Abstract
Recently, longitudinal stent deformation (LSD) has been reported increasingly. Even though the reported cases included almost all stent designs, most cases were seen in the Element™ stent design (Boston Scientific, Natick, MA, USA). It is considered that stent design, lesion and procedural characteristics play a role in the etiology of LSD. Yet, the effect of LSD on long-term clinical outcomes has not been studied well. Element stents implanted between January 2013 and April 2015 in our hospital were examined retrospectively. Patients were grouped into two according to the presence of LSD, and their clinical, lesion and procedural characteristics were studied. Twenty-four LSD’s were detected in 1812 Element stents deployed in 1314 patients (1.83 % of PCI cases and 1.32 % of all Element stents). LMCA lesions (16.7 % vs 1.6 %, p < 0.001), complex lesions (75 % vs 35.1 %, p < 0.001), bifurcation lesions (37.5 % vs 18.3 %, p = 0.017), ostial lesions (33.3 % vs 12.8 %, p = 0.003), using of extra-support guiding catheter (54.2 % vs 22.3 %, p < 0.001) and extra-support guidewire (37.5 % vs 16.2 %, p = 0.005) were found to be more frequent in cases with LSD than in cases without it. In addition, the number of stents, stent inflation pressure and the use of post-dilatation were significantly different between the two groups. Two patients had an adverse event during the follow-up period. LSD is a rarely encountered complication, and is more common in complex lesions such as ostial, bifurcation and LMCA lesions. The use of extra-support guiding catheter, extra-support guidewires and low stent inflation pressure increases the occurrence of LSD. Nevertheless, with increased awareness of LSD and proper treatment, unwanted long-term outcomes can be successfully prevented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the first coronary angioplasty, almost every innovation in the field of invasive cardiology has been a revolutionary innovation compared to the previous one. Nevertheless, every innovation has its own problem either trifle or troublesome. Plain old angioplasty aroused great interest in coronary revascularization but dissection, acute recoil and high restenosis rates have led to the routine use of bare metal stents (BMS). Despite the low dissection and acute recoil rate of BMS, the high instent restenosis (ISR) rate in the long term has called for the search of better stents. Although ISR rates have become better with the first generation drug eluting stents (DES), concerns about late stent thrombosis (ST) have loomed large. The main objective of new stent designs is to minimize the ST and ISR rates and to maximize the procedural success rate. In this respect, the usage of cobalt–chromium and platinum–chromium instead of steel, thinner stent struts, modification of stent designs with fewer connectors between the hoops have been tried, without sacrificing the radial and longitudinal strength, for maximal conformability, flexibility, traceability, deliverability, radio-opacity and easier side branch access. In addition, different anti-proliferative agents have been used [1, 2].
Better clinical outcomes have been achieved with these innovations but there has been a recent increase in case reports and case series regarding longitudinal deformation of newer stent designs. Even though the reported cases included almost all stent designs, the majority of cases were seen in the Element™ stent design (Boston Scientific, Natick, MA, USA) [3, 4]. Results of bench test evaluating longitudinal stent deformation (LSD) of different stent designs have also been published [5−7]. In the current study, clinical, anatomical and procedural characteristics of cases where LSD was seen were examined, and ISR and ST rates in the long-term follow-up period were evaluated.
Methods
Patients who underwent percutaneous interventions and had at least one Promus Element (Boston Scientific, Natick, MA, USA) or Taxus Element (Boston Scientific, Natick, MA, USA) stent implanted in Kosuyolu Cardiovascular Research and Education Hospital between January 2013 and April 2015 were included in the study. Antiplatelet, anticoagulant and other therapies before, during and after all percutaneous coronary interventions (PCI) were done according to the current guidelines [8, 9]. All clinical, laboratory and demographic properties of the patients were recorded from hospital files and computer records. Angiographic data were reviewed retrospectively by six competent interventional cardiologists in terms of lesion and procedural characteristics. LSD is defined as the deformation or shortening of stent in the longitudinal axis at later stages of stenting procedures in the initial absence of any shortening or increase in radio-opacity or deformation in the proximal or distal segment of the freshly implanted stent, and a total of 1812 stents (1555 Promus Element stents and 257 Taxus Element stents) used in 1333 interventions in 1314 patients were examined. LSD was detected in 24 patients. The angiographic images of all 24 cases with LSD were reviewed and confirmed by three competent interventional cardiologists. Patients were divided into two groups according to the presence of LSD, and clinical and angiographic data between the two groups were compared. Patients with LSD were evaluated for ST and ISR by hospital data and telephone calls. All work was done in compliance with the declaration of Helsinki, and the study was performed with the approval of local ethics committee.
