Abstract
Few data exist regarding the effect of image quality on measurements of two-dimensional longitudinal strain (2DLS). In the 2DLS for Diagnosing Chest Pain in the Emergency Room (2DSPER) multicenter study, 2DLS was not useful for ruling out acute coronary syndromes (ACS) in the emergency department (ED). The aim of this substudy was to determine the effect of 2D image quality on the diagnostic accuracy of 2DLS for ACS. We reviewed apical views used for 2DLS analysis in all 605 patients included in the 2DSPER study. Studies with the best image quality (HighQ, n = 177), were compared to the lower quality group (LowQ, n = 428). Abnormal 2DLS was defined as PSS20% > − 17% (PSS20% being the peak left ventricular systolic strain value identifying the 20% worst strain values). Global longitudinal strain (GLS) and PSS20% were significantly worse in LowQ compared to HighQ patients. LowQ independently predicted abnormal 2DLS (OR 1.9, 95% CI 1.3–2.9, P = 0.003). The sensitivity of PSS20% > − 17% for ACS was 85% for LowQ vs. 73% for HighQ (P = 0.2), specificity 22% vs. 38% (P < 0.0001) and overall accuracy 29% vs. 44% (P = 0.0004). Despite better overall accuracy in the HighQ group there was no significant difference between the receiver operating characteristic curves of either GLS or PSS20% in the two groups and abnormal 2DLS did not predict ACS even in HighQ patients (OR 1.7, 95% CI 0.7–4.3, P = 0.3). LowQ echo is associated with worse 2DLS. Abnormal 2DLS was not clinically useful for excluding ACS in the ED even in patients with optimal 2D image quality.
Clinical Trial Registration URL: http://www.clinicaltrials.gov. Unique identifier: NCT01163019.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rapid, but accurate, diagnosis of ischemic chest pain (CP) in the emergency department (ED) is challenging, in view of the fact that in the united states alone 7 million patients present each year to the ED with CP [1]. Two-dimensional longitudinal strain (2DLS) analysis using speckle tracking imaging echocardiography is a useful tool for the assessment of global and segmental left ventricular (LV) function [2,3,4]. Several small single-center studies have reported that 2DLS can accurately detect coronary artery disease (CAD) and identify patients with acute coronary syndromes (ACS), even when imaging is performed up to 48 h after the last CP episode and when standard 2D echo studies do not show wall motion abnormalities (WMA) [5,6,7,8,9,10].
The 2D Strain Echocardiography for Diagnosing Chest Pain in the Emergency Room (2DSPER) study was a multicenter, prospective, blinded study designed to assess the diagnostic value of 2DLS in the assessment of patients presenting to the ED with CP, a non-diagnostic ECG and a normal troponin level on admission [11]. In that study 2DLS was not found to be a useful tool to rule out ACS in the ED, due to a low specificity (26%) and a low overall accuracy (33%). In 2DSPER a new 2DLS parameter was used, the peak systolic strain value identifying the worst 20% LV segments (PSS20%), because this parameter was reported to be superior to global longitudinal strain (GLS) for the diagnosis of ACS [6]. Abnormal 2DLS was predefined as PSS20% > − 17%.
Adequate 2D image quality is essential for accurate 2DLS analysis, but there is little data regarding its impact on the accuracy of 2DLS analysis [12,13,14,15]. Per protocol the 2DSPER multicenter study excluded patients with inadequate image quality. Nevertheless, it is unclear whether selecting only patients with the best image quality would have improved the diagnostic accuracy of 2DLS for ruling out ACS in the ED. Our aim, in the present subanalysis, was to determine the effect of 2D image quality on the diagnostic accuracy of 2DLS for ACS in patients presenting to the ED with CP.
Methods
The 2DSPER was a prospective multicenter blinded study conducted by the Israeli Echo Research Group [11]. Patients over the age of 45 who presented to the ED with CP and suspected ACS were enrolled in 11 Israeli medical centers participating in the study. Patients were excluded from the trial if they had ≥ 1 mm ST elevation or depression, elevated initial troponin, previous myocardial infarction or coronary bypass surgery, other than normal sinus rhythm, complete left bundle brunch block, moderate or severe valvular disease or cardiomyopathy.
