Abstract
Purpose
Growing evidence suggests that certain commonly used diabetes medications have the potential to differentially alter breast cancer risk. We evaluated the influence of metformin, insulin, and sulfonylureas on risk of incident invasive breast cancer.
Methods
We conducted a retrospective cohort study of women ≥40 years of age enrolled in a health plan between 1996 and 2011. Ever, current (≤12 months), and duration (<1, 1–2.9, ≥3 years) of diabetes medication use were obtained from pharmacy databases and modeled as time varying. Multivariable Cox proportional hazards models adjusting for potential confounders including screening mammography and body mass index were used to estimate hazard ratios (HRs) and 95% Confidence Intervals (CIs).
Results
Among 10,050 women with diabetes, 57 % used metformin, 43 % used sulfonylureas, 32 % used insulin, and 301 were diagnosed with breast cancer over median follow-up of 6.7 years. Results suggested no significant decreased risk of breast cancer among metformin users (HR 0.86; 95% CI 0.65–1.12). We found no association between increased breast cancer risk and long-acting insulin (HR 0.95; 95% CI 0.51–1.77), but reduced risk with short-/rapid-acting insulin (HR 0.69; 95% CI 0.50–0.94), and suggestion of a dose–response with increasing duration of short-/rapid-acting insulin use (HR 0.87; 95% CI 0.76–1.00). Estimates for sulfonylurea users suggested increased risk with ever use (HR 1.18; 95% CI 0.90–1.53) and with longer durations of use (≥3 years: HR 1.23; 95% CI 0.88–1.73), but confidence intervals included 1.0.
Conclusions
Our results provide little support for the previously hypothesized decreased risk of breast cancer with metformin use or for an increased risk with insulin use. Implications for possible residual confounding by screening mammography and comorbidity should be considered in breast cancer pharmacoepidemiology studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the increasing prevalence of obesity and an aging population, type 2 diabetes mellitus is rapidly becoming the most common chronic disease in the USA [1]. The association between diabetes and cancer is complex with evidence indicating a 20 % increased risk of breast cancer and poorer breast cancer prognosis and mortality among women with diabetes [2–5]. It has been suggested that diabetes medications, such as metformin, might have possible anticancer effects. However, the evidence remains inconsistent and sparse.
Lower breast cancer risk among women with diabetes treated with metformin is reported in some, [6–14] but not all, [15–22] epidemiological studies. These and recent meta-analyses [23–27] warrant the ongoing evaluation and consideration of metformin as a viable anticancer therapy [28–31]. Risk of breast cancer associated with other diabetic medications is rarely studied, and most results are inconclusive. Insulin glargine is associated with increased cancer risk in numerous studies [32–35], but these findings were not consistently confirmed [36], and for insulin analogs other than insulin glargine no increased risk of breast cancer has been reported. While sulfonylureas were reported to have increased risks of colorectal and pancreatic cancers in one study [15], no association was found for breast cancer. Overall, few studies accounted for potentially important confounders including screening mammography [6, 18], body mass index (BMI) [7, 14, 18], and comorbidity [20] in women who were using these medications and those who were not.
To investigate the association between these diabetes agents and incident invasive breast cancer risk among women with diabetes, we conducted a cohort study within a large integrated health system with computerized information on medication use, comorbidity, breast cancer screening, incident breast cancers, and risk factors for breast cancer.
Materials and methods
Study population
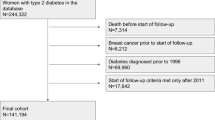
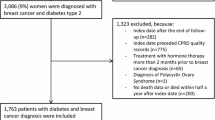
We conducted a retrospective cohort study among women enrolled in Group Health Cooperative (GH), a nonprofit integrated health system that provides comprehensive health care to approximately 600,000 individuals throughout Washington State and parts of Idaho.
Women aged 40 years and older between 1 January 1996 and 31 December 2011 entered the study cohort at the date of diabetes detection or 1 January 1996, whichever was later. Diabetes was defined as any of the following: (1) pharmacy dispensing for a diabetes medication; (2) glycated hemoglobin (HbA1c) ≥7.5 %; (3) 2+ fasting plasma glucose >125 mg/dL in a 12-month period; (4) hospital discharge diagnosis of diabetes (ICD-9 codes 250); or (5) 2+ outpatient diagnoses of diabetes within a 6-month period. Only women enrolled at GH for at least 2 years prior to cohort entry and residing in one of the 13 counties served by the Western Washington Cancer Surveillance System [37], a population-based cancer registry and member of the Surveillance, Epidemiology and End Results (SEER) Program of the National Cancer Institute [38], were included in the study. Women were excluded if they had gestational diabetes, breast cancer, or a mastectomy procedure during the 2 years prior to cohort entry. Women were followed until the earliest of breast cancer diagnosis, prophylactic mastectomy, death, disenrollment from GH (defined as a membership lapse of ≥92 days), or the end of the study follow-up period (31 December 2012). The Institutional Review Board at GH approved this study.
