Abstract
The early detection of subclinical myocardial dysfunction can contribute to the treatment and prevention of heart failure (HF). The aim of the study was to (i) describe myocardial global longitudinal strain (GLS) patterns in a large general population sample from Norway and their relation to established cardiovascular disease (CVD) risk factors; (ii) to determine its normal thresholds in healthy individuals and (iii) ascertain the relation of myocardial GLS to stage A subclinical heart failure (SAHF). Participants (n = 1855) of the 7th survey of the population-based Tromsø Study of Norway (2015–2016) with GLS measurements were studied. Linear and logistic regression models were used for assessment of the associations between CVD risk factors and GLS. Mean GLS (SD) in healthy participants was − 15.9 (2.7) % in men and − 17.8 (3.1) % in women. Among healthy subjects, defined as those without known cardiovascular diseases and comorbidities, GLS declined with age. An increase of systolic blood pressure (SBP) of 10 mm Hg was associated with a 0.2% GLS reduction. Myocardial GLS in individuals with SAHF was 1.2% lower than in participants without SAHF (p < 0.001). Mean myocardial GLS declines with age in both sexes, both in a general population and in the healthy subsample. SBP increase associated with GLS decline in women. Our findings indicate high sensitivity of GLS for early subclinical stages of HF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is a leading cause of death worldwide [1]. Global myocardial longitudinal strain (GLS) is a derived deformation parameter, enabling detection of subtle left ventricular (LV) function abnormalities. GLS is superior to LV ejection fraction (LVEF) in prediction of cardiovascular mortality in patients with chronic kidney disease [2], all-cause mortality in patients with systolic heart failure (HF) [3] and atrial fibrillation [4]. Furthermore, myocardial GLS was found to be an independent predictor of the adverse outcomes after acute myocardial infarction (MI) [5], infective endocarditis [6], aortic stenosis [7], hypertrophic cardiomyopathy [8] and stroke [9]. The role of myocardial GLS in CVD mortality prediction in populations with low CVD risk has also been investigated [10]. In patients with arterial hypertension, myocardial GLS was related to structural remodeling of the LV [11]. Kuznetsova et al. have recently shown that high mean arterial pressure was associated with a decline in GLS over a follow-up of 4.7 years [12]. However, there are few studies of the associations between systolic blood pressure (SBP), hypertension treatment and GLS in general unselected populations.
To date there is no consensus, and thus no established clinical guidelines [13, 14], as to what constitutes cut points for normal myocardial GLS, however peak GLS level of − 20% mentioned as expected in healthy persons [13]. Assessment of cut off points of normal myocardial GLS in healthy individuals have produced varying results. Most population studies find higher reference values in healthy subjects [15, 16].
Stage A subclinical HF (SAHF) define individuals with absence of clinical symptoms or structural heart disease but presence of risk factors for HF [17]. SAHF progression is associated with impairment of structural and functional state of the heart over time with progression to the next stage of HF [18]. Myocardial GLS has improved prediction of subsequent clinical HF in patients with Stage B subclinical HF [19] and myocardial GLS is already known to be related to SAHF in high risk groups [20,21,22]. However, whether this applies to the whole SAHF group is, to the best of our knowledge, unknown. Whether GLS adds information in SAHF group beyond CVD risk factors and self-reported dyspnea symptoms in a general population has yet to be elucidated.
The main aim of our study is to describe peak-myocardial GLS in a large general population sample from Norway and their relation to established CVD risk factors. Secondary aims are to determine GLS normal thresholds in healthy individuals and the relation of myocardial GLS to SAHF.
Methods
Study population
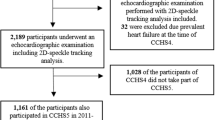
The Tromsø Study is a prospective cohort study, which was initiated in 1974 with the aim of assessing the role of known modifiable risk factors for CVD in Northern Norway and detection of new targets for prevention of CVD. The design of the study was described in previous publications [23]. Seven consecutive surveys have been conducted. Our study sample included 840 men and 1015 women from 7th survey in The Tromsø Study who underwent echocardiography and had myocardial GLS data (Fig. 1). We excluded those with missing values on risk factors (n = 108) leaving 1747 individuals aged 40–99 years for the main analyses.
Flowchart of the study participants. The Tromsø Study (2015–2016). aParticipants excluded from GLS analysis due to inappropriate imaging quality. bIndividuals with any of the following: left ventricle geometry abnormalities, left ventricle ejection fraction < 50%, severe valvular heart disease, history of myocardial infarction, heart failure or stroke. cMissing information on any of the following variables: myocardial infarction, angina, stroke, bronchitis, hypertension, diabetes, atrial fibrillation, heart failure, HbA1c, left ventricle ejection fraction. dIncluded those with the present at least one of the following: diabetes, metabolic syndrome, obesity, arterial hypertension, angina. eFive individuals with missing information were excluded from GLS analyses according to SBP groups. One individual excluded from logistic regression analysis
Data collection
Self-reported history of MI, HF, atrial fibrillation, angina, stroke, diabetes, chronic obstructive pulmonary disease was collected by questionnaires. Additionally, we included those who experienced atrial fibrillation during echocardiography as atrial fibrillation “positive” individuals. Participants with HbA1c ≥ 6.5% were treated as having diabetes regardless of self-reported status. Breathlessness was assessed by the modified UK Medical Research Council (mMRC) breathlessness/dyspnea scale [24].
