Abstract
In idiopathic dilated cardiomyopathy (DCM), myocardial deformational parameters and their relationships remain incompletely characterized. We measured those parameters in patients with DCM, during left ventricular reverse remodeling (LVRR). Prospective study of 50 DCM patients (in sinus rhythm), with left ventricular ejection fraction (EF) <40%. LVRR was defined as an increase of ten units of EF and decrease of diastolic left ventricular diameter (LVDD) in the absence of resynchronization therapy. Performed morphological analysis, myocardial performance quantification (LV and RV Tei indexes) and LV averaged peak systolic longitudinal strain (SSR long) and circumferential strain (SSR circ). At baseline, mean EF was 25.4 ± 9.8%, LVDD was 62.4 ± 7.4 mm, LVDD/BSA of 34.2 ± 4.5 mm/m2 and 34% had MR grade >II/IV. LVRR occurred in 34% of patients within 17.6 ± 15.6 months and was associated with a reduced rate of death or heart failure hospitalization (5.9% vs. 33.3; p = 0.03). Patients with LVRR had a final EF of 48.9 ± 7.9% (Δ LV EF of 22.4%) and there was a significant decrease (p < 0.05) in: LVDD/BSA, LV systolic diameter/BSA, LV diastolic volume, LV systolic volume, LV mass; an increase (p < 0.05) in sphericity index. However, measures of diastolic function (LA volume/BSA, e′velocity and’ E/e′ratio), final LV and RV Tei indexes were not significantly different from baseline. Additionally, final SSR circ and SSR long values were not different from basal. Patients who recovered EF >50% (n = 10), SSR circ and SSR long were inferior to normal. Improvement in EF occurred in one-third of DCM pts and was associated with a decrease of major cardiac events. There was an improvement of diastolic and systolic volumes and in sphericity index, confirming truly LV reverse reshaping. However, myocardial performance indexes, SSR long and SSR circ in reverse-remodeled DCM were still abnormal, suggesting a maintained myocardial systolic and diastolic dysfunction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Progression of heart failure (HF) is associated with left ventricle (LV) remodeling, which manifests as gradual increases in left ventricular end-diastolic and end-systolic volumes, wall thinning, and a change in chamber geometry to a more spherical, less elongated shape, with a continuous decrease in ejection fraction [1 ]. When ventricular remodeling is advanced, it begins to be self-supporting and capable of conducting the progression of the disease, regardless of neurohormonal status. This explains why medical therapies lose their effectiveness in terminal HF, and some device-based therapies (cardiac resynchronization and mechanical ventricular assistance), that can affect the remodeling of the LV, have been beneficial. Left ventricular reverse remodeling (LVRR) is characterized by decrease of LV dimensions, normalization of LV shape and improvement of systolic function. A favorable response to drug therapy with ACEI, β-blockers and aldosterone antagonists was reported, with almost complete reversal of LV dysfunction. An increase in left ventricular ejection fraction (EF) of more than 15 units has been described, associated with an increase in functional capacity, an increase in cardiac index and a decrease in pulmonary capillary pressure, associated with a better prognosis [2–5]. The improvement of myocyte Ca2+ handling or the restoration of the response of down-regulated β-adrenergic receptors to sympathetic activation may play a role in normalizing EF in patients with dilated cardiomyopathy (DCM) [6]. Molecular mechanisms of reverse remodeling have not been fully elucidated.
The existence of the new-called HF with recovered ejection fraction (HF-Recovered) represents a distinct HF phenotype with biochemical properties and natural history that differs from the traditional HF population [7]. Predictors of LVRR probably discriminate patients in whom EF can recover only with medical therapy, from patients who may require cardiac devices or referring for heart transplantation.
EF is the most widely used parameter for the global assessment of LV systolic dysfunction. A combined myocardial performance index (isovolumic contraction time plus isovolumic relaxation time divided by ejection time, ‘Tei index’) has been applied in the echocardiographic evaluation of patients with DCM [8]. This index can also be obtained by tissue Doppler imaging (Tei-TDI) [9].
