Abstract
Left ventricular strain echocardiography is reported to be more sensitive in detecting myocardial ischemia than conventional transthoracic echocardiography (TTE). We evaluated the usefulness of 2D strain analysis for the assessment of acute chest pain in emergency department (ED). Patients presenting to ED with acute chest pain were recruited. Patients with ST-elevation myocardial infarction, known coronary artery disease (CAD), non-ischemic cardiomyopathy, or non-cardiac chest pain were excluded. The pretest probability of CAD and TTEs were evaluated in all patients. TTEs included visual assessments of regional wall motion abnormality (RWMA) and analysis of global and regional longitudinal strain (GLS and RLS). The diagnosis of CAD and the occurrence of cardiac events during 1 month after ED visit were reviewed. Cardiac events were observed in 25 % of total 104 patients, and CAD was detected in 36 % of 69 patients with coronary imaging tests. Compared to RWMA, RLS showed higher sensitivity (sensitivity/specificity = 64/89 vs. 92/77 %) with similar diagnostic accuracy (79.7 vs. 82.6 %, p = 0.791) for CAD. RLS also demonstrated better diagnostic performance than either GLS (sensitivity/specificity = 92/57 %) or pretest probability (sensitivity/specificity = 72/64 %). Similarly, RLS had the higher predictive value for 1-month cardiac events. In multivariable analyses including pretest probability, LVEF, RWMA, cardiac enzyme, GLS, and RLS; only pretest probability (OR 1.91, 95 % CI 1.22–2.99, p = 0.005) and RLS (OR 25.42, 95 % CI 1.84–342.04, p = 0.016) independently predicted CAD. Strain echocardiography appears to be effective in diagnosing CAD and predicting future events with high sensitivity and negative predictive value in acute chest pain patients visiting ED.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chest pain is reported to be the second most common reason that patients present to emergency department (ED) in the US, next to abdominal pain [1]. Although the incidence of coronary artery disease (CAD) in Korea was relatively low compared with Western countries, the death rate associated with CAD has been increased in recent years [2]. The identification of patients at high risk for acute coronary syndrome in ED using conventional assessment of clinical symptoms, electrocardiogram (ECG), and cardiac enzymes is frequently challenging. The misdiagnosis or overdiagnosis of patients with acute chest pain can be associated with serious clinical events or a waste of medical resources, respectively [3–5].
Conventional transthoracic echocardiography (TTE) is known to be useful in EDs for the detection of acute myocardial infarction (MI) with a higher sensitivity than ECG [6, 7]. However, a previous study showed that TTE was not useful for detecting patients with significant CAD without infarction when performed after resolution of chest pain [8]. In addition, current guideline recommends TTE in patients with suspected myocardial ischemia as an appropriate use only if a resting TTE can be performed during pain [9]. In actual clinical practice, a large proportion of patients with chest pain visit EDs only after the resolution of symptoms that are possibly caused by transient myocardial ischemia, and the absence of regional wall motion abnormality (RWMA) on TTE does not exclude the possibility of CAD in those patients. Furthermore, the detection of RWMA on TTE is subjective and observer-dependent [10].
The assessment of left ventricular (LV) strain using two-dimensional speckle-tracking echocardiography increases the sensitivity for detecting myocardial ischemia compared to visual assessment with RWMA [11–13]. Some researchers also reported that changes in LV strain persist after transient myocardial ischemia which was resolved without residual wall motion abnormality [14, 15]. These data suggests the possible role of LV strain for the diagnosis of CAD in patients with recent myocardial ischemic insult. Using automated functional imaging (AFI) software, LV longitudinal strain can be easily analyzed online and the results are provided as a LV longitudinal strain map. However, clinical usefulness of strain echocardiography in chest pain patients in EDs has not been elucidated. Thus, we investigated the usefulness of TTE with online strain analysis for the initial assessment of acute chest pain in ED.
