-based compounds as a new class of ATX inhibitors [76]. Their potency is increased dramatically by introduction of a boronic acid moiety, designed to target the catalytic Thr residue in ATX. The most potent analogs show IC50 values <10 nM in LPC hydrolysis assays [76, 77]. Injection of these compounds into mice results in a rapid fall in circulating LPA levels, consistent with LPA being rapidly produced and degraded in vivo. The crystal structure of the ATX in complex with a boronic acid inhibitor reveals that it forms a reversible covalent bond with the Thr210 nucleophile in the hydrophobic lipid-binding pocket of ATX [25]. Another small-molecule inhibitor of ATX, PF-8380, shows adequate oral bioavailability and in vivo potency in reducing LPA levels in plasma and at sites of inflammation [78], indicating that ATX is a major source of LPA during inflammation. Furthermore, a close pharmacokinetic/pharmacodynamic relationship was observed. Compounds like PF-8380 can serve as useful tools for elucidating the role of ATX in tumor progression in mice.
8 Concluding remarks
Given its mitogenic and chemotactic properties, together with the wide distribution of LPA receptors, it is not surprising that LPA, when produced in the tumor–stroma microenvironment, can enhance cancer progression. Although the clinical consequences of enhanced or aberrant LPA production and signaling remain to be determined, studies in mice have provided strong evidence that the ATX–LPA receptor signaling axis contributes to tumor formation, angiogenesis, and metastasis. The in vivo studies also indicate that distinct oncogenic events, such as H-Ras or c-Myc activation, must collaborate with LPA signaling to promote tumor progression. The LPA2 receptor provides perhaps the strongest case for a link between LPA signaling and cancer, since Lpa 2 -knockout mice show a marked decrease in colon tumor incidence. Additional evidence is provided by the study on transgenic overexpression of ATX and LPA receptors in mouse mammary gland. To more broadly assess the importance of LPA signaling in tumor maintenance and progression, a logical approach would be to crossbreed LPA receptor-null mice with genetically engineered mouse tumor models, in which cancer is initiated by Cre-recombinase-mediated activation of oncogenic mutations in specific tissues.
The LPA6 receptor represents an interesting case, since it may function as a tumor suppressor in familial bladder cancer and loss of function mutations have been detected in patients; nucleotide substitutions in the LPA6-encoding gene (P2RY5) are considered a cancer-predisposing factor. Obviously, these intriguing findings require further validation and investigation. Lpa 6 -knockout mice will provide a powerful tool to examine the suspected tumor-suppressing function of LPA6.
Hopefully, the knowledge on ATX–LPA signaling gleaned in academic labs can now be applied toward the development of new drugs for cancer treatment in the foreseeable future. That ATX is an extracellular enzyme and GPCRs, such as those for LPA, are highly druggable will add to their attractiveness as targets. Potent small-molecule inhibitors that target ATX in vivo have already been described. Now that the crystal structure of ATX has been determined, drug development efforts will undoubtedly get a further boost.
References
Choi, J. W., Herr, D. R., Noguchi, K., Yung, Y. C., Lee, C. W., Mutoh, T., et al. (2010). LPA receptors: subtypes and biological actions. Annual Review of Pharmacology and Toxicology, 50, 157–186.
Moolenaar, W. H., van Meeteren, L. A., & Giepmans, B. N. (2004). The ins and outs of lysophosphatidic acid signaling. Bioessays, 26, 870–881.
Tokumura, A., Majima, E., Kariya, Y., Tominaga, K., Kogure, K., Yasuda, K., et al. (2002). Identification of human plasma lysophospholipase D, a lysophosphatidic acid-producing enzyme, as autotaxin, a multifunctional phosphodiesterase. Journal of Biological Chemistry, 277, 39436–39442.
Umezu-Goto, M., Kishi, Y., Taira, A., Hama, K., Dohmae, N., Takio, K., et al. (2002). Autotaxin has lysophospholipase D activity leading to tumor cell growth and motility by lysophosphatidic acid production. The Journal of Cell Biology, 158, 227–233.
