Abstract
Tricuspid annular plane systolic excursion (TAPSE) is a robust measure of RV function, but the performance of transesophageal echocardiography (TEE) measured TAPSE during surgery is not well established. We aim to evaluate feasibility of various TEE views before, during and after surgery. Furthermore, we compare performance of individual TEE measurements depending on view and method (AMM- and M-mode as well as 2D) as well as TAPSE measured using TEE with transthoracic echocardiography (TTE) TAPSE. The study was conducted from January 2015 through September 2016. In 47 patients with normal left ventricular ejection fraction, TEE was prospectively performed during coronary artery bypass grafting surgery. TAPSE and tricuspid annulus tissue Doppler imaging (TDI) were recorded in five different views at pre-specified time points during surgery. Data were analyzed for availability (obtainable/readable images) and reliability (intra-/inter-observer bias and precision). Finally, TEE TAPSE was compared to TTE TAPSE immediately before and after surgery. TAPSE and TDI with TEE was achievable in > 90% of patients in the transgastric view during surgery. The AM- and M-mode had the best reliability and the best correlation with TAPSE measured with TTE. The deep transgastric view was achievable in less than 50% after sternotomy, and TAPSE measured from 2D had a poorer performance compared to the AM- and M-mode. TDI demonstrated a high reliability throughout surgery. RV function can be evaluated by TAPSE and TDI using TEE during surgery. TEE values from the transgastric view demonstrated high performance throughout surgery and a good agreement with TTE TAPSE measurements.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Right ventricular (RV) failure during heart surgery carries a poor prognosis and the condition continues to be a challenge to identify and quantify early, before it becomes clinically important [1]. Tricuspid annular plane systolic excursion (TAPSE) has, since its description in 1984, been a cornerstone in the evaluation of RV function [2, 3]. TAPSE has mainly been assessed by transthoracic echocardiography (TTE), because of its robustness, both in terms of feasibility and reproducibility [4,5,6,7,8]. In contrast, per-operative echocardiography performed by transesophageal echocardiography (TEE), including TAPSE measurements in the assessment of RV function is not well established yet. It has recently been shown that M-mode TEE TAPSE in the 4-chamber view does not correlate with TTE TAPSE due to angle misalignment, but that off-line software automated tracing of TAPSE in the 4-chamber view can partly compensate for this [9]. However, during surgery, it would be preferable not to rely on off-line analysis. Morita et al. [10] used manual tracing of TAPSE in the same TEE 4-chamber view and found good correlation with RV-FAC during heart surgery. However, they did not evaluate reliability of the method nor agreement with TTE TAPSE [10]. Another approach is the anatomic M (AM)-mode with TEE [12]. It can potentially reduce angle errors inherent in M-mode imaging by optimizing the cursor vector within the 2D image plane. The AM-mode for TAPSE by TEE was recently evaluated by Flo et al., and they found good agreement with TAPSE measured by TTE, immediately after induction of anesthesia [11]. However, the authors did not evaluate the feasibility of TEE TAPSE throughout surgery. The latter is important as chest opening, air in the mediastinum and post bypass hemodynamics might alter conditions for feasibility. Thus, to purposefully use TEE TAPSE for early detection of changes in RV function during heart surgery, its feasibility and the optimal way of measurement throughout surgery needs to be determined. Until now no systematic evaluation of systematic evaluation of TEE TAPSE feasibility and repoducibility exists. Before evaluating the performance of TAPSE measured by TEE in the failing RV, we found it necessary first to describe the performance of multiple ways of measuring TEE TAPSE in RVs without failure. Consequently we evaluated TEE TAPSE in a homogenous patient population with a low risk of RV impairment during cardiac surgery.
The primary aim of the study was thus to evaluate five different TEE TAPSE views at pre-specified time points during surgery, applying the AM-mode and M-mode as well as tracing the 4-chamber view to determine each individual approach’s feasibility (availability and intra-/inter-observer reliability) and their agreement with TTE TAPSE before and after surgery. In addition, we measured another marker of RV function namely tissue Doppler velocities (TDI) of the tricuspid annulus and evaluated the performance in terms of intra- and inter-observer reliability throughout surgery.
Methods
Design
The study was a single-center prospective observational study. The Danish Capital Region Regional Ethics Committee waived the need for informed consent because participation in the study was considered non-jurisdictional since the study qualified as quality assurance (protocol# H-4-2014-FSP). All data handling was performed in accordance with Danish law and was approved by the Danish Data Protection Agency (journal # 2012-58-0004 RH-2017-78, I-Suite #: 05350) and the Danish Patient Safety Authority.