Methods
Study subjects and protocol
Patients who were older than 20 years and who had presented to ED with acute chest pain between January 2011 and December 2011 were prospectively enrolled in our hospital’s chest pain registry. Acute chest pain was defined as chest pain of longer than 5 min experienced within the 24 h before the ED visit. All patients were initially assessed by an ED attending physician with initial ECG, cardiac enzyme (CK-MB and Troponin I), and chest X-ray. Patients with ST-elevation MIs, unstable hemodynamic conditions, or alternative diagnoses of non-cardiac chest pain as based on the initial assessment were not included in this study (Fig. 1). Study candidates who required further cardiac evaluation underwent routine TTE including strain analysis in ED. After TTE, patients who met the following criteria were excluded from this study: (1) known CAD confirmed by previous coronary angiography (CAG) or coronary CT angiography (CCTA), (2) non-ischemic cardiomyopathy including dilated cardiomyopathy and hypertrophic cardiomyopathy confirmed by previous studies or routine TTE, (3) poor echocardiographic window, (4) significant arrhythmia, (5) severe valvular heart diseases, and (6) severe pulmonary arterial hypertension. The decision of whether to perform further tests for CAD using CCTA or CAG, or to discharge from ED was made by an ED attending physician and an on-call cardiologist, not by study protocol. If there was significant stenosis on CCTA, CAG was performed subsequently. Strain data were not provided to the ED attending physician, the on-call cardiologist, or the cardiologists who interpreted the routine TTE. Patients were monitored for any clinical events during 1 month (30 days) following the ED visit. This study was approved by the ethical committee of the Institutional Review Board at our hospital.
Study flow diagram. Patients meeting the exclusion criteria were counted in the multiple response data. ED indicates emergency department; MI myocardial infarction, CAD coronary artery disease, CM cardiomyopathy, VHD valvular heart disease, PAH pulmonary arterial hypertension, CT computed tomography
Echocardiographic examination
TTEs were performed using a Vivid Q system (GE Vingmed; Horten, Norway) with a 3.5 MHz transducer. The examinations included measurements of cardiac dimensions, volumes, and LV ejection fractions (EF) using the established guidelines of the American Society of Echocardiography. Regional LV function was evaluated and scored for each segment by visual assessment of RWMA based on the same guidelines. Peak early (E) and late (A) mitral inflow velocities and early diastolic (E′) and atrial (A′) mitral annulus velocities were measured. After standard routine echocardiography, scanning of apical 4-chamber, 2-chamber, and 3-chamber views from the apical window was performed to quantify LV strain using an M3S probe without a dual-focusing tool. The frame rate (range 60–100 frames/s) and probe frequency (range 1.7–2.0 MHz) were adjusted during the end-expiratory period for optimal image acquisition. Sector width and image depth were optimized to maintain an adequate frame rate without losing the 2D image quality. To obtain reliable strain values, three consecutive heartbeats were stored in cine-loop format. Strain analysis was done online in the ED, immediately after image acquisition, by one investigator unaware of the results of patients’ ECGs or cardiac enzymes using EchoPAC® (BT 06.6.1.0, GE Vingmed; Horten, Norway) with the AFI technique as previously described [16]. Analysis of each apical view was performed by manually identifying three points: two on each side of the mitral valve and a third at the LV apex. The software automatically detected the endocardium and created U-shaped regions of interest that encompassed the basal, mid, and apical segments of two opposite LV walls. Tracking quality was automatically assessed and we double-checked the quality visually. If necessary, we manually readjusted the endocardial tracing. The AFI software divided the LV into 18 segments and provided the peak systolic segmental longitudinal strain (SLS) in a bull’s eye format. Peak systolic global longitudinal (GLS) was calculated from the average of the segmental strains. Abnormal regional longitudinal strain (RLS) was defined as two or more adjacent abnormal segments showing a SLS value of less than the cutoff value (Fig. 2). Adjacent segments were defined as segments sharing the same plane between two segments. For example, the inferior basal segment is adjacent to the inferoseptal basal segment but not to the inferoseptal mid segment. If SLS abnormality was seen only among the apical six segments, abnormal RLS was defined as three or more adjacent abnormal SLS. We referred to the recommendation of American heart association for myocardial segments corresponding to each coronary artery and modified it for 18 segment model (supplement Figure 1) [17]. For inter- and intra-observer variability, two different sonographers acquired the two sets of echocardiographic images on the same patient (n = 10) the one after the other.
