Abstract
To investigate the role of right ventricular free wall strain (RVFWSL) to predict low functional capacity in repaired tetralogy of Fallot (rTOF). We prospectively enrolled 33 patients with rTOF with moderate to severe PR who underwent rest and peak exercise echocardiography on a semisupine cycloergometer. Conventional function and strain imaging parameters of both ventricles were measured. Patients performing < 7 METS were defined to have low functional capacity. Logistic regression was used to identify parameters associated with low functional capacity. Eleven patients (33.3%) had low functional capacity. These patients were shorter (height 155 ± 7 vs 163 ± 9 cm, p = 0.023), more frequently female (27.3 vs 72.7%, p = 0.024) and had history of Blalock–Taussig shunt (45.5 vs 9.1%, p = 0.027). On multivariate analysis RVFWSL was the only predictor of low functional capacity OR 1.39 (CI 95%, 1.06–1.83., p = 0.018) per % change. A RVFWSL < 17% (absolute value) had an AUC of 0.785, sensitivity of 81.8% and specificity of 77.3% to predict low functional capacity. Right ventricular free wall strain is an independent predictor of low functional capacity in repaired tetralogy of Fallot with moderate to severe PR. A value < 17% might be useful in deciding when to perform pulmonary valve replacement, when functional capacity cannot be objectively measured.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart disease, occurring in approximately one in 3500 births [1]. Surgical repair has significantly changed the natural history of disease. However late after TOF repair significant comorbidities such as arrhythmias, sudden cardiac death, valvular heart disease and heart failure are common and contribute to adverse clinical outcomes [2]. Pulmonary regurgitation (PR) is the most common hemodynamic sequelae, and the main culprit for late complications [3]. NYHA functional class in patients with PR after TOF repair is a powerful predictor of hospitalization and death [4]. Accordingly guidelines give a Class I recommendation to perform pulmonary valve replacement (PVR) for patients with repaired TOF and moderate or greater PR with cardiovascular symptoms not otherwise explained (dyspnea, chest pain, and/or exercise intolerance). In the absence of symptoms, right ventricular dilation or dysfunction are considered reasonable triggers for PVR [2]
When measured objectively, more than 50% of patients who reported no symptoms have a reduced functional capacity [5, 6]. However stress testing is not always feasible. Therefore, we aimed to identify resting echocardiographic parameters that could predict low functional capacity.
Materials and methods
Study population
We prospectively enrolled asymptomatic patients (NYHA Class I) with repaired TOF and moderate to severe pulmonary regurgitation regularly evaluated in a dedicated adult congenital heart disease clinic, who were referred for echocardiographic examination to our department during the period March 2018–June 2019. To be eligible, patients had to be able to exercise on a semisupine cycle ergometer. Exclusion criteria included pregnancy, significant comorbidities limiting prognosis (life expectancy < 1 year) and associated major cardiac anomalies (atrioventricular canal, major aortopulmonary collateral arteries, pulmonary hypertension and Ebstein anomaly). All patients gave their informed consent prior to their inclusion in the study.
Echocardiographic examination
A complete baseline echocardiogram was performed before stress test, all measurements were performed according to current recommendations [7] using a Vivid-E9 machine (General Electric, Milwaukee, USA). Pulmonary regurgitation and stenosis were classified as mild, moderate or severe according to the recommendations of the American Society of Echocardiography [8,9,10]. Briefly, severity was visually assessed by an experienced echocardiographer, patients with more than mild pulmonary regurgitation were included in the study. Using color Doppler, and continuous wave Doppler, we evaluated jet width/annulus ratio, pulmonary regurgitation spectrum, pressure half time (PHT), early termination of the PR and diastolic flow reversal in the proximal branches. A PHT < 100 ms, PR index < 0.77, presence of diastolic flow reversal in the pulmonary branches and PR jet width/pulmonary annulus > 0.7, were the severity parameters used. Patients with the presence of 3 of this criteria, or 2 if PR index was < 0.77 and diastolic flow reversal in the pulmonary branches was present were classified as severe PR, while patients not satisfying these criteria were classified as moderate.