Stracke, M. L., Krutzsch, H. C., Unsworth, E. J., Arestad, A., Cioce, V., Schiffmann, E., et al. (1992). Identification, purification, and partial sequence analysis of autotaxin, a novel motility-stimulating protein. Journal of Biological Chemistry, 267, 2524–2529.
Chun, J., Hla, T., Lynch, K. R., Spiegel, S., & Moolenaar, W. H. (2010). International Union of Basic and Clinical Pharmacology. LXXVIII. Lysophospholipid receptor nomenclature. Pharmacological Reviews, 62, 579–587.
Mills, G. B., & Moolenaar, W. H. (2003). The emerging role of LPA in cancer. Nature Reviews Cancer, 3, 582–591.
van Corven, E. J., Hordijk, P. L., Medema, R. H., Bos, J. L., & Moolenaar, W. H. (1993). Pertussis toxin-sensitive activation of p21ras by G protein-coupled receptor agonists in fibroblasts. Proceedings of the National Academy of Sciences of the United States of America, 90, 1257–1261.
Kranenburg, O., & Moolenaar, W. H. (2001). Ras-MAP kinase signaling by lysophosphatidic acid and other G protein-coupled receptor agonists. Oncogene, 20, 1540–1546.
Guillermet-Guibert, J., Bjorklof, K., Salpekar, A., Gonella, C., Ramadani, F., Bilancio, A., et al. (2008). The p110beta isoform of phosphoinositide 3-kinase signals downstream of G protein-coupled receptors and is functionally redundant with p110gamma. Proceedings of the National Academy of Sciences of the United States of America, 105, 8292–8297.
Kranenburg, O., Poland, M., van Horck, F. P., Drechsel, D., Hall, A., & Moolenaar, W. H. (1999). Activation of RhoA by lysophosphatidic acid and Galpha12/13 subunits in neuronal cells: induction of neurite retraction. Molecular Biology of the Cell, 10, 1851–1857.
Stam, J. C., Michiels, F., van der Kammen, R. A., Moolenaar, W. H., & Collard, J. G. (1998). Invasion of T-lymphoma cells: cooperation between Rho family GTPases and lysophospholipid receptor signaling. EMBO Journal, 17, 4066–4074.
van Leeuwen, F. N., Olivo, C., Grivell, S., Giepmans, B. N., Collard, J. G., & Moolenaar, W. H. (2003). Rac activation by lysophosphatidic acid LPA1 receptors through the guanine nucleotide exchange factor Tiam1. Journal of Biological Chemistry, 278, 400–406.
van Corven, E. J., Groenink, A., Jalink, K., Eichholtz, T., & Moolenaar, W. H. (1989). Lysophosphatidate-induced cell proliferation: identification and dissection of signaling pathways mediated by G proteins. Cell, 59, 45–54.
Jalink, K., van Corven, E. J., & Moolenaar, W. H. (1990). Lysophosphatidic acid, but not phosphatidic acid, is a potent Ca2(+)-mobilizing stimulus for fibroblasts. Evidence for an extracellular site of action. Journal of Biological Chemistry, 265, 12232–12239.
Stortelers, C., Kerkhoven, R., & Moolenaar, W. H. (2008). Multiple actions of lysophosphatidic acid on fibroblasts revealed by transcriptional profiling. BMC Genomics, 9, 387.
Harper, K., Arsenault, D., Boulay-Jean, S., Lauzier, A., Lucien, F., & Dubois, C. M. (2010). Autotaxin promotes cancer invasion via the lysophosphatidic acid receptor 4: participation of the cyclic AMP/EPAC/Rac1 signaling pathway in invadopodia formation. Cancer Research, 70, 4634–4643.
Lee, Z., Cheng, C. T., Zhang, H., Subler, M. A., Wu, J., Mukherjee, A., et al. (2008). Role of LPA4/p2y9/GPR23 in negative regulation of cell motility. Molecular Biology of the Cell, 19, 5435–5445.
Stefan, C., Jansen, S., & Bollen, M. (2005). NPP-type ectophosphodiesterases: unity in diversity. Trends in Biochemical Sciences, 30, 542–550.
van Meeteren, L. A., & Moolenaar, W. H. (2007). Regulation and biological activities of the autotaxin-LPA axis. Progress in Lipid Research, 46, 145–160.