Blood pressure (BP) was measured three times with 1-min intervals using an automated device Dinamap Pro care 300 Monitor (GE Medical Systems Information Technologies, Tampa, FL, USA). The mean of the last two readings was used in the analysis. Hypertension was defined as SBP ≥ 140 mm Hg, diastolic blood pressure (DBP) ≥ 90 mm Hg or self-reported use of antihypertensive medication. Metabolic syndrome was defined according to American Heart Association (AHA)/National Heart, Lung and Blood Institute statement [25].
Study groups definitions
Healthy persons were defined as those without known cardiovascular diseases and comorbidities. We excluded those with hypertension, diabetes, atrial fibrillation, HF, angina, MI, stroke, chronic obstructive pulmonary disease and ejection fraction of the left ventricle (LV EF) < 50% leaving a “healthy” subsample of 1068 individuals (Fig. 1). To assess the effect of increasing echocardiographic pathology by age we additionally excluded from the healthy subsample those with severe valve dysfunction, LV or left atrial (LA) enlargement or severe tricuspid regurgitation (> 2.8 m/s).
For defining the SAHF individuals we excluded subjects (n = 1146) with known CVD (previous history of MI, HF or stroke) and echocardiographic geometric LV abnormalities (Left ventricular myocardial mass index (LVMMi) > 50 in men and > 47 in women; relative LV wall thickness (rwt) > 0.42 or rwt ≤ 0.42 with LVMMi > 50 in men and > 47 in women), LV EF < 50%, and severe valve dysfunction (mitral and aortic stenosis and regurgitation ≥ grade 3) (Fig. 1). Thus, we identified a subset of 709 individuals who may include those with SAHF. In the American College of Cardiology Foundation/AHA guidelines guidelines [17], SAHF is defined as the presence of at least one of the following conditions: diabetes, metabolic syndrome, obesity, arterial hypertension or angina. Applying these criteria, we identified 220 individuals with SAHF (Fig. 1).
Echocardiography imaging
In The Tromsø 7 Study echocardiography was performed by a qualified sonographer using a GE Vivid E9 (GE Medical, Horten, Norway) ultrasound scanner. Offline image reading using EchoPac software (EchoPac version 113; GE Medical, Horten, Norway) was performed by one reader (MS).
Conventional echocardiography
Cineloops were recorded using standard 4-chamber, 2-chamber and long-axis apical views according to a prespecified protocol [26]. We obtained the images at a framerate of 50–70 frames per second. Ultrasound examinations were performed according to American Society of Echocardiography (ASE) and European Association of Cardiovascular Imaging (EACVI) guidelines [13] in the left lateral decubitus position. M-Mode images were aligned in the parasternal long axis view and recorded in the short axis view. LV myocardial mass was calculated according to ASE guidelines and indexed by height2.7 [13]. LVEF and LA volume were calculated using the biplane Simpson’s method. LA volume was indexed (LAVi) by body surface area (BSA) [27]. Mitral valve Doppler measurements were performed with a Doppler sample volume of 2-mm placed between the tip of the mitral leaflets in the apical 4-chamber view. We adjusted the spectral gain until the flow curves became clear [28]. The insonation angle for Doppler measurements was kept perpendicular toward the mitral inflow. Maximal velocity flow was measured in early diastole and after atrial p-wave.
Tissue Doppler parameters such as peak septal and lateral é were derived from apical 4-chamber view with 5-mm sample volume located at the septal and lateral side of the mitral annulus. Abnormal echo parameters considered as tricuspid regurgitation velocity > 2.8 m/s; LAVi > 34 ml/m2 [29].
Two-dimensional strain
Two-dimensional strain was analyzed according to EACVI/ASE common standards for 2D speckle tracking echocardiography [30]. The endo- and epicardial borders were initially traced with the use of automated function imaging. Myocardial GLS values were obtained from averaging of endo- mid- and epicardial layer’s GLS values from three apical views based on 17-segment model. Images were checked visually for clear visibility of the endo- and epicardial borders during the entire cardiac cycle. Attention was paid to accurate placement of region of interest (ROI) with the aim of avoiding inclusion of extracardiac structures. Furthermore, we paid attention not to include papillary muscles in contour of LV or the fibrous part of the basal inferoseptum or LV outflow tract [31]. ROI was visually assessed and manually adjusted in case of inappropriate tracking. Views with more than two segments with inappropriate tracking were excluded from the analysis.
Statistical methods
The study population included individuals aged from 40 to 99 years divided in 10-year age groups. Baseline characteristics of the study participants were described with the use of means with standard deviations and proportions. For analyses of associations between myocardial GLS and SBP we divided study population by the following SBP groups: < 120, 120–129, 130–139, 140–159, 160–169, 170–179 and ≥ 180 mm Hg.
According to the sex-specific SBP groups, means for myocardial GLS were adjusted for age using linear regression analysis. Absolute means were tabulated for those aged 63 years. Comparisons between groups were performed by analysis of variance (ANOVA), χ2 test and Fisher’s exact test. For analysis of GLS change by age we used weighted linear regression. The “Weight” variable for regression equation was estimated from number of individuals in each age group. Lower limit of normal (LLN) myocardial GLS for “healthy” subpopulation was defined as absolute mean GLS minus 1.96*standard deviation. Bootstrapping with 1000 samples was used to define upper 97.5th and lower 2.5th percentiles for LLN with confidence intervals [32]. We used quantile regression for estimation of the p value for trend of LLN change by age. Logistic regression models were applied to estimate odds ratios (OR) for different risk factors of myocardial GLS below age and sex-specific LLN (abnormal GLS). The OR for each of the following predictors (BMI, history of: MI, atrial fibrillation, angina, diabetes, stroke, arterial hypertension and breathlessness scale) were estimated separately.
