Abstract
Objective
The aim of our study was to evaluate the level of agreement between tricuspid annular plane systolic excursion (TAPSE) measured by transthoracic echocardiography (TTE) and TAPSE measured using transesophageal echocardiography (TEE) in anesthetized patients.
Materials and methods
Thirty patients scheduled for elective cardiac surgery were prospectively studied. Shortly after induction of anesthesia before the operation, TAPSE was measured by TTE using M-mode in apical 4chamber view (4CH) and by TEE in six different views: using 2D echocardiography in midesophageal (ME) 4CH view, using M-mode in deep transgastric right ventricle (dTG RV) view at 0° and dTG RV longaxis view (LAX) as well as using anatomical M-mode (AM-mode) in ME 4CH, dTG RV at 0° and dTG RV LAX views.
Results
Bland–Altman analysis showed a good agreement for TAPSE measured using M-mode in TTE and using AM-mode in TEE in the ME 4CH and dTG RV at 0° views (−2.5 ± 18 and −2.2 ± 14% respectively). The agreement between TAPSE measured in TTE and TEE using 2D in ME 4CH, using M-mode in dT GRV 0° and using M-mode and AM-mode in dTG RV LAX view showed a significant systematic underestimation of the measurements (−8.8 ± 21, −8.8 ± 24, −17.8 ± 28 and −6.4 ± 20%).
Conclusion
Our study showed that the right ventricular function can be accurately and precisely estimated using TAPSE measurement by TEE in the midesophageal four chamber and deep transgastric right ventricle view at 0° using anatomical M-mode.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The undeniable importance of right ventricular (RV) dysfunction in the process of cardiopulmonary bypass weaning and its negative prognostic impact on cardiac surgical outcome [1–4], calls for an accurate evaluation of RV function in the perioperative setting using transesophageal echocardiography (TEE).
The widespread use of TEE in the operating room, allows for the evaluation of RV function, but considering the complex shape of the RV chamber that makes the accurate evaluation of the RV ejection fraction (EF) using geometric models difficult, it is not uncommon to use qualitative visual assessment. Therefore there is a rising demand for the application of quantitative methods to assess RV function in the intraoperative period.
Tricuspid annular plane systolic excursion (TAPSE) is one of the recommended methods for the quantitative assessment of RV function [5, 6]. It measures the longitudinal systolic displacement of the base of RV free wall towards the apex, which is assumed to represent the global right ventricular function [7]. Indeed, most of the RV muscular fibers lie in a base-to-apex direction and RV ejection relies more on its longitudinal shortening rather than the transverse shortening [8–10].
The standard method of measuring TAPSE is M-mode of the lateral RV wall in the apical 4-chamber (4CH) view in transthoracic echocardiography (TTE) by placing the M-mode line at the junction of the tricuspid valve annulus and the RV free wall. The most important limitation of this method is its angle dependence [5, 7].
The midesophageal 4-chamber (ME 4CH) view in TEE is a less suitable view to measure TAPSE using M-mode because here the M-mode line is almost perpendicular to the lateral aspect of the tricuspid annulus, which makes the acquisition of M-mode impossible.
There are different methods to overcome the flaw of TEE in measuring TAPSE. It has been recommended to use the 2-D ME 4CH view to evaluate TAPSE by measuring the difference between systolic and diastolic distances of the lateral tricuspid annulus to the right ventricular apex [11].
Anatomical M-mode (AM-mode) with its characteristic steerable line can be used if available to adjust the cursor freely to the direction of the annular motion in order to correct any undesirable angle [12–14]. Alternatively it is possible to measure TAPSE in TEE by M-mode in the modified deep transgastric (dTG) RV views [15–17] where the M-mode cursor can be properly aligned with the lateral tricuspid annular plane.
The aim of our study was to evaluate the level of agreement between different methods of measuring TAPSE using TEE with TAPSE measured in TTE in anesthetized patients scheduled for elective cardiac surgery.