Two examples of longitudinal strain bull’s eye diagrams acquired from two patients with significant stenosis of the left anterior descending artery (left) and the right coronary artery (right), respectively. Abnormal segments with each cut-off value of −15 and −13 % (segmental longitudinal strain) are marked with dots and triangles, respectively. With cutoff values of −15 and −13 %, both cases had abnormal regional longitudinal strain (RLS) by definition
Definition of pretest probability, CAD, and event
The pretest probability of CAD provides useful information for the diagnosis of CAD [18]. We retrospectively estimated pretest probability in all patients. We took into account age, sex, and type of chest pain, along with other traditional risk factors (diabetes, hyperlipidemia, hypertension, smoking) which are known to be important determinants of disease prevalence and severity [19–21]. Chest pain was classified into three categories of Diamond: typical angina, atypical angina, and non-anginal pain [18]. Based on the age groups, sex, type of chest pain, and number of risk factors; all patients were scored on a scale of 4–19. We used this score as pretest probability. The presence of significant CAD (CAD>70) was defined as ≥70 % stenosis in one or more vessels on CAG or CCTA. One-month events included cardiac death, revascularization, acute coronary syndrome, and ED visit or hospitalization with recurrent chest pain requiring further evaluation for CAD within 1 month following the initial ED visit. Information on 1-month events was obtained from medical records of patients with follow-up visits or from telephone interviews with patients without follow-up visits after 1 month following the initial ER visit. The presence of positive cardiac enzymes was defined as any elevation of CK-MB or troponin I above the normal range. Positive RWMA was defined as the presence of at least two adjacent segments having wall motion scores of >1.
Statistical analysis
Statistical analyses were performed using IBM SPSS version 20.0. Categorical variables are presented as a number and percentage (%). The Chi square or Fisher’s exact tests were used for comparison of categorical variables. Continuous variables are expressed as mean ± SD and were compared using an independent t test or the Mann–Whitney test. Intra- and inter-observer variability was analyzed as interclass correlation (ICC) or kappa coefficients. Receiver operating characteristic (ROC) curve analysis was used to identify cutoff values to distinguish patients with CAD from controls. Generalized estimating equation was used to compare accuracy of the different diagnostic methods for CAD. For multivariable logistic regression analyses, variables with significant p values on univariable analyses as well as other clinically important variables were included into the models in order to compare prediction of CAD among diagnostic tools. A two-tailed p value of <0.05 was considered statistically significant.
Results
Patients and clinical characteristics
One hundred and eighty-six patients who presented to ED with acute chest pain were selected as study candidates excluding patients satisfying initial exclusion criteria (Fig. 1). Routine TTE was performed in all 186 patients. However, 40 patients (22 %) were excluded from strain analysis because of poor echo window (n = 21), significant arrhythmia (n = 17), or poor patient cooperation (n = 2) which prevented precise evaluation. Therefore, 146 patients (78 %) among the initial study candidates were feasible candidates for online strain analysis in ED. Following obtaining a history and routine TTE, additional 40 patients (22 %) with known CAD, non-ischemic cardiomyopathy, or severe cardiac disease other than CAD were excluded. Of the remaining patients, two were lost to follow-up. Total 104 patients (mean age 55 ± 14 years; 64 males) were finally included and 26 patients had a 1-month event (no cardiac death, 21 revascularization, 3 unstable angina, and 2 acute MI). Sixty-nine patients underwent CCTA (n = 52), CAG (n = 33), or both (n = 16). Out of the 69 patients, 25 patients (36 %) were found to have significant CAD and they also had 1-month events. Thirty-seven patients were discharged from ED without CCTA or CAG. Among these, one patient (3 %) had a 1-month event (Fig. 1). The clinical characteristics presented in Table 1 were compared between the positive-event group and the negative-event group. Heart rate and blood pressure were not different in the two groups. In the positive-event group, the mean age (60 ± 10 vs. 53 ± 15 years, p = 0.017), the proportion of male patients (85 vs. 54 %, p = 0.005) and the proportion of active smoker (50 vs. 19 %, p = 0.002) were all significantly higher. The proportion of hypertension, diabetes, dyslipidemia, and CRF was not significantly different between two groups. Typical chest pain was observed more frequently in the positive-event group. The pretest score in the positive-event group was also significantly higher (12 ± 3 vs. 10 ± 3, p < 0.001).