Intra- and inter-reader variability of myocardial GLS was assessed in recordings of 27 of 30 randomly selected participants. Three individuals were excluded due to inappropriate image quality. Intra-reader variability was assessed in repeated GLS measurements by one reader (M.S) with 3-months intervals. To assure external validity of measurements as well as internal inter-reader variability was assessed with two readers (M.S. and A.R and presented as intra-class correlation coefficients (ICC) and mean difference ± SD. Coefficient of repeatability (CR) was calculated using the formula 2.77*SDw with SDw as the within-subject standard deviation. Visual assessment of inter-observer variability was performed with use of a Bland–Altman plot.
A two-sided p < 0.05 was considered statistically significant. Statistical analyses were performed using SAS statistical package, version 9.4 (SAS Institute, Cary, NC, USA).
Results
Descriptive characteristics
The descriptive echocardiographic and clinical characteristics of the study population are presented in 10-year age groups (Table 1). Study sample included 840 (45.3%) men and 1015 (54.7%) women. The prevalence of self-reported pathology increased across the entire age range except for MI, diabetes and angina pectoris which have the highest prevalence in 70–79 years individuals. Of the echocardiographic characteristics: LVMMi, LAVi, Mitral E-wave deceleration time (DT), E/e′ ratio showed a linear relation to age, while LVEF and E/A ratio did not.
Myocardial GLS in The Tromsø 7 Study
In our general population sample, mean myocardial GLS declined with age in both men and women (Fig. 2).
Age and sex-specific myocardial GLS means with 95% CI bands in general and healthy subsamples (n = 1747). The Tromsø Study (2015–2016). For “General” subsample: p-value (Difference between men and women by age groups): 40–49: p < 0.001; 50–59: p < 0.001; 60–69: p < 0.001; 70–79: p < 0.001; 80 + : p < 0.001. p-value (for change of mean myocardial GLS by age) Men: p < 0.001; Women: p < 0.001. Numbers for men and women: 40–49 (M99; W144) 50-59 (M144; W188) 60–69 (M314; W345) 70–79 (M200; W225); 80 + (M39; W49); Total n = 1747. For “Healthy” subsample: p-value (difference between men and women by age groups) 40–49: p < 0.001; 50–59: p < 0.001; 60–69: p < 0.001; 70–79: p = 0.009; 80 + : p = 0.115. p-value (for change of mean myocardial GLS by age) Men: p = 0.001; Women: p < 0.001. Numbers for healthy: 40–49 (M81; W119); 50–59 (M109; W155); 60–69 (M170; W230); 70–79 (M72; W98); 80 + (M19; W15); Total n = 1068. GLS global longitudinal strain, CI confidence interval
Myocardial GLS of the healthy participants
The prevalence of healthy individuals by age from The Tromsø 7 Study sample according to the healthy/unhealthy criteria is presented in Table 2. We found that the prevalence of healthy women was stable between 40 and 59 with a decline after 60 years of age (p for change of healthy proportions by age < 0.001). In men the decrease of healthy individuals starts earlier than in women but then follows the same slope by age (p < 0.001). There was no interaction between age group and sex (p = 0.457).
Mean myocardial GLS (SD) in healthy participants (n = 1068) was − 15.9 (2.7) % in men (n = 451) and − 17.8 (3.1) % in women (n = 617). Figure 2 describes mean levels of myocardial GLS in healthy participants according to age and sex. Healthy women had higher values of myocardial GLS than men in all age groups. Significant change of mean myocardial GLS by age was observed for both sexes (p = 0.001 and < 0.001 in men and women respectively). In the healthy subgroup without echo abnormalities the age effect on GLS was no longer significant in men (p-value for men 0.179, for women < 0.001).
The comparison of GLS in healthy versus unhealthy individuals is demonstrated in Online Resources 2 (for men) and 3 (for women) as well as the numbers of individuals with measured myocardial GLS (Online Resource 4).
Abnormal myocardial GLS in The Tromsø 7 Study sample
With the use of mean myocardial GLS values in the healthy individuals aged 40–99 years, myocardial GLS LLN equaled − 10.6% for men and − 11.7% for women. Data shown in Table 3 estimates LLN with bootstrapped 2.5th and 97.5th CI by age groups and sex. A tendency of declining LLN with the age was still present in both men and women, however the differences were non-significant (p-values for age trend were 0.522 and 0.801 for men and women respectively).
Abnormal myocardial GLS and risk factors
We estimated OR for factors possibly associated with abnormal myocardial GLS (Table 4). Individuals with diabetes had 2.91-fold (95% CI 1.52, 5.55) increased risk of having abnormal myocardial GLS. All other predictors had significant effect on abnormal GLS excluding hypertension and mMRC scale ≥ 2. Table 5 shows the difference in GLS for each of the significant predictors of GLS. The lowest myocardial GLS (SD) of − 14.3 (3.5) % was found in individuals with self-reported HF.
Myocardial GLS and SBP
Myocardial GLS in women declines as SBP increase (Fig. 3). In men with and without antihypertensive treatment differences in myocardial GLS between SBP groups were non-significant (p = 0.206 and p = 0.276 for untreated and treated men respectively). Men and women with BP treatment had lower values of myocardial GLS than those without treatment. In linear regression analysis adjusted for age and sex, 10 mm Hg increase of SBP resulted in a 0.2% decrease of myocardial GLS (β = 0.235; p < 0.001). After adjustment for age, sex, BMI, history of: MI, atrial fibrillation, angina, diabetes, stroke, arterial hypertension and breathlessness scale, SBP remained an independent predictor of myocardial GLS decline (β = 0.146; p < 0.001).