In recent years, novel technologies, like speckle tracking echocardiography, are useful to detect and comprehend the abnormalities that occur in cardiac diseases. LV global strain is an accurate and sensitive measure of myocardium deformation, allowing the angle-independent quantification of myocardial function in 2D, based on the LV active shortening in the longitudinal, circumferential and radial direction, which is more reproducible than EF and does not rely on geometrical assumptions [10].
There is insufficient research about regional myocardial function and strain rate analysis in patients with normalized EF after optimal pharmacologic therapy. One study demonstrated subclinical LV dysfunction by strain rate analysis at rest and during exercise in patients with normalized EFs [7] and studies on Tei index changes are only described after mechanical LVRR [11, 12]. The aim of this prospective study was to evaluate echocardiographic parameters of patients with idiopathic DCM, comparing the results after optimal pharmacologic therapy, particularly in patients with reverse-remodeled cardiomyopathy.
Methods
Study population
We included consecutive adult patients with DCM followed in a HF outpatient clinic, with a diagnosis of less than 24-month duration and with two initial values of EF of <0.40 more than 1 year apart. This study respects to a recent cohort of patients following a previous published investigation [13], conducted by the same authors.
We excluded patients with ischemic cardiomyopathy: history of myocardial infarction or angina, significant coronary artery disease more than 50% diameter narrowing in any of the major coronary arteries or their branches, positive exercise or pharmacological stress-induced perfusion abnormalities on nuclear scintigraphy or with positive ischemic gadolinium late-enhancement on cardiac magnetic resonance imaging (MRI). We also excluded patients with other secondary forms of DCM: history of moderate or severe hypertension; diabetes mellitus with end-organ damage or on insulin therapy, primary mitral or aortic valvular disease of at least moderate degree; heavy alcohol use (>100 g/day), chemotherapy-induced and peripartum cardiomyopathy. We didn’t include patients with acute HF with positive biopsy of active myocarditis, with positive serology for acute phase of bacterial or viral infection or with a cardiac MRI with a suspicion of acute myocarditis. All patients were in sinus rhythm and patients with history of uncontrolled atrial and ventricular arrhythmias were excluded.
At baseline, patients underwent clinical assessment, transthoracic echocardiogram and blood laboratory measurements. Patients were managed according to current clinical practice guidelines [14] and clinicians aimed to reach the recommended target doses for all therapies. During the follow up, periodic clinical evaluation, laboratory measurements and echocardiogram were performed on a 3–6-month basis. This study was performed in accordance with the recommendations set by the Declaration of Helsinki [15] and with the local legal requirements. Our observational study was also performed according to the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement [16].
Definition of LVRR
LVRR was defined by the simultaneous presence of the following conditions: (a) occurrence in two subsequent echocardiograms of an absolute increase of ten units of EF, concomitant with a decrease in diastolic left ventricular diameter (LVDD), without worsening of mitral regurgitation (MR), if present; (b) this increase occurred in the absence of cardiac resynchronization therapy (CRT) or mechanical ventricular assistance. Patients who received CRT were considered to have no LVRR, so we only considered in the analysis the echocardiographic parameters measured before the implantation of CRT.
Transthoracic echocardiography protocol
A standardized complete echocardiographic examination was performed, at baseline and during follow-up, using a commercially available Vivid 7 system (GE Vingmed, Horton, Norway), with a M4S (2.5-MHz) probe. Digital grayscale two-dimensional cine loops from three consecutive heartbeats were obstained from standard apical views (four chamber, two chamber, and long axis) and standard LV short-axis views (basal, mid and apical) at depths of 11 to 20 cm; frame rates were 45–90 Hz.
The chamber quantification parameters were measured according to the professional standards defined by the American Society of Echocardiography and the European Association of Echocardiography [17], EF (%) was calculated by Simpson’s biplane method; degree of mitral and tricuspid regurgitation by Doppler, scored on a scale from 0 to 4; pulmonary artery systolic pressure (PASP) was calculated by tricuspid velocities. LV mass was calculated using the formula proposed by Devereux et al. [18]. LV sphericity index was calculated as the ratio of dimensions of long axis view and minor axis view. The early diastolic (E) and atrial (A) wave velocities, the E/A ratio, and the E-wave deceleration time were measured using pulsed wave Doppler recording from the apical four-chamber view. Spectral pulsed-wave Doppler–derived early diastolic velocity (e´) was obtained from the septal and lateral mitral annulus and an average was used. E/e′ratio was calculated to obtain an estimate of LV filling pressure.