Materials and methods
Patients
The study was performed in a university affiliated cardiac surgery center, supported by the local research foundation (Herzzentrum Leipzig, HELIOS Kliniken GmbH). The local ethics committee approved the protocol of this prospective study (Az:014-15-26012015). Written informed consent was obtained from all patients. Thirty patients aged 18 years and older in sinus rhythm scheduled for elective cardiac surgery with a class I indication for intraoperative echocardiography were recruited between February and March 2015. Exclusion criteria were contraindications to TEE, atrial fibrillation, tricuspid regurgitation greater than grade 1 and prior tricuspid valve surgery.
Data acquisition
All echocardiographic data sets were obtained with the “GE Vivid 9” imaging platform (GE, Milwaukee, WI). For transthoracic examination a M5S-TTE probe (GE) and for transesophageal examinations a 6VT.D-TEE probe (GE) was used.
The TEE probe was passed into the esophagus following the intravenous induction of general anesthesia and tracheal intubation as per local protocol.
The same anesthesiologist (AF) performed all of the echocardiographic examinations.
TAPSE measurements were accomplished under stable hemodynamic conditions in the induction room before skin incision in the following order: firstly the transthoracic apical 4CH view (Fig. 1a) with TAPSE M-Mode curve was acquired (Fig. 1b). All of the transesophageal images were acquired subsequently starting with the ME 4CH view. An x-plane image of the left ventricle was acquired. Then the probe was adjusted to provide the best possible visualization of the RV endocardial border; in this view a video loop of ME 4CH view (Fig. 1c) together with a still frame applying AM-mode for TAPSE were recorded (Fig. 1d). The probe was then advanced to the deep TG position to obtain the dTG RV inflow-outflow view at 0° (dTG RV at 0°) aligning the cursor with the direction of tricuspid annular motion. M-mode and AM-mode recordings of the tricuspid annular motion were obtained (Fig. 1e). Finally the image plane was rotated to obtain the dTG RV inflow-outflow long axis view (dTG RV LAX) and still frames of M-mode and AM-mode of the tricuspid annular motion were obtained (Fig. 1f). For TAPSE measurements in M-mode, the cursor was aligned with the junction of the right ventricular free wall and tricuspid valve (white dashed line in Fig. 1); in anatomical M-mode the cursor was freely moved to achieve a parallel intercept angle with the direction of the tricuspid annular movement (green dashed line in Fig. 1). TAPSE was measured as the distance between the systolic and diastolic excursion of the tricuspid valve (blue arrow in Fig. 1b).
The acquisition of images required for the study was followed by a comprehensive 2D and 3D TEE examination in all patients according to the current guidelines [5, 15] and following our routine standard protocol. All TTE and TEE data sets were digitally stored and transferred to a software workstation (Image Arena; TomTec Inc., Unterschleissheim, Germany) for a later offline analysis.
Data analysis
The anesthesiologist who performed the examination carried out the measurements using the software on the ultrasound machine.
Feasibility was assessed by the successful acquisition of 2D loops and images to permit the accomplishment of measurements. Images were considered adequate for the assessment of the right and left ventricular function if endocardial borders could be visualized throughout the entire cardiac cycle. In case of M-mode and AM-mode the images were regarded as adequate when the curve of the lateral tricuspid annular motion was properly displayed over the entire cardiac cycle.
TAPSE in TTE and TEE was measured as the amount of the longitudinal movement of the annulus from end diastole to peak systole using M-mode and AM-mode curves. In TEE it was additionally measured in 2D ME 4CH view as the difference between systolic and diastolic distances of the lateral tricuspid annulus to the right ventricular apex (blue arrow in Fig. 1c).
The interrogation angle (α-angle) of M-mode line in dTG RV views was measured offline in Image Arena to assess the significance of the possible error.
The reliability of the 7 TAPSE measurements was evaluated by calculating intra- and inter-observer variability. In order to test the intra-observer reproducibility, all the measurements were repeated offline a few weeks later by the same observer.
To assess inter-observer reliability a second observer who was not directly involved in the image acquisition and was unaware of the previous results, performed the measurements offline on a subgroup of ten patients selected at random [18].