Patients were diagnosed as having ACS based on the clinical presentation and evidence of myocardial ischemia on stress ECG, stress echocardiography or scintigraphy and/or with the presence of a culprit lesion (≥ 70 stenosis in a major coronary artery) on coronary computed tomography angiography (CCTA) or invasive coronary angiography. The study was approved by the local institutional review board of each participating center and all patients signed an informed consent form.
Transthoracic echocardiography was performed using commercially available General Electric systems (VIVID Q or S6 or Vivid 7, GE Vingmed Ultrasound AS, Horten, Norway). Apical long axis, 4-chamber and 2-chamber views were digitally recorded at a frame rate of > 40 fps for offline 2DLS analysis. Standard echocardiographic findings, but not 2DLS findings, were available to the attending physician.
An echo study was performed within 24 h of the last chest pain episode. Patients with suboptimal 2D echo image quality, defined as ≥ 2 technically suboptimal segments from apical views, were excluded from the study. All echocardiograms were analyzed in a core lab (Lady Davis Carmel Medical Center) by a single experienced sonographer blinded to all clinical data. Of the 700 patients initially enrolled in the 2DSPER study 48 (6.9%) did not meet the 2D echo image quality criteria and were withdrawn from the study after the initial core lab analysis. The final cohort included 605 patients who had complete clinical and echocardiographic data, including adequate 2DLS analysis. In all 605 patients included, tracking in all LV segments was feasible according to the 2DLS analysis software.
All 605 echocardiograms included in the final 2DSPER study cohort were included in the current substudy, and reviewed by a single experienced sonographer blinded to all clinical and 2DLS data. Studies with the best image quality, defined as optimal visualization of all left ventricular segments throughout the cardiac cycle in all three views, were classified as high quality (HighQ), and the rest as low quality (LowQ).
All echocardiograms were analyzed using a dedicated 2DLS software (EchoPAC SW version 113.0.3; GE Vingmed Ultrasound AS). For each patient global longitudinal strain (GLS) was computed, and an additional histographic analysis of the 2DLS was performed from which the peak systolic strain of the worst 20% segments was computed as previously reported [6, 11]. Briefly, histograms of PSS from traces of 150–200 small segments of the left ventricular myocardium were generated from each of the three apical views, and combined into a single histogram for the entire left ventricle. For each histogram, the 20th-percentile PSS value was calculated (PSS20%), separating the 20% higher (worse) strain values from the rest. Based on previous unpublished data a pre-specified PSS20% value of > − 17% was used to define abnormal 2DLS.
Continuous variables are presented as mean ± SD and categorical variables as numbers and percentages. Characteristics of HighQ and LowQ patients were compared using the Student’s t-test or the Wilcoxon two sample test for continuous variables and χ2 or Fisher’s exact test for categorical data. When multiple comparisons were performed, the Bonferroni correction was applied. Diagnostic accuracy was assessed by receiver operating characteristic (ROC) curves, and sensitivity and specificity were calculated. Areas under the receiver operating characteristics curves (AUC) were compared using the method of DeLong et al. [16]. Multiple logistic regression models were used to calculate odds ratios (OR) and corresponding 95% CI for potential factors affecting PSS20%, and for predictors of ACS. Differences were considered statistically significant at the 2-sided P < 0.05. Statistical analyses were performed using SAS 9.4 software (SAS Institute Inc., Cary NC, USA).
Results
Of the 605 patients included in the final study cohort, 177 patients (29%) had optimal image quality (HighQ group). HighQ patients were younger than LowQ patients, had a lower body mass and body mass index (BMI) and were less likely to have hypertension and to be on beta blocker therapy, but more likely to be males and to have minor ST deviation on ECG (Table 1). In both groups the TIMI risk score was low to moderate. The echocardiographic findings of HighQ and LowQ patients are summarized in Table 2. LowQ patients had a significantly higher heart rate, lower LV ejection fraction, thicker LV septum and worse diastolic function as compared to HighQ patients, but there were no significant differences in visual WMA between the groups.