Patients
Patients were included from January 2015 through September 2016. In order to have a standardized patient population; all patients underwent surgery by the same head surgeon or two of that surgeon’s junior faculty. Patients admitted to the same head surgeon and anesthesiologist were included if they met the following criteria: above 18 years of age; elective CABG procedure; left ventricular ejection fraction of more than 50%; no more than mild heart valve pathology on preoperative TTE and placement of a TEE probe. Patients with non-sinus rhythm on electrocardiogram (ECG) recognized preoperatively or in the operating room were excluded. Moreover, patients were excluded if they had evidence of pulmonary hypertension (pulmonary artery pressure estimated above 25 mmHg systolic), heart malformations or shunts on cardiac catheterization or TTE. All treatment decisions were left to the discretion of the treating anesthesiologist and heart surgeon. TEE exams had not been performed in any of the patients’ prior to enrollment in the study.
Procedure
Patients underwent general anesthesia and had TTE TAPSE measurements performed after induction of anesthesia and endotracheal intubation had been performed. The TEE probe was placed after completion of TTE measurements. TEE measurements were performed at pre-specified time points: before skin incision, after sternotomy, after pericardiotomy, following cardiopulmonary bypass, and after sternal closure. Immediately following removal of the TEE probe another TTE acquisition was made, while the patient was still on the operating table. The maximum time allotted between TTE and corresponding first and last TEE acquisition was less than 10 min during which the patient was hemodynamically stable and without any change in fluid balance. Brief interruptions of surgery were allowed to accommodate image acquisition.
Echocardiography
An experienced cardiac anesthesiologist (AK), with extensive echocardiographic experience and certified diploma with the National Board of Echocardiography, acquired all images.
Images were recorded twice approximately 5 min apart over five consecutive synchronized cardiac cycles utilizing either a Philips IE33 (Philips Healthcare, Inc., Andover, MA); (35 patients) or a Philips EPIQ7C ultrasound machine (Philips Healthcare, Inc., Andover, MA); (15 patients). The EPIQ7C machine can apply AM-mode as opposed to the Philips IE33. For TTE imaging a S5-1 probe was used and for TEE imaging a X7-2 probe was used. Imaging data were stored centrally for off line analysis.
TTE TAPSE was imaged using the traditional method with M-mode of the lateral tricuspid annulus in the apical 4-chamber view. The following 5 TEE views were acquired: (1) Lateral tricuspid annulus manual base to apex distance change tracking from end-diastole to end-systole in the mid-esophageal 4-CHamber view (0–10°) (4CH-TAPSE), (2) M-Mode of the lateral tricuspid annulus in the TransGastric RV-inflow view (100–130°) modified for optimal cursor angle positioning for maximal excursion (MMTG-TAPSE). (3) The same view with AM-mode applied (patients imaged with EPIQ7c) for additional angle optimization by re-orienting the cursor vector (AMMTG-TAPSE—see Fig. 1), (4) M-Mode of the lateral tricuspid annulus in the Deep TransGastric view (0–10°) (MMDTG-TAPSE) and finally (5) in the same view AM-mode was applied (patients imaged with EPIQ7C) for additionally angle optimization (AMMDTG-TAPSE). Care was taken to use the same omniplane angle in one set of views as in the other set of views.
In addition, TDI of the lateral tricuspid annulus were acquired. The TDI of the tricuspid annulus was acquired in the mid-esophageal 4-CHamber view (0–10°) (4CH-TDI), the transgastric RV-inflow view (100–130°) modified for optimal cursor angle for maximal velocity (TG-TDI) as well as the Deep TransGastric view (0–10°) (DTG-TDI).
All images were analyzed using Philips Intellispace Cardiovascular Imaging software as the average of all readable images over all recorded cardiac cycles, because apneic measurements were not performed. Obtainability was defined as the acquisition of an image deemed readable during the exam. Readable images were defined as complete delineation of the endocardial border of the RV and tricuspid annulus in B-mode; completely traceable lines in M- and AM-mode; and completely traceable envelopes of PW and TD velocities. Readability was not evaluated until off-line.
For intra-observer precision 10 randomly selected patients had a second reading done by the primary reader separated by a minimum timespan of 3 month. Data were analyzed in a blinded manner. For assessment of inter-observer precision, a second echocardiographic reader (LG), analyzed the same 10 patients, in a blinded manner. The study was part of a larger data analysis of the peri-operative use of TEE for assessment of RV function.