Echocardiographic characteristics
The echocardiographic characteristics of the patients are presented in Table 2. As expected, LV EF was lower in the positive-event group (54.7 ± 11.3 vs. 62.1 ± 6.4, p = 0.003). Among other conventional echocardiographic parameters, LV end-diastolic dimensions (50.7 ± 4.3 vs. 48.4 ± 4.4, p = 0.026), LV end-systolic dimensions (32.7 ± 5.7 vs. 29.4 ± 3.3, p = 0.010), and LV mass index (99.4 ± 25.5 vs. 85.0 ± 16.8, p = 0.001) were significantly larger in the positive-event group compared to the negative-event group. A lower e’ velocity and a higher E/e′ ratio were also observed in the positive-event group. RWMA was detected by visual assessment in 23 (22 %) patients, and 16 (73 %) of these patients experienced an event.
Strain analysis including image acquisition usually took 2–5 min. Mean GLS was −17.6 ± 3.0 % in all study patients. The positive-event group had a mean GLS of −14.6 ± 2.8 % and the negative-event group had a mean GLS of −18.5 ± 2.5 (p < 0.001). We showed RWMA and abnormal RLS compared with significantly stenotic coronary arteries in Supplement Table 1. The sensitivity and specificity of RWMA and abnormal RLS for a stenotic coronary artery were shown in Supplement Table 2. Intra- and inter-observer variability for GLS (ICC) was 0.99 (95 % CI 0.96–1.00, p < 0.001) and 0.98 (95 % CI 0.92–0.99, p < 0.001). Intra- and inter-observer variability for RLS (ICC) was 0.95 (95 % CI 0.80–0.99, p < 0.001) and 0.90 (95 % CI 0.44–0.97, p = 0.001). Inter- and intra-observer variability to determine presence of RWMA was 0.894 and 1.000 as kappa coefficient (p < 0.001).
Diagnostic performance of strain echocardiography
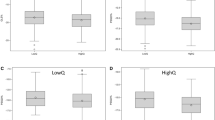
ROC curves for LVEF, pretest probability, and GLS are presented along with plots of sensitivity and specificity for RLS and RWMA, which are categorical variables (Fig. 3). The area under the curve (AUC) for GLS for CAD>70 was 0.83 (95 % CI 0.73–0.93, p < 0.001), which was higher than the AUCs for LVEF (0.75, 95 % CI 0.62–0.88, p = 0.001) and pretest probability (0.73, 95 % CI 0.61–0.86, p = 0.001) (Fig. 3, left). However, the difference of AUCs for GLS, LVEF, and pretest probability was not statistically significant (GLS vs. LVEF, p = 0.217; GLS vs. pretest probability, p = 0.217; LVEF vs. pretest probability, p = 0.249). The plot of sensitivity and specificity for RLS is shown with cutoff values of −11, −12, −13, −14, and −15 %. Table 3 shows the details of RLS diagnostic performance at the five consecutive cutoff points. The plot for RLS shows a left and upward shifted graph compared to the ROC curve of GLS, indicating better diagnostic power for RLS compared to GLS. The largest sum of sensitivity and specificity for CAD>70 was observed at cutoff values of −13 % for RLS, −17.8 % for GLS, and 11 for pretest probability. The graphs for a cardiac event (Fig. 3, right) are very similar with those for CAD>70. The AUCs for LVEF, pretest probability and GLS for a cardiac event were 0.72 (95 % CI 0.59–0.84, p < 0.001), 0.78 (95 % CI 0.68–0.88, p < 0.001) and 0.84 (95 % CI 0.76–0.93, p < 0.001), respectively. The plot of RLS for a cardiac event also demonstrates a left and upward shifted graph compared to the graphs of GLS. The optimal cutoff values for RLS, GLS, and pretest probability for a cardiac event were same as those for CAD>70. Table 4 details the diagnostic performances for CAD>70 for pretest probability, cardiac enzymes, RWMA, GLS, and RLS. The values are presented at the optimal cutoff points for pretest probability, GLS, and RLS (11, −17.8, and −13 %, respectively). Although the accuracy among the different methods was not different (p = 0.095), the sensitivity of GLS and RLS (both 92.0 %) was much higher than the sensitivity of positive RWMA (64 %). The specificities of GLS and RLS (56.8 and 77.3 %, respectively) were lower than that of positive RWMA (88.6 %). The prediction of CAD among diagnostic tools was also compared using multivariable analyses (Table 5). In model 1, pretest probability, RWMA, cardiac enzyme, and GLS were significant. When RLS was added in model 1 instead of GLS (model 2), only pretest probability and RLS showed significant prediction of CAD. In model 3 including both GLS and RLS, pretest probability [Odds ratio (OR) 1.91, 95 % confidence interval (CI) 1.22–2.99, p = 0.005] and RLS (OR 25.42, 95 % CI 1.84–342.04, p = 0.016) still showed significance.