Data collection
Data collection spanned from 2 years prior to cohort entry through the end of follow-up.
We used automated health plan pharmacy data to ascertain information on use of metformin, insulin, sulfonylureas, and other diabetes medications (e.g., thiazolidinediones) dispensed at GH-owned or contracted pharmacies. We also collected information on pharmacy dispensings of statins, oral contraceptives, and hormone replacement therapy (HRT).
We collected potential confounders from GH automated data that contain information on patient demographics, enrollment, inpatient and outpatient diagnoses, and procedures including all breast services, laboratory results, pathology, and vital signs. Breast cancer risk factors were obtained through GH’s Breast Screening Recruitment and Reminder survey [39] that women complete at the time of each mammography screening and upon turning 40 years of age. Information on deaths was obtained through GH’s linkage to the Washington State death tapes [40].
To determine mammography screening, we ascertained examination date and indication designated by the interpreting radiologist from GH administrative databases. We only included screening procedures where the patient reported no symptoms at the time of the examination and the indication was designated as screening [41]. Screening procedures also included all short interval follow-up (SIFU) examinations unless the SIFU took place <9 months after a diagnostic examination. A woman was categorized as adherent if she received at least one screening procedure within rolling 2-year intervals. Less than 1 % of screening procedures were breast MRI examinations; therefore, we refer to screening procedures as screening mammography.
Exposure classification
Exposures of interest included metformin, insulin, and sulfonylureas. We did not evaluate diabetes medications other than these classes due to very low prevalence of use. Following the cohort entry date, women were defined as a user of a medication class of interest if they had 2+ dispensings for any medications in the class of interest during any 6-month period that spanned from 2 years prior to cohort entry through end of follow-up. Dispensing data are continuous, and thus, exposure status was updated daily. Women were allowed to be users of multiple medication classes.
Exposures of interest were further characterized by total duration of use. Duration was estimated by first organizing dispensings into episodes of continuous use. The first episode for a class of interest began with the first dispensing of a medication in that class. For each dispensing, the date when the pills would run out (run-out date) was estimated by multiplying the days’ supply by 1.25 to account for an assumed 80 % compliance [42]. Successive dispensings with ≤60-day gap between the run-out date of one dispensing and date of the subsequent dispensing were considered as continuous use. The end date of a continuous episode was the run-out date of the last dispensing in that episode. Duration was calculated as the amount of time between the start and end dates of the episode. Multiple episodes were summed for total duration of use of each medication class.
Outcomes
Linkage between GH enrollees and the Western Washington SEER tumor registry provided complete ascertainment of breast cancer cases and information on American Joint Committee on Cancer (AJCC) stage [43], histology, and hormone receptor status.
Statistical analysis
We used descriptive statistics to describe patient characteristics by medication exposure and breast cancer status. We used Cox proportional hazards models with time since cohort entry to examine the association between diabetes medication use and risk of incident invasive breast cancer while adjusting for potential confounders. We estimated hazard ratios (HRs) and 95% Confidence Intervals (CIs) for metformin, insulin, and sulfonylureas all of which were modeled as time-varying exposures. In the analyses of ever versus never use of each of these diabetes medications, women were allowed to transition from being nonusers to users as soon as they met the criteria for being a user (i.e., two dispensings in 6 months). All three medication classes were included in the same model. In the analyses of current use (defined as any use in prior 12 months), current use of each medication class was evaluated while adjusting for ever use of the other two classes. We also evaluated the relation between duration of diabetes medication use (categorized as 0, <1, 1–2.9, and 3+ years of use) and invasive breast cancer risk among women who had at least 3 years of follow-up. Women entered the duration analyses at 1 year following cohort entry to allow for a 3-year potential exposure period at cohort entry (which included a 2-year exposure period prior to cohort entry). Duration of each diabetes medication class was evaluated while adjusting for ever use of the other two diabetes medication classes in the same model. Linear trend of duration use was also evaluated. For insulin, we further categorized it into any long-acting (LA) insulin use and any short- or rapid (SA/RA)-acting insulin use.
All models were adjusted for variables considered a priori to be potential confounders, including: age at cohort entry (40–49 vs. 50–59, 60–69, 70–79, 80+ years); study entry year (1996–1999 vs. 2000–2003, 2004–2007, 2008–2011); smoking status at entry (current, past vs. never/unknown); menopausal status at entry (peri- or premenopausal vs. postmenopausal); Charlson comorbidity score [44] (0 vs. 1, 2+, time varying); statin use (ever vs. never use, time varying); HRT (ever vs. never use, time varying); and other diabetes medications (ever vs. never use, time varying). For breast cancer cases, we evaluated tumor characteristics (stage, histology, and hormone receptor status) by medication use and tested differences using Chi-square tests. A statistically significant difference by treatment status was defined as p value ≤0.05.