Statistics
Continuous variables were calculated as the mean and 95% confidence interval or standard deviation. Categorical variables are presented as absolute numbers and percentages. The observer variation of TAPSE readings was assessed by the interclass-correlation coefficient (Pearson).
Bland and Altman (BA) analysis with plot construction and calculation of the mean of the difference (bias) as well as limits of agreement (LOA) [12] was used in the comparison of inter- and intra-observer precision. The percentage error of intra- and inter-observer agreement was calculated as the coefficient of variation. To determine the best agreement of the TTE TAPSE with the different TEE projections, BA analysis was also used with error- as well as the correlation-coefficient calculation. Analyses were performed using SPSS, version 23.0 for Mac OS (SPSS, Inc. Chicago, IL, USA) and Prism version 5.0 for Mac OS X.
Results
Patients
Forty-seven patients were included in the study. Patient flow is shown in Fig. 2. Three patients were excluded: one because of newly developed atrial fibrillation in the operating room, one due to an aortic stenosis on TEE diagnosed in the operating room, and one patient because both TEE and TTE image quality were unacceptably low, leaving 44 patients for evaluation. Patients were low risk CABG patients as demonstrated by patient characteristics in Table 1.
Availability
The percentage of obtainable and readable images with various echocardiographic approaches is shown in Table 2. Availability of TTE TAPSE was high both before and after surgery. TAPSE measured with TEE was readily available in all mid-esophageal and transgastric views, both before and throughout surgery in 2D, M-mode and AM-mode. In deep transgastric views, the availability of TAPSE measurements by TEE was below 50% during surgery, and was only achievable at the end of surgery in less than one-third of patients when applying TDI-mode.
Reliability
The intra- and inter-observer correlation and precision of the various TAPSE views are shown in Table 3 and with BA plots in Fig. 3. The bias was low (between 0.1 and 0.9 mm), and the percentage error good (9.1–12.5%) for all M- and AM-mode TAPSE measurements, irrespective of view, and comparable reliability as TTE assessed TAPSE. In contrast, the distance tracking of TAPSE in 2D had an unacceptable high bias (0.4–2.3 mm) and a low precision (> 20%). TDI assessment was reliable in TG and DTG views, but not in the 4CH view.
Interchangeability
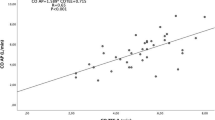
Agreement and correlation between TTE TAPSE and TEE TAPSE in various projections are shown in Table 4 with BA plots in Fig. 4. All projections showed moderate to strong correlation to TTE TAPSE, apart from the MMTG view, where the bias was > 3 mm and a CV% > 25%. The AM M-mode TAPSE both in the transgastric and deep transgastric view had the best correlation (> 95%) with TTE TAPSE.
Discussion
Right ventricular function remains a challenge to evaluate and quantify, especially during cardiac surgery. The utility of TAPSE measured by TEE is increasingly being recognized and could prove a valuable tool in RV assessment in settings where TTE is not feasible. The first step in this process is to find an accessible and reproducible TEE TAPSE measure. The main findings in the present study were: TAPSE can easily be measured by TEE, especially in transgastric views during the entire surgical procedure; Assessment of TAPSE demonstrated a high intra- and inter-observer reliability for all AM and M-mode methods; The AM-mode in the modified RV-inflow view was the single projection having the best agreement and precision compared to measurement of TAPSE using standard TTE; At the same time, the transgastric projection had easily available images throughout surgery.
This study is to our knowledge the first to systematically evaluate the performance of a wide array of ways to measure TEE TAPSE throughout surgery. Comparison of TAPSE measured by TTE and TEE has recently been published in outpatients scheduled for TEE by Skinner et al. [13] and in elective cardiac surgery patients after induction of anesthesia in studies by Flo et al. [11] as well as by Markin et al. [9]. Moderate to high agreement was observed between TAPSE measured by TEE and TTE in these patient populations [9, 11, 13]. Neither of these studies evaluated TAPSE during surgery, which justifies the present study evaluating the feasibility of TAPSE measurement throughout surgery. The methods used to measure TEE TAPSE in the studies by Markin et al. [9] and Skinner et al. require post processing of the acquired image to obtain a TAPSE value and we elected to only evaluate measures that are rapidly available to the clinicians like the AM-mode used by Flo et al. [11]. We found a high agreement and a good precision between TAPSE measured by TTE and the AM-mode of deep transgastric view. However, although this view had a high performance, it lacked availability throughout surgery, since this view could only be obtained in less than half of the patients, while the chest was open. This clearly disqualifies the use of the deep transgastric approach, since the view applied for the baseline measurement must be accessible throughout surgery to track changes in TAPSE.