Kanda, H., Newton, R., Klein, R., Morita, Y., Gunn, M. D., & Rosen, S. D. (2008). Autotaxin, an ectoenzyme that produces lysophosphatidic acid, promotes the entry of lymphocytes into secondary lymphoid organs. Nature Immunology, 9, 415–423.
Dusaulcy, R., Rancoule, C., Gres, S., Wanecq, E., Colom, A., Guigne, C., et al. (2011). Adipose-specific disruption of autotaxin enhances nutritional fattening and reduces plasma lysophosphatidic acid. Journal of Lipid Research, 52(6), 1247–1255.
van Meeteren, L. A., Ruurs, P., Christodoulou, E., Goding, J. W., Takakusa, H., Kikuchi, K., et al. (2005). Inhibition of autotaxin by lysophosphatidic acid and sphingosine 1-phosphate. Journal of Biological Chemistry, 280, 21155–21161.
Nishimasu, H., Okudaira, S., Hama, K., Mihara, E., Dohmae, N., Inoue, A., et al. (2011). Crystal structure of autotaxin and insight into GPCR activation by lipid mediators. Nature Structural and Molecular Biology, 18, 205–212.
Hausmann, J., Kamtekar, S., Christodoulou, E., Day, J. E., Wu, T., Fulkerson, Z., et al. (2011). Structural basis of substrate discrimination and integrin binding by autotaxin. Nature Structural and Molecular Biology, 18, 198–204.
Pamuklar, Z., Federico, L., Liu, S., Umezu-Goto, M., Dong, A., Panchatcharam, M., et al. (2009). Autotaxin/lysopholipase D and lysophosphatidic acid regulate murine hemostasis and thrombosis. Journal of Biological Chemistry, 284, 7385–7394.
van Meeteren, L. A., Ruurs, P., Stortelers, C., Bouwman, P., van Rooijen, M. A., Pradere, J. P., et al. (2006). Autotaxin, a secreted lysophospholipase D, is essential for blood vessel formation during development. Molecular and Cellular Biology, 26, 5015–5022.
Tanaka, M., Okudaira, S., Kishi, Y., Ohkawa, R., Iseki, S., Ota, M., et al. (2006). Autotaxin stabilizes blood vessels and is required for embryonic vasculature by producing lysophosphatidic acid. Journal of Biological Chemistry, 281, 25822–25830.
Fotopoulou, S., Oikonomou, N., Grigorieva, E., Nikitopoulou, I., Paparountas, T., Thanassopoulou, A., et al. (2010). ATX expression and LPA signalling are vital for the development of the nervous system. Dev Biol, 339, 451–464.
Koike, S., Keino-Masu, K., & Masu, M. (2010). Deficiency of autotaxin/lysophospholipase D results in head cavity formation in mouse embryos through the LPA receptor-Rho-ROCK pathway. Biochemical and Biophysical Research Communications, 400, 66–71.
Matas-Rico, E., Garcia-Diaz, B., Llebrez-Zayas, P., Lopez-Barroso, D., Santin, L., Pedraza, C., et al. (2008). Deletion of lysophosphatidic acid receptor LPA1 reduces neurogenesis in the mouse dentate gyrus. Molecular and Cellular Neuroscience, 39, 342–355.
Gennero, I., Laurencin-Dalicieux, S., Conte-Auriol, F., Briand-Mesange, F., Laurencin, D., Rue, J., et al. (2011). Absence of the lysophosphatidic acid receptor LPA1 results in abnormal bone development and decreased bone mass. Bone, 49(3), 395–403.
Ye, X., Hama, K., Contos, J. J., Anliker, B., Inoue, A., Skinner, M. K., et al. (2005). LPA3-mediated lysophosphatidic acid signalling in embryo implantation and spacing. Nature, 435, 104–108.
Sumida, H., Noguchi, K., Kihara, Y., Abe, M., Yanagida, K., Hamano, F., et al. (2010). LPA4 regulates blood and lymphatic vessel formation during mouse embryogenesis. Blood, 116, 5060–5070.