Fractional area change (calculated as (end-diastolic area − end-systolic area)/end-diastolic area × 100) in ME 4CH loops was used to assess RV function in TEE. Left ventricular function was assessed using the biplane Simpson’s method in TEE x-plane 4CH loop.
Statistical analysis
Continuous variables are presented as mean and standard deviation (SD) or 95% confidence interval (CI 95%). Categorical variables are expressed as percentage.
To assess the correlation between TAPSE measurements obtained by TTE and TEE we used Pearson regression and Passing–Bablock [19] regression analysis that enabled us to identify the possible presence of a systematical bias despite a linear correlation.
Bland–Altman Analysis was used to assess the accuracy and precision of TAPSE measurements between TTE and TEE values in each patient. The accuracy or agreement of measurements, defined as the closeness of measurements to the gold standard value, is represented with the mean difference and its 95% CI. The precision of measurements is represented with the limits of agreement, defined as how close to each other are the repeated measures [20–24].
To determine the clinical relevance of the agreement and precision of our measurements for this study, we accepted the variability previously observed in referenced normal values [5, 6] and we decided that a variation of the mean difference of ±4% and limits of agreement of ±30% are acceptable and clinically irrelevant.
The intra-class coefficient correlation (ICC) was calculated to assess both intra- and inter-observer variability of the measurements. ICC values <0.2 indicates poor, 0.2–0.4 fair, 0.41–0.6 moderate, 0.61–0.8 good and >0.81 very good agreement.
A p value <0.05 represents statistical significance.
Statistical analysis, Passing–Bablok and Bland–Altman plots were performed by MedCalc Statistical Software version 15.6.1 (MedCalc Software bvba, Ostend, Belgium; 2015).
Results
Demographic
The study group comprised of 30 patients. Clinical characteristics of the study population are shown in Table 1.
The cardiac operations included ten cases of mitral valve repair, one mitral valve replacement, ten aortic valve replacements, five aortic valve replacements combined with ascending aortic replacement, two aortic valve replacements combined with coronary artery bypass grafting (CABG), one isolated CABG, and one atrial septal defect closure.
TAPSE measurements
It was feasible in both TTE and TEE to obtain appropriate echocardiographic images in all patients to perform the necessary measurements.
Mean values of TAPSE measurements in different views ranged between 15.92 and 18.97 mm. Details are shown in Table 2.
The TAPSE measurements showed a good correlation with fractional area change (FAC) calculations: in 24 patients with FAC ≥ 35% TAPSE was >17 mm (mean TAPSE value 21 mm); in 6 patients with a calculated FAC < 35% TAPSE was <17 mm (the mean TAPSE value was 11.5 in 4 out of 6 patients who had an FAC between 30 and 35%; the mean TAPSE value was 10 mm in the remaining 2 patients with FAC < 30%).
Interrogation angle
The mean angle between M-mode line and the direction of tricuspid annular plane motion was 29.7° (± 7.2) in dTG RV at 0° view versus 33.4° (± 11.2) in dTG RV LAX view. In dTG RV at 0°, 60% of the patients showed an angle < 30°compared to 43% in dTG RV LAX.
Agreement in TAPSE measurements
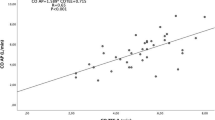
The Pearson regression as well as the Passing–Bablok regression showed an excellent linear relationship between all the measurements (r = 0.93 for ME 4CH 2D, r = 0.94 for ME 4CH AM-mode, r = 0.92 for dTG RV at 0° M-mode, r = 0.97 for dTG RV at 0° AM-mode, r = 0.87 for dTG RV LAX M-mode and r = 0.95 for dTG RV LAX AM-mode). The Passing–Bablok scatter diagram additionally showed, an excellent agreement of the measurements using AM-mode in dTG at 0° and ME 4CH views, and a systematic underestimation of the values for the other four measurements (Figs. 2, 3).
Using TAPSE measured with M-mode in TTE as the standard reference, we found an average mean difference of −1.33 mm (95%CI −5.06–2.43). The results of the Bland–Altman analysis are shown in Table 3.