Exercise stress echocardiography
We performed exercise echocardiography (ESE) using semi supine cycle ergometry (Schiller CE 0124 Ergosana). With an Initial workload of 25 W, with 25 W increments every 2 min. Dedicated images for right free wall, left ventricular global longitudinal strain and three-dimensional volumes/ejection fraction were recorded at rest, peak stress and early recovery. All right function parameters were measured using a focused right ventricular view [11]. The following parameters were measured at rest and at peak exercise: tricuspid annular plane systolic excursion (TAPSE), right ventricular fractional area change (RV FAC), tissue Doppler (TDI) tricuspid and mitral annular velocities, trans-tricuspid and transmitral inflow velocities, peak tricuspid regurgitation jet velocity, peak systolic transpulmonary gradient, peak protodiastolic pulmonary gradient (from pulmonary regurgitation continuous Doppler), end diastolic and end systolic left ventricular volumes as well as left ventricular ejection fraction. All images were stored for offline analysis.
Furthermore, we measured left ventricular contractile reserve (LVCR) defined as the stress/rest ratio of force, calculated as the ratio between systolic pressure (by automated cuff sphygmomanometer) and left ventricular end-systolic volume. End-systolic volume was obtained from the apical four- and two-chamber views using the biplane Simpson method [12, 13].
Right ventricular contractile reserve (RVCR) was defined as any increase in RV FAC between rest and peak exercise stress, calculated as [(RV FAC at peak exercise—RV FAC at rest)/RV FAC at rest] × 100 [14]. Right ventricular force (elastance) was calculated as the ratio between protodiastolic peak pulmonary gradient (as a surrogate of mean pulmonary artery pressure) [15] and right ventricular end-systolic area. The ratio of early trans-tricuspid flow velocity to annular velocity (E/e´) was considered an index of RV filling pressures. Lung ultrasound scanning was performed at rest and soon after exercise in the semisupine position using the simplified 4 region scan protocol [16].
Patients with < 7 metabolic equivalent of task (METs) were defined to have low functional capacity [17]. METs were calculated using the generated power (Watts) and the patient´s weight during cycle ergometry [18].
Strain analysis
Images were stored and analyzed offline in a dedicated workstation (EchoPAC GE v11.3). The images were analyzed by an experienced echocardiographer in strain imaging blinded to clinical data. For right ventricular free-wall longitudinal strain (RVFWSL), the delineation started at the lateral tricuspid annulus level and stopped at the insertion of the RV free wall in the LV [19]. The endocardium was manually traced using the single wall tracking tool and adjusted to the wall thickness. RVFWSL was calculated from a focused right chamber view, by averaging the segmental maximum peak longitudinal strain of the RV free wall. For LV strain and LV mechanical dispersion, standard four, three and two chamber views were used, according to the EACVI/ ASE/Industry Task Force for 2D speckle tracking echocardiography [20]. Adequate tracking was visually assessed before acceptance. Inter-observer variability was assessed in 14 anonymized cases by using measures from two observers (ARC and HRZ). Intra-observer variability was assessed in the same cases measured by the same with a 2 weeks difference period.