In our experience, the lack of availability using the deep transgastric view is probably due to misalignment issues. During ongoing surgery, a more anterior position of the tricuspid annulus as well as air artifacts after sternotomy are more prominent in this view compared to the modified transgastric RV-inflow view.
The four measures of TEE TAPSE based on M-mode and AM-mode had comparable intra-observer and inter-observer reliability with M-mode based measurement of TTE TAPSE in the present study, which has also been found in previous studies [14,15,16,17]. All AM-modes measures’ agreement with TEE-TAPSE had low biases between − 0.1 and 0.6 mm and precision error values below 10.1%. In contrast, conventional M-mode readings of TAPSE did not agree well with TTE TAPSE with biases up to − 3.2% and precisions errors up to 29.6%. The most obvious reason for the difference between M-and AM-mode is the ability of the AM-mode to actually compensate for angle errors (see Fig. 1). To our knowledge very few studies have used AM-mode in echocardiographic evaluation, although its utility in TAPSE measurement by TEE could prove valuable as suggested by the present study and recent observations published by Forner et al. [11].
The tracing method in 4-chamber 2D (4CH-TAPSE) is often encouraged as a reliable way to circumvent the angle error inherent for TAPSE measured by TEE [10, 11, 18]. Measurement with 2D imaging (4 CH TAPSE) had an intra-observer and inter-observer limits of agreement of − 8 to 7 mm and − 11 to 7 mm, respectively. The precision was between 22 and 27%. Although, this is below the 30% margin often advocated as a cut-off for acceptable inter-method agreement for physiological variables [11, 19], it should be used judiciously. The inherent difficulty in accurately defining the apex of the heart with TEE is probably the explanation for the impaired performance. In this respect, Markin et al. [9] used automated tracing instead, which led to a higher reliability with an observer R of 0.71. However, the authors did not provide observer reliability by means of a Bland- Altman analysis. We found a comparable R of 0.70 with manual tracing of TAPSE, but at the same time an unacceptable high bias with LOA ranging from-8 to7 mm, which demonstrates that the method carries a higher uncertainty, despite a good correlation.
Assessment of tissue Doppler of the lateral tricuspid annulus has been advocated as an alternative to TAPSE when assessing RV longitudinal function [20]. Previous studies with TTE have estimated correlation coefficients of 0.75 to 0.93 for inter- and intra-observer precision using this approach [15, 21]. In the setting of TEE assessment of RV function, both 4-chamber [22] and transgastric views have been applied [23]. Accordingly, we observed similar intra- and inter-observer correlations for TEE tissue Doppler measurements, with the best performance of the deep transgastric TDI. Not surprisingly, but in accordance with the TEE TAPSE assessment, this approach was seldom available during surgery, where only one-third of the patients had accessible measurements after the sternum had been opened. Favorably, the transgastric view was almost always accessible (> 90%) in the patients during the entire surgical procedure. Moreover, a good intra-and inter-observer reliability in the transgastric view was observed, when paying careful attention to an ambiguous S′ (Fig. 5). The ambiguity issue was overcome by a pre-assessment consensus on how to read the largest deflection of the S′, by which the method’s performance improved markedly. This ambiguous S′ wave has also been reported by David et al. [23] who studied tissue Doppler velocities in the transgastric RV-inflow view before and after, but not during CABG surgery. The 4-chamber tissue Doppler view showed a poor observer reliability and its use should be discouraged, as already suggested by David et al. [23]. In our experience, turning the TEE probe to the right side causes an almost perpendicular cursor vector alignment, making readings indistinguishable from PW Doppler blood flow signals arising from the inferior caval vein, which has a similar appearance as the PW TDI signals from the tricuspid annulus [24].
The limitation of this study is that it was done in a single center and although image interpretation was done by several readers, the image acquisition was obtained by a single echocardiographer. Acquisition by several operators would have provided insight into the variability in image acquisition, but could not be carried out due to time constraints set by the surgery. Another limitation is the fact, that the majority of patients in the present study had right side heart chambers of normal size and function. Because of this, we do not know if observations and method interchangeability can be generalized to patients with right heart failure. However, the size of TAPSE varied between 2 and 30 mm in the present study, indicating a certain robustness of the observations.