LowQ patients were more likely to be admitted to the hospital as compared to HighQ patients (Table 3). ACS was diagnosed in 48 (11.2%) of the LowQ group and 26 patients (14.7%) of the HighQ group (P = 0.29). The majority of ACS patients had unstable angina pectoris. Coronary anatomy using either CCTA (n = 52) or coronary angiography (n = 123) was available for 165 patients (27%). A culprit lesion was identified in all 67 patients with ACS and known coronary anatomy, most of which had single vessel disease treated by percutaneous coronary intervention. Coronary anatomy was available in 98/531 (18%) patients without ACS and none of them had significant CAD. There was no significant difference between the LowQ and HighQ groups in all clinical and anatomical parameters presented in Table 3 other than the rate of hospital admission.
Both GLS and PSS20% were significantly worse in LowQ as compared to HighQ patients, but the difference between the two groups was small (Table 2; Fig. 1). PSS20% was significantly worse in patients with ACS as compared to No-ACS only in the HighQ group (LowQ: − 14.4 ± 2.5 vs. − 15.15 ± 2.6%, P = 0.089, HighQ: − 15.3 ± 2.7 vs. − 16.5 ± 2.1%, P = 0.013). LowQ was an independent variable associated with abnormal 2DLS, together with male gender, higher BMI, higher heart rate and abnormal LV early relaxation (Table 4).
Impact of image quality and the presence of ACS on 2DLS. Box plots of GLS (a) and PSS20% (b) showing a significantly worse 2DLS in LowQ patients as compared to HighQ (P = 0.0008 and P < 0.0001, respectively). c PSS20% of ACS and No-ACS in the LowQ group showing no significant difference (P = 0.089). d PSS20% of ACS patients in the HighQ group showing significantly worse values compared to No-ACS (P = 0.013). Boxes represent interquartile range, horizontal lines median, diamonds represent average, whiskers represent minimum (1%) and maximum (99%) and circles represent outliers. Although differences in 2DLS were statistically significant in a, b and d there was a considerable overlap between groups
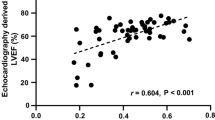
The sensitivity of abnormal 2DLS for the diagnosis of ACS in the HighQ group was 73%, similar to that of the LowQ group (Table 5). The negative predictive value of a normal 2DLS was 89% in HighQ patients, similar to the LowQ patients. The specificity and overall accuracy of abnormal 2DLS for the diagnosis of ACS were significantly higher in the HighQ group, but remained low at 38% and 44%, respectively, with a very low positive predictive value of only 17%, similar to that of the LowQ group. Despite the significantly better overall accuracy of abnormal 2DLS for the diagnosis of ACS in the HighQ group, ROC curves of 2DLS for the diagnosis of ACS were similar in LowQ and HighQ patients, and the AUC for both GLS and PSS20% were low (57.5–63.4%) and not significantly different between LowQ and HighQ patients (Fig. 2). Abnormal 2DLS (PSS20% > − 17%) did not predict ACS in the HighQ group (OR 1.69, 95% CI 0.67–4.28, P = 0.27).
The effect of image quality on GLS and PSS20% receiver operating characteristics curves for the detection of ACS. Both GLS (a) and PSS20% (b) had a low diagnostic accuracy for ACS regardless of image quality (P = 0.45 and P = 0.89 for difference between High Q and LowQ curves, respectively). The green arrow (b) represents the difference between the ROC curves at the predefined cutoff value of PSS20%= − 17%. Numbers in parenthesis reflect area under the ROC curves
Discussion
To date there are over 2000 published papers on 2D strain echocardiography using speckle tracking imaging. Yet large multicenter studies designed to test the clinical utility of 2D strain echocardiography in real world scenarios are lacking. The 2DSPER prospective multicenter study clearly showed that 2DLS has a low accuracy for the detection of ACS in low to medium risk patients presenting with CP to the ED, despite a number of smaller studies which have reported optimistic results [5,6,7,8,9,10]. Caspar et al. recently reported an AUC of 92% for GLS in patients with suspected non-ST elevation ACS, compared to 60% in the 2DSPER total cohort and 62% in the HighQ subgroup [10]. The study of Caspar et al, however, included a selected group of only 58 patients out of 150 consecutive patients with suspected non-ST elevation ACS, and only 25 did not have ACS. Interestingly, most of the Non-ACS patients were women, in whom better strain values are expected, which may account for the better 2DLS values in Caspar’s Non-ACS group [18, 19].