Mean myocardial GLS levels stratified by SBP, sex and antihypertensive treatment. The Tromsø Study (2015–2016). Means are adjusted for age and estimated for a mean age of 63 years using linear regression. p-value between SBP groups: Men (Untreated) = 0.206; Women (Untreated) < 0.001; Men (Treated) = 0.276; Women (Treated) = 0.898. SBP systolic blood pressure; GLS global longitudinal strain, SD standard deviation
Subclinical HF and myocardial GLS
In the subgroup without LV echocardiographic abnormalities (total n = 709), 120 (29.1%) of women and 100 (33.8%) of men were categorized as SAHF individuals. Mean myocardial GLS (SD) (n) in those with SAHF were − 16.7 (2.5) % (n = 220) and − 17.9 (2.6) % (n = 489) in participants without SAHF (p < 0.001). In the SAHF positive group 3.2% reported dyspnea by exertion (mMRC scale ≥ 2, versus 1.6% in individuals without SAHF (p = 0.257).
Inter-observer variability of GLS
We benchmarked the single reader (MS) against another clinical echocardiographist (AR) who had extensive experience of routine measurement of myocardial GLS. Analyses of myocardial GLS reproducibility (Online Resource 1) and Bland–Altman plots visual assessment (Fig. 4) showed good to excellent intra- and inter-observer agreement levels.
Bland-Altman plot for inter-observer study. The Tromsø 7 Study. Difference in GLS: difference between observer AR and observer MS measurements (AR minus MS); bMean GLS: mean GLS of two observers AR and MS; SD: standard deviation; GLS: Global longitudinal strain; AR: observer 1; MS: observer 2. *P-value for linear regression model [y (difference in GLS) = × (mean GLS)] = 0.408
Discussion
This is the first study to our knowledge to explore GLS patterns and its associations to CVD risk factors and SAHF in a general population. The main results of this study were the following: (1) mean GLS in healthy participants aged 40–99 years was − 15.9 (2.7) % in men and − 17.8 (3.1) % in women with significant change of GLS by age in both sexes; (2) GLS LLN was estimated as − 10.6% for men and − 11.7% for women aged 40–99 years; (3) GLS declines in women with increase of SBP; (4) Increase of SBP by 10 mm Hg results in 0.2% GLS reduction in age and sex adjusted regression model; (5) Myocardial GLS in individuals with SAHF was 1.2% lower (p < 0.001) than in participants without SAHF.
Myocardial GLS in general population
Our findings of a decline in myocardial GLS with age confirmed previous studies describing the same age and sex related myocardial GLS patterns [15, 33]. However, there was a number of controversial reports with no detected myocardial GLS age change in general or healthy samples [34,35,36]. Additionally, we found that change in myocardial GLS by age disappears in men when individuals with echo abnormalities were excluded from the “healthy” subgroup.
Mean myocardial GLS ± SD values derived from averaging of endo- mid- and epicardial layer’s GLS values in healthy participants in The Tromsø 7 Study sample were similar to those published in Dalen et al. work (− 15.9 ± 2.3% in men and − 17.4 ± 2.3% in women) based on data of 1266 healthy individuals participated in HUNT study of Norway [37]. However, other authors found significantly higher absolute values of mean myocardial GLS in healthy subjects. One of the possible reasons of different GLS values found in healthy individuals among the studies is the use of the different myocardial layers (endo- midwall or epicardial layer) for calculating the GLS since recent reports show endocardial GLS approximately 30% higher than epicardial GLS [35]. In the guidelines GLS level of − 20% is considered as the borderline in healthy subjects [13]. Guideline based GLS LLN values by vendor (GE Software) were higher than values we found. It is also important that myocardial GLS values of our study were derived using EchoPac version (EchoPac ver. 113) which was newer than these listed in the guidelines [13]. Castel et al. reported that upgrades of speckle tracking software were associated with significant changes in GLS values [38]. It is worth to mention that sample sizes in HUNT and Tromsø studies were much larger than in the other studies. Thus, Alcidi et al. reported myocardial GLS ± SD level of − 22.7 ± 1.8% in a sample of 266 healthy individuals [15]. The authors found significant change of myocardial GLS by age even though the participants age (mean ± SD) was 39.2 ± 17.5 years compared with 63.0 ± 10.8 in Tromsø 7 population sample.
Taking into the account the small sample size of “healthy” individuals in higher age groups, we assessed bootstrapped 95% CI for myocardial GLS LLN. We found no significant change of LLN by age neither in men nor women.
Our results indicate that subclinical myocardial dysfunction assessment should not be limited to considering hypertension alone, as myocardial GLS is influenced by other comorbidities and risk factors as well. We found that BMI was associated with presence of myocardial GLS below LLN. It was consistent with previous research of Bendiab et al. [39] where most of the risk factors were inversely correlated with myocardial GLS. The BMI has been described as an independent factor for low myocardial GLS, previously [39]. However, the associations between myocardial GLS and self-reported dyspnea symptoms are more complicated. Relatively low myocardial GLS (SD) − 14.8 (3.5) % in those with mMRC scale ≥ 2 can be explained by the characteristics of the selected sample and association of abnormal myocardial GLS with diastolic dysfunction and LV filling pressures [40]. Another explanation of the low myocardial GLS levels in patients with dyspnea could be the unrecognized systolic dysfunction which prevalence according to earlier reports reaches 15.7% (95% CI 12.9–19.0) in individuals aged 65 years or older [41].
Myocardial GLS and BP
In our study we tried to expand the current knowledge about factors contributing to myocardial GLS decline. SBP was chosen as such as a factor due to its known association to myocardial GLS in different patient groups [16] and the high prevalence of arterial hypertension worldwide. Another important aspect is that myocardial GLS decline in hypertensives reflects subclinical damage of LV structure and function due to early microscarring of the subendocardium, especially in the highly hypertrophied muscles [42]. Furthermore, increased afterload is known to prolong contraction and delay active relaxation [43] and reduce longitudinal strain and strain-rate [44].