A decline in TAPSE following surgery has been described previously [25,26,27,28,29], a phenomenon we also observed. The present CABG population was patients with preserved left ventricular function and without clinical signs of right sided heart failure after the surgical procedure. We believe it is a strength of the study that the methodology behind TAPSE assessment is described during “normal” changes after a CABG procedure, before we start to evaluate the performance of the method in a population with RV failure following cardiac surgery (Fig. 6).
Conclusion
This study demonstrates that RV function can be evaluated by means of TAPSE measured by TEE and the method has good agreement and precision with TTE assessed TAPSE. However, the availability during surgery is highly variable and dependent on the choice of view. Among the views with a high availability, throughout the entire surgical procedure, was the transgastric view. The AM-mode demonstrated good correlation with TAPSE measured by TTE and had low intra- and inter-observer variability. We do not recommend routine use of the 2D 4-chamber view with distance tracking of TAPSE, which showed poor observer agreement and a low correlation with TTE assessed TAPSE. An alternative approach to evaluate RV systolic function may be by tissue Doppler measurements. In this respect, the transgastric TDI had the best performance with a low bias and a good precision.
References
Vlahakes GJ (2012) Right ventricular failure after cardiac surgery. Cardiol Clin 30:283–289. https://doi.org/10.1016/j.ccl.2012.03.010
Kaul S, Tei C, Hopkins JM, Shah PM (1984) Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 107:526–531
Sato T, Tsujino I, Oyama-Manabe N et al (2013) Simple prediction of right ventricular ejection fraction using tricuspid annular plane systolic excursion in pulmonary hypertension. Int J Cardiovasc Imaging 29:1799–1805. https://doi.org/10.1007/s10554-013-0286-7
Grønlykke L, Ravn HB, Gustafsson F et al (2016) Right ventricular dysfunction after cardiac surgery - diagnostic options. Scand Cardiovasc J. https://doi.org/10.1080/14017431.2016.1264621
Kjaergaard J, Petersen CL, Kjaer A et al (2006) Evaluation of right ventricular volume and function by 2D and 3D echocardiography compared to MRI. Eur J Echocardiogr 7:430–438. https://doi.org/10.1016/j.euje.2005.10.009
Hamilton-Craig CR, Stedman K, Maxwell R et al (2016) Accuracy of quantitative echocardiographic measures of right ventricular function as compared to cardiovascular magnetic resonance. IJCHA 12:38–44. https://doi.org/10.1016/j.ijcha.2016.05.007
Sato T, Tsujino I, Ohira H et al (2012) Validation study on the accuracy of echocardiographic measurements of right ventricular systolic function in pulmonary hypertension. J Am Soc Echocardiogr 25:280–286. https://doi.org/10.1016/j.echo.2011.12.012
Smith JL, Bolson EL, Wong SP et al (2003) Three-dimensional assessment of two-dimensional technique for evaluation of right ventricular function by tricuspid annulus motion. Int J Cardiovasc Imaging 19:189–197
Markin NW, Chamsi-Pasha M, Luo J et al (2016) Transesophageal speckle-tracking echocardiography improves right ventricular systolic function assessment in the perioperative setting. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2016.10.002
Morita Y, Nomoto K, Fischer GW (2016) Modified tricuspid annular plane systolic excursion using transesophageal echocardiography for assessment of right ventricular function. J Cardiothorac Vasc Anesth 30:122–126. https://doi.org/10.1053/j.jvca.2015.07.024
Flo Forner A, Hasheminejad E, Sabate S et al (2017) Agreement of tricuspid annular systolic excursion measurement between transthoracic and transesophageal echocardiography in the perioperative setting. Int J Cardiovasc Imaging 26:71. https://doi.org/10.1007/s10554-017-1128-9
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Skinner H, Kamaruddin H, Mathew T (2016) Tricuspid annular plane systolic excursion: comparing transthoracic to transesophageal echocardiography. J Cardiothorac Vasc Anesth. https://doi.org/10.1053/j.jvca.2016.09.001
Tamborini G, Muratori M, Brusoni D et al (2009) Is right ventricular systolic function reduced after cardiac surgery? A two- and three-dimensional echocardiographic study. Eur J Echocardiogr 10:630–634. https://doi.org/10.1093/ejechocard/jep015