Receiver operating characteristic curves for LV EF, pretest probability, and global longitudinal strain and graphs of sensitivity and specificity for regional longitudinal strain and regional wall motion abnormality. Left graphs was shown in 69 patients who underwent coronary angiography or coronary CT angiography. Right graphs was shown in 104 patients who followed up for 1 month after visit to emergency department
Discussion
In the present study, we investigated the usefulness of TTE including online longitudinal strain analysis in evaluating acute chest pain in ED for significant CAD. RLS had higher sensitivity for CAD with similar accuracy compared with RWMA. Approximately 80 % of patients with acute chest pain who required further evaluation for CAD were feasible for performing strain echocardiography with online analysis in ED. Recent studies have shown that both RLS and GLS have diagnostic value for CAD and that the diagnostic accuracy of strain echocardiography in patients with chest pain is superior to that of RWMA by 2D echocardiography [11, 13, 22–24]. Nevertheless, most of these studies included stable patients with suspicion of CAD who were scheduled for elective CAG, and none demonstrated the diagnostic value of strain echocardiography in an emergency room setting, where physicians frequently encounter patients with chest pain.
We defined significant CAD as ≥70 % stenosis in one or more vessels on CAG or CCTA. Although CAG is the reference standard test to define significant coronary artery stenosis, the high diagnostic accuracy of CCTA has been reported in many studies [25–27]. Among 69 patients who underwent coronary imaging tests in this study, 33 patients underwent CAG and 52 patients did CCTA. All 16 patients who had ≥50 % stenosis on CCTA were performed with CAG and the ≥70 % stenosis in the patients actually confirmed by CAG. The <50 % stenosis on CCTA was considered as insignificant stenosis without further tests since especially high sensitivity and NPV of CCTA have been reported [25, 27].
In terms of global strain, previous studies have reported the diagnostic performance of GLS with optimal cutoff values. Choi et al. [11] demonstrated that decreased GLS with a cutoff value of −17.9 % was associated with multi-vessel disease or left main disease in stable CAD. Two other studies reported that GLS had higher and similar sensitivity/specificity for significant CAD (≥50 % stenosis) compared to pretest likelihood and stress echocardiography, respectively [13, 22]. These two studies proposed GLS cutoff points of −17.77 and −17.4 % as the optimal values with the highest sensitivity/specificity. The optimal GLS cutoff point found in this study, −17.8 %, is very similar to these previously reported values. Unlike global strain, few studies have investigated the role of regional strain for the diagnosis of CAD or have proposed cutoff values of regional strain for the diagnosis of significant CAD. Gjesdal et al. [28] reported that SLS of −13 and −16 % predicted transmural infarction and non-transmural infarction, respectively. More recently Grenne et al. [23] reported that abnormal longitudinal strain in five or more segments identified patients with acute coronary occlusion demonstrating a cutoff value of SLS as −14 %. Another recent study showed that four or more abnormal SLS with a cutoff value of −15 % for significant CAD (≥75 % stenosis) [12]. In the present study, we defined abnormal RLS as at least two adjacent segments with abnormal SLS and determined the diagnostic performance at the five different abnormal SLS cutoff values (Table 4). From the data, the sum of sensitivity and specificity was largest at a SLS cutoff point of −13 % and accuracy was highest at a SLS cutoff point of −12 %. However, caution is needed to use the presented cut-off values as reference values since low inter-vendor agreement in 2-dimensional strain was reported [29]. One the other hand, for the reason why GLS performed worse than RLS for prediction, we consider that GLS is the average of segmental strain and does not well reflect regional dysfunction of LV caused by single coronary arterial occlusion.