We have found mean myocardial GLS decline up to − 15.9% in patients with arterial hypertension. This value was higher than GLS LLN in both men and women with the significant difference with those without arterial hypertension (GLS = − 16.6%, p < 0.001). Adjusted for age and sex 10 mm Hg SBP increase was responsible for 0.2% of myocardial GLS decrease. This confirmed the association between SBP and myocardial GLS found in earlier studies [39].
We assessed the sex-related LV function in hypertensive individuals. Previous reports have found contradicting results [45]. We found that in women myocardial GLS declined from − 18.4% in SBP group of < 120 mm Hg to − 17.1% in those within SBP > 180 mm Hg (p < 0.001). We revealed a similar decline among men, however without significant difference between SBP groups. Presumable cause could be the small number of men with the highest SBP levels (only 9 persons in the SBP > 180 mm Hg group). Mean myocardial GLS was lower in the high-normal SBP group of 130–139 mm Hg compare to normal SBP groups in both men and women, showing that longitudinal function of LV was already impaired in these groups of study participants. The previous report by Tadic et al. showed that myocardial GLS was lower in high-normal BP individuals with no such BP effect on radial LV function [46]. We revealed that women have larger values of myocardial GLS in both healthy individuals as well as in those with CVD risk factors. Partly it could be explained by pathophysiological diversities between men and women reflected in complex relationships between LV mechanics and sex hormones. Thus, Salem et al. showed that higher levels of testosterone in men were associated with decreased myocardial GLS [47].
It is worth to mention that hypertensive individuals are characterized by increased afterload which leads to thickening of the LV wall and LV hypertrophy development [48] as a compensatory mechanism. Some studies demonstrated that decreased longitudinal systolic function cannot be attributed to the afterload increase in patients with arterial hypertension and LV hypertrophy [49], which might be due to low effect of increased blood-pressure on the compensatory hypertrophied ventricle, where the smaller ventricle and thicker walls lead to reduced wall stress. Kim at al. in a study of 145 hypertensive patients [11] showed that different ventricular regions have different susceptibility for stress induced afterload with inhomogeneous development of ventricular hypertrophy. Myocardial GLS has been shown to be lower in ventricular regions with more pronounced LV hypertrophy. Concerning the fact that in our study sample individuals with 70 + years of age had mean LVMMi > 47 g/m2.7, we assume that arterial hypertension exerts its negative influence on myocardial GLS through microscarring and insufficient myocardial perfusion in LV hypertrophy.
Myocardial GLS and SAHF
Identification of individuals with SAHF who are at risk of developing advanced HF stages appears to be a promising CVD primary prevention strategy. In most of the cases patients without symptoms are rarely involved in screening procedures until development of later HF stages. In our study we found that mean GLS (SD) in individuals with SAHF − 16.7 (2.5) % was lower compared to those without − 17.9 (2.6)% (p < 0.001). The components defining SAHF (elevated SBP, diabetes, obesity or atherosclerosis) were found to be associated with abnormal GLS, possibly indicating the presence of subclinical damage of the myocardium [20, 21]. It is worth to mention that myocardial GLS may have benefits in early HF detection because symptoms of HF are not always present in even more advanced HF stages (Stage B HF). Thus, Redfield et al. reported that 14% of patients with dilated cardiomyopathy and LVEF < 50% had never experienced any of HF symptoms [50].
Myocardial GLS and vendor-specific software
Different vendor-specific image postprocessing algorithms were earlier considered as an issue which could potentially limit clinical use of the strain imaging [51]. However, launching of EACVI/ASE Strain Standardization Task Force [30] resulted in increased number of evidence on improvement of concordance in strain imaging between vendors [52]. Yingchoncharoen et al. reported no significant difference of GLS variability in healthy individuals between EchoPac and non-EchoPac software (p = 0.98) [16]. Based on these findings we assume that values of myocardial GLS in healthy population of our study is valid not only for EchoPac but also for another vendor’s software.
Strengths and limitations
This is a large population-based study with a large age range providing a good power to estimate the normal range of normal strain values. Strain is reduced with increasing afterload. Possible use of afterload adjustment for example, indexing myocardial GLS to the population-based average BP may solve the issue, however data on SBP and DBP during echo examination in The Tromsø 7 Study is lacking. Single center study design could be a possible source of reduced validity of the findings. Another limitation is the low sample size above 80 years of age. Data on use of cardiotoxic drugs is not available in The Tromsø Study and accordingly not included as risk factor in SAHF definition.
Clinical implications
The results we demonstrated could potentially be used in control of the patients with SAHF with help of GLS monitoring over time. Age-related GLS LLN is a promising parameter for clinical follow-up in group of patients with subclinical HF due to its sensitivity for early myocardial function impairment.
Conclusions
In large unselected samples from the general population myocardial GLS values were found both in the total and healthy subsamples. Mean myocardial GLS declined with age in both sexes in general and in healthy participants. SBP increase was associated with GLS decline in women. GLS was decreased in subjects with subclinical HF. The close association of GLS to SAHF parameters indicates its importance for subclinical heart disease diagnostics.