Figures 2 and 3 illustrate agreement of TAPSE between M-mode in TTE and different TEE measurements presented as Bland–Altman plot (left) with the representation of the mean difference (blue solid line) and 95% limits of agreement from − 1.96 to + 1.96 s (brown dashed lines) presented as units (mm), and Passing–Bablok regression analysis (right) with 95% CI.
The Bland–Altman analysis confirmed a high agreement in TAPSE measurement using AM-mode in dTG RV at 0° and ME 4CH views showing no significant mean difference and a narrow 95% confidence interval (mean difference of −2.2, 95% CI −4.7 to 0.15% and mean difference of −2.5%, 95% CI −5.9 to 1.0% respectively). The 95% limits of agreement (<20%) and its CI (<25%) were narrow in both views showing a high level of precision.
The significant systematic underestimation of TAPSE values measured by the other 4 methods in TEE compared to TTE was confirmed by the Bland–Altman analysis. The agreement of measurements performed with 2D in 4CH view, M-mode in dTG at 0° and AM-mode in dTG LAX ranged between −6 and −8% (−1.1 and −1.46 mm), and the agreement of measurements using M-mode in dTG RV LAX was −17% (>3 mm). The line of equality did not lie within 95%CI of the mean difference in any of the four analyses. Except for TAPSE measurement by M-mode in dTG RV LAX in which 95% limits of agreement was high (>40%), in the other three measurements it was ≤30% showing good precision.
The Bland–Altman analysis used in both dTG RV views regarding the angle of interrogation (α-angle) (Table 4), showed a good agreement and precision of the measurements using M-mode in the dTG RV at 0° if the angle of α was <30° (mean difference −2.5%) compared to the same view with an angle of α > 30°, that showed a significant underestimation (mean difference of −15%); however in the dTG RV LAX all the measurements showed significant underestimation irrespective of the α angle (mean difference of −10.3% by α < 30° and mean difference of −22.2%, by α > 30°).
Intra-observer and inter-observer variability
The intra-class coefficient correlation between the seven different TAPSE values showed a very good reproducibility for measurements, ranging from 0.86 to 0.94 for intra-observer and 0.86–0.95 for inter-observer variability (Table 5).
Discussion
The present study showed that TEE can be used to measure TAPSE with excellent agreement and precision compared to TTE.
The level of agreement between TAPSE measurements in TEE compared to TTE was however dependent upon the specific view used.
The need for quantitative assessment of RV systolic function in the perioperative setting makes TAPSE a valuable tool for quick evaluation thereof [5, 6, 25–29]. Since it is not possible to measure TAPSE by M-mode in the ME 4CH view in TEE, alternative ways like 2D method and AM-mode in the ME 4CH view, and the use of M-mode or AM-mode in the modified deep transgastric RV views have been proposed.
To the best of our knowledge there is no publication assessing the validity of different TAPSE measurements in TEE compared to standard TTE.
The measurements in our study using AM-mode in the ME 4CH view and dTG RV view at 0° showed the best agreement (<2.5%) and a good precision (<20%) which was consistent with our predetermined limits of variability (agreement <4% and precision <30%).
The AM-mode technology allows the interrogation of the tricuspid annular movement irrespective of the angle of interrogation. Unlike conventional M-mode, anatomical M-mode images are reconstructed from 2D images leading to the loss of characteristic high temporal resolution of M-mode [12]. However it did not lead to a wider dispersion of 95% CI of the mean difference of our measurements performed by AM-mode and neither the intra- nor inter-observer variability were affected.
Despite the promising characteristics of AM-mode, there has not been widespread use of it in assessing TAPSE in TEE. We found only one study [30] that described its usefulness for estimating TAPSE in TEE. Different TAPSE measurement methods in TEE (M-mode, speckle tracking and tissue tracking) were compared to the stroke volume, however the authors did not compare these measurements with TTE.
Our measurements using 2D echocardiography showed a systematic underestimation of the agreement of measurements (−8%) but the precision remained within our previously defined limit (<30%). Which means that 2D technology on average estimated TAPSE values 1.5 mm lower than TTE, but with an acceptable variability.