Regarding diagnostic performance, visual assessment of RWMA as the sole method to detect CAD by conventional TTE showed a sensitivity of 64 % which was even lower than the sensitivity of pretest probability (72 %) in the present study (Table 5). Even though the accuracy was not statistically different between RWMA and RLS, the sensitivity (92 %) of RLS was much higher than that of RWMA. Improved sensitivity of RLS to detect the significant CAD is very important in terms of usefulness of RLS in acute chest pain patients in ED because the most significant limitation of RWMA on conventional echocardiography was low sensitivity as a primary diagnostic tool. In ischemic cascade, it is well-known that systolic dysfunction is followed by cellular dysfunction and diastolic dysfunction and is caused by relatively longer ischemic insult or repetitive ischemia [30]. With conventional echocardiography RWMA by visual assessment can be detected only when visible systolic dysfunction occurred. In addition RWMA reflects radial thickening rather than longitudinal deformation. Becker el al. [31] demonstrated that radial strain accurately discriminated normokinetic, hypokinetic, or akinetic segments compared to cardiac magnetic resonance imaging. A later studies showed longitudinal strain is more sensitive than radial strain to detect ischemia [32, 33]. Those data might explain why longitudinal strain is more sensitive than RWMA, which was demonstrated in the current study. On the other hand, the sensitivity of RWMA in the present study was much higher than that of the other study. Tsai et al. [12] reported that the sensitivity of RWMA for detecting significant CAD was only 19 %. In this study the echocardiologist who interpreted RWMA from the acquired images could know some clinical information, which included the main reason to perform echocardiography such as acute chest pain and patients’ location such as ED. The clinical information may result in the high sensitivity of RWMA and no difference of accuracy between RLS and RWMA because assessment of RWMA is subjective.
Strain echocardiography can be easily carried out in ED. It does not have the risks associated with the use of a contrast agent or radiation exposure. Furthermore, neither fasting nor additional medication is required for echocardiography. Recently-developed AFI software allows for easy strain analysis [34, 35]. In this study, we used online strain analysis to evaluate acute chest pain in ED. The feasibility of this method was limited in some patients with a poor echocardiographic window, but its use could be acceptable in daily clinical practice when considering the lack of additional risks and the relatively low cost. Furthermore, the high sensitivity (92/92 %) and NPV (93/94 %) for GLS and RLS in this study population were comparable with those of CCTA. A recent review article reported pooled sensitivity and NPV of CCTA as 98 and 96 %, respectively [27]. However, in aspect of specificity, RLS and GLS has still have limitation. Thus, consecutive work-up for patients with abnormal strain value should be individualized according to clinical situation.
There were some limitations to this study. First, only 69 (66 %) patients underwent CAG or CCTA. This prevented us from calculating the diagnostic performance for significant CAD in all patients. However, we could see the sensitivity and specificity for predicting cardiac events in most patients. In addition, although we showed cut-off values for global and regional strain abnormality, the values may not be used as reference values in other conditions. Especially, it is because strain values are affected by the vendor difference. Moreover, we could not analyze correlation between the level of decreased RLS and the anatomical or functional severity of coronary stenosis such as fractional flow reserve in the same territories. As in all other studies of echocardiography, image quality was an important limitation in our study. This could also be a significant limiting factor for the application of TTE with strain to patients in ED in real clinical settings. Finally, our study population is very limited in terms of inclusion criteria and the small number of patients. We only included patients who visited the ED with acute chest pain and excluded patients who were considered as having non-cardiac chest pain on the initial assessment. Therefore, our result should not be applied to patients with chest pain in other settings.