References
Cardiovascular diseases (CVDs) WHO fact sheet (2017) http://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
Krishnasamy R, Isbel NM, Hawley CM, Pascoe EM, Burrage M, Leano R, Haluska BA, Marwick TH, Stanton T (2015) Left ventricular global longitudinal strain (GLS) is a superior predictor of all-cause and cardiovascular mortality when compared to ejection fraction in advanced chronic kidney disease. PLoS ONE 10(5):e0127044. https://doi.org/10.1371/journal.pone.0127044
Sengelov M, Jorgensen PG, Jensen JS, Bruun NE, Olsen FJ, Fritz-Hansen T, Nochioka K, Biering-Sorensen T (2015) Global longitudinal strain is a superior predictor of all-cause mortality in heart failure with reduced ejection fraction. JACC Cardiovasc Imaging 8(12):1351–1359. https://doi.org/10.1016/j.jcmg.2015.07.013
Modin D, Sengelov M, Jorgensen PG, Bruun NE, Olsen FJ, Dons M, Fritz Hansen T, Jensen JS, Biering-Sorensen T (2018) Global longitudinal strain corrected by RR interval is a superior predictor of all-cause mortality in patients with systolic heart failure and atrial fibrillation. ESC Heart Fail 5(2):311–318. https://doi.org/10.1002/ehf2.12220
Bendary A, Tawfeek W, Mahros M, Salem M (2018) The predictive value of global longitudinal strain on clinical outcome in patients with ST-segment elevation myocardial infarction and preserved systolic function. Echocardiography 35(7):915–921. https://doi.org/10.1111/echo.13866
Lauridsen TK, Alhede C, Crowley AL, Kisslo J, Sorensen LL, Hansen TF, Risum N, Larsen CT, Hassager C, Sogaard P, Dahl A, Bruun NE (2018) Two-dimensional global longitudinal strain is superior to left ventricular ejection fraction in prediction of outcome in patients with left-sided infective endocarditis. Int J Cardiol 260:118–123. https://doi.org/10.1016/j.ijcard.2018.01.031
Kearney LG, Lu K, Ord M, Patel SK, Profitis K, Matalanis G, Burrell LM, Srivastava PM (2012) Global longitudinal strain is a strong independent predictor of all-cause mortality in patients with aortic stenosis. Eur Heart J Cardiovasc Imaging 13(10):827–833. https://doi.org/10.1093/ehjci/jes115
Hiemstra YL, Debonnaire P, Bootsma M, van Zwet EW, Delgado V, Schalij MJ, Atsma DE, Bax JJ, Marsan NA (2017) Global longitudinal strain and left atrial volume index provide incremental prognostic value in patients with hypertrophic cardiomyopathy. Circ Cardiovasc Imaging. https://doi.org/10.1161/circimaging.116.005706
Olsen FJ, Jorgensen PG, Mogelvang R, Jensen JS, Fritz-Hansen T, Bech J, Biering-Sorensen T (2016) Predicting paroxysmal atrial fibrillation in cerebrovascular ischemia using tissue doppler imaging and speckle tracking echocardiography. J Stroke Cerebrovasc Dis 25(2):350–359. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.10.004
Biering-Sorensen T, Biering-Sorensen SR, Olsen FJ, Sengelov M, Jorgensen PG, Mogelvang R, Shah AM, Jensen JS (2017) Global longitudinal strain by echocardiography predicts long-term risk of cardiovascular morbidity and mortality in a low-risk general population: the copenhagen city heart study. Circ Cardiovasc Imaging. https://doi.org/10.1161/circimaging.116.005521
Kim SA, Park SM, Kim MN, Shim WJ (2016) Assessment of left ventricular function by layer-specific strain and its relationship to structural remodelling in patients with hypertension. Can J Cardiol 32(2):211–216. https://doi.org/10.1016/j.cjca.2015.04.025
Kuznetsova T, Nijs E, Cauwenberghs N, Knez J, Thijs L, Haddad F, Yang WY, Kerkhof PL, Voigt JU, Staessen JA (2019) Temporal changes in left ventricular longitudinal strain in general population: clinical correlates and impact on cardiac remodeling. Echocardiography 36(3):458–468. https://doi.org/10.1111/echo.14246
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt J-U (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–270
Galderisi M, Cosyns B, Edvardsen T, Cardim N, Delgado V, Di Salvo G, Donal E, Sade LE, Ernande L, Garbi M, Grapsa J, Hagendorff A, Kamp O, Magne J, Santoro C, Stefanidis A, Lancellotti P, Popescu B, Habib G, Committee ESD, Committee ESD (2017) Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: an expert consensus document of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 18(12):1301–1310. https://doi.org/10.1093/ehjci/jex244
Alcidi GM, Esposito R, Evola V, Santoro C, Lembo M, Sorrentino R, Lo Iudice F, Borgia F, Novo G, Trimarco B, Lancellotti P, Galderisi M (2017) Normal reference values of multilayer longitudinal strain according to age decades in a healthy population: a single-centre experience. Eur Heart J Cardiovasc Imaging. https://doi.org/10.1093/ehjci/jex306
Yingchoncharoen T, Agarwal S, Popovic ZB, Marwick TH (2013) Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr 26(2):185–191. https://doi.org/10.1016/j.echo.2012.10.008
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL, American College of Cardiology F, American Heart Association Task Force on Practice G (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol 62(16):e147–e239. https://doi.org/10.1016/j.jacc.2013.05.019