The 2DSPER study, in contrast to the other reported studies, is the only large multicenter study, resembling more closely a “real world” scenario. We have extensively discussed that in the original 2DSPER publication [11]. The main difference between the 2DSPER and the other smaller studies was in the 2DLS values of the Non-ACS patients, which were worse, with less negative values as compared to the other studies, resulting in a low specificity and a low overall accuracy of an abnormal 2DLS for the diagnosis of ACS. The assumption that 2DLS has a “memory effect” in ACS patients, explaining the reduced 2DLS observed long after the ischemic episode, may not be true [6]. The reduced 2DLS in ACS patients may be the result of factors other than ischemia that impair myocardial performance.
One possible explanation for the difference between the results of the current study and those reported by others, could be that in an effort to enroll into 2DSPER all comers under challenging conditions (portable machines used outside the echo lab), patients with suboptimal image quality were enrolled as well. This may have resulted in falsely worse 2DLS values in the Non-ACS group and inability to separate ACS from Non-ACS. However, our data clearly show that inadequate image quality was not the reason for the failure of 2DLS to accurately identify ACS patients, and thus to explain the difference between our findings and those of the other studies. Although the specificity of an abnormal 2DLS in the HighQ group was significantly better than in the LowQ group, it remained low (38%), and therefore the overall accuracy, although significantly better in the HighQ group as well, also remained low (44%). Furthermore, there was no significant difference between the LowQ and HighQ groups in the AUC of both GLS and PSS20% ROC curves which were all low, in contrast to the previous reports [6,7,8,9,10]. A significant difference in accuracy between two groups at a particular cutoff value (PSS20%= − 17% in our case), can coexist with non-significant difference between the two AUC (Fig. 2b).
The differences in average GLS and PSS20% values of the LowQ and HighQ groups, although statistically significant, were small (absolute difference 0.8% for GLS and 1.2% for PSS20%). The LowQ and HighQ groups were similar in most clinical, echocardiographic and angiographic parameters. In particular, they had similar rates of ACS and revascularization. Patients in the LowQ group were slightly older and more likely to be female. LowQ was associated with worse 2DLS values despite the fact that women generally have better 2DLS [19, 20]. They had a higher heart rate and worse diastolic function (significantly lower e′ and higher E/e′). Body weight and BMI were higher in the LowQ group which is not surprising, since image quality is often compromised in patients with high BMI values, resulting in worse 2DLS. This association, however, may not be related to their body habitus or to image quality but to an actual reduction in myocardial function which has been reported in patients with elevated BMI [21]. LowQ echoes were independently associated with abnormal 2DLS, as were male gender, BMI, a higher heart rate and impaired early relaxation. This association between 2DLS and gender, BMI and heart rate has been previously described [18, 19, 21, 22]. The association between impaired diastolic and systolic function is also not surprising since they often coexist [20].
Although adequate image quality is justly considered a prerequisite for an accurate 2DLS analysis, the effect of image quality on 2DLS has not been adequately studied [12]. MacRon et al. studied 70 patients, 28 of whom had inadequate image quality (defined as ≥ 3 segments not analyzable visually), and reported a good reproducibility and correlation between 2DLS and cardiac magnetic resonance (CMR) LV ejection fraction irrespective of image quality [13]. Obokata et al., on the other hand, reported better correlation between CMR and echocardiographic GLS in patients with good image quality [14]. The feasibility of speckle tracking is dependent on image quality, and has been reported to be better with GE systems as compared to other vendors in patients with medium range image quality [23]. Feasibility of speckle tracking, however, does not guarantee the accuracy of the derived 2DLS data. Tracking quality is usually worse in apical and basal segments, and in anterior and posterolateral segments which are more challenging to image [22]. It appears that impaired speckle identification and tracking in patients with LowQ images produce falsely worse deformation values, similar to poorly visualized LV segments that are often incorrectly perceived as hypokinetic to the human eye.