Three-dimensional (3D) analysis
Dataset acquisition for 3DE images was performed using second harmonic imaging from the apical approach. During acquisition, we used the multi-slice display to ensure that the entire LV or RV cavity was included in the dataset. Four to six consecutive electrocardiography-gated sub-volumes were acquired during breath holding to generate full-volume datasets with a minimum volume rate of 20 vps [21]. Datasets were stored digitally in raw-data format and exported to a separate workstation. Measurements of 3DE LV volumes and LVEF were performed using a commercially available software package (4D AutoLVQ, GE Vingmed Ultrasound, Horten, Norway). Briefly, initialization of LV endocardial border tracing was manually performed by identifying two points on the 4-chamber view image at end-diastole and at end-systole (1 point in the middle of the mitral annulus and a second point at the LV apex). Manual editing of the semi-automatically generated endocardial contours was routinely applied to include the LV outflow tract, as well as papillary muscles and trabeculae within the LV cavity [22]. Measurements of the 3D RV volumes and RVEF were performed using the analysis by TomTec software (TomTec Imaging Systems, Unterschleissheim, Germany). Three orthogonal planes and various landmarks were selected to define the end-diastolic and end-systolic frames. The program automatically supplies 4-chamber, sagittal, and coronal RV views on the basis of the initial view adjustment. Right ventricular end diastolic volume (RVEDV) and right ventricular end systolic volume (RVESV) were calculated from 3D echocardiographic data sets. RVEF was determined as follows: RVEF = [(RVEDV-RVESV)/RVEDV] × 100.
Statistical analysis
Statistical analysis was performed using Stata V12.1. Shapiro–Wilk test was used to study the distribution of numerical variables. Parametric variables are expressed as mean ± standard deviation, comparison between groups was done with Student’s t test. Non parametric variables are expressed as median and interquartile ranges, comparison between groups was performed using Wilcoxon sum rank test. Categorical variables are summarized as percentage, comparison between groups was done with Xi2. To identify which parameters were independently associated with low functional capacity, multivariate logistic regression was performed including significant variables on univariate analysis. ROC curves were plotted to identify the cut-off value of RVFWSL to predict low functional capacity. Sensitivity, specificity and likelihood ratios were calculated using this cut-off value assuming the best case scenario. Two tailed P values with an α error less than 0.05 were considered statistically significant. RVFWSL variability was assessed by analyzing intra-class correlation (ICC) in 14 randomly selected cases.
Results
Forty-two patients met the inclusion criteria, eight were excluded (two patients were not able to exercise, one because of osteo-muscular disease and the other with Down syndrome without the ability to follow the instructions for exercise, one patient was pregnant, one patient had an unstable stent in a pulmonary branch and four patients had associated major cardiac anomalies.)
A total of thirty-four patients were enrolled, one was eliminated due to non-interpretable functional capacity (development of an anxiety crisis at the beginning of exercise n = 1) (Fig. 1).
Thirty-three patients with repaired Tetralogy of Fallot and moderate to severe PR (42% women; mean age 26.3 ± 6.7) were enrolled. Demographic and clinical data are summarized in Table 1. ESE was feasible in all patients. Eleven patients (33.3%) were found to have low functional capacity (achieved < 7 MET). Patients with low functional capacity were shorter (height 155 ± 7 vs 163 ± 9 cm, p = 0.023), more frequently female (27.3 vs 72.7%, p = 0.024) and had more common history of Blalock–Taussig shunt (45.5 vs 9.1%, p = 0.027). Additionally, the period of time from repair surgery to ESE was longer in those with low functional capacity (21.3 ± 6.5 vs 17.5 ± 4.9 years, p = 0.07). Importantly, the prevalence of severe pulmonary regurgitation and RVCR was comparable among groups (63.6 vs 72.7%, p = 0.709) and (72.7 vs 81.8%, p = 0.687) respectively.
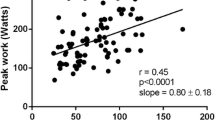
None of the resting LV systolic or diastolic echocardiographic parameters were related to low functional capacity. Both LV GLS and contractile reserve were impaired in both groups, whereas patients with low functional capacity had lower values of LV contractile reserve (1.4 ± 0.37 vs 1.7 ± 0.48, p = 0.048), (Table 2). Right ventricular ejection fraction was comparable in both groups (50.5 ± 6.5 vs 48.3 ± 7.7, p = 0.505) but only feasible in 67% of patients. RVFWSL (14.4 ± 4.8 vs 20.2 ± 3.6, p = 0.0005) was the only resting echocardiographic parameter related to low functional capacity. In multivariate analysis including gender, height, RVFWSL and previous shunt palliation, RVFWSL remained the only predictor of low functional capacity (OR 1.39 CI 95%, 1.06–1.83., p = 0.018 per % change). Table 3. A RVFWSL < 17% (absolute value) had an AUC of 0.785 to predict low functional capacity (Fig. 2). In the best case scenario (since there was no validation in an independent cohort) this cut off value had a sensitivity of 81.8% and specificity of 77.3% to predict low functional capacity. A representative example of a patient with low functional capacity and normal functional capacity and their correspondent RVFWSL values is shown in Fig. 3.