Because BMI was missing on 46 % of women and at least 2 years of follow-up data were required to determine adherence to screening during the study period (missing on 15 % of women), adjustment for BMI and mammography screening were done in sensitivity analyses. Among women with available information on BMI, we evaluated diabetes medication use and risk of invasive breast cancer in models with further adjustment for BMI (<25.0, 25.0–29.9, 30.0–34.9, 35.0+, time varying). To adjust for screening mammography, defined as having any screening mammography in past 24 months (time varying), we restricted the analyses to women who entered the study cohort beginning 1 January 1999 since mammography data were not fully available until 1997. We also explored the proportion of women who were adherent to screening mammography over the first 8 years of study by medication status.
We evaluated the proportional hazards assumption by testing for interaction between the exposures of interest and the logarithm of follow-up time. No evidence suggested violation of the assumptions. All analyses were performed using SAS statistical software version 9.3 (SAS Institute Inc., Cary, North Carolina).
Results
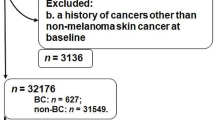
The mean age of the 10,050 women with diabetes was 62 years, and the median duration of follow-up was 6.7 years. During the study period, 57 % were users of metformin, 32 % insulins, 43 % sulfonylureas, and 1.4 % other diabetes agents either alone or in combination (medication use categories not mutually exclusive).
We observed 301 (3 %) incident invasive breast cancers during the follow-up. Descriptive statistics on the cohort overall and by breast cancer status are reported in Table 1. By individual medication class, incident invasive breast cancers were observed among 2.4 % of metformin ever users (n = 135), 2.0 % of insulin ever users (n = 65), and 3.2 % of sulfonylurea ever users (n = 138; Table 1). Compared to women without breast cancer, cases were older and more likely to be postmenopausal, have more comorbidity per Charlson comorbidity index of 1+, non-smokers, and have family history of breast cancer. Cases were also more likely to use HRT, less likely to use statins, and fewer received mammography screening. For diabetes medications, cases were also less likely to be users of metformin and insulin compared to women without breast cancer. Among women that did not have an incident breast cancer diagnosed during follow-up, 13 % died (n = 1,239), 14 % disenrolled from GH (n = 1,398), and 0.2 % had a prophylactic mastectomy (n = 19). Characteristics of women by use of individual diabetes medication classes are reported in Table 2.
Among women 52+ years old at cohort entry, adherence to biennial breast screening by use of different diabetes medication classes is described in Table 3. At 1-year follow-up, adherence to screening mammography was greater among users of metformin (45 %) compared to users of insulin (33 %) and sulfonylureas (34 %). By the third year of follow-up, adherence to biennial screening mammography was greater with use of insulin (64 %) and sulfonylureas (65 %) than with metformin use (53 %). Adherence to screening mammography remained slightly higher in insulin and sulfonylurea users versus metformin throughout the subsequent years of follow-up. Adherence in the non-medication group was in the high 50 s to low 60 s throughout year 1–8 of follow-up.
The majority of breast cancer cases were diagnosed at AJCC stage I (54.8 %) or stage II (30.5 %). Most tumors were estrogen receptor (ER) positive (80 %), progesterone receptor (PR) positive (74 %), and ductal histology (78 %). Fewer tumors of lobular histology were observed among metformin users (6 vs. 16 %) versus nonusers of metformin (Table 4). No differences were observed in breast cancer characteristics by use of insulin or sulfonylureas.
Metformin users had no significantly reduced risk of breast cancer with ever use (HR 0.86; 95% CI 0.65–1.12) and current use (use in the prior 12 months: HR 0.90; 95% CI 0.69–1.16) (Table 5). A reduced breast cancer risk was observed with 1–2.9 years of metformin use (HR 0.39; 95% CI 0.19–0.80) versus nonusers, while no apparent association with <1 year and 3+ years of metformin use, and linear trend of duration use was found.
A reduced breast cancer risk was observed among ever users (HR 0.67; 95% CI 0.50–0.91) and current users (HR 0.64; 95% CI 0.46–0.88) of insulin (Table 5). Analyses of insulin by subtype showed this reduced risk to be specific to SA/RA insulin (HR 0.69; 95% CI 0.50–0.94). A slight reduced risk of incident breast cancer was also observed with greater duration of insulin use (linear trend, HR 0.86; 95% CI 0.76–0.98). Estimates for use of sulfonylureas were suggestive of an increased risk with ever use (HR 1.18; 95% CI 0.90–1.53) and with longer duration of use (3+ years: HR 1.23; 95% CI 0.88–1.73), but CIs included 1.0 (Table 5).