Contos, J. J., Ishii, I., Fukushima, N., Kingsbury, M. A., Ye, X., Kawamura, S., et al. (2002). Characterization of lpa(2) (Edg4) and lpa(1)/lpa(2) (Edg2/Edg4) lysophosphatidic acid receptor knockout mice: signaling deficits without obvious phenotypic abnormality attributable to lpa(2). Molecular and Cellular Biology, 22, 6921–6929.
Kawagoe, H., Stracke, M. L., Nakamura, H., & Sano, K. (1997). Expression and transcriptional regulation of the PD-Ialpha/autotaxin gene in neuroblastoma. Cancer Research, 57, 2516–2521.
Zhang, G., Zhao, Z., Xu, S., Ni, L., & Wang, X. (1999). Expression of autotaxin mRNA in human hepatocellular carcinoma. Chinese Medical Journal, 112, 330–332.
Yang, S. Y., Lee, J., Park, C. G., Kim, S., Hong, S., Chung, H. C., et al. (2002). Expression of autotaxin (NPP-2) is closely linked to invasiveness of breast cancer cells. Clinical & Experimental Metastasis, 19, 603–608.
Stassar, M. J., Devitt, G., Brosius, M., Rinnab, L., Prang, J., Schradin, T., et al. (2001). Identification of human renal cell carcinoma associated genes by suppression subtractive hybridization. British Journal of Cancer, 85, 1372–1382.
Hoelzinger, D. B., Mariani, L., Weis, J., Woyke, T., Berens, T. J., McDonough, W. S., et al. (2005). Gene expression profile of glioblastoma multiforme invasive phenotype points to new therapeutic targets. Neoplasia, 7, 7–16.
Yang, Y., Mou, L., Liu, N., & Tsao, M. S. (1999). Autotaxin expression in non-small-cell lung cancer. American Journal of Respiratory Cell and Molecular Biology, 21, 216–222.
Baumforth, K. R., Flavell, J. R., Reynolds, G. M., Davies, G., Pettit, T. R., Wei, W., et al. (2005). Induction of autotaxin by the Epstein–Barr virus promotes the growth and survival of Hodgkin lymphoma cells. Blood, 106, 2138–2146.
Masuda, A., Nakamura, K., Izutsu, K., Igarashi, K., Ohkawa, R., Jona, M., et al. (2008). Serum autotaxin measurement in haematological malignancies: a promising marker for follicular lymphoma. British Journal of Haematology, 143, 60–70.
Kehlen, A., Englert, N., Seifert, A., Klonisch, T., Dralle, H., Langner, J., et al. (2004). Expression, regulation and function of autotaxin in thyroid carcinomas. International Journal of Cancer, 109, 833–838.
Nam, S. W., Clair, T., Kim, Y. S., McMarlin, A., Schiffmann, E., Liotta, L. A., et al. (2001). Autotaxin (NPP-2), a metastasis-enhancing motogen, is an angiogenic factor. Cancer Research, 61, 6938–6944.
Black, E. J., Clair, T., Delrow, J., Neiman, P., & Gillespie, D. A. (2004). Microarray analysis identifies autotaxin, a tumour cell motility and angiogenic factor with lysophospholipase D activity, as a specific target of cell transformation by v-Jun. Oncogene, 23, 2357–2366.
Zirn, B., Samans, B., Wittmann, S., Pietsch, T., Leuschner, I., Graf, N., et al. (2006). Target genes of the WNT/beta-catenin pathway in Wilms tumors. Genes, Chromosomes & Cancer, 45, 565–574.
Tice, D. A., Szeto, W., Soloviev, I., Rubinfeld, B., Fong, S. E., Dugger, D. L., et al. (2002). Synergistic induction of tumor antigens by Wnt-1 signaling and retinoic acid revealed by gene expression profiling. Journal of Biological Chemistry, 277, 14329–14335.
Dufner-Beattie, J., Lemons, R. S., & Thorburn, A. (2001). Retinoic acid-induced expression of autotaxin in N-myc-amplified neuroblastoma cells. Molecular Carcinogenesis, 30, 181–189.
Zirn, B., Samans, B., Spangenberg, C., Graf, N., Eilers, M., & Gessler, M. (2005). All-trans retinoic acid treatment of Wilms tumor cells reverses expression of genes associated with high risk and relapse in vivo. Oncogene, 24, 5246–5251.