ROC curve analysis. Receiver-operating characteristic (ROC) curves demonstrating diagnostic accuracy of right ventricular free wall longitudinal strain (RVFWSL) to predict low functional capacity. Sens sensitivity, Sp specificity, LR likelihood ratio, AUC area under the receiver-operating characteristic curve
We performed a second multivariate analysis including LV GLS, although it was not statistically significant in univariate analysis. In this model RVFWSL remained the only independent predictor of low functional capacity (OR 1.3, CI 95% 1.03–1.63, p = 0.027 per % change) (Table 4.)
A good inter-observer agreement was found in the measurement of RVFWSL, ICC 0.95 (0.85–0.98, 95%CI).
Discussion
This study provides new evidence about the feasibility of ESE and clinical value of RVFWSL in patients with repaired tetralogy of Fallot (rTOF) and moderate to severe PR.
Our main findings can be summarized as follows: (1) right ventricular function quantification using TAPSE, FAC and right ventricular free wall strain is highly feasible in patients with rTOF and moderate to severe PR during exercise (2) in patients with rTOF and moderate to severe PR, subclinical left ventricular dysfunction is common (low GLS values and LVCR), however resting diastolic and systolic function parameters are not related to functional capacity. (3) low rest RVFWSL is an independent predictor of low functional capacity.
Surgical repair has improved survival in patients with tetralogy of Fallot, leading to an exponential growth of this population. Nonetheless late after repair complications are common and contribute to adverse clinical outcomes [2]. Severe pulmonary regurgitation is common (consistently 67% of our study population had severe PR), and contributes to adverse outcomes [3]. The presence of symptoms in patients with severe PR is currently a trigger for PVR according to the latest guidelines [2] aiming to improve symptoms and avoid ventricular function deterioration, although a significant benefit in mortality has yet to be demonstrated [23,24,25]. However the presence of symptoms can be underestimated, since patients with rTOF are in general younger than other patients with cardiovascular disease (i.e. HF, CAD, etc.) and have a long standing disease adapting their daily activities to their performance. Over 50% of patients with adult congenital heart disease (ACHD) in NYHA class 1 who underwent cardiopulmonary exercise testing, have been previously shown to have a peak VO2 below 80% of predicted for age and gender and thus, have an impaired functional capacity despite the lack of symptoms [5, 6]. In our study 33.3% of the patients were found to be symptomatic during ESE, most of which had severe PR, uncovering the need for PVR according to current guideline recommendations [2]. This finding highlights clinical assessment in the outpatient setting might not be sensitive enough and ESE may have important additional prognostic value in patients with rTOF. Furthermore, reclassification of NYHA with an objective test has prognostic implications as it has been shown that adult congenital heart disease patients with NYHA class II have a 2.5 fold increased risk of death. (5) With the increasing number of patients with ACHD, it might not be always feasible to perform cardiopulmonary exercise testing (CPET) or ESE, furthermore ACHD patients may not be able to exercise. Accordingly, the value of resting imaging variables as surrogate of low functional class might be useful for clinical decision making.
Although left ventricular dysfunction is common (reduced LVEF and/or GLS) in patients with rTOF, and its presence carries increased risk of mortality [26], we found none of these parameters were useful to predict a low functional capacity. Importantly RVFWSL was the only resting echocardiographic parameter capable to predict low functional capacity. Alghamdi et al. reported that RVFWSL was the best predictor of functional capacity, even superior to RVEF measured with cardiac MRI [27]. Also the most recent guidelines on multimodality imaging in ACHD support the use of RVFWSL in the follow up of ACHD patients [28]. Our study supports these findings and adds to literature a RVFWSL cut off value of < 17% (absolute value) during rest echocardiography which strongly correlates to low functional capacity.