Statistical analysis
Continuous variables were shown using mean ± standard deviation or medians (with ranges) as appropriate, and categorical variables were described using frequencies and percentages. p < 0.05 was taken as significant. Independent samples t test or Mann–Whitney U test was used to compare continuous variables. Categorical variables were compared using Chi square test (χ2) as appropriate. Odds ratios (OR) with 95 % confidence intervals (95 % CI) were calculated for variables with significant p value in univariate analysis. Statistical analyses were performed using SPSS version 15.0 (SPSS for Windows, version 15.0; SPSS Inc., Chicago, IL, USA).
Results
Twenty-four LSD’s (23 Promus Element stents and 1 Taxus Element stent) were detected in a total of 1812 Element stents (1555 Promus Element stents and 257 Taxus Element stents) deployed in 1314 patients (1.83 % of PCI cases and 1.32 % of all Element stents). The clinical and laboratory characteristics are shown in Table 1. Left main coronary artery (LMCA) lesions [16.7 % vs 1.6 %, p < 0.001, OR 12.13 (95 % CI 3.9–37.72)], complex lesions (AHA/ACC type B2 or C) [75 % vs 35.1 %, p < 0.001, OR 5.54 (95 % CI 2.19–14.03)], bifurcation lesions [37.5 % vs 18.3 %, p = 0.017, OR 2.67 (95 % CI 1.16–6.16)] and ostial lesions [33.3 % vs 12.8 %, p = 0.003, OR 3.4 (95 % CI 1.44–8.04)] were found to be more frequent in cases with LSD than in cases without it. As for interventional characteristics, the uses of extra-support guiding catheter [54.2 % vs 22.3 %, p < 0.001, OR 4.11 (95 % CI 1.83–9.25)] and extra-support wire 37.5 % vs 16.2 %, p = 0.005, OR 3.1 (95 % CI 1.34–7.15) were higher in patients with LSD. In addition, the number of stents [2 (1–3) vs 1 (1–4), p < 0.001, OR 2.67 (95 % CI 1.67–4.26)], stent inflation pressure [15 (12–20) vs 17 (12–25), p = 0.011, OR 0.85 (95 % CI 0.74–0.98)] and the use of post-dilatation [100 % vs 62.9 %, p = 0.005, OR 1.59 (95 % CI 1.54–1.65)] were significantly different between the two groups (see Table 2). The apparent causes of LSD were as follow; re-crossing of post-dilatation balloon in ten patients, deep intubation and/or manipulation of guiding catheter in six patients, re-crossing with a second stent in four, crossing of a side-branch balloon in two, crossing of side-branch stent in one and the use of GuideLiner® in one patient (see Table 3; Figs. 1, 2, 3, 4). Optimal stent expansion and plaque coverage was achieved only by post-dilatation with non-compliant balloon in 18 patients whereas additional stenting was needed in six patients.
a Angiographic image of a long segment stenosis of RCA. After pre-dilatation, a 275 × 38 mm Promus Element stent was implanted to the distal and a 275 × 32 mm Promus Element stent was implanted to the proximal in an overlapping manner. b No stent deformation in the proximal RCA. During the withdrawal of stent balloon, deep engagement of guiding catheter occurred, and compressed the proximal stent struts. It was post-dilated with a 3.0 × 20 mm balloon and optimal result was obtained. c, d Final images
a Angiographic image of LCx bifurcation lesion. After pre-dilatation, a 275 × 24 mm Promus Element stent was deployed (b, c) using provisional approach. Kissing post-dilatation to the side branch was planned. After re-wiring, a balloon was passed uneventfully to the side-branch but the balloon to the main vessel got stuck to the stent struts and deformation occurred (d, e). f Angiography after final dilatation
a Angiographic appearance of a tortuous, severely stenosed LCx. Pre-dilatation balloon could not pass and Guideliner® was used for pre-dilatation (b). Subsequently, a 2.5 × 32 mm Promus Element stent was deployed (c). Upon withdrawal of stent balloon, deep engagement of Guideliner® caused crushing of the proximal stent (arrows) (d, e). The crushed segment was dilated with a 2.75 × 12 mm balloon. There was haziness in segment proximal to the stent and a 275 × 16 mm Promus Element stent was deployed in an overlapping manner. Final angiographic result was seen on f
a 2.25 × 32 mm Promus Element stent was deployed to a long CTO segment of LAD. At the distal part, flow-limiting edge dissection was noted after stenting, and a second stent was planned (a). On b, normal stent proximal segment is seen without any deformation. The second stent got stuck in the proximal segment of the first stent and LSD occurred (c). After stenting of distal segment, proximal stent was post-dilated with a 2.5 × 15 mm balloon. On d, final angiographic image was seen. After 7 months, the patient presented with exertional angina, and coronary angiography showed diffuse ISR of distal stent and restenosis of the proximal stent especially at the deformed region. CABG was planned
Two patients had an adverse event during the follow-up period (mean 13.6 months, range 1–28 months). A 71-year-old female died of gastrointestinal bleeding in the 3 month of follow-up. A 65-year-old man had angina episodes in the 7 month, and underwent by-pass surgery because of diffuse ISR of left anterior descending (LAD) artery. Other patients did not have any adverse event during the follow-up period.
