Abstract
Purpose
Many studies have investigated the possible association between birth order and risk of childhood cancer, although the evidence to date has been inconsistent. Birth order has been used as a marker for various in utero or childhood exposures and is relatively straightforward to assess.
Methods
Data were obtained on all children born in Denmark between 1973 and 2010, involving almost 2.5 million births and about 5,700 newly diagnosed childhood cancers before the age of 20 years. Data were analyzed using Poisson regression models.
Results
We failed to observe associations between birth order and risk of any childhood cancer subtype, including acute lymphoblastic leukemia; all rate ratios were close to one. Further analyses stratified by birth cohort (those born between 1973 and 1990, and those born between 1991 and 2010) also failed to show any associations. Considering stillbirths and/or controlling for birth weight and parental age in the analyses had no effect on the results. Analyses by years of birth (those born between 1973 and 1990, and those born between 1991 and 2010) did not show any changes in the overall pattern of no association.
Conclusions
In this large cohort of all children born in Denmark over an almost 40-year period, we did not observe an association between birth order and the risk of childhood cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Little is known about the etiology of the heterogeneous group of childhood cancers, but both genetic and environmental factors have been suggested to play a role [1–3]. Many studies have investigated the possible association between birth order and risk of childhood cancer, although the evidence to date has been inconsistent [1, 4–12]. As birth order is relatively straightforward to record, either through routine data sources such as birth registries or through questionnaire-based studies, where it is generally acknowledged to be well reported [13], it has often been used as a surrogate marker for in utero and/or childhood exposures.
Most notably, birth order has been used as a proxy for examining the role of infectious exposures early in life and the subsequent development of acute lymphoblastic leukemia (ALL), a topic about which there has been much debate, particularly with respect to the “delayed infection” hypothesis [14–16]. According to this hypothesis, ALL results from an abnormal reaction to delayed exposure to common infections [17, 18]. It would then be expected that firstborn children would have less contact with infectious agents than children with older siblings and as such have an increased risk of ALL. However, given that data from medical records suggest that children who develop ALL between the ages of 2–5 years have, on average, more infectious illness episodes in the first year of life than those who do not [14, 19–21], it would also be plausible for children with increasing birth order to be at increased risk of ALL.
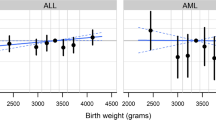
With respect to in utero exposures, birth order acts as a surrogate for hormone levels, as a mother’s first pregnancy differs endocrinologically from later pregnancies [22] with both estrogen and progesterone levels shown to be higher during first pregnancies [23]. Indeed, epidemiological studies suggest a decreased risk of testicular cancer with increasing birth order [24]. There is also a well-established positive relationship between maternal parity and birth weight [25], with high birth weight associated with several different childhood cancer types, including ALL [5, 9, 26, 27]. Furthermore, there is recent evidence to suggest that maternal immune response may also vary with parity [28], and taken together, these two observations may be important for ALL development. One study observed an elevated risk with high birth weight in ALL patients who were firstborn rather than later-born, which may or may not reflect the combination of larger fetal size and later exposure to infectious pathogens incurred more frequently in the firstborn child [29]. While birth weight is regarded as a causal factor for several childhood cancers, parental age shows inconsistent evidence [1], but both factors are related to birth order.
In addition to causal mechanisms, alternative explanations cannot be ruled out. One may speculate that having a child with cancer would impact on family planning, for example by not having further children or by delaying having further children. Hence, sampling in case–control studies might increase the chance for controls to be of higher birth order due to larger average numbers of siblings. Lastly, in the case–control studies requiring active participation, family size may be related to willingness to participate introducing selection bias into a study, as it was observed for other family characteristics [30].
The objective of the present study was to investigate the association between birth order and childhood cancer in a nationwide birth cohort over a long time period. For this, we obtained data on all children born in Denmark between 1973 and 2010, involving almost 2.5 million births and about 5,700 newly diagnosed childhood cancers before the age of 20 years.