In sensitivity analyses, risk estimates for metformin use remained similar after adjusting for BMI (n = 5,436) and screening mammography (n = 6,393). However, adjustment for screening mammography resulted in moving the risk estimates for insulin (HR 0.94; 95% CI 0.54–1.65) and sulfonylureas (HR 0.96; 95% CI 0.62–1.48) toward the null. In sensitivity analyses by insulin subtype, risk estimates for SA/RA insulin were no longer statistically significant with adjustment for BMI (HR 0.63; 95% CI 0.34–1.15) and attenuated toward the null with adjustment for screening mammography (HR 0.87; 95% CI 0.47–1.59); estimates for LA insulin use increased with adjustment for BMI (HR 1.09; 95% CI 0.32–3.74) and screening (HR 1.87; 95% CI 0.69–5.05) but remained nonsignificant.
Discussion
Results of this study to evaluate commonly used diabetes medications and incident breast cancer risk are in general reassuring. Findings showed no significant association between lower breast cancer risk and use of metformin. SA/RA insulin use was associated with a reduced breast cancer risk, but LA insulin and sulfonylureas were not. In fact, our results suggest that sulfonylurea users may be at a higher risk of breast cancer. However, further adjustment for breast cancer screening in a subgroup of the cohort raises questions about the robustness of our results and other studies that do not adjust for mammography screening.
The existing literature describing the role of diabetes medications in breast cancer etiology is unclear. For metformin, an inhibitory influence on breast cancer is biologically plausible via AMPK pathways, involvement of tumor suppressor gene LKB1, and inhibition of cell proliferation by mTOR-targeted effects [45, 46], but not fully understood. Another recent population-based study from an integrated health system by Soffer et al. [19] also showed little effect of metformin therapy alone on risk of breast cancer and other gynecological cancers. This study did, however, suggest that the combination of metformin with other diabetes medications lowered the risk of breast cancer compared with metformin alone (HR 0.85; 95% CI 0.69–1.04). This would imply that the potential mechanism by which metformin (and other diabetes medications) affect cancer risk may depend on whether glycemic control was achieved and severity of disease. Many other clinical factors could potentially explain observed associations between diabetes medications and breast cancer screening and risk. Physicians may be less inclined to strongly urge screening mammography in sicker patients taking multiple oral diabetes medications and insulin due to other acute health issues that require immediate attention or limited life expectancy of these patients. In contrast, a patient with well-controlled, mild diabetes that is on metformin monotherapy and otherwise healthy may have more opportunity to discuss and receive referrals for screening mammography.
Some preclinical work suggests that metformin influences development of triple-negative breast cancers [47], although few epidemiological studies thus far have reported differences based on hormone receptor or HER2–neu status. In one small study of 90 women with breast cancer and diabetes [48], the frequency of PR-positive tumors in women treated with metformin was significantly higher than in women treated with sulfonylureas only (p = 0.043) or in combination with insulin (p = 0.041). We found little evidence of differences in hormone receptor status in users of metformin, insulin, and sulfonylureas compared to nonusers. Further research is needed in this area to elucidate the effects of diabetes medications on breast cancer subtypes.
Our null findings on risk of breast cancer in relation to LA insulin use are consistent with recent meta-analyses [36] that report possibly decreased risk or no association and run counter to others that previously received considerable attention indicating that LA insulin analogs were associated with significantly increased risk of breast cancer. In a large population-based cohort study in the Netherlands [34], users of LA insulin glargine had an increased risk of breast cancer (HR 1.58; 95% CI 1.22–2.05) compared to users of human insulin. No association was found with non-glargine insulin analogs (HR 0.95; 95% CI 0.83–1.08) in that study [34]. Outside of the hypothesized mitogenic role for insulin analogs in breast cancer [49], studies that observed increased breast cancer risk with LA insulin attributed their findings to confounding by indication. Such a bias could arise if less healthy users or users with more severe diabetes were more likely to develop breast cancer and differentially prescribed LA insulin.
While sulfonylureas were reported to increase risk of colorectal (HR 1.80; 95% CI 1.29–2.53) and pancreatic cancers (HR 4.95; 95% CI 2.74–8.96) in one study [15], no association was found with breast cancer (HR 0.98; 95% CI 0.69–1.41). Similarly, in a nested case–control study in the UK General Practice Research Database [7] neither short- nor long-term use of sulfonylureas were associated with breast cancer risk. Given the unclear mechanism and slight suggestion of increased risk of breast cancer in our study and other solid tumors in other studies, further investigation of sulfonylureas in relation to cancer risk is warranted.
In several studies, women with diabetes are reported to have lower rates of mammography screening [50–52]. In an analysis of women ages 40–79 years from the Women’s Health Initiative clinical trials [6], metformin users had a higher frequency of mammography utilization compared with nonusers. In our study, we observed similar patterns of screening in the first year of follow-up with greater adherence to biennial mammography among metformin users relative to users of insulin and sulfonylureas. By the third year of follow-up, this pattern changed. Adherence to screening mammography was marginally but consistently higher with use of insulin and sulfonylureas than in metformin users. Differences in screening mammography by type of medication use could introduce detection bias to studies of breast cancer risk [53]. The implication of residual confounding in previous studies unable to adjust for breast cancer screening should be considered in light of the change in estimates observed for insulin and sulfonylureas after adjusting for screening.