Although the precise mechanism by which RVFWSL predicts low functional capacity is not clear, several theories might account for this finding. First, RVFWSL strongly correlates with the degree of histological fibrosis (R = 0.8, p < 0.0001), and was found to be markedly superior to TAPSE (r = 0.34, 0.05) [29]. Therefore the degree of right ventricular fibrosis resulting in lower RVFWSL might contribute to abnormal exercise capacity. Second, patients with rTOF have been shown to have reduced right ventricular contractile reserve (RVCR) during stress compared to healthy subjects [30, 31]. Up to 40% of patients with rTOF do not have an increase in right ventricular function parameters during stress, supporting the notion of subclinical right ventricular dysfunction [14, 30]. Furthermore late after rTOF in a small subset during a 4.2 years follow up small increases in end systolic and diastolic volumes below guideline recommended thresholds were found, however a significant change in RVFWSL occurred [32]. These findings suggests RVFWSL might be able to detect patients with right ventricular dysfunction at an earlier stage, just as global longitudinal strain of the left ventricle has been shown to be useful to refine prognostic stratification [33,34,35].
The study of RVFWSL in patients with rTOF is particularly important as it carries incremental prognostic value as it has been related to poor quality of life, and adverse events (composite of death or heart failure), and in the present study with impaired functional class [36].
Study limitations
Small sample from a single institution is a limitation that needs to be acknowledged. However, our results add to the reported prognostic value of RVFWSL and for the first time (to the best of our knowledge) we present a cut off value of RVFWSL to predict low functional capacity in patients with repaired tetralogy of Fallot and moderate to severe PR. Our laboratory lacks the capacity of measuring expired gases and thus, the performance of a complete CPET, however the evaluation of NYHA functional class has been shown to be prognostically important in patients with ACHD. Although functional capacity was measured with the calculation of METs during semi supine cycloergometer, there is plenty of scientific evidence supporting the measurement of functional capacity with the calculation of METs and its strong predictive value for mortality [37, 38].
Moreover, previously reported mean peak VO2 values among rTOF individuals with mean age of 29–32 years are 24.2–25.2 ml/kg/min (corresponding to mean 71% of predicted) [39]. The threshold to define low functional capacity in our study was 7 METs which corresponds to an estimated VO2 of 24.5 ml/min/kg. Hence in our cohort, individuals of similar age within the low functional capacity group achieved a median of 6.2 METs which likely represents true impaired exercise capacity.
Cardiac magnetic resonance (CMR) was not available within an acceptable time limit in most of our patients and therefore CMR data is not reported. However, the objective of this study was not to investigate a correlation between RVFWSL and RVEF measured with MRI and 3D echocardiogram which has been previously reported [27, 32], but to identify resting echocardiographic predictors of low functional capacity. Despite the fact that 3D and MRI RVED and volumes have a good correlation (r = 0.73), [40] in our study less than a 50% of the acquisitions were considered optimal (most of our patients had severe pulmonary regurgitation and important RV dilation which limits the acquisition quality) and was only feasible in 67% of the patients.
Quantification of pulmonary regurgitation in our study was performed by integrating multiple parameters as recommended by the American Society of Echocardiography guidelines. Although CMR was not performed to quantitate PR, echocardiography can reliable detect severe PR with multi parametric assessment compared to CMR. It has been shown in patients with rTOF that combining multiple 2D and Doppler echocardiography parameters; specifically, if diastolic flow reversal in branch pulmonary arteries and PR index < 0.77 were both present, the probability of having severe pulmonary valve regurgitation was 100% as compared with CMR (defined as the presence of ≥ 40% regurgitant volume) [41]. Furthermore, echocardiography can reliably distinguish mild pulmonary regurgitation, and has been shown to have a sensitivity of 97% to identify more than moderate PR compared to CMR [42]. Quantitative assessment of PR with echocardiography is challenging and lacks validation, and therefore was not used in this study. In our study ten patients had a CMR available with quantitation of pulmonary regurgitation severity with a time limit of 6 months. Agreement between CMR and echocardiography for classifying PR was 90% with a kappa coefficient of 0.62, p = 0.01 in this patient subset.