Discussion
The main findings of our study are as follow: (i) LSD is a rare phenomenon in Element stent design (1.83 % of PCI cases and 1.32 % of all Element stents); (ii) in terms of lesion characteristics, LSD is more frequent in LMCA, ostial, bifurcation and complex lesions, in terms of procedural characteristics, LSD is related with the use of extra-support guiding catheter, extra-support guidewires, use of more than one stents and post-dilatation, and lower stent inflation pressure; (iii) the guidewire bias during post-dilatation or passage of a second stent is an important factor in LSD, and extra-support guidewire also increases LSD and (iv) with appropriate treatment, acute and long-term adverse events can be minimized in LSD.
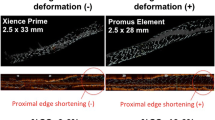
LSD has been described as longitudinal distortion or shortening of the stent in the longitudinal axis [10]. Even though LSD is generally seen in the proximal segment, distal LSD has also been reported. General angiographic appearance of the shortening of proximal end of the stent is like a wedding band due to strut overlap. In literature, it has also been termed as the “longitudinal stent compression”, “concertina effect” or “accordion effect”. When suspected angiographically, intravascular ultrasound (IVUS) or optical coherence tomography (OCT) can be of use. Collapse of struts and malapposition can be seen in this shortened stent segment. Although LSD has been increasingly reported in recent years, it still is a rare complication. In a case series with 9310 stents of different stent designs by Williams et al., LSD was seen in 0.097 % of stents and 0.2 % of patients in nine cases over a 4 year period. Authors reported LSD in six Promus Element stents (0.86 %), one TAXUS stent (0.19 %), one Biomatrix stent (0.11 %) and one Endeavor stent (0.1 %), and LSD was not reported in other various stent types [3]. Mamas et al. stated in their analysis of Food and Drug Administration Manufacturer and User Facility Device Experience (FDA-MAUDE) database that most LSDs (45 out of 57 cases; 78.9 %) were in stents of Element platform. They further emphasized the increased rate of LSD in recent years [4]. Leibundgut et al., in their study of 1392 PCIs where 2936 Promus Element stents were placed, stated that LSD was present in 20 patients (1.44 % of the PCI cases, 0.68 % of all Promus Element stents). And they reported that ostial lesions, number of stents and the presence of bifurcation lesions were the predictors of LSD [11]. Almost all reported cases and case series have generally stated that LSD was more frequent in LMCA, ostial and bifurcation lesions, and tortuous and long segments. In addition, in terms of procedural characteristics, this complication was observed more often in the use of extra support guide catheters, aggressive guide catheter manipulation, mother and daughter catheter systems, multiple balloons, bifurcation stent techniques, rotational atherectomy and/or adjunctive imaging (IVUS or OCT) techniques [3, 4, 11, 12].
Although all of the above-mentioned factors play a role in LSD, most reported cases blamed a second material (postdilation balloon, stent, etc.) as the culprit. In fact, the second material can get stuck on the proximal stent struts if they are not well apposed. Especially when there is a substantial difference in vessel size between proximal and distal segments, stent selection is done according to distal vessel diameter, and subsequent post-dilation with a larger non-compliant balloon is performed to the proximal segment (proximal optimization) [13]. If the stent inflation pressure is kept low to avoid distal edge dissection, the malapposition of the proximal segment is very likely, and LSD can occur on the passage of post-dilatation balloon or device. In addition to inflation pressure, another significant factor we found in our study is the use of extra-support guidewires. The extra-support guidewires tend to follow the outer curve of the coronary artery causing the wire bias. A passing balloon or stent along this wire is more likely to get stuck in the stent struts, especially if they are under-expanded [14, 15].