The left ventricular global myocardial index (LV Tei-index) determined was calculated as Mitral Valve Closure to Opening Time (MVCO) LV Ejection time/LV Ejection time. It was measured at the septal and lateral sites of the mitral annulus, and the average was utilized. RV myocardial performance index (RV Tei index) was determined as the difference in duration between tricuspid regurgitation and pulmonary ejection divided by pulmonary ejection duration.
Speckle-tracking circumferential strain rates were assessed from basal, mid, and apical LV short-axis views, and the longitudinal strain rate was assessed from the basal, mid, and apical levels in apical four-chamber, two-chamber, and long-axis views. For speckle-tracking strain rate analysis, the peak of the R wave on the electrocardiogram was used as the reference time point for end-diastole. The endocardial border was traced manually in the end-diastolic frame. The software subsequently automatically traced the borders in the other frames. Segments which failed to track were manually adjusted by the operator. Graphical displays of deformation parameters for each segment were then generated automatically. Circumferential and longitudinal global strain was obtained by averaging the peak strain values from the 18 regional longitudinal strain curves: SSR circ and SSR long. Normal values for SSR circ and SSR long were considered −20.9 to −27.8 and −15.9 to −22.1%, respectively, according to literature [19]. All data were stored digitally for off-line analysis on Echo-Pac PC software (7.3.0 GE, Horton Norway) and was performed by two echocardiography specialists, blinded to the study.
Statistical analysis
All values are reported as mean ± SD, median ± interquartile range or as percentages according to characteristics of data. Differences between subjects in each arm were assessed using Χ2 test for categorical variables and Student’s t-test or Mann–Whitney test for continuous variables, as appropriate. A two-tailed p < 0.05 was considered to indicate statistical significance.
To evaluate changes from baseline a paired Student’s t-test was used. Data were analysed using SPSS 23.0 statistical package (SPSS Inc., Chicago, IL, USA).
Results
We studied 50 patients, 28 men (56%), aged 59 ± 10 years, followed for 39 ± 22 months. The majority of patients were in NYHA class II (62%). Sixty percent of patients performed coronariography and 78% of patients performed cardiac MRI to rule out ischemic cardiomyopathy or myocarditis.
On EKG, 66% had left bundle branch block (LBBB), 22% had LV hypertrophy criteria and all were in sinus rhythm.
At the end of the follow-up, 94% were treated with angiotensin-converting enzyme inhibitors (ACEI)/ angiotensin II receptor blockers (ARB), 98% with β-blockers, 60% with aldosterone antagonists. Optimal recommended doses of ACEI/ARB were reached in 42% (20–30 mg lisinopril, 5–10 mg perindopril, 16–32 mg candesartan) and optimal doses of β-blockers were reached in 48% (25–50 mg bid carvedilol, 5–10 mg bisoprolol). Only 4% died (2 deaths), 22% were hospitalized for HF worsening and 48% implanted cardiac devices: implantable cardiac defibrillator (ICD) in 40%, CRT plus ICD in 8%.
At baseline, mean left ventricular EF was 25.4 ± 9.8%, LVDD was 62.4 ± 7.4 mm, LVDD/BSA of 34.2 ± 4.5 mm/m2 and MR grade >II/IV was present in 34% of patients.
Left ventricular reverse remodeling (LVRR)
LVRR occurred in 34% of patients (n = 17) within 17.6 ± 15.6 months of medical therapy. Mean time interval between baseline and final echocardiogram was 38.5 ± 21.9 months. Between groups (LVRR or no LVRR) there was no difference of mean time of follow-up echocardiograms (43.9 ± 2.4 vs. 35.8 ± 22.0; p = 0.21). The initial LVEF of patients who recovered LV function was 24.9 ± 9.0% and was not different from the value of 26.5 ± 11.2% (p = 0.58) of those who did not recover.