The inherent lower frame rate and hence the lower temporal resolution of 2D technology compared to M-mode confronts the observer with the challenge of the correct recognition of endocardial borders and accurate identification of the RV apex when using the 2D method. This may be the reason for the slightly higher intra- and inter-observer variability observed in our study compared to the M-mode measurements although it remained within very good agreement.
The 2D method has been described as an alternative method to measure TAPSE in TEE. Only a few studies utilized this method in the assessment of TAPSE [31, 32] in correlation with outcome or to compare this measurement with the overall RV function. We could not find any validation of 2D measurement compared to the standard method in TTE. Yasir Qureshi et al. [33] recently demonstrated the usefulness of TAPSE measurement in TTE using 2D compared to M-mode in children. They also found a systematic underestimation of 1 mm in 2D values, which is consistent with our results, indicating that it could be a good alternative when other assessment methods are not available.
In order to find a solution for the difficulty RV assessment in TEE, new standard and non-standard RV views [15–17] have been introduced over the past few years with which TAPSE can be measured.
The use of the deep TG RV inflow-outflow view at 0° ensures good visualization of the tricuspid valve, tricuspid annulus and RV free wall motion. This view is obtained by making a small modification in the standard TG RV inflow–outflow view at 0°view, by advancing the probe until the RV free wall lies as parallel to the cursor as possible. In our study we could demonstrate that the use of AM-mode should serve to further optimize the angle of interrogation to obtain a precise and accurate measurement, as α-angle greater than 30° led to a significant underestimation of TAPSE. When the angle of interrogation was no greater than 30° the agreement of our measurements showed no differences to that of the standard TTE measurement.
The deep TG RV inflow-outflow view at 120–160° described by Kasper et al. [16] allows good visualization of the right ventricular structures. David et al. [34] showed the feasibility of measuring tricuspid annular motion and velocity in this dTG RV LAX view with TEE but they did not compare the values with TTE. Nevertheless this view has some limitations: firstly we experienced more difficulty aligning the cursor to the free wall, secondly in comparison with the dTG RV inflow-outflow view at 0° and standard 4CH view a somewhat more posteriorly located part of the free wall is observed in this view. It is known that the amount of tricuspid annular motion in this region is not equal to the anterior part, which shows the greatest displacement [35]. This is in concordance with our findings showing a systematic underestimation of measurements when using M-mode irrespective of the angle of interrogation and even when using AM-mode technology in the dTG RV inflow-outflow view at 120–160°.
Limitation of the study
The quality of 2D images is not only essential for accurate 2D measurements but also for measurements made by AM-mode. Frame rate together with an absence of artifact determine the degree of temporal and axial resolution of the acquired images, which directly influence the quality and reproducibility of the measurements, whereas M-mode inherently possesses an excellent temporal resolution thanks to its high frame rate.
Most of the patients in our study had right ventricles of normal size and function therefore we do not know if the good agreement between the different methods remains true in severely compromised right ventricles.
Conclusion
This study demonstrates that the evaluation of RV function by means of TAPSE measurement in TEE can be performed with an excellent level of agreement and precision compared to TTE.
The most accurate and precise measurements can be achieved with the use of anatomical M-mode either in the ME 4CH view or dTG RV view at 0°, as well as in the dTG RV view at 0° using M-mode assuming the interrogation angle does not exceed 30°. Therefore we do not recommend the dTG RV LAX view to measure TAPSE.
However if AM-mode technology is not available, TAPSE measurements using 2D in the ME 4CH view can provide a reliable alternative taking the slight underestimation of the values into account. The clinical importance of this slight underestimation should be further evaluated.