Although LSD can be seen in all stent designs, the majority of reported cases are with the Element stent design [16]. The Element platform is an ultra-thin (81 μm) platinum–chromium scaffold, modified to improve deliverability, vessel conformability, side-branch access, radio-opacity, radial strength, and fracture resistance. Element design has a three-dimensional, double-helix configuration with segments joined by two connectors [17]. It is believed that thin strut and fewer connectors are responsible for relatively frequent occurrence of LSD. Bench testing is used to evaluate mechanical behavior of stent such as longitudinal distortion. Recent bench testing has demonstrated a correlation between the number of connectors between stent hoops and longitudinal integrity independent of strut thickness [5–7]. On the other hand, some argued that enhanced visibility of Element stent, as compared to other stents, provides easier recognition of LSD and claim this to be the reason for the high incidence of LSD in Element stents [18]. Moreover, PLATINUM, PERSEUS Workhorse and PERSEUS Small Vessel trials of the Element stent series, in which Element stent platform was used in 2034 patients, LSD was not reported. This may be because these trials excluded complex lesions [19–21].
The clinical significance is also unclear as the frequency of stent deformation was relatively low. But this complication can cause incomplete plaque coverage, dissection and luminal obstruction. LSD may also reduce scaffolding and drug delivery to the coronary vessel wall and may lead to a higher risk of ISR. Additionally, strut malapposition and metal overload may act as a facilitating factor for ST [4]. Although there have been reported cases of ST and ISR, a recently published CT angiography study involving 374 patients who underwent PCI stated that LSD and stent fracture had no effect on MACE [22].
To prevent LSD, aggressive catheter manipulation for ostial and proximal lesions and deep engagement of catheter during withdrawal of stent balloons, post-dilatation balloons or adjunctive imaging devices should be avoided. Moreover, when a second balloon or stent is passed to the distal or side-branch through a freshly-implanted stent, extra care should be taken not to get stuck to stent struts, especially if extra-support guidewires are used. An additional procedural trick to avoid LSD may be to pull back the stent balloon some mm after implantation and re-inflate the balloon to post-dilate the proximal segment more without risk of distal edge dissection. However, this maneuver is limited by the size of the proximal segment. Nonetheless, if LSD occurs, complete apposition should be rendered with gradual balloon dilatation, and additional stenting should be performed in case of edge dissection or incomplete plaque coverage.
Conclusions
LSD is a rarely encountered complication but can be seen in complex lesions such as ostial, bifurcation and LMCA lesions. The use of extra-backup guiding catheter, extra-support guidewires and low inflation pressure increases the occurrence of LSD. Nevertheless, with increased awareness of LSD and proper treatment, unwanted long-term outcomes can be successfully prevented.
Limitations
Retrospective nature of the study and the lack of definitive diagnostic criteria for LSD are the major limitations of our study. Moreover, the few number of LSD cases encountered in the study due to the rare nature of this complication may not provide sufficient information regarding the long-term outcomes (especially ISR and ST). Large-scale prospective studies are needed to definitely determine the predisposing factors of LSD and its long-term outcomes.
References
Serruys PW, Silber S, Garg S, van Geuns RJ, Richardt G, Buszman PE, Kelbaek H, van Boven AJ, Hofma SH, Linke A, Klauss V, Wijns W, Macaya C, Garot P, DiMario C, Manoharan G, Kornowski R, Ischinger T, Bartorelli A, Ronden J, Bressers M, Gobbens P, Negoita M, van Leeuwen F, Windecker S (2010) Comparison of zotarolimus-eluting and everolimus-eluting coronary stents. N Engl J Med 363:136–146
Stone GW, Midei M, Newman W, Sanz M, Hermiller JB, Williams J, Farhat N, Mahaffey KW, Cutlip DE, Fitzgerald PJ, Sood P, Su X, Lansky AJ, SPIRIT III Investigators (2008) Comparison of an everolimus-eluting stent and a paclitaxel-eluting stent in patients with coronary artery disease: a randomized trial. J Am Med Assoc 299:1903–1913
Williams PD, Mamas MA, Morgan KP, El-Omar M, Clarke B, Bainbridge A, Fath-Ordoubadi F, Fraser DG (2012) Longitudinal stent deformation: a retrospective analysis of frequency and mechanisms. EuroIntervention 8(2):267–274