In conclusion, considering the non-invasiveness and easy accessibility, LV strain echocardiography using online analysis may be useful to diagnose CAD and predict future events in acute chest pain patients presenting to ED. In particular, the sensitivity and NPV of RLS were comparable with previously reported values in CCTA. A comprehensive study is warranted to further confirm the usefulness and accuracy of strain echocardiography in diagnosis of ischemic heart disease in acute chest pain patients.
References
Nawar EW, Niska RW, Xu J (2007) National hospital ambulatory medical care survey: 2005 emergency department summary. Adv Data 386:1–32
Lee HA, Park H (2012) Trends in ischemic heart disease mortality in Korea, 1985–2009: an age-period-cohort analysis. J Prev Med Public Health 45(5):323–328
Pope JH, Aufderheide TP, Ruthazer R et al (2000) Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med 342(16):1163–1170
Loten C, Isbister G, Jamcotchian M et al (2009) Adverse outcomes following emergency department discharge of patients with possible acute coronary syndrome. Emerg Med Australas 21(6):455–464
Saadat H, Shiri H, Salarpour Z et al (2011) Exploitation of resources and cardiovascular outcomes in low-risk patients with chest pain hospitalized in coronary care units. Int J Gen Med 4:695–698
Peels CH, Visser CA, Kupper AJ et al (1990) Usefulness of two-dimensional echocardiography for immediate detection of myocardial ischemia in the emergency room. Am J Cardiol 65(11):687–691
Sabia P, Afrookteh A, Touchstone DA et al (1991) Value of regional wall motion abnormality in the emergency room diagnosis of acute myocardial infarction. A prospective study using two-dimensional echocardiography. Circulation 84(3 Suppl):I85–I92
Sasaki H, Charuzi Y, Beeder C et al (1986) Utility of echocardiography for the early assessment of patients with nondiagnostic chest pain. Am Heart J 112(3):494–497
Douglas PS, Garcia MJ, Haines DE et al (2011) ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 appropriate use criteria for echocardiography. a report of the American college of cardiology foundation appropriate use criteria task force, American society of echocardiography, American heart association, American society of nuclear cardiology, heart failure society of America, heart rhythm society, society for cardiovascular angiography and interventions, society of critical care medicine, society of cardiovascular computed tomography, and society for cardiovascular magnetic resonance endorsed by the American college of chest physicians. J Am Coll Cardiol 57(9):1126–1166
Picano E, Lattanzi F, Orlandini A et al (1991) Stress echocardiography and the human factor: the importance of being expert. J Am Coll Cardiol 17(3):666–669
Choi JO, Cho SW, Song YB et al (2009) Longitudinal 2D strain at rest predicts the presence of left main and three vessel coronary artery disease in patients without regional wall motion abnormality. Eur J Echocardiogr 10(5):695–701
Tsai WC, Liu YW, Huang YY et al (2010) Diagnostic value of segmental longitudinal strain by automated function imaging in coronary artery disease without left ventricular dysfunction. J Am Soc Echocardiogr 23(11):1183–1189
Montgomery DE, Puthumana JJ, Fox JM et al (2012) Global longitudinal strain aids the detection of non-obstructive coronary artery disease in the resting echocardiogram. Eur Heart J Cardiovasc Imaging 13(7):579–587
Williams RI, Payne N, Phillips T et al (2005) Strain rate imaging after dynamic stress provides objective evidence of persistent regional myocardial dysfunction in ischaemic myocardium: regional stunning identified? Heart 91(2):152–160
Ishii K, Imai M, Suyama T et al (2009) Exercise-induced post-ischemic left ventricular delayed relaxation or diastolic stunning: is it a reliable marker in detecting coronary artery disease? J Am Coll Cardiol 53(8):698–705
Belghitia H, Brette S, Lafitte S et al (2008) Automated function imaging: a new operator-independent strain method for assessing left ventricular function. Arch Cardiovasc Dis 101(3):163–169
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the cardiac imaging committee of the council on clinical cardiology of the American heart association. Circulation 105(4):539–542