While our study is the first to provide detailed data on women’s screening mammography practices, there are several limitations to be considered. First, our study subjects are from a single health system in Western Washington State and may not be representative of other populations. Further, information on baseline covariates and eligibility criteria for these enrollees only went back 2 years. While this study included 10,050 women with diabetes (median follow-up: 6.7 years), we observed only 301 incident breast cancer cases and some estimates had wide confidence intervals. It is possible that associations between diabetes medications and breast cancer risk would become clearer with greater follow-up and/or a larger sample size. Second, we did not have any information about intake of the medications. Thus, patients who fill prescriptions but do not subsequently take the medication may be misclassified as users. Similarly, we only ascertained medication dispensings at pharmacies owned or contracted by Group Health. However, health plan pharmacy data are considered a robust measure of medication exposure and previous studies find that enrollees obtain 97 % of their medications at health plan-owned or contracted pharmacies [54, 55]. Third, we were only able to perform sensitivity analyses on a subgroup of women to adjust for important covariates such as BMI and screening mammography since these data were not available for all women in the earlier years. The relation between BMI and the diabetes–breast cancer association is complex with the effects of BMI differing by menopausal status and mammography screening [56]. Residual confounding by these covariates and other unknown/unmeasured risk factors is possible. We lacked information on potential confounders such as diet and level of physical activity, and women prescribed and adherent to metformin and other diabetes medications may differ from nonusers by factors not measured in this study. Also, not all women in the study had data available on HbA1c at cohort entry and throughout follow-up and the possible role of medication adherence and control of diabetes on risk of breast cancer should be evaluated in future studies.
Our study contributes to the growing body of the literature on the role of diabetes medications and breast cancer risk and has several key strengths. This population-based cohort of women enrolled in an integrated health system had longitudinal follow-up and complete ascertainment of incident breast cancers based on linkage to the local SEER registry. We had comprehensive data on medication use based on pharmacy dispensing that allowed us to model breast cancer risk in relation to duration and time-varying use of diabetes medications. We adjusted for many important confounders including BMI and mammography screening. We were also able to report on tumor characteristics and mammography screening adherence by diabetes medication use.
Our study indicates no association between use of long-acting insulin and breast cancer risk, and short-/rapid-acting insulin use may possibly reduce breast cancer risk. We demonstrated little evidence to suggest that metformin use reduces breast cancer risk among women with diabetes. However, the chemopreventive effects of metformin remain to be fully understood and questions regarding a possible role for metformin in adjuvant breast cancer therapy will be better answered from ongoing clinical trials [31].
References
Cowie CC, Rust KF, Ford ES, Eberhardt MS, Byrd-Holt DD, Li C, Williams DE, Gregg EW, Bainbridge KE, Saydah SH, Geiss LS (2009) Full accounting of diabetes and pre-diabetes in the U.S. population in 1988–1994 and 2005–2006. Diabetes Care 32(2):287–294. doi:10.2337/dc08-1296
Wolf I, Sadetzki S, Catane R, Karasik A, Kaufman B (2005) Diabetes mellitus and breast cancer. Lancet Oncol 6(2):103–111. doi:10.1016/S1470-2045(05)01736-5
Larsson SC, Mantzoros CS, Wolk A (2007) Diabetes mellitus and risk of breast cancer: a meta-analysis. Int J Cancer 121(4):856–862. doi:10.1002/ijc.22717
Boyle P, Boniol M, Koechlin A, Robertson C, Valentini F, Coppens K, Fairley LL, Boniol M, Zheng T, Zhang Y, Pasterk M, Smans M, Curado MP, Mullie P, Gandini S, Bota M, Bolli GB, Rosenstock J, Autier P (2012) Diabetes and breast cancer risk: a meta-analysis. Br J Cancer 107(9):1608–1617. doi:10.1038/bjc.2012.414