Materials and methods
From the Central Population Register (CPR), we obtained information on all children born in Denmark between 1 January 1973 (start of the Danish Medical Birth Registry, see below) and 31 December 2010. Since 1968, all Danish residents receive a unique CPR number, which includes date of birth and sex of the child, and permits accurate record linkage between the different national registries in Denmark [31]. The CPR also includes up-to-date information on vital status, migration, and first-degree relatives. Through the mother of the index child, all siblings, including their date of birth, were identified in the CPR and all stillbirths in the Danish Medical Birth Register, i.e., information used as the basis for counting of birth order and pregnancy order. The Danish Medical Birth Register was established in 1973 [33] and includes information on parental age at child birth as well as the birth weight of the child.
From the nationwide Danish Cancer Registry established in 1943 [32], we identified all children diagnosed with cancer below the age of 20 years within the defined birth cohort. The cancers were grouped according to the International Childhood Cancer Classification (ICCC; ICCC-1 (Birch Marsden Code; [34]) until 2003 and ICCC-3 [35] thereafter). We used the 12 main groups of ICCC, but combined groups XI and XII with group X as “others (X–XII)” because of small numbers and very heterogeneous subtypes. In addition, we subdivided group I into acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), and other leukemias. Furthermore, we specifically looked at non-Hodgkin lymphoma and Hodgkin lymphoma in the lymphoma group, and astrocytoma, ependymoma, and the group of intracranial and intraspinal embryonal tumors (mainly medulloblastoma and therefore called like this) in the group of CNS tumors.
Our key exposure variable, birth order, was defined in two ways. First, we defined birth order counting all live births of the same mother, in line with the hypothesis that the number of older siblings would matter (see above mentioned delayed infection hypothesis). The group of firstborn children was subdivided into those without siblings (only children) and those with further siblings with the same mother, to obtain a surrogate measure of even lesser infectious contacts for only children compared with other firstborns, while acknowledging the distinction was only to arise in the future. Second, we defined birth order including stillborn children of the same mother, in line with the hypotheses that the pregnancy order would matter. In both definitions, multiple births were treated by assigning the same birth order to multiples and then continuing the counting while accounting for the real number of siblings; for example, for a mother having twins and one further child, the twins would both have a birth order of one while the last child was counted as the third child. In Denmark, the definition of stillbirth was changed from ≥28 to ≥22 gestational weeks during our study period, namely in the year 2004. Thus, the birth of a child with no signs of life in gestational weeks 22–27 would have been registered as a spontaneous abortion in the period from 1973 to 2003.
When including birth weight and parental age at the child’s birth as other explanatory variables to adjust for potential confounding, maternal age was dichotomized at age 35 years, paternal age at age 40 years, and birth weight was categorized into three categories of <2.5, 2.5–4, and >4 kg. Alternatively, we have also modeled paternal and maternal age using finer categorizations, specifically by categorizing them into 5-year age groups starting with <25 years and ending with >40 years for mothers and >45 years for fathers, respectively. Further sensitivity analyses looked separately at children born between 1973 and 1990, and born between 1991 and 2010, respectively, as day care patterns and birth rates may have changed over time.
Statistical analyses
We used Poisson regression models to evaluate associations between birth order and childhood cancer, estimating the rate ratios (RRs) and corresponding 95 % confidence intervals (CIs), with and without controlling for maternal age, paternal age, and birth weight. All children were followed up from date of birth until the age of 20 years, date of death, date of emigration out of Denmark, date of first cancer diagnosis, or end of study period (31 October 2013), whichever occurred first. The firstborn children served as the reference group for the comparisons. For comparability with results from previous studies, RRs for linear trend (with increasing birth order) and corresponding 95 % CIs were also calculated using Poisson regression models. The main analysis included all cancers diagnosed up to 20 years of age, but additional analyses were performed restricting to those cases aged 0–14 years at diagnosis for quantitative comparison with previous studies using this age range for their definition of childhood cancer. For the main analyses, birth order excluded stillbirths and RRs were adjusted for maternal age, paternal age, and birth weight. Alternatively logistic regression models and Cox proportional hazards regression models were applied to investigate whether the choice of statistical model would change any of the results.