We found that patients who recovered LV function had, at baseline: younger age (54.7 ± 10.8, vs. 60.6 ± 8.8; p = 0.05) and smaller LVDD/BSA (mm/m2) (32.3 ± 4.8 vs 35.2 ± 4.1, p = 0.03). See Tables 1 and 2 for further details.
Patients that had LVRR had a lower BNP at the end of follow-up (36.9 ± 34.3 vs. 143.5 ± 137.5; p < 0.01) and less major cardiac events (death or HF hospitalization) (5.9% vs. 33.3; p = 0.03), compared to those that didn’t have LVRR. In these patients, the heart rate decreased significantly during follow-up (67.6 ± 19.1 vs. 73.9 ± 11.7 bpm, p = 0.02), probably related to the effect with β-blockers. However, LBBB rate and QRS duration didn’t change from baseline (58.8% vs. 47.1, p = 0.50; 136.1 ± 34.9 vs. 133.7 ± 35.2, p = 0.66, respectively).
Patients with LVRR had a final EF of 48.9 ± 7.9% (Δ LV EF of 22.4%), and had a significant decrease (p < 0.05) (see Table 3) in: LVDD (53.5 ± 6.7 mm; Δ LVDD of ± 7.2 mm), LVDD/BSA (28.3 ± 3.0 mm/m2), LV systolic diameter/BSA (20.5 ± 0.6 mm/mm2), LV diastolic volume (145.5 ± 32.7 ml), LV systolic volume (73.6 ± 25.2 ml), LV mass (233.9 ± 68.8 g); and an increase (p < 0.05) in sphericity index (1.57 ± 0.18) and only 5.9 patients (n = 1) had a final MR ≥ rade II/IV.
Controversially, in patients with reverse remodeled DCM, measures of diastolic function as LA volume/BSA, e′velocity and E/e′ratio, were not significantly different from baseline (detailed in Table 3). Also, surprisingly, there weren’t significant changes in LV Tei index from baseline (basal: 0.82 ± 0.38; final: 0.74 ± 0.23; p = 0.45). This was also true for RV Tei index (basal: 0.56 ± 0.35; final 0.39 ± 0.17; p = 0.13). Additionally, final strain values were not significantly different from basal: SSR circ: −8.48 ± 2.85 vs. −4.80 ± 4.02%; p = 0.31, SSR long: −10.27 ± 3.77% vs. − 13.06 ± 2.90%; p = 0.08.
Comparing patients with LVRR and no LVRR, there weren’t significant differences in final LV Tei index (0.75 ± 0.22 vs. 0.85 ± 0.23 p = 0.15), in final SSR circ (−10.0 ± 4.2% vs. −8.2 ± 3.1%, p = 0.17) and in SSR long (−12.5 ± 3.0 vs. 11.5 ± 4.2%, p = 0.40).
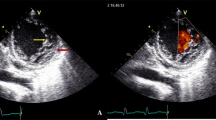
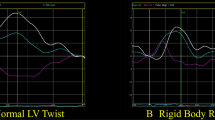
In the group of patients who improved EF ≥50% (n = 10), SSR circ was substantially inferior to normal (−10.0 ± 4.1%) and SSR long was also inferior, although close to normal values (−13.1 ± 3.5%). See Table 4 for further details. In Fig. 1 there is an example of a patient with LVRR who improved EF to 56%, but still have a diminished SSR circ and SSR long.
A subgroup analysis in patients with LVRR and hypertension revealed that final SSR circ was significantly lower (−7.68 ± 3.05% vs. − 10.74 ± 3.77%; p = 0.01), compared to patients without hypertension. We didn’t find differences in another strain rate parameters. The subgroup analysis of basal and final strain rates in patients with diabetes didn’t show any significant differences between groups.