Peairs KS, Barone BB, Snyder CF, Yeh HC, Stein KB, Derr RL, Brancati FL, Wolff AC (2011) Diabetes mellitus and breast cancer outcomes: a systematic review and meta-analysis. J Clin Oncol 29(1):40–46. doi:10.1200/JCO.2009.27.3011
Chlebowski RT, McTiernan A, Wactawski-Wende J, Manson JE, Aragaki AK, Rohan T, Ipp E, Kaklamani VG, Vitolins M, Wallace R, Gunter M, Phillips LS, Strickler H, Margolis K, Euhus DM (2012) Diabetes, metformin, and breast cancer in postmenopausal women. J Clin Oncol 30(23):2844–2852. doi:10.1200/JCO.2011.39.7505
Bodmer M, Meier C, Krahenbuhl S, Jick SS, Meier CR (2010) Long-term metformin use is associated with decreased risk of breast cancer. Diabetes Care 33(6):1304–1308. doi:10.2337/dc09-1791
Bosco JL, Antonsen S, Sorensen HT, Pedersen L, Lash TL (2011) Metformin and incident breast cancer among diabetic women: a population-based case–control study in Denmark. Cancer Epidemiol Biomarkers Prev 20(1):101–111. doi:10.1158/1055-9965.EPI-10-0817
Tseng CH (2014) Metformin may reduce breast cancer risk in Taiwanese women with type 2 diabetes. Breast Cancer Res Treat 145(3):785–790. doi:10.1007/s10549-014-2985-8
Redaniel MT, Jeffreys M, May MT, Ben-Shlomo Y, Martin RM (2012) Associations of type 2 diabetes and diabetes treatment with breast cancer risk and mortality: a population-based cohort study among British women. Cancer Causes and Control 23(11):1785–1795. doi:10.1007/s10552-012-0057-0
Ferrara A, Lewis JD, Quesenberry CP Jr, Peng T, Strom BL, Van Den Eeden SK, Ehrlich SF, Habel LA (2011) Cohort study of pioglitazone and cancer incidence in patients with diabetes. Diabetes Care 34(4):923–929. doi:10.2337/dc10-1067
Ruiter R, Visser LE, van Herk-Sukel MP, Coebergh JW, Haak HR, Geelhoed-Duijvestijn PH, Straus SM, Herings RM, Stricker BH (2012) Lower risk of cancer in patients on metformin in comparison with those on sulfonylurea derivatives: results from a large population-based follow-up study. Diabetes Care 35(1):119–124. doi:10.2337/dc11-0857
Hsieh MC, Lee TC, Cheng SM, Tu ST, Yen MH, Tseng CH (2012) The influence of type 2 diabetes and glucose-lowering therapies on cancer risk in the Taiwanese. Exp Diabetes Res 2012:413782. doi:10.1155/2012/413782
Libby G, Donnelly LA, Donnan PT, Alessi DR, Morris AD, Evans JM (2009) New users of metformin are at low risk of incident cancer: a cohort study among people with type 2 diabetes. Diabetes Care 32(9):1620–1625. doi:10.2337/dc08-2175
Currie CJ, Poole CD, Gale EA (2009) The influence of glucose-lowering therapies on cancer risk in type 2 diabetes. Diabetologia 52(9):1766–1777. doi:10.1007/s00125-009-1440-6
Qiu H, Rhoads GG, Berlin JA, Marcella SW, Demissie K (2013) Initial metformin or sulphonylurea exposure and cancer occurrence among patients with type 2 diabetes mellitus. Diabetes Obes Metab 15(4):349–357. doi:10.1111/dom.12036
Wang SY, Chuang CS, Muo CH, Tu ST, Lin MC, Sung FC, Kao CH (2013) Metformin and the incidence of cancer in patients with diabetes: a nested case–control study. Diabetes Care 36(9):e155–e156. doi:10.2337/dc13-0708
Tsilidis KK, Capothanassi D, Allen NE, Rizos EC, Lopez DS, van Veldhoven K, Sacerdote C, Ashby D, Vineis P, Tzoulaki I, Ioannidis JP (2014) Metformin does not affect cancer risk: a cohort study in the U.K. Clinical Practice Research Datalink analyzed like an intention-to-treat trial. Diabetes Care 37(9):2522–2532. doi:10.2337/dc14-0584
Soffer D, Shi J, Chung J, Schottinger JE, Wallner LP, Chlebowski RT, Lentz SE, Haque R (2015) Metformin and breast and gynecological cancer risk among women with diabetes. BMJ Open Diabetes Res Care 3(1):e000049. doi:10.1136/bmjdrc-2014-000049
Morden NE, Liu SK, Smith J, Mackenzie TA, Skinner J, Korc M (2011) Further exploration of the relationship between insulin glargine and incident cancer: a retrospective cohort study of older Medicare patients. Diabetes Care 34(9):1965–1971. doi:10.2337/dc11-0699
van Staa TP, Patel D, Gallagher AM, de Bruin ML (2012) Glucose-lowering agents and the patterns of risk for cancer: a study with the General Practice Research Database and secondary care data. Diabetologia 55(3):654–665. doi:10.1007/s00125-011-2390-3
Kowall B, Stang A, Rathmann W, Kostev K (2015) No reduced risk of overall, colorectal, lung, breast, and prostate cancer with metformin therapy in diabetic patients: database analyses from Germany and the UK. Pharmacoepidemiol Drug Saf 24(8):865–874. doi:10.1002/pds.3823