Ammar KA, Jacobsen SJ, Mahoney DW, Kors JA, Redfield MM, Burnett JC Jr, Rodeheffer RJ (2007) Prevalence and prognostic significance of heart failure stages: application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. Circulation 115(12):1563–1570. https://doi.org/10.1161/CIRCULATIONAHA.106.666818
Yang H, Negishi K, Wang Y, Nolan M, Marwick TH (2017) Imaging-guided cardioprotective treatment in a community elderly population of stage B heart failure. JACC Cardiovasc Imaging 10(3):217–226. https://doi.org/10.1016/j.jcmg.2016.11.015
Chen XJ, Sun XL, Zhang Q, Gao XL, Liang YJ, Jiang J, Kang Y, Chen YC, Zeng Z, Yu CM (2016) Uncontrolled blood pressure as an independent risk factor of early impaired left ventricular systolic function in treated hypertension. Echocardiography 33(10):1488–1494. https://doi.org/10.1111/echo.13289
Holland DJ, Marwick TH, Haluska BA, Leano R, Hordern MD, Hare JL, Fang ZY, Prins JB, Stanton T (2015) Subclinical LV dysfunction and 10-year outcomes in type 2 diabetes mellitus. Heart 101(13):1061–1066. https://doi.org/10.1136/heartjnl-2014-307391
Ho JE, McCabe EL, Wang TJ, Larson MG, Levy D, Tsao C, Aragam J, Mitchell GF, Benjamin EJ, Vasan RS, Cheng S (2017) Cardiometabolic traits and systolic mechanics in the community. Circ Heart Fail. https://doi.org/10.1161/circheartfailure.116.003536
Jacobsen BK, Eggen AE, Mathiesen EB, Wilsgaard T, Njolstad I (2012) Cohort profile: the Tromso study. Int J Epidemiol 41(4):961–967. https://doi.org/10.1093/ije/dyr049
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F, American Heart A, National Heart L, Blood I (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 112(17):2735–2752. https://doi.org/10.1161/CIRCULATIONAHA.105.169404
Cook S, Malyutina S, Kudryavtsev AV, Averina M, Bobrova N, Boytsov S, Brage S, Clark TG, Diez Benavente E, Eggen AE, Hopstock LA, Hughes A, Johansen H, Kholmatova K, Kichigina A, Kontsevaya A, Kornev M, Leong D, Magnus P, Mathiesen E, McKee M, Morgan K, Nilssen O, Plakhov I, Quint JK, Rapala A, Ryabikov A, Saburova L, Schirmer H, Shapkina M, Shiekh S, Shkolnikov VM, Stylidis M, Voevoda M, Westgate K, Leon DA (2018) Know your heart: rationale, design and conduct of a cross-sectional study of cardiovascular structure, function and risk factors in 4500 men and women aged 35–69 years from two Russian cities, 2015–18. Wellcome Open Res 3:67. https://doi.org/10.12688/wellcomeopenres.14619.3
Du Bois D, Du Bois EF (1989) A formula to estimate the approximate surface area if height and weight be known 1916. Nutrition 5(5):303–311 discussion 312–303
Appleton CP, Jensen JL, Hatle LK, Oh JK (1997) Doppler evaluation of left and right ventricular diastolic function: a technical guide for obtaining optimal flow velocity recordings. J Am Soc Echocardiogr 10(3):271–292
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu BA, Waggoner AD (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the american society of echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29(4):277–314. https://doi.org/10.1016/j.echo.2016.01.011
Voigt JU, Pedrizzetti G, Lysyansky P, Marwick TH, Houle H, Baumann R, Pedri S, Ito Y, Abe Y, Metz S, Song JH, Hamilton J, Sengupta PP, Kolias TJ, d’Hooge J, Aurigemma GP, Thomas JD, Badano LP (2015) Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 16(1):1–11. https://doi.org/10.1093/ehjci/jeu184
Negishi K, Negishi T, Kurosawa K, Hristova K, Popescu BA, Vinereanu D, Yuda S, Marwick TH (2015) Practical guidance in echocardiographic assessment of global longitudinal strain. JACC Cardiovasc Imaging 8(4):489–492. https://doi.org/10.1016/j.jcmg.2014.06.013
Wood M (2005) Bootstrapped confidence intervals as an approach to statistical inference. Organ Res Methods 8(4):454–470. https://doi.org/10.1177/1094428105280059
Kleijn SA, Pandian NG, Thomas JD, Perez de Isla L, Kamp O, Zuber M, Nihoyannopoulos P, Forster T, Nesser HJ, Geibel A, Gorissen W, Zamorano JL (2015) Normal reference values of left ventricular strain using three-dimensional speckle tracking echocardiography: results from a multicentre study. Eur Heart J Cardiovasc Imaging 16(4):410–416. https://doi.org/10.1093/ehjci/jeu213
Shi J, Pan C, Kong D, Cheng L, Shu X (2016) Left ventricular longitudinal and circumferential layer-specific myocardial strains and their determinants in healthy subjects. Echocardiography 33(4):510–518. https://doi.org/10.1111/echo.13132
Nagata Y, Wu VC, Otsuji Y, Takeuchi M (2017) Normal range of myocardial layer-specific strain using two-dimensional speckle tracking echocardiography. PLoS ONE 12(6):e0180584. https://doi.org/10.1371/journal.pone.0180584
Kocabay G, Muraru D, Peluso D, Cucchini U, Mihaila S, Padayattil-Jose S, Gentian D, Iliceto S, Vinereanu D, Badano LP (2014) Normal left ventricular mechanics by two-dimensional speckle-tracking echocardiography. Reference values in healthy adults. Rev Esp Cardiol 67(8):651–658. https://doi.org/10.1016/j.rec.2013.12.009
van Dalen BM, Kauer F, Vletter WB, Soliman OI, van der Zwaan HB, Ten Cate FJ (1985) Geleijnse ML (2010) Influence of cardiac shape on left ventricular twist. J Appl Physiol 108(1):146–151. https://doi.org/10.1152/japplphysiol.00419.2009