It may not be easy to differentiate an “adequate quality” echo study from an “inadequate quality” echo, and there is no clear cutoff separating the two. An integral automatic quality check built into the speckle tracking algorithm, could prove extremely valuable in ensuring accurate, objective and reliable speckle tracking and in obtaining optimal 2DLS data derived thereof. Such a mechanism, if properly validated, could prove useful in clinical practice to ensure adequate image quality before attempting 2DLS analysis. Based on our data, even such an algorithm, unfortunately, would probably not improve sufficiently the usefulness of 2DLS for the detection of ACS.
The 2DSPER study included only patients with image quality deemed suitable for 2DLS analysis. It is possible that with poorer image quality, the impact of image quality on 2DLS analysis would be greater. High-end machines such as the Vivid E95 were not used in this study. We do not know whether using high-end machines instead of smaller mid-range systems would have significantly improved 2DLS performance in the 2DSPER study, but some of the studies that had reported a high accuracy of 2DLS for detecting ACS used similar systems to those used in the 2DSPER study [6, 10].
In conclusion, we found that image quality was not the main reason for the negative results in the 2DSPER study, since even in the HighQ group abnormal 2D strain could not accurately diagnose ACS. Compared to HighQ images, LowQ images were associated with worse 2DLS and independently predicted an abnormal 2DLS. The diagnostic accuracy of 2DLS, although somewhat better in the HighQ group, remained disappointingly low. This study does not support the use of 2DLS to rule out ACS in patients presenting with CP to the ED, even if they have optimal image quality.
References
Januzzi JL, McCarthy CP (2018) Evaluating chest pain in the emergency department. J Am Coll Cardiol 71:617–619. https://doi.org/10.1016/j.jacc.2017.11.065
Liel-Cohen N, Tsadok Y, Beeri R et al (2010) A new tool for automatic assessment of segmental wall motion based on longitudinal 2D strain a multicenter study by the israeli echocardiography research group. Circ Cardiovasc Imaging 3:47–53. https://doi.org/10.1161/CIRCIMAGING.108.841874
Reisner SA, Lysyansky P, Agmon Y et al (2004) Global longitudinal strain: a novel index of left ventricular systolic function. J Am Soc Echocardiogr 17:630–633. https://doi.org/10.1016/j.echo.2004.02.011
Leitman M, Lysyansky P, Sidenko S et al (2004) Two-dimensional strain-a novel software for real-time quantitative echocardiographic assessment of myocardial function. J Am Soc Echocardiogr 17:1021–1029. https://doi.org/10.1016/j.echo.2004.06.019
Lee M, Chang S-A, Cho EJ et al (2015) Role of strain values using automated function imaging on transthoracic echocardiography for the assessment of acute chest pain in emergency department. Int J Cardiovasc Imaging 31:547–556. https://doi.org/10.1007/s10554-015-0588-z
Shimoni S, Gendelman G, Ayzenberg O et al (2011) Differential effects of coronary artery stenosis on myocardial function: the value of myocardial strain analysis for the detection of coronary artery disease. J Am Soc Echocardiogr 24:748–757. https://doi.org/10.1016/j.echo.2011.03.007
Nucifora G, Schuijf JD, Delgado V et al (2010) Incremental value of subclinical left ventricular systolic dysfunction for the identification of patients with obstructive coronary artery disease. Am Heart J 159:148–157. https://doi.org/10.1016/j.ahj.2009.10.030
Dahlslett T, Karlsen S, Grenne B et al (2014) Early assessment of strain echocardiography can accurately exclude significant coronary artery stenosis in suspected non-ST-segment elevation acute coronary syndrome. J Am Soc Echocardiogr 27:512–519. https://doi.org/10.1016/j.echo.2014.01.019
Choi JO, Cho SW, Song Y, Bin et al (2009) Longitudinal 2D strain at rest predicts the presence of left main and three vessel coronary artery disease in patients without regional wall motion abnormality. Eur J Echocardiogr 10:695–701. https://doi.org/10.1093/ejechocard/jep041