Discussion
HF has classically been a clinical syndrome associated with cardiac dilatation and impaired cardiac contractility. Left ventricular EF is the most extensively investigated echocardiographic systolic function parameter and has been established as a powerful predictor of mortality for patients with HF. The myocardial performance index is a Doppler-derived time interval index that combines both systolic and diastolic cardiac performance. The Tei index is easily derived using conventional pulsed Doppler echocardiography, as previously described by Tei and colleagues [8]. The mean normal value of the Tei index is 0.39 ± 0.05 for the LV, while for the right ventricle (RV) it is 0.28 ± 0.04 [8, 20]. Higher index values correspond to more pathological states with overall cardiac dysfunction. The Tei index appears to have close correlation with the widely accepted systolic and diastolic hemodynamic parameters, is a useful method for the study of congestive HF syndrome and has been shown to have strong prognostic value in severe cardiac diseases, such as DCM. A study of Dujardin et al. [21] showed that Tei index and EF were the most significant independent predictors of outcome in patients with DCM. Ikeda et al. [22] demonstrated that patients with DCM and cardiac events had higher LV and RV Tei indexes at the initial follow-up examination; and RV Tei index had a significant linear correlation with LV Tei index. The 6-year survival rate was significantly lower in patients with both LV Tei index ≥ 0.78 and RV Tei index ≥ 0.49 than in other patients [22]. In our study, there was a decrease in RV and LV Tei indexes in patients that had recovery in EF, but didn’t reach normal values, indicating that those patients have risk of cardiac events and maintained systolic and diastolic dysfunction.
Experimental and clinical studies showed that LV systolic function is a complex, coordinated action involving longitudinal contraction, circumferential shortening, and radial thickening [23]. Strain rate imaging has a theoretic advantage over Doppler tissue imaging that is relatively immune to cardiac translational motion and tethering [24]. Myocardial strain is comprised by three components: longitudinal, circumferential and radial, disposed in a complex helicoid arrangement, in order to facilitate the ejection and suction of the blood [25]. It is well established that the longitudinal cardiac fibres located in the subendocardium are the first to be affected by myocardial injury [24]. Several authors showed that global strain is a powerful predictor of cardiac events and appears to be a better parameter than EF in patients with HF [26–28]. Circumferential and longitudinal speckle-tracking strain rate analysis can be useful to detect subclinical myocardial systolic and diastolic dysfunction.
In our population, measures of diastolic function, myocardial performance indexes, longitudinal and circumferential strain rate analysis with reverse-remodelled DCM were impaired and were not different from baseline. Additionally, in patients who improved LVEF to normal values, circumferential and longitudinal SSR were still impaired. Thus, multidirectional myocardial analysis may well be important for a better understanding of subclinical myocardial dysfunction in patients with HF. These findings suggest that in treated patients with DCM with reverse remodelling, left ventricular mechanics may not be normal, even when EFs are normal.
Another finding was that in patients with LVRR, LBBB rate and QRS duration didn’t change from baseline, and this may contributed to the absence of changes in Tei indexes or global strain parameters. We also found that patients with LVRR and hypertension (although of mild degree) had a lower final SSR circ; this is consistent with other studies that showed that hypertension may contribute to subtle LV dysfunction and affect strain rate parameters [29].
Remains unclear, however, what are the predictors of adverse outcome in patients with reverse-remodelled DCM, defined as depressed left ventricular EF, and normalized after optimal pharmacologic therapy. One study showed that LVRR was a favourable prognostic indicator in patients with DCM irrespective of its detection timing (early vs. late >24 months recovery) [30]. The Penn Heart Failure Study [31], which included of 1821 chronic HF patients divided in three categories based on echocardiograms: HF-reduced EF (HF-REF) if EF was <50%, HF preserved EF (HF-PEF) if EF was consistently ≥50%, and HF-Recovered if EF on enrolment in PHFS was ≥50%, but prior EF was <50%; showed that HF-Recovered is associated with a better event-free survival than HF-REF and HF-PEF. However, these patients continued to experience a significant number of HF hospitalizations, suggesting persistent HF risk. These authors demonstrated that HF-Recovered patients had abnormal BNP, uric acid, ST2, and sFlt-1 and nearly half had detectable troponin I, indicating that there is persistent neurohormonal activation, increased oxidative stress, and cardiomyocyte injury and stress, despite apparent recovery of EF. These findings provide a rationale to continue background medical or device therapy for HF-Recovered patients. The recurrence was significantly correlated with the discontinuation of heart failure drugs [32]. These results suggest that continuous medical therapy may be mandatory in patients who recover from LV systolic dysfunction.