All analyses were performed using SAS/STAT software [36].
Results
The birth cohort comprised 2,461,283 children, of which 1,262,979 (51.3 %) were boys, born between 1973 and 2010 inclusively. Annual numbers of births varied between 52,716 in 1985 and 73,327 in 1975. Among the total cohort, 1,099,058 children were firstborn (44.7 %), of which 227,913 (9.3 % of total and 20.7 % of firstborn) remained only children, with 906,852 (36.8 %) second-born, 336,017 (13.7 %) third-born, and 119,356 (4.8 %) with a birth order of four or higher. When stillbirths were taken into account, there were only slight changes to the birth order proportions: 1,094,468 (44.5 %) firstborn, 905,362 (36.8 %) second-born, 339,069 (13.8 %) third-born, and 122,384 (5.0 %) with a birth order of four or higher.
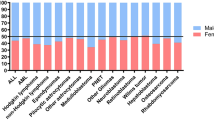
In the study population accruing a total of 38.6 million person-years of follow-up, 5,699 childhood cancers were observed, with leukemias and CNS tumors each representing approximately one quarter of cases. While 96.6 % of children had complete follow-up [because of either reaching age 20 years (51.4 %) or the end of the observation period (31 October 2013)] or had developed cancer (0.2 %), 1.0 % had died of other reasons and 2.2 % were lost to follow-up (emigrated from Denmark). Table 1 shows demographic characteristics of cancer subtypes with respect to age, sex, and birth order. Distributions by age and sex were in accordance with those reported by childhood cancer registries in developed countries, with higher proportions of boys being diagnosed with lymphomas, and cancers such as retinoblastoma, neuroblastoma, and hepatic tumors occurring between the ages 1–4 years, and lymphomas occurring in adolescents (15–19 years). Regarding birth order, 45.6 % of cancer cases were firstborn, similar to the proportion in the overall cohort.
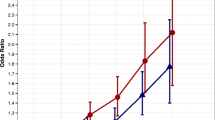
Table 2 shows the associations between birth order and childhood cancers at ages 0–19 years. No significant associations were observed between birth order and any of the cancer subtypes when using all firstborn children as the reference group; for the majority of cancer types, rate ratios (RRs) were all around one. For acute lymphoblastic leukemia (ALL), all RRs were slightly below one. None of the RRs of linear trends were statistically significant, including for ALL.
RRs for Hodgkin lymphoma and non-Hodgkin lymphoma were not different. For Hodgkin lymphoma, for birth order 2, 3, and 4 and higher compared with firstborn, the RRs were 0.90 (CI 0.69–1.17), 1.16 (CI 0.82–1.64), and 1.29 (CI 0.76–2.22). The respective RRs for non-Hodgkin lymphoma were 0.92 (CI 0.67–1.26), 0.68 (CI 0.41–1.12), and 1.17 (CI 0.61–2.26). Among CNS tumors, RRs for ependymoma were 0.83 (CI 0.56–1.22), 0.94 (CI 0.55–1.61), and 0.31 (CI 0.08–1.31), for astrocytoma were 0.94 (CI 0.77–1.15), 0.93 (CI 0.69–1.24), and 0.98 (CI 0.61–1.57), and for medulloblastoma were 1.00 (CI 0.75–1.33), 0.64 (CI 0.39–1.04), and 0.57 (CI 0.24–1.32).
Table 2 also shows the same set of results between birth order and different types of cancers among cases aged 0–14 years. Results were similar to the broader age range. None of the RRs for linear trend were statistically significant.
Sensitivity analyses taking into account stillbirths of the same mother in the counting of pregnancy order had no notable effect as RRs only marginally changed compared with the main analysis (data not shown). Adjustment for parental age and birth weight had little effect, except marginally for all cancers combined and CNS tumors, where non-adjusted RRs were slightly lower than one (but statistically nonsignificant) and varied around one after adjustment (data not shown), and also the way how paternal and maternal age were modeled (dichotomous or using a finer categorization, see Methods) had no impact. Sensitivity analysis by time period (born between 1973 and 1990, and born between 1991 and 2010, respectively) did not show any consistent patterns, with small deviations most likely due to chance (data not shown).