Conclusions
Right ventricular free wall strain is an independent predictor of low functional capacity in repaired tetralogy of Fallot patients with moderate to severe pulmonary regurgitation. A value < 17% might be useful in deciding when to perform pulmonary valve replacement, especially in those in which functional capacity cannot be objectively measured.
References
Villafañe J, Feinstein JA, Jenkins KJ et al (2013) Hot topics in tetralogy of Fallot. J Am Coll Cardiol 62:2155–2166. https://doi.org/10.1016/j.jacc.2013.07.100
Stout KK, Daniels CJ, Aboulhosn JA et al (2018) 2018 AHA/ACC Guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. https://doi.org/10.1161/CIR.0000000000000603
Pandya B, Quail MA, Cullen S (2013) Clinical issues and outcomes in adults following repair of tetralogy of Fallot. Curr Treat Options Cardiovasc Med 15:602–614. https://doi.org/10.1007/s11936-013-0264-3
Giardini A, Specchia S, Tacy TA et al (2007) Usefulness of cardiopulmonary exercise to predict long-term prognosis in adults with repaired tetralogy of Fallot. Am J Cardiol 99:1462–1467. https://doi.org/10.1016/j.amjcard.2006.12.076
Bredy C, Ministeri M, Kempny A et al (2018) New York Heart Association (NYHA) classification in adults with congenital heart disease: relation to objective measures of exercise and outcome. Eur Heart J - Qual Care Clin Outcomes 4:51–58. https://doi.org/10.1093/ehjqcco/qcx031
Lim FY, Yap J, Gao F et al (2018) Correlation of the New York Heart Association classification and the cardiopulmonary exercise test: a systematic review. Int J Cardiol 263:88–93. https://doi.org/10.1016/j.ijcard.2018.04.021
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39.e14. https://doi.org/10.1016/j.echo.2014.10.003
Valente AM, Cook S, Festa P et al (2014) Multimodality imaging guidelines for patients with repaired tetralogy of Fallot: a report from the American Society of Echocardiography. J Am Soc Echocardiogr 27:111–141. https://doi.org/10.1016/j.echo.2013.11.009
Zoghbi WA, Asch FM, Bruce C et al (2019) Guidelines for the Evaluation of Valvular Regurgitation After Percutaneous Valve Repair or Replacement. J Am Soc Echocardiogr 32:431–475. https://doi.org/10.1016/j.echo.2019.01.003
Zoghbi WA, Adams D, Bonow RO et al (2017) Recommendations for noninvasive evaluation of native valvular regurgitation. J Am Soc Echocardiogr 30:303–371. https://doi.org/10.1016/j.echo.2017.01.007
Genovese D, Mor-Avi V, Palermo C et al (2019) Comparison between four-chamber and right ventricular–focused views for the quantitative evaluation of right ventricular size and function. J Am Soc Echocardiogr 32:484–494. https://doi.org/10.1016/j.echo.2018.11.014
Picano E, Ciampi Q, Wierzbowska-Drabik K et al (2018) The new clinical standard of integrated quadruple stress echocardiography with ABCD protocol. Cardiovasc Ultrasound. https://doi.org/10.1186/s12947-018-0141-z
Cortigiani L, Huqi A, Ciampi Q et al (2018) Integration of wall motion, coronary flow velocity, and left ventricular contractile reserve in a single test: prognostic value of vasodilator stress echocardiography in patients with diabetes. J Am Soc Echocardiogr 31:692–701. https://doi.org/10.1016/j.echo.2017.11.019
Ait-Ali L, Siciliano V, Passino C et al (2014) Role of stress echocardiography in operated Fallot: feasibility and detection of right ventricular response. J Am Soc Echocardiogr 27:1319–1328. https://doi.org/10.1016/j.echo.2014.08.006