Study limitations
This study englobes a small number of patients at a single center, so future studies of larger populations may elucidate findings of subclinical systolic and diastolic dysfunction in patients with LVRR. We didn’t perform radial strain or LV torsion due to software limitations; those parameters may be important for the comprehension of the mechanism of reverse remodeling in DCM patients.
Conclusions
Improvement in EF occurred in 34% of DCM pts and was associated with better capacity, lower BNP, a decrease in diastolic and systolic volumes and in sphericity index, confirming truly LV reverse reshaping. However, more sensitive measures like myocardial performance and tissue deformational indexes did not show significant changes.
Therefore, measurements of both regional myocardial systolic and diastolic function as assessed by circumferential and longitudinal speckle-tracking strain rates may be very helpful for understanding subtle LV myocardial dysfunction that cannot be detected by conventional echocardiographic parameters such as EF in patients with reverse-remodeled DCM.
References
Cohn JN, Ferrari R, Sharpe N (2000) Cardiac remodeling–concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. Behalf of an International Forum on cardiac remodeling. J Am Coll Cardiol 35(3):569–582
Groenning BA, Nilsson JC, Sondergaard L, Fritz-Hansen T, Larsson HB, Hildebrandt PR (2000) Antiremodeling effects on the left ventricle during beta-blockade with metoprolol in the treatment of chronic heart failure. J Am Coll Cardiol 36(7):2072–2080
Greenberg B, Quinones MA, Koilpillai C, Limacher M, Shindler D, Benedict C et al (1995) Effects of long-term enalapril therapy on cardiac structure and function in patients with left ventricular dysfunction. Results of the SOLVD echocardiography substudy. Circulation 91(10):2573–2581
Arnold RH, Kotlyar E, Hayward C, Keogh AM, Macdonald PS (2003) Relation between heart rate, heart rhythm, and reverse left ventricular remodelling in response to carvedilol in patients with chronic heart failure: a single centre, observational study. Heart 89(3):293–298
Boccanelli A, Mureddu GF, Cacciatore G, Clemenza F, Di Lenarda A, Gavazzi A et al (2009) Anti-remodelling effect of canrenone in patients with mild chronic heart failure (AREA IN-CHF study): final results. Eur J Heart Fail 11(1):68–76
Kubo H, Margulies KB, Piacentino V 3rd, Gaughan JP, Houser SR (2001) Patients with end-stage congestive heart failure treated with beta-adrenergic receptor antagonists have improved ventricular myocyte calcium regulatory protein abundance. Circulation 104(9):1012–1018
Lupon J, Gaggin HK, de Antonio M, Domingo M, Galan A, Zamora E et al (2015) Biomarker-assist score for reverse remodeling prediction in heart failure: the ST2-R2 score. Int J Cardiol 184:337–343
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ et al (1995) New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function–a study in normals and dilated cardiomyopathy. J Cardiol 26(6):357–366
Su HM, Lin TH, Voon WC, Lee KT, Chu CS, Yen HW et al (2006) Single-beat differentiation among left ventricular filling patterns by pulsed wave Doppler echocardiography. J Am Soc Echocardiogr 19(3):274–279
Marwick TH (2006) Measurement of strain and strain rate by echocardiography: ready for prime time? J Am Coll Cardiol 47(7):1313–1327
Yu CM, Lin H, Fung WH, Zhang Q, Kong SL, Sanderson JE (2003) Comparison of acute changes in left ventricular volume, systolic and diastolic functions, and intraventricular synchronicity after biventricular and right ventricular pacing for heart failure. Am Heart J 145(5):E18
Soliman OI, van Dalen BM, Theuns DA, ten Cate FJ, Nemes A, Jordaens LJ et al (2009) The ischemic etiology of heart failure in diabetics limits reverse left ventricular remodeling after cardiac resynchronization therapy. J Diabetes Complicat 23(5):365–370
Amorim S, Campelo M, Martins E, Moura B, Sousa A, Pinho T et al (2016) Prevalence, predictors and prognosis of ventricular reverse remodeling in idiopathic dilated cardiomyopathy. Revista portuguesa de cardiologia 35(5):253–260