Caspar T, Samet H, Ohana M et al (2017) Longitudinal 2D strain can help diagnose coronary artery disease in patients with suspected non-ST-elevation acute coronary syndrome but apparent normal global and segmental systolic function. Int J Cardiol 236:91–94. https://doi.org/10.1016/j.ijcard.2017.02.068
Shiran A, Blondheim DS, Shimoni S et al (2017) Two-dimensional strain echocardiography for diagnosing chest pain in the emergency room: a multicentre prospective study by the Israeli echo research group. Eur Hear J-Cardiovasc Imaging 18:1016–1024. https://doi.org/10.1093/ehjci/jew168
Voigt JU, Pedrizzetti G, Lysyansky P et al (2015) Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 16:1–11. https://doi.org/10.1093/ehjci/jeu184
MacRon L, Lairez O, Nahum J et al (2011) Impact of acoustic window on accuracy of longitudinal global strain: a comparison study to cardiac magnetic resonance. Eur J Echocardiogr 12:394–399. https://doi.org/10.1093/ejechocard/jer029
Obokata M, Nagata Y, Wu VCC et al (2016) Direct comparison of cardiacmagnetic resonance feature tracking and 2D/3D echocardiography speckle tracking for evaluation of global left ventricular strain. Eur Heart J Cardiovasc Imaging 17:525–532. https://doi.org/10.1093/ehjci/jev227
Trache T, Stobe S, Tarr A et al (2014) The agreement between 3D, standard 2D and triplane 2D speckle tracking: effects of image quality and 3D volume rate. Echo Res Pract 1:71–83. https://doi.org/10.1530/ERP-14-0025
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845. https://doi.org/10.2307/2531595
Antman EM, Cohen M, Bernink PJLM et al (2000) The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA 284:835–842. https://doi.org/10.1001/jama.284.7.835
Dalen H, Thorstensen A, Aase SA et al (2010) Segmental and global longitudinal strain and strain rate based on echocardiography of 1266 healthy individuals: the HUNT study in Norway. Eur J Echocardiogr 11:176–183. https://doi.org/10.1093/ejechocard/jep194
Park JH, Lee JH, Lee SY et al (2016) Normal 2-dimensional strain values of the left ventricle: a substudy of the normal echocardiographic measurements in Korean population study. J Cardiovasc Ultrasound 24:285–293. https://doi.org/10.4250/jcu.2016.24.4.285
Hung CL, Gonçalves A, Shah AM et al (2017) Age- and sex-related influences on left ventricular mechanics in elderly individuals free of prevalent heart failure: the ARIC study (atherosclerosis risk in communities). Circ Cardiovasc Imaging. https://doi.org/10.1161/CIRCIMAGING.116.004510
Vitarelli A, Martino F, Capotosto L et al (2014) Early myocardial deformation changes in hypercholesterolemic and obese children and adolescents: a 2D and 3D speckle tracking echocardiography study. Medicine (Baltimore) 93:1–10. https://doi.org/10.1097/MD.0000000000000071
Marwick TH, Leano RL, Brown J et al (2009) Myocardial strain measurement with 2-dimensional speckle-tracking echocardiography. Definition of normal range. JACC Cardiovasc Imaging 2:80–84. https://doi.org/10.1016/j.jcmg.2007.12.007
Takigiku K, Takeuchi M, Izumi C et al (2012) Normal range of left ventricular 2-dimensional strain: Japanese Ultrasound Speckle Tracking of the Left Ventricle (JUSTICE) study. Circ J 76:2623–2632. https://doi.org/10.1253/circj.cj-12-0264
Funding
Supported by Grants from Clalit Health Services and from the Israel Heart Society.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
All authors report non-financial support from GE Healthcare, Haifa, Israel, during the conduct of the study. Zvi Friedman was a GE Healthcare employee at the time of the study.
Rights and permissions
About this article
Cite this article
Shiran, A., Blondheim, D.S., Shimoni, S. et al. Effect of image quality on accuracy of two-dimensional strain echocardiography for diagnosing ischemic chest pain: a 2DSPER multicenter trial substudy. Int J Cardiovasc Imaging 35, 617–625 (2019). https://doi.org/10.1007/s10554-018-1495-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-018-1495-x