Masuyama T, Kodama K, Kitabatake A et al (1986) Continuous-wave Doppler echocardiographic detection of pulmonary regurgitation and its application to noninvasive estimation of pulmonary artery pressure. Circulation 74:484–492
Scali MC, Zagatina A, Simova I et al (2017) B-lines with lung ultrasound: the optimal scan technique at rest and during stress. Ultrasound Med Biol 43:2558–2566. https://doi.org/10.1016/j.ultrasmedbio.2017.07.007
Goldman L, Hashimoto B, Cook EF, Loscalzo A (1981) Comparative reproducibility and validity of systems for assessing cardiovascular functional class: advantages of a new specific activity scale. Circulation 64:1227–1234
American College of Sports Medicine, Riebe D, Ehrman JK, et al (2018) ACSM’s guidelines for exercise testing and prescription, 10th edn. Wolters Kluwer, Philadelphia
Badano LP, Kolias TJ, Muraru D, et al (2018) Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J 19:591–600. https://doi.org/10.1093/ehjci/jey042
Voigt J-U, Pedrizzetti G, Lysyansky P, et al (2015) Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J 16:1–11. https://doi.org/10.1093/ehjci/jeu184
Lang RM, Badano LP, Tsang W, et al (2012) EAE/ASE Recommendations for image acquisition and display using three-dimensional echocardiography. Eur Heart J 13:1–46. https://doi.org/10.1093/ehjci/jer316
Rodríguez-Zanella H, Muraru D, Secco E et al (2018) Added value of 3- versus 2-dimensional echocardiography left ventricular ejection fraction to predict arrhythmic risk in patients with left ventricular dysfunction. JACC Cardiovasc Imaging. https://doi.org/10.1016/j.jcmg.2018.07.011
Ferraz Cavalcanti PE, Sá MPBO, Santos CA et al (2013) Pulmonary valve replacement after operative repair of tetralogy of Fallot. J Am Coll Cardiol 62:2227–2243. https://doi.org/10.1016/j.jacc.2013.04.107
Bokma JP, Geva T, Sleeper LA et al (2018) A propensity score-adjusted analysis of clinical outcomes after pulmonary valve replacement in tetralogy of Fallot. Heart 104:738–744. https://doi.org/10.1136/heartjnl-2017-312048
Harrild DM, Berul CI, Cecchin F et al (2009) Pulmonary valve replacement in tetralogy of Fallot: impact on survival and ventricular tachycardia. Circulation 119:445–451. https://doi.org/10.1161/CIRCULATIONAHA.108.775221
Anabtawi A, Mondragon J, Dodendorf D, Laskey WK (2017) Late-stage left ventricular dysfunction in adult survivors of tetralogy of Fallot repair in childhood. Open Heart 4:e000690. https://doi.org/10.1136/openhrt-2017-000690
Alghamdi MH, Mertens L, Lee W, et al (2013) Longitudinal right ventricular function is a better predictor of right ventricular contribution to exercise performance than global or outflow tract ejection fraction in tetralogy of Fallot: a combined echocardiography and Magnetic Resonance Study. Eur Heart J 14:235–239. https://doi.org/10.1093/ehjci/jes137
Di Salvo G, Miller O, Babu Narayan S, et al (2018) Imaging the adult with congenital heart disease: a multimodality imaging approach—position paper from the EACVI. Eur Heart J 19:1077–1098. https://doi.org/10.1093/ehjci/jey102
Lisi M, Cameli M, Righini FM et al (2015) RV Longitudinal deformation correlates with myocardial fibrosis in patients with end-stage heart failure. JACC Cardiovasc Imaging 8:514–522. https://doi.org/10.1016/j.jcmg.2014.12.026
Bhatt SM, Wang Y, Elci OU et al (2019) Right ventricular contractile reserve is impaired in children and adolescents with repaired tetralogy of Fallot: an exercise strain imaging study. J Am Soc Echocardiogr 32:135–144. https://doi.org/10.1016/j.echo.2018.08.008