Discussion
In this large study which included almost 2.5 million children born over a 37-year period and 5,699 cases of childhood cancer, we failed to observe associations between birth order and risk of any of the childhood cancer subtypes. Considering stillbirths and/or controlling for birth weight or parental age in the analyses had no effect on the results. Hence, we did not find support for the hypothesis that either the number of older siblings or the pregnancy order would matter.
Our study has a number of strengths over those previously published. Firstly, we adopted a nationwide approach with complete follow-up and virtually no missing data and thus provide a factual reflection of the situation in Denmark. Furthermore, we had the opportunity to incorporate accurate data on stillbirths into our analyses, as well as on some potential confounding factors, in particular birth weight and parental age—although neither variable impacted the overall results. However, one of the limitations was the lack of socioeconomic characteristics, such as parental education or income, given that previous research has shown that individual social position was not related to the risk of childhood leukemia in Denmark, but children born in low-income municipalities had an increased risk [37].
For ALL, results from epidemiological studies are not very consistent. In a five-state register-based study in the USA with 4,699 ALL cases diagnosed between 1980 and 2004, odds ratios were nonsignificantly lower than one, namely 0.97, 0.96, and 0.94, for children born second, third, or fourth or higher, respectively, compared with firstborn children [4]. In a Californian register-based case–control study of 4,721 ALL cases diagnosed between 1988 and 2008 (overlapping with [4]), the observed odds ratio was 0.97 (CI 0.87–1.08) for higher birth order versus first [6]. Similarly, a Californian record-based case–control study with 3,402 ALL cases aged 0–5 years from 1988 to 2007 (overlapping with [4, 6]) showed nonsignificant odds ratios of 1.00, 0.95, and 0.91 for birth orders second, third, and fourth or higher, respectively, compared with firstborn children, but indicated some stronger decrease in non-Hispanic Whites compared with Hispanic Whites [7]. A pooled analysis from the Childhood Leukemia International Consortium (CLIC), using data from 11 questionnaire-based case–control studies from eight countries with a total of 7,399 ALL cases diagnosed between 1979 and 2001, showed a pooled odds ratio of 0.94 (CI 0.88–1.00) for later-born versus firstborn with no monotonic trend of decrease with increasing birth order, but with substantial heterogeneity across studies (I 2 of 71 %) [8]. Individual study odds ratios ranged from 0.69 (CI 0.55–0.86; France) to 1.44 (CI 1.15–1.79; Quebec, Canada). In addition, a previous Danish cohort study involving cases diagnosed between 1968 and 1992 did show a nonsignificant trend of decreasing relative risks in the subgroup of ALL cases aged 0–4 years at diagnosis, but not in older children with ALL, but the majority of those cases are included in our larger case sample [38]. However, a large register-based study combining 1,905 ALL cases from Denmark, Iceland, Norway, and Sweden diagnosed between 1984 and 1999 did show a significant monotonic trend with decrease in risk of 0.90 (CI 0.84–0.96) per one unit increase in birth order, specifically for B-precursor ALL [5]. This is surprising as there is some overlap of the study with the present study in relation to their Danish cases; design features cannot explain the differences with both studies using an identical setup of registries and it cannot be explained further by the restriction to the subtype, as 86 % of ALL were B-precursor ALL in the other study. Reasons are therefore either a stronger effect in the other Scandinavian countries compared with Denmark or that the previous study included cases from an earlier time period; however, the differences between the two studies were also not marked with clearly overlapping confidence intervals. The most recent study from Sweden, however, using 3.57 million children in a national cohort, showed results that were compatible with ours, namely a small but non-statistically significant inverse association with birth order, with an RR for trend by increasing birth order of 0.98 (CI 0.93–1.04) [39].