Mamas MA, Williams PD (2012) Longitudinal stent deformation: insights on mechanisms, treatments and outcomes from the Food and Drug Administration Manufacturer and User Facility Device Experience database. EuroIntervention 8(2):196–204
Ormiston JA, Webber B, Webster MWI (2011) Stent longitudinal integrity. Bench insights into a clinical problem. J Am Coll Cardiol Cardiovasc Interv 4:1310–1317
Prabhu S, Schikorr T, Mahmoud T, Jacobs J, Potgieter A, Simonton C (2012) Engineering assessment of the longitudinal compression behavior of contemporary coronary stents. EuroIntervention 8:275–281
Shannon J, Latib A, Takagi K, Chieffo A, Figini F, Sacco F, Ferrarello S, Montorfano M (2013) Procedural trauma risks longitudinal shortening of the Promus Element™ stent platform. Catheter Cardiovasc Interv 81(5):810–817
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions.(2011) 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 58(24):e44–e122
Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A (2014) 2014 ESC/EACTS guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 35(37):2541–2619
Hanratty CG, Walsh SJ (2011) Longitudinal compression: a “new” complication with modern coronary stent platfroms—time to think beyond deliverability? EuroIntervention 7:872–877
Leibundgut G, Gick M, Toma A, Valina C, Löffelhardt N, Büttner HJ, Neumann FJ (2013) Longitudinal compression of the platinum-chromium everolimus-eluting stent during coronary implantation: predisposing mechanical properties, incidence, and predictors in a large patient cohort. Catheter Cardiovasc Interv 81(5):E206–E214
Seth A, Dhall A (2013) Longitudinal stent shortening: the long and short of it!! Catheter Cardiovasc Interv 81(5):818–819
Kirma C, Esen AM (eds) (2014) From diagnosis to treatment—percutaneous coronary interventions, 1st edn. Akademi yayınevi, Istabul
Colombo A, Stankovic G (2007) Problem oriented approaches in interventional cardiology, 1st edn. Informa UK Ltd., Colchester, pp 9–19
Sayar N (2014) Stenting. In Kirma C, Esen AM (eds) From diagnosis to treatment—percutaneous coronary interventions, 1st edn. Akademi yayınevi, Istabul, pp 174–186
Arnous S, Shakhshir N, Wiper A, Ordoubadi FF, Williams P, Clarke B, Mahadavan V, El-Omar M, Mamas M, Fraser D (2015) Incidence and mechanisms of longitudinal stent deformation associated with biomatrix, resolute, element, and xience stents: angiographic and case-by-case review of 1,800 PCIs. Catheter Cardiovasc Interv 86(6):1002–1011
Menown IBA, Noad R, Garcia EJ, Meredith I (2010) The platinum chromium element stent platform: from alloy, to design, to clinical practice. Adv Ther 27:129–141
Abdel-Wahab M, Sulimov DS, Kassner G, Geist V, Toelg R, Richardt G (2012) Longitudinal deformation of contemporary coronary stents: an integrated analysis of clinical experience and observations from the bench. J Interv Cardiol 25(6):576–585
Stone GW, Teirstein PS, Meredith IT, Farah B, Dubois CL, Feldman RL, Dens J, Hagiwara N, Allocco DJ, Dawkins KD, PLATINUM Trial Investigators (2011) A prospective, randomized evaluation of a novel everolimus-eluting coronary stent: the PLATINUM (a Prospective, Randomized, Multicenter Trial to Assess an Everolimus-Eluting Coronary Stent System [PROMUS Element] for the treatment of up to two de novo coronary artery lesions) trial. J Am Coll Cardiol 57:1700–1708
Allocco DJ, Cannon LA, Britt A, Heil JE, Nersesov A, Wehrenberg S, Dawkins KD, Kereiakes DJ (2010) A prospective evaluation of the safety and efficacy of the TAXUS Element paclitaxel-eluting coronary stent system for the treatment of de novo coronary artery lesions: design and statistical methods of the PERSEUS clinical program. Trials 11:1
Kereiakes DJ, Popma JJ, Cannon LA, Kandzari DE, Kimmelstiel CD, Meredith IT, Teirstein PS, Verheye S, Allocco DJ, Dawkins KD, Stone GW (2012) Longitudinal stent deformation: quantitative coronary angiographic analysis from the PERSEUS and PLATINUM randomised controlled clinical trials. EuroIntervention 8(2):187–195
Chung MS, Yang DH, Kim YH, Roh JH, Song J, Kang JW, Ahn JM, Park DW, Kang SJ, Lee SW, Lee CW, Park SW, Park SJ, Lim TH (2016) Stent fracture and longitudinal compression detected on coronary CT angiography in the first- and new-generation drug-eluting stents. Int J Cardiovasc Imaging 32(4):637–646
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Guler, A., Guler, Y., Acar, E. et al. Clinical, angiographic and procedural characteristics of longitudinal stent deformation. Int J Cardiovasc Imaging 32, 1163–1170 (2016). https://doi.org/10.1007/s10554-016-0905-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-016-0905-1