Olmos-Temois SG, Santos-Martínez LE, Álvarez-Álvarez R et al (2016) Interobserver agreement on the echocardiographic parameters that estimate right ventricular systolic function in the early postoperative period of cardiac surgery. Med Intensiva. https://doi.org/10.1016/j.medin.2016.02.013
Kopecna D, Briongos S, Castillo H et al (2014) Interobserver reliability of echocardiography for prognostication of normotensive patients with pulmonary embolism. Cardiovasc Ultrasound 12:29. https://doi.org/10.1186/1476-7120-12-29
de Knegt MC, Biering-Sorensen T, Sogaard P et al (2014) Concordance and reproducibility between M-mode, tissue Doppler imaging, and two-dimensional strain imaging in the assessment of mitral annular displacement and velocity in patients with various heart conditions. Eur Heart J Cardiovasc Imaging 15:62–69. https://doi.org/10.1093/ehjci/jet119
Peter Slinger MF (2011) Principles and Practice of Anesthesia for Thoracic Surgery. Springer, New York
Møller-sørensen H, Graeser K, Hansen KL et al (2013) Measurements of cardiac output obtained with transesophageal echocardiography and pulmonary artery thermodilution are not interchangeable. Acta Anaesthesiol Scand 58:80–88. https://doi.org/10.1111/aas.12227
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39.e14. https://doi.org/10.1016/j.echo.2014.10.003
Pinedo M, Villacorta E, Tapia C et al (2010) Inter- and intra-observer variability in the echocardiographic evaluation of right ventricular function. Rev Esp Cardiol 63:802–809
Unsworth B, Casula RP, Kyriacou A et al (2010) The right ventricular annular velocity reduction caused by coronary artery bypass graft surgery occurs at the moment of pericardial incision. Am Heart J 159:314–322. https://doi.org/10.1016/j.ahj.2009.11.013
David J-S, Tousignant CP, Bowry R (2006) Tricuspid annular velocity in patients undergoing cardiac operation using transesophageal echocardiography. J Am Soc Echocardiogr 19:329–334. https://doi.org/10.1016/j.echo.2005.09.013
Pinto FJ, Wranne B, St Goar FG et al (1992) Systemic venous flow during cardiac surgery examined by intraoperative transesophageal echocardiography. Am J Cardiol 69:387–393
Wranne B, Pinto FJ, Hammarström E et al (1991) Abnormal right heart filling after cardiac surgery: time course and mechanisms. Br Heart J 66:435–442
Fusini L, Tamborini G, Gripari P et al (2011) Feasibility of intraoperative three-dimensional transesophageal echocardiography in the evaluation of right ventricular volumes and function in patients undergoing cardiac surgery. J Am Soc Echocardiogr 24:868–877. https://doi.org/10.1016/j.echo.2011.05.002
Mitoff PR, Beauchesne L, Dick AJ et al (2012) Imaging the failing right ventricle. Curr Opin Cardiol. https://doi.org/10.1097/HCO.0b013e32834fec4e
Rösner A, Avenarius D, Malm S et al (2015) Changes in Right Ventricular Shape and Deformation Following Coronary Artery Bypass Surgery-Insights from Echocardiography with Strain Rate and Magnetic Resonance Imaging. Echocardiography 32:1809–1820. https://doi.org/10.1111/echo.12973
Grønlykke L, Ihlemann N, Ngo AT et al (2016) Measures of right ventricular function after transcatheter versus surgical aortic valve replacement. Interact Cardiovasc Thorac Surg. https://doi.org/10.1093/icvts/ivw350
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflict of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All data handling was performed in accordance with Danish law and was approved by the Danish Data Protection Agency (journal # 2012-58-0004 RH-2017-78, I-Suite #: 05350) and the Danish Patient Safety Authority.
Informed consent
The Danish Capital Region Regional Ethics Committee waived the need for informed consent because participation in the study was considered non-jurisdictional because the study qualified as quality assurance (protocol# H-4-2014-FSP).
Rights and permissions
About this article
Cite this article
Korshin, A., Grønlykke, L., Nilsson, J.C. et al. The feasibility of tricuspid annular plane systolic excursion performed by transesophageal echocardiography throughout heart surgery and its interchangeability with transthoracic echocardiography. Int J Cardiovasc Imaging 34, 1017–1028 (2018). https://doi.org/10.1007/s10554-018-1306-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-018-1306-4