Taken together and including our results for ALL, there is perhaps a suggestion of an overall, slight 10 % decrease in risk in children of second or higher birth order compared with firstborn children. However, statistical significance depends on the size of study, and there is also some heterogeneity across studies. This could be due to random variation or because the predictive power of birth order, as a surrogate for a particular exposure, may depend on the source population of the study. Overall, these observations do not lend support to the delayed infection hypothesis, but neither do they contradict it.
In Denmark, social contacts through day care are very common, and the proportion of 0- to 6-year-old children attending day care increased from just over 40 % in 1980 to 75 % in 1999 [40]; this is higher than in many other countries, and hence, in Denmark birth order may be a less predictive proxy of social contacts than elsewhere [8]. Given the UK findings of more frequent infections during infancy in children with ALL, it is perhaps surprising that the estimated rate ratio does not point in the other direction [19].
However, while birth order has been used a surrogate for exposure to infections in childhood, it is also an important determinant of other conditions both in the child (e.g., allergy) and the mother (e.g., preeclampsia). With respect to the mother, birth order has also been shown to impact on maternal immune response, including levels of IgE and IFN-γ as well as maternal/fetal HLA mismatch, which given the well-documented in utero origins of ALL may well be important [41, 42]. Indeed, it is possible that it is the changing maternal immune response with birth order, alongside other prenatal events, that impacts on the development of ALL.
A recent review suggests some evidence of an increased risk of childhood AML with increasing birth order, although the authors suggested this could in part be due to a maternal age effect [43]. We did find a slightly increased risk even after adjustment for maternal age, although stronger for those born second or third than fourth or higher. An earlier Danish cohort study with cases diagnosed between 1968 and 1992 found a nonsignificantly increased risk of Hodgkin lymphoma with increasing birth order [relative risk of 1.26 (CI 0.92–1.73)] [44], while in our study the respective relative risk of increase in birth order by 1 was 1.06 (CI 0.92–1.22).
Our lack of observation of an association between any of the solid cancers and birth order contrasts with the large US study described above, where reduced risks restricted to birth order of four and higher compared with firstborn children were observed for CNS tumors (OR 0.77, CI 0.68–0.89), neuroblastomas (OR 0.68, CI 0.55–0.84), and Wilms tumors (OR 0.67, CI 0.54–0.84), leading to an overall decreased odds ratio for their combined 17,672 cancer cases combined of 0.87 (CI 0.81–0.93) [4]. Our respective rate ratio for all cancers combined was 1.00, and no association was seen with any of the three diagnostic subgroups. For later-born children compared with firstborn children, a recent review of neuroblastoma found no clear evidence of an association, although the majority of studies found slightly decreased risks [45]. A large registry-based study in the Nordic countries of 3,983 CNS tumor cases confirmed our finding of no association with birth order, acknowledging some overlap in the Danish cases with our birth cohort [10]. In a similar study in the Nordic countries involving 3,298 cases of Wilms tumor, the odds ratio of later-born children compared with firstborn children was 0.98, again consistent with our findings [11]. Overall, there appears to be little evidence of an association between birth order and childhood solid tumor risk. The findings in the US study for high birth order needs attention regarding which underlying exposure may be reflected in the very high birth order in this setting since that might explain the findings being different to the Nordic countries; the US proportion of those born fourth or higher was twice as high as in Denmark (approximately 10 % [4] compared with 5 %), but we do not know whether this plays any role.
In conclusion, we did not observe an association between birth order and the risk of childhood cancer. Taking the evidence from all published studies together, there may be a weak protective effect for ALL, although this is still not clear and there is little insight into any causal mechanisms. As these results are based on a large nationwide cohort covering a long time span with all Danish children being included, they have some weight in the overall interpretation while results from smaller studies or case–control studies should be interpreted with caution.