Decensi A, Puntoni M, Goodwin P, Cazzaniga M, Gennari A, Bonanni B, Gandini S (2010) Metformin and cancer risk in diabetic patients: a systematic review and meta-analysis. Cancer Prev Res 3(11):1451–1461. doi:10.1158/1940-6207.CAPR-10-0157
Soranna D, Scotti L, Zambon A, Bosetti C, Grassi G, Catapano A, La Vecchia C, Mancia G, Corrao G (2012) Cancer risk associated with use of metformin and sulfonylurea in type 2 diabetes: a meta-analysis. Oncologist 17(6):813–822. doi:10.1634/theoncologist.2011-0462
Col NF, Ochs L, Springmann V, Aragaki AK, Chlebowski RT (2012) Metformin and breast cancer risk: a meta-analysis and critical literature review. Breast Cancer Res Treat 135(3):639–646. doi:10.1007/s10549-012-2170-x
Zhang P, Li H, Tan X, Chen L, Wang S (2013) Association of metformin use with cancer incidence and mortality: a meta-analysis. Cancer Epidemiol 37(3):207–218. doi:10.1016/j.canep.2012.12.009
Franciosi M, Lucisano G, Lapice E, Strippoli GF, Pellegrini F, Nicolucci A (2013) Metformin therapy and risk of cancer in patients with type 2 diabetes: systematic review. PLoS One 8(8):e71583. doi:10.1371/journal.pone.0071583
Goodwin PJ, Stambolic V, Lemieux J, Chen BE, Parulekar WR, Gelmon KA, Hershman DL, Hobday TJ, Ligibel JA, Mayer IA, Pritchard KI, Whelan TJ, Rastogi P, Shepherd LE (2011) Evaluation of metformin in early breast cancer: a modification of the traditional paradigm for clinical testing of anti-cancer agents. Breast Cancer Res Treat 126(1):215–220. doi:10.1007/s10549-010-1224-1
Hadad S, Iwamoto T, Jordan L, Purdie C, Bray S, Baker L, Jellema G, Deharo S, Hardie DG, Pusztai L, Moulder-Thompson S, Dewar JA, Thompson AM (2011) Evidence for biological effects of metformin in operable breast cancer: a pre-operative, window-of-opportunity, randomized trial. Breast Cancer Res Treat 128(3):783–794. doi:10.1007/s10549-011-1612-1
Jiralerspong S, Palla SL, Giordano SH, Meric-Bernstam F, Liedtke C, Barnett CM, Hsu L, Hung MC, Hortobagyi GN, Gonzalez-Angulo AM (2009) Metformin and pathologic complete responses to neoadjuvant chemotherapy in diabetic patients with breast cancer. J Clin Oncol 27(20):3297–3302. doi:10.1200/JCO.2009.19.6410
Goodwin PJ (2010) ClinicalTrials.gov—a phase III randomized trial of metformin versus placebo on recurrence and survival in early stage breast cancer NCT01101438. Accessed 18 Feb 2014
Hemkens LG, Grouven U, Bender R, Gunster C, Gutschmidt S, Selke GW, Sawicki PT (2009) Risk of malignancies in patients with diabetes treated with human insulin or insulin analogues: a cohort study. Diabetologia 52(9):1732–1744. doi:10.1007/s00125-009-1418-4
Jonasson JM, Ljung R, Talback M, Haglund B, Gudbjornsdottir S, Steineck G (2009) Insulin glargine use and short-term incidence of malignancies-a population-based follow-up study in Sweden. Diabetologia 52(9):1745–1754. doi:10.1007/s00125-009-1444-2
Ruiter R, Visser LE, van Herk-Sukel MP, Coebergh JW, Haak HR, Geelhoed-Duijvestijn PH, Straus SM, Herings RM, Stricker BH (2012) Risk of cancer in patients on insulin glargine and other insulin analogues in comparison with those on human insulin: results from a large population-based follow-up study. Diabetologia 55(1):51–62. doi:10.1007/s00125-011-2312-4
Colhoun HM, Group SE (2009) Use of insulin glargine and cancer incidence in Scotland: a study from the Scottish Diabetes Research Network Epidemiology Group. Diabetologia 52(9):1755–1765. doi:10.1007/s00125-009-1453-1
Bronsveld HK, Ter Braak B, Karlstad O, Vestergaard P, Starup-Linde J, Bazelier MT, De Bruin ML, de Boer A, Siezen CL, van de Water B, van der Laan JW, Schmidt MK (2015) Treatment with insulin (analogues) and breast cancer risk in diabetics; a systematic review and meta-analysis of in vitro, animal and human evidence. Breast cancer Res BCR 17(1):100. doi:10.1186/s13058-015-0611-2
Cancer Surveillance System. http://www.fhcrc.org/en/labs/phs/projects/cancer-surveillance-system.html
Surveillance Epidemiology and End Results (SEER) Program Overview of the SEER Program. http://seer.cancer.gov/about/overview.html
Group Health Breast Cancer Surveillance Registry. http://www.grouphealthresearch.org/surveillanceproject Accessed June 15 2011