Castel AL, Menet A, Ennezat PV, Delelis F, Le Goffic C, Binda C, Guerbaai RA, Levy F, Graux P, Tribouilloy C, Marechaux S (2016) Global longitudinal strain software upgrade: implications for intervendor consistency and longitudinal imaging studies. Arch Cardiovasc Dis 109(1):22–30. https://doi.org/10.1016/j.acvd.2015.08.006
Bendiab NST, Meziane-Tani A, Ouabdesselam S, Methia N, Latreche S, Henaoui L, Monsuez JJ, Benkhedda S (2017) Factors associated with global longitudinal strain decline in hypertensive patients with normal left ventricular ejection fraction. Eur J Prev Cardiol 24(14):1463–1472. https://doi.org/10.1177/2047487317721644
DeVore AD, McNulty S, Alenezi F, Ersboll M, Vader JM, Oh JK, Lin G, Redfield MM, Lewis G, Semigran MJ, Anstrom KJ, Hernandez AF, Velazquez EJ (2017) Impaired left ventricular global longitudinal strain in patients with heart failure with preserved ejection fraction: insights from the RELAX trial. Eur J Heart Fail 19(7):893–900. https://doi.org/10.1002/ejhf.754
van Riet EE, Hoes AW, Limburg A, Landman MA, van der Hoeven H, Rutten FH (2014) Prevalence of unrecognized heart failure in older persons with shortness of breath on exertion. Eur J Heart Fail 16(7):772–777. https://doi.org/10.1002/ejhf.110
Cameli M, Mandoli GE, Lisi E, Ibrahim A, Incampo E, Buccoliero G, Rizzo C, Devito F, Ciccone MM, Mondillo S (2019) Left atrial, ventricular and atrio-ventricular strain in patients with subclinical heart dysfunction. Int J Cardiovasc Imaging 35(2):249–258. https://doi.org/10.1007/s10554-018-1461-7
Leite S, Rodrigues S, Tavares-Silva M, Oliveira-Pinto J, Alaa M, Abdellatif M, Fontoura D, Falcao-Pires I, Gillebert TC, Leite-Moreira AF, Lourenco AP (2015) Afterload-induced diastolic dysfunction contributes to high filling pressures in experimental heart failure with preserved ejection fraction. Am J Physiol Heart Circ Physiol 309(10):H1648–H1654. https://doi.org/10.1152/ajpheart.00397.2015
Rosner A, Bijnens B, Hansen M, How OJ, Aarsaether E, Muller S, Sutherland GR, Myrmel T (2009) Left ventricular size determines tissue Doppler-derived longitudinal strain and strain rate. Eur J Echocardiogr 10(2):271–277. https://doi.org/10.1093/ejechocard/jen230
Tadic M, Cuspidi C, Celic V, Ivanovic B, Pencic B, Grassi G (2019) The influence of sex on left ventricular strain in hypertensive population. J Hypertens 37(1):50–56. https://doi.org/10.1097/HJH.0000000000001838
Tadic M, Cuspidi C, Backovic S, Kleut M, Ivanovic B, Scepanovic R, Iracek O, Celic V (2014) High-normal blood pressure, functional capacity and left heart mechanics: is there any connection? Blood Press 23(5):315–321. https://doi.org/10.3109/08037051.2014.907978
Salem JE, Nguyen LS, Hammoudi N, Preud’homme G, Hulot JS, Leban M, Funck-Brentano C, Touraine P, Isnard R, Bachelot A, Group CS (2018) Complex association of sex hormones on left ventricular systolic function: insight into sexual dimorphism. J Am Soc Echocardiogr 31(2):231–240. https://doi.org/10.1016/j.echo.2017.10.017
Mayet J, Hughes A (2003) Cardiac and vascular pathophysiology in hypertension. Heart 89(9):1104–1109. https://doi.org/10.1136/heart.89.9.1104
Narayanan A, Aurigemma GP, Chinali M, Hill JC, Meyer TE, Tighe DA (2009) Cardiac mechanics in mild hypertensive heart disease: a speckle-strain imaging study. Circ Cardiovasc Imaging 2(5):382–390. https://doi.org/10.1161/CIRCIMAGING.108.811620
Redfield MM, Gersh BJ, Bailey KR, Rodeheffer RJ (1994) Natural history of incidentally discovered, asymptomatic idiopathic dilated cardiomyopathy. Am J Cardiol 74(7):737–739. https://doi.org/10.1016/0002-9149(94)90323-9
Takigiku K, Takeuchi M, Izumi C, Yuda S, Sakata K, Ohte N, Tanabe K, Nakatani S, investigators J (2012) Normal range of left ventricular 2-dimensional strain: Japanese Ultrasound Speckle Tracking of the Left Ventricle (JUSTICE) study. Circ J 76(11):2623–2632. https://doi.org/10.1253/circj.cj-12-0264
Yang H, Marwick TH, Fukuda N, Oe H, Saito M, Thomas JD, Negishi K (2015) Improvement in strain concordance between two major vendors after the strain standardization initiative. J Am Soc Echocardiogr 28(6):642–648. https://doi.org/10.1016/j.echo.2014.12.009
Acknowledgements
Current study was supported by UiT-The Arctic University of Norway, Tromsø.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have conflict of interest.
Ethical approval
The Tromsø Study protocol was approved by the Regional Committee for Medical and Health Research Ethics, North Norway (2014/940/REK Nord) and was performed according ethical standards outlined in the 1964 Declaration of Helsinki.
Informed consent
All participants of the study provided signed informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Stylidis, M., Leon, D.A., Rӧsner, A. et al. Global myocardial longitudinal strain in a general population—associations with blood pressure and subclinical heart failure: The Tromsø Study. Int J Cardiovasc Imaging 36, 459–470 (2020). https://doi.org/10.1007/s10554-019-01741-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01741-3