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, Dickstein K et al (2012) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the european society of cardiology. Developed in collaboration with the heart failure Association (HFA) of the ESC. Eur Heart J 33(14):1787–1847
Puri KS, Suresh KR, Gogtay NJ, Thatte UM. (2009) Declaration of Helsinki, 2008: implications for stakeholders in research. J Postgrad Med.55(2):131–134
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 147(8):573–577
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 1–39(1):e14
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I et al (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57(6):450–458
Yingchoncharoen T, Agarwal S, Popovic ZB, Marwick TH (2013) Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr 26(2):185–191
Tei C, Dujardin KS, Hodge DO, Bailey KR, McGoon MD, Tajik AJ et al (1996) Doppler echocardiographic index for assessment of global right ventricular function. J Am Soc Echocardiogr 9(6):838–847
Dujardin KS, Tei C, Yeo TC, Hodge DO, Rossi A, Seward JB (1998) Prognostic value of a Doppler index combining systolic and diastolic performance in idiopathic-dilated cardiomyopathy. Am J Cardiol 82(9):1071–1076
Ikeda R, Yuda S, Kobayashi N, Nakahara N, Nakata T, Tsuchihashi K et al (2001) [Usefulness of right ventricular Doppler index for predicting outcome in patients with dilated cardiomyopathy]. J Cardiol 37(3):157–164
Okada M, Tanaka H, Matsumoto K, Ryo K, Kawai H, Hirata K-i (2012) Subclinical myocardial dysfunction in patients with reverse-remodeled dilated cardiomyopathy. J Am Soc Echocardiogr 25(7):726–732
Yip G, Abraham T, Belohlavek M, Khandheria BK (2003) Clinical applications of strain rate imaging. J Am Soc Echocardiogr 16(12):1334–1342
D’Hooge J, Heimdal A, Jamal F, Kukulski T, Bijnens B, Rademakers F et al (2000) Regional strain and strain rate measurements by cardiac ultrasound: principles, implementation and limitations. Eur J Echocardiogr 1(3):154–170
Cho GY, Marwick TH, Kim HS, Kim MK, Hong KS, Oh DJ (2009) Global 2-dimensional strain as a new prognosticator in patients with heart failure. J Am Coll Cardiol 54(7):618–624
Stanton T, Leano R, Marwick TH. Prediction of all-cause mortality from global longitudinal speckle strain: comparison with ejection fraction and wall motion scoring. Cir Cardiovasc Imaging. 2009;2(5):356–64
Nahum J, Bensaid A, Dussault C, Macron L, Clemence D, Bouhemad B et al (2010) Impact of longitudinal myocardial deformation on the prognosis of chronic heart failure patients. Circ Cardiovasc Imaging 3(3):249–56
Mottram PM, Haluska B, Leano R, Cowley D, Stowasser M, Marwick TH (2004) Effect of aldosterone antagonism on myocardial dysfunction in hypertensive patients with diastolic heart failure. Circulation 110(5):558–565
Ikeda Y, Inomata T, Iida Y, Iwamoto-Ishida M, Nabeta T, Ishii S et al (2016) Time course of left ventricular reverse remodeling in response to pharmacotherapy: clinical implication for heart failure prognosis in patients with idiopathic dilated cardiomyopathy. Heart Vessels 31(4):545–554
Basuray A, French B, Ky B, Vorovich E, Olt C, Sweitzer NK et al (2014) Heart failure with recovered ejection fraction: clinical description, biomarkers, and outcomes. Circulation 129(23):2380–2387
Moon J, Ko YG, Chung N, Ha JW, Kang SM, Choi EY et al (2009) Recovery and recurrence of left ventricular systolic dysfunction in patients with idiopathic dilated cardiomyopathy. Can J Cardiol 25(5):e147–e150
Funding
The funding was provided by Portuguese Society Cardiology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Amorim, S., Rodrigues, J., Campelo, M. et al. Left ventricular reverse remodeling in dilated cardiomyopathy- maintained subclinical myocardial systolic and diastolic dysfunction. Int J Cardiovasc Imaging 33, 605–613 (2017). https://doi.org/10.1007/s10554-016-1042-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-016-1042-6