Chen, M., & O’Connor, K. L. (2005). Integrin alpha6beta4 promotes expression of autotaxin/ENPP2 autocrine motility factor in breast carcinoma cells. Oncogene, 24, 5125–5130.
Nam, S. W., Clair, T., Campo, C. K., Lee, H. Y., Liotta, L. A., & Stracke, M. L. (2000). Autotaxin (ATX), a potent tumor motogen, augments invasive and metastatic potential of ras-transformed cells. Oncogene, 19, 241–247.
Boucharaba, A., Serre, C. M., Gres, S., Saulnier-Blache, J. S., Bordet, J. C., Guglielmi, J., et al. (2004). Platelet-derived lysophosphatidic acid supports the progression of osteolytic bone metastases in breast cancer. The Journal of Clinical Investigation, 114, 1714–1725.
Boucharaba, A., Serre, C. M., Guglielmi, J., Bordet, J. C., Clezardin, P., & Peyruchaud, O. (2006). The type 1 lysophosphatidic acid receptor is a target for therapy in bone metastases. Proceedings of the National Academy of Sciences of the United States of America, 103, 9643–9648.
David, M., Wannecq, E., Descotes, F., Jansen, S., Deux, B., Ribeiro, J., et al. (2010). Cancer cell expression of autotaxin controls bone metastasis formation in mouse through lysophosphatidic acid-dependent activation of osteoclasts. PLoS One, 5, e9741.
Yu, S., Murph, M. M., Lu, Y., Liu, S., Hall, H. S., Liu, J., et al. (2008). Lysophosphatidic acid receptors determine tumorigenicity and aggressiveness of ovarian cancer cells. Journal of the National Cancer Institute, 100, 1630–1642.
Taghavi, P., Verhoeven, E., Jacobs, J. J., Lambooij, J. P., Stortelers, C., Tanger, E., et al. (2008). In vitro genetic screen identifies a cooperative role for LPA signaling and c-Myc in cell transformation. Oncogene, 27, 6806–6816.
Liu, S., Umezu-Goto, M., Murph, M., Lu, Y., Liu, W., Zhang, F., et al. (2009). Expression of autotaxin and lysophosphatidic acid receptors increases mammary tumorigenesis, invasion, and metastases. Cancer Cell, 15, 539–550.
Lin, S., Wang, D., Iyer, S., Ghaleb, A. M., Shim, H., Yang, V. W., et al. (2009). The absence of LPA2 attenuates tumor formation in an experimental model of colitis-associated cancer. Gastroenterology, 136, 1711–1720.
Lin, S., Lee, S. J., Shim, H., Chun, J., & Yun, C. C. (2010). The absence of LPA receptor 2 reduces the tumorigenesis by Apc Min mutation in the intestine. American Journal of Physiology. Gastrointestinal and Liver Physiology, 299, G1128–G1138.
Nakai, Y., Ikeda, H., Nakamura, K., Kume, Y., Fujishiro, M., Sasahira, N., et al. (2011). Specific increase in serum autotaxin activity in patients with pancreatic cancer. Clinical Biochemistry, 44(8–9), 576–581.
Lu, Y., Lemon, W., Liu, P. Y., Yi, Y., Morrison, C., Yang, P., et al. (2006). A gene expression signature predicts survival of patients with stage I non-small cell lung cancer. PLoS Medicine, 3, e467.
Lee, S., Jeong, J., Majewski, T., Scherer, S. E., Kim, M. S., Tuziak, T., et al. (2007). Forerunner genes contiguous to RB1 contribute to the development of in situ neoplasia. Proceedings of the National Academy of Sciences of the United States of America, 104, 13732–13737.
Pasternack, S. M., von Kugelgen, I., Aboud, K. A., Lee, Y. A., Ruschendorf, F., Voss, K., et al. (2008). G protein-coupled receptor P2Y5 and its ligand LPA are involved in maintenance of human hair growth. Nature Genetics, 40, 329–334.
Yanagida, K., Masago, K., Nakanishi, H., Kihara, Y., Hamano, F., Tajima, Y., et al. (2009). Identification and characterization of a novel lysophosphatidic acid receptor, p2y5/LPA6. Journal of Biological Chemistry, 284(26), 17731–17741.