Diamond GA, Forrester JS (1979) Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 300(24):1350–1358
Morise AP, Haddad WJ, Beckner D (1997) Development and validation of a clinical score to estimate the probability of coronary artery disease in men and women presenting with suspected coronary disease. Am J Med 102(4):350–356
Chaitman BR, Bourassa MG, Davis K et al (1981) Angiographic prevalence of high-risk coronary artery disease in patient subsets (CASS). Circulation 64(2):360–367
Detrano R, Yiannikas J, Salcedo EE et al (1984) Bayesian probability analysis: a prospective demonstration of its clinical utility in diagnosing coronary disease. Circulation 69(3):541–547
Nucifora G, Schuijf JD, Delgado V et al (2010) Incremental value of subclinical left ventricular systolic dysfunction for the identification of patients with obstructive coronary artery disease. Am Heart J 159(1):148–157
Grenne B, Eek C, Sjoli B et al (2010) Acute coronary occlusion in non-ST-elevation acute coronary syndrome: outcome and early identification by strain echocardiography. Heart 96(19):1550–1556
Kukulski T, Jamal F, Herbots L et al (2003) Identification of acutely ischemic myocardium using ultrasonic strain measurements. A clinical study in patients undergoing coronary angioplasty. J Am Coll Cardiol 41(5):810–819
Budoff MJ, Dowe D, Jollis JG et al (2008) Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (assessment by coronary computed tomographic angiography of individuals undergoing invasive coronary angiography) trial. J Am Coll Cardiol 52(21):1724–1732
Miller JM, Rochitte CE, Dewey M et al (2008) Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 359(22):2324–2336
Guo SL, Guo YM, Zhai YN et al (2011) Diagnostic accuracy of first generation dual-source computed tomography in the assessment of coronary artery disease: a meta-analysis from 24 studies. Int J Cardiovasc Imaging 27(6):755–771
Gjesdal O, Hopp E, Vartdal T et al (2007) Global longitudinal strain measured by two-dimensional speckle tracking echocardiography is closely related to myocardial infarct size in chronic ischaemic heart disease. Clin Sci (Lond) 113(6):287–296
Takigiku K, Takeuchi M, Izumi C et al (2012) Normal range of left ventricular 2-dimensional strain: Japanese ultrasound speckle tracking of the left ventricle (JUSTICE) study. Circ J 76(11):2623–2632
Braunwald E, Kloner RA (1982) The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation 66(6):1146–1149
Becker M, Bilke E, Kuhl H et al (2006) Analysis of myocardial deformation based on pixel tracking in two dimensional echocardiographic images enables quantitative assessment of regional left ventricular function. Heart 92(8):1102–1108
Reant P, Labrousse L, Lafitte S et al (2008) Experimental validation of circumferential, longitudinal, and radial 2-dimensional strain during dobutamine stress echocardiography in ischemic conditions. J Am Coll Cardiol 51(2):149–157
Feigenbaum H, Mastouri R, Sawada S (2012) A practical approach to using strain echocardiography to evaluate the left ventricle. Circ J 76(7):1550–1555
Amundsen BH, Helle-Valle T, Edvardsen T et al (2006) Noninvasive myocardial strain measurement by speckle tracking echocardiography: validation against sonomicrometry and tagged magnetic resonance imaging. J Am Coll Cardiol 47(4):789–793
Leitman M, Lysyansky P, Sidenko S et al (2004) Two-dimensional strain-a novel software for real-time quantitative echocardiographic assessment of myocardial function. J Am Soc Echocardiogr 17(10):1021–1029
Acknowledgments
We would like to acknowledge the echocardiographers at the Samsung Medical Center; Ji-Hye Gwak, Yu-Rim Han, Bo-Kyoung Kang, Ji-Soo Jeong, and Yun-A Kim.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, M., Chang, SA., Cho, E.J. et al. Role of strain values using automated function imaging on transthoracic echocardiography for the assessment of acute chest pain in emergency department. Int J Cardiovasc Imaging 31, 547–556 (2015). https://doi.org/10.1007/s10554-015-0588-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-015-0588-z