D’Alto M, Pavelescu A, Argiento P et al (2017) Echocardiographic assessment of right ventricular contractile reserve in healthy subjects. Echocardiography 34:61–68. https://doi.org/10.1111/echo.13396
Scherptong RWC, Mollema SA, Blom NA et al (2009) Right ventricular peak systolic longitudinal strain is a sensitive marker for right ventricular deterioration in adult patients with tetralogy of Fallot. Int J Cardiovasc Imaging 25:669–676. https://doi.org/10.1007/s10554-009-9477-7
Tower-Rader A, Mohananey D, To A et al (2018) Prognostic value of global longitudinal strain in hypertrophic cardiomyopathy. JACC Cardiovasc Imaging. https://doi.org/10.1016/j.jcmg.2018.07.016
Kusunose K, Goodman A, Parikh R et al (2014) Incremental prognostic value of left ventricular global longitudinal strain in patients with aortic stenosis and preserved ejection fraction. Circ Cardiovasc Imaging 7:938–945. https://doi.org/10.1161/CIRCIMAGING.114.002041
Sengeløv M, Jørgensen PG, Jensen JS et al (2015) Global longitudinal strain is a superior predictor of all-cause mortality in heart failure with reduced ejection fraction. JACC Cardiovasc Imaging 8:1351–1359. https://doi.org/10.1016/j.jcmg.2015.07.013
van Grootel RWJ, van den Bosch AE, Baggen VJM et al (2019) The prognostic value of myocardial deformation in adult patients with corrected tetralogy of Fallot. J Am Soc Echocardiogr 32:866–875.e2. https://doi.org/10.1016/j.echo.2019.03.014
Myers J, Prakash M, Froelicher V et al (2002) Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 346:793–801. https://doi.org/10.1056/NEJMoa011858
Kodama S (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301:2024. https://doi.org/10.1001/jama.2009.681
Kempny A, Dimopoulos K, Uebing A et al (2012) Reference values for exercise limitations among adults with congenital heart disease. Relation to activities of daily life–single centre experience and review of published data. Eur Heart J 33:1386–1396. https://doi.org/10.1093/eurheartj/ehr461
Iriart X, Montaudon M, Lafitte S et al (2009) Right ventricle three-dimensional echography in corrected tetralogy of fallot: accuracy and variability. Eur J Echocardiogr 10:784–792. https://doi.org/10.1093/ejechocard/jep071
Renella P, Aboulhosn J, Lohan DG et al (2010) Two-dimensional and doppler echocardiography reliably predict severe pulmonary regurgitation as quantified by cardiac magnetic resonance. J Am Soc Echocardiogr 23:880–886. https://doi.org/10.1016/j.echo.2010.05.019
Mercer-Rosa L, Yang W, Kutty S et al (2012) Quantifying pulmonary regurgitation and right ventricular function in surgically repaired tetralogy of Fallot: a comparative analysis of echocardiography and magnetic resonance imaging. Circ Cardiovasc Imaging 5:637–643. https://doi.org/10.1161/CIRCIMAGING.112.972588
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
This study has been approved by the ethics committee and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
All patients gave their informed consent prior to their inclusion in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Cuitlahuac Arroyo-Rodríguez and Juan Francisco Fritche–Salazar contributed equally to this study.
Rights and permissions
About this article
Cite this article
Arroyo-Rodríguez, C., Fritche-Salazar, J.F., Posada-Martínez, E.L. et al. Right ventricular free wall strain predicts functional capacity in patients with repaired Tetralogy of Fallot. Int J Cardiovasc Imaging 36, 595–604 (2020). https://doi.org/10.1007/s10554-019-01753-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01753-z