Kaplan, M. H., Smith, D. I., & Sundick, R. S. (1993). Identification of a G protein coupled receptor induced in activated T cells. Journal of Immunology, 151, 628–636.
Majewski, T., Lee, S., Jeong, J., Yoon, D. S., Kram, A., Kim, M. S., et al. (2008). Understanding the development of human bladder cancer by using a whole-organ genomic mapping strategy. Laboratory Investigation, 88, 694–721.
Song, H., Ramus, S. J., Shadforth, D., Quaye, L., Kjaer, S. K., Dicioccio, R. A., et al. (2006). Common variants in RB1 gene and risk of invasive ovarian cancer. Cancer Research, 66, 10220–10226.
Kazantseva, A., Goltsov, A., Zinchenko, R., Grigorenko, A. P., Abrukova, A. V., Moliaka, Y. K., et al. (2006). Human hair growth deficiency is linked to a genetic defect in the phospholipase gene LIPH. Science, 314, 982–985.
Crawford, J. M. (2008). The origins of bladder cancer. Laboratory Investigation, 88, 686–693.
Baker, D. L., Fujiwara, Y., Pigg, K. R., Tsukahara, R., Kobayashi, S., Murofushi, H., et al. (2006). Carba analogs of cyclic phosphatidic acid are selective inhibitors of autotaxin and cancer cell invasion and metastasis. Journal of Biological Chemistry, 281, 22786–22793.
Durgam, G. G., Virag, T., Walker, M. D., Tsukahara, R., Yasuda, S., Liliom, K., et al. (2005). Synthesis, structure-activity relationships, and biological evaluation of fatty alcohol phosphates as lysophosphatidic acid receptor ligands, activators of PPARgamma, and inhibitors of autotaxin. Journal of Medicinal Chemistry, 48, 4919–4930.
Zhang, H., Xu, X., Gajewiak, J., Tsukahara, R., Fujiwara, Y., Liu, J., et al. (2009). Dual activity lysophosphatidic acid receptor pan-antagonist/autotaxin inhibitor reduces breast cancer cell migration in vitro and causes tumor regression in vivo. Cancer Research, 69, 5441–5449.
van Meeteren, L. A., Brinkmann, V., Saulnier-Blache, J. S., Lynch, K. R., & Moolenaar, W. H. (2008). Anticancer activity of FTY720: phosphorylated FTY720 inhibits autotaxin, a metastasis-enhancing and angiogenic lysophospholipase D. Cancer Letters, 266, 203–208.
Gupte, R., Patil, R., Liu, J., Wang, Y., Lee, S. C., Fujiwara, Y., et al. (2011). Benzyl and naphthalene methylphosphonic acid inhibitors of autotaxin with anti-invasive and anti-metastatic activity. ChemMedChem, 6, 922–935.
Albers, H. M., Dong, A., van Meeteren, L. A., Egan, D. A., Sunkara, M., van Tilburg, E. W., et al. (2010). Boronic acid-based inhibitor of autotaxin reveals rapid turnover of LPA in the circulation. Proceedings of the National Academy of Sciences of the United States of America, 107, 7257–7262.
Albers, H. M., van Meeteren, L. A., Egan, D. A., van Tilburg, E. W., Moolenaar, W. H., & Ovaa, H. (2010). Discovery and optimization of boronic acid based inhibitors of autotaxin. Journal of Medicinal Chemistry, 53, 4958–4967.
Gierse, J., Thorarensen, A., Beltey, K., Bradshaw-Pierce, E., Cortes-Burgos, L., Hall, T., et al. (2010). A novel autotaxin inhibitor reduces lysophosphatidic acid levels in plasma and the site of inflammation. Journal of Pharmacology and Experimental Therapeutics, 334, 310–317.
Acknowledgments
Work related to this review is supported by grants from the Dutch Cancer Society and the Netherlands Organization of Pure Research. We thank Anastassis Perrakis for designing Fig. 1.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Houben, A.J.S., Moolenaar, W.H. Autotaxin and LPA receptor signaling in cancer. Cancer Metastasis Rev 30, 557–565 (2011). https://doi.org/10.1007/s10555-011-9319-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-011-9319-7