References
Denault AY, Haddad F, Jacobsohn E, Deschamps A (2013) Perioperative right ventricular dysfunction. Curr Opin Anaesthesiol 26(1):71–81. doi:10.1097/ACO.0b013e32835b8be2
Vandenheuvel MA, Bouchez S, Wouters PF, De Hert SG (2013) A pathophysiological approach towards right ventricular function and failure. Eur J Anaesthesiol 30(7):386–394. doi:10.1097/EJA.0b013e3283607a2d
Haddad F, Elmi-Sarabi M, Fadel E, Mercier O, Denault AY (2016) Pearls and pitfalls in managing right heart failure in cardiac surgery. Curr Opin Anaesthesiol 29(1):68–79. doi:10.1097/ACO.0000000000000284
Lella LK, Sales VL, Goldsmith Y, Chan J, Iskandir M, Gulkarov I, Tortolani A, Brener SJ, Sacchi TJ, Heitner JF (2015) Reduced right ventricular function predicts long-term cardiac re-hospitalization after cardiac surgery. PLoS ONE 10(7):e0132808. doi:10.1371/journal.pone.0132808
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28 (1):1–39 e14. doi:10.1016/j.echo.2014.10.003
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23 (7):685–713. doi:10.1016/j.echo.2010.05.010. quiz 786–688
Kaul S, Tei C, Hopkins JM, Shah PM (1984) Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 107(3):526–531
Ho SY, Nihoyannopoulos P (2006) Anatomy, echocardiography, and normal right ventricular dimensions. Heart 92(Suppl 1):i2–i13. doi:10.1136/hrt.2005.077875
Leather HA, Ama R, Missant C, Rex S, Rademakers FE, Wouters PF (2006) Longitudinal but not circumferential deformation reflects global contractile function in the right ventricle with open pericardium. Am J Physiol Heart Circ Physiol 290(6):H2369–H2375. doi:10.1152/ajpheart.01211.2004
Hashimoto I, Watanabe K (2016) Geometry-related right ventricular systolic function assessed by longitudinal and radial right ventricular contractions. Echocardiography 33(2):299–306. doi:10.1111/echo.13039
Wouters P (2010) The right ventricle. In: Feneck RO, Kneeshaw J, Ranucci M (eds) Core topics in transesophageal echocardiography. Cambridge University Press, Cambridge; New York, p 416
Carerj S, Micari A, Trono A, Giordano G, Cerrito M, Zito C, Luzza F, Coglitore S, Arrigo F, Oreto G (2003) Anatomical M-mode: an old-new technique. Echocardiography 20(4):357–361
Donal E, Coisne D, Pham B, Ragot S, Herpin D, Thomas JD (2004) Anatomic M-mode, a pertinent tool for the daily practice of transthoracic echocardiography. J Am Soc Echocardiogr 17(9):962–967. doi:10.1016/j.echo.2004.05.009
Mele D, Pedini I, Alboni P, Levine RA (1998) Anatomic M-mode: a new technique for quantitative assessment of left ventricular size and function. Am J Cardiol 81 (12A):82G-85G
Hahn RT, Abraham T, Adams MS, Bruce CJ, Glas KE, Lang RM, Reeves ST, Shanewise JS, Siu SC, Stewart W, Picard MH, American Society of Echocardiography, Society of Cardiovascular A (2014) Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Anesth Analg 118 (1):21–68. doi:10.1213/ANE.0000000000000016
Kasper J, Bolliger D, Skarvan K, Buser P, Filipovic M, Seeberger MD (2012) Additional cross-sectional transesophageal echocardiography views improve perioperative right heart assessment. Anesthesiology 117(4):726–734. doi:10.1097/ALN.0b013e318269054b
Tan CO, Harley I (2014) Perioperative transesophageal echocardiographic assessment of the right heart and associated structures: a comprehensive update and technical report. J Cardiothorac Vasc Anesth 28(4):1100–1121. doi:10.1053/j.jvca.2013.05.031
Ling LF, Obuchowski NA, Rodriguez L, Popovic Z, Kwon D, Marwick TH (2012) Accuracy and interobserver concordance of echocardiographic assessment of right ventricular size and systolic function: a quality control exercise. J Am Soc Echocardiogr 25(7):709–713. doi:10.1016/j.echo.2012.03.018
Bilic-Zulle L (2011) Comparison of methods: Passing and Bablok regression. Biochem Med (Zagreb) 21(1):49–52