Washington State Department of Health, Center for Health Statistics. Death Data. http://www.doh.wa.gov/DataandStatisticalReports/VitalStatisticsData/DeathData. Accessed June 15 2011
Breast Cancer Surveillance Consortium. breastscreening.cancer.gov/data/bcsc_data_definitions.pdf. Updated 16 Sept 2009. Accessed May 18 2015
Boudreau DM, Yu O, Chubak J, Wirtz HS, Bowles EJ, Fujii M, Buist DS (2014) Comparative safety of cardiovascular medication use and breast cancer outcomes among women with early stage breast cancer. Breast Cancer Res Treat 144(2):405–416. doi:10.1007/s10549-014-2870-5
Singletary SE, Allred C, Ashley P, Bassett LW, Berry D, Bland KI, Borgen PI, Clark GM, Edge SB, Hayes DF, Hughes LL, Hutter RV, Morrow M, Page DL, Recht A, Theriault RL, Thor A, Weaver DL, Wieand HS, Greene FL (2003) Staging system for breast cancer: revisions for the 6th edition of the AJCC Cancer Staging Manual. Surg Clin N Am 83(4):803–819. doi:10.1016/S0039-6109(03)00034-3
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45(6):613–619
Alimova IN, Liu B, Fan Z, Edgerton SM, Dillon T, Lind SE, Thor AD (2009) Metformin inhibits breast cancer cell growth, colony formation and induces cell cycle arrest in vitro. Cell Cycle 8(6):909–915
Ben Sahra I, Regazzetti C, Robert G, Laurent K, Le Marchand-Brustel Y, Auberger P, Tanti JF, Giorgetti-Peraldi S, Bost F (2011) Metformin, independent of AMPK, induces mTOR inhibition and cell-cycle arrest through REDD1. Cancer Res 71(13):4366–4372. doi:10.1158/0008-5472.CAN-10-1769
Liu B, Fan Z, Edgerton SM, Deng XS, Alimova IN, Lind SE, Thor AD (2009) Metformin induces unique biological and molecular responses in triple negative breast cancer cells. Cell Cycle 8(13):2031–2040
Berstein LM, Boyarkina MP, Tsyrlina EV, Turkevich EA, Semiglazov VF (2011) More favorable progesterone receptor phenotype of breast cancer in diabetics treated with metformin. Med Oncol 28(4):1260–1263. doi:10.1007/s12032-010-9572-6
Kurtzhals P, Schaffer L, Sorensen A, Kristensen C, Jonassen I, Schmid C, Trub T (2000) Correlations of receptor binding and metabolic and mitogenic potencies of insulin analogs designed for clinical use. Diabetes 49(6):999–1005
Jimenez-Garcia R, Hernandez-Barrera V, Carrasco-Garrido P, Gil A (2009) Prevalence and predictors of breast and cervical cancer screening among Spanish women with diabetes. Diabetes Care 32(8):1470–1472. doi:10.2337/dc09-0479
Beckman TJ, Cuddihy RM, Scheitel SM, Naessens JM, Killian JM, Pankratz VS (2001) Screening mammogram utilization in women with diabetes. Diabetes Care 24(12):2049–2053
Fontana SA, Baumann LC, Helberg C, Love RR (1997) The delivery of preventive services in primary care practices according to chronic disease status. Am J Public Health 87(7):1190–1196
Etzioni R, Xia J, Hubbard R, Weiss NS, Gulati R (2014) A reality check for overdiagnosis estimates associated with breast cancer screening. J Natl Cancer Inst. doi:10.1093/jnci/dju315
Boudreau DM, Doescher MP, Jackson JE, Fishman PA, Saver BG (2004) Impact of healthcare delivery system on where HMO-enrolled seniors purchase medications. Ann Pharmacother 38(7–8):1317–1318. doi:10.1345/aph.1D569
Buist DS, LaCroix AZ, Brenneman SK, Abbott T 3rd (2004) A population-based osteoporosis screening program: who does not participate, and what are the consequences? J Am Geriatr Soc 52(7):1130–1137. doi:10.1111/j.1532-5415.2004.52311.x
Dittus K, Geller B, Weaver DL, Kerlikowske K, Zhu W, Hubbard R, Braithwaite D, O’Meara ES, Miglioretti DL, Breast Cancer Surveillance C (2013) Impact of mammography screening interval on breast cancer diagnosis by menopausal status and BMI. J Gen Intern Med 28(11):1454–1462. doi:10.1007/s11606-013-2507-0
Acknowledgments
This study was supported by the US National Institutes of Health (Grant No. R03CA167589 to D.M.B) at Group Health Research Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Group Health institutional review board.
Conflict of interest
The authors declare that they have no potential conflicts of interest.
Rights and permissions
About this article
Cite this article
Calip, G.S., Yu, O., Elmore, J.G. et al. Comparative safety of diabetes medications and risk of incident invasive breast cancer: a population-based cohort study. Cancer Causes Control 27, 709–720 (2016). https://doi.org/10.1007/s10552-016-0744-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-016-0744-3