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Bland JM, Altman DG (1990) A note on the use of the intraclass correlation coefficient in the evaluation of agreement between two methods of measurement. Comput Biol Med 20(5):337–340
Chhapola V, Kanwal SK, Brar R (2015) Reporting standards for Bland–Altman agreement analysis in laboratory research: a cross-sectional survey of current practice. Ann Clin Biochem 52 (Pt 3):382–386. doi:10.1177/0004563214553438
Giavarina D (2015) Understanding Bland Altman analysis. Biochem Med (Zagreb) 25(2):141–151. doi:10.11613/BM.2015.015
Mantha S, Roizen MF, Fleisher LA, Thisted R, Foss J (2000) Comparing methods of clinical measurement: reporting standards for bland and altman analysis. Anesth Analg 90(3):593–602
Focardi M, Cameli M, Carbone SF, Massoni A, De Vito R, Lisi M, Mondillo S (2015) Traditional and innovative echocardiographic parameters for the analysis of right ventricular performance in comparison with cardiac magnetic resonance. Eur Heart J Cardiovasc Imaging 16(1):47–52. doi:10.1093/ehjci/jeu156
Galli E, Guirette Y, Feneon D, Daudin M, Fournet M, Leguerrier A, Flecher E, Mabo P, Donal E (2015) Prevalence and prognostic value of right ventricular dysfunction in severe aortic stenosis. Eur Heart J Cardiovasc Imaging 16(5):531–538. doi:10.1093/ehjci/jeu290
Nguyen T, Cao L, Movahed A (2014) Altered right ventricular contractile pattern after cardiac surgery: monitoring of septal function is essential. Echocardiography 31(9):1159–1165. doi:10.1111/echo.12657
Pleister A, Kahwash R, Haas G, Ghio S, Cittadini A, Baliga RR (2015) Echocardiography and heart failure: a glimpse of the right heart. Echocardiography 32(Suppl 1):S95–S107. doi:10.1111/echo.12678
Portnoy SG, Rudski LG (2015) Echocardiographic evaluation of the right ventricle: a 2014 perspective. Curr Cardiol Rep 17(4):21. doi:10.1007/s11886-015-0578-8
Tousignant C, Kim H, Papa F, Mazer CD (2012) Evaluation of TAPSE as a measure of right ventricular output. Can J Anaesth 59(4):376–383. doi:10.1007/s12630-011-9659-3
Morita Y, Nomoto K, Fischer GW (2016) Modified tricuspid annular plane systolic excursion using transesophageal echocardiography for assessment of right ventricular function. J Cardiothorac Vasc Anesth 30(1):122–126. doi:10.1053/j.jvca.2015.07.024
Fusini L, Tamborini G, Gripari P, Maffessanti F, Mazzanti V, Muratori M, Salvi L, Sisillo E, Caiani EG, Alamanni F, Fiorentini C, Pepi M (2011) Feasibility of intraoperative three-dimensional transesophageal echocardiography in the evaluation of right ventricular volumes and function in patients undergoing cardiac surgery. J Am Soc Echocardiogr 24(8):868–877. doi:10.1016/j.echo.2011.05.002
Qureshi MY, Eidem BW, Reece CL, O’Leary PW (2015) Two-dimensional measurement of tricuspid annular plane systolic excursion in children: can it substitute for an m-mode assessment? Echocardiography 32(3):528–534. doi:10.1111/echo.12687
David JS, Tousignant CP, Bowry R (2006) Tricuspid annular velocity in patients undergoing cardiac operation using transesophageal echocardiography. J Am Soc Echocardiogr 19(3):329–334. doi:10.1016/j.echo.2005.09.013
Atsumi A, Ishizu T, Kameda Y, Yamamoto M, Harimura Y, Machino-Ohtsuka T, Kawamura R, Enomoto M, Seo Y, Aonuma K (2013) Application of 3-dimensional speckle tracking imaging to the assessment of right ventricular regional deformation. Circ J 77(7):1760–1768
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Flo Forner, A., Hasheminejad, E., Sabate, S. et al. Agreement of tricuspid annular systolic excursion measurement between transthoracic and transesophageal echocardiography in the perioperative setting. Int J Cardiovasc Imaging 33, 1385–1394 (2017). https://doi.org/10.1007/s10554-017-1128-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-017-1128-9