Abbreviations
- ALL:
-
Acute lymphoblastic leukemia
- AML:
-
Acute myeloblastic leukemia
- CNS:
-
Central nervous system
- RR:
-
Rate ratio
- CI:
-
95 % Confidence interval
References
Little J (1999) Epidemiology of childhood cancer. IARC Science Publication, Lyon, p 149
Savage S, Schüz J (2011) Environmental chemicals and childhood cancer. In: Nriagu J (ed) Encyclopedia of environmental health. Elsevier, Amsterdam, pp 336–347
Buffler P, Kwan M, Reynolds P, Urayama K (2005) Environmental and genetic risk factors for childhood leukemia: appraising the evidence. Cancer Invest 23(1):60–75
Von Behren J, Spector LG, Mueller BA, Carozza SE, Chow EJ, Fox EE, Horel S, Johnson KJ, McLaughlin C, Puumala SE, Ross JA, Reynolds P (2011) Birth order and risk of childhood cancer: a pooled analysis from five US States. Int J Cancer 128(11):2709–2716
Hjalgrim LL, Rostgaard K, Hjalgrim H, Westergaard T, Thomassen H, Forestier E, Gustafsson G, Kristinsson J, Melbye M, Schmiegelow K (2004) Birth weight and risk for childhood leukemia in Denmark, Sweden, Norway, and Iceland. J Natl Cancer Inst 96(20):1549–1556
Oksuzyan S, Crespi CM, Cockburn M, Mezei G, Kheifets L (2012) Birth weight and other perinatal characteristics and childhood leukemia in California. Cancer Epidemiol 36(6):e359–e365
Marcotte EL, Ritz B, Cockburn M, Yu F, Heck JE (2014) Exposure to infections and risk of leukemia in young children. Cancer Epidemiol Biomarker Prev 23(7):1195–1203
Rudant J, Lightfoot T, Urayama KY, Petridou E, Dockerty JD, Magnani C, Milne L, Spector LG, Ashton L, Dessypris N, Kang AY, Miller M, Rondelli R, Simpson J, Stiakaki E, Orsi L, Roman E, Metayer C, Infante-Rivard C, Clavel J (2015) Childhood acute lymphoblastic leukemia and indicators of early immune stimulation: a childhood leukemia international consortium (CLIC). Am J Epidemiol 181:549–562
Schüz J, Kaatsch P, Kaletsch U, Meinert R, Michaelis J (1999) Association of childhood cancer with factors related to pregnancy and birth. Int J Epidemiol 28(4):631–639
Schmidt LS, Kamper-Jørgensen M, Schmiegelow K, Johansen C, Lähteenmäki P, Träger C, Stokland T, Grell K, Gustafson G, Kogner P, Sehested A, Schüz J (2010) Infectious exposure in the first years of life and risk of central nervous system tumours in children: analysis of birth order, childcare attendance and seasonality of birth. Br J Cancer 102(11):1670–1675
Schüz J, Schmidt LS, Kogner P, Lähteenmäki PM, Pal N, Stokland T, Schmiegelow K (2011) Birth characteristics and Wilms tumors in children in the Nordic countries: a register-based case–control study. Int J Cancer 128(9):2166–2173
Johnson KJ, Carozza SE, Chow EJ, Fox EE, Horel S, McLaughlin CC, Mueller BA, Puumala SE, Reynolds P, Von Behren J, Spector LG (2011) Birth characteristics and childhood carcinomas. Br J Cancer 105(9):1396–1401
Olson JE, Shu XO, Ross JA, Pendergrass T, Robison LL (1997) Medical record validation of maternally reported birth characteristics and pregnancy-related events: a report from the Children’s Cancer Group. Am J Epidemiol 145(1):58–67
Crouch S, Lightfoot T, Simpson J, Smith A, Ansell P, Roman E (2012) Infectious illness in children subsequently diagnosed with acute lymphoblastic leukemia: modeling the trends from birth to diagnosis. Am J Epidemiol 176(5):402–408
Wiemels J (2012) Perspectives on the causes of childhood leukemia. Chem Biol Interact 196(3):59–67
Greaves MF (2001) Commentary: birth order and risk of childhood acute lymphoblastic leukaemia (ALL). Int J Epidemiol 30(6):1438–1439
Greaves M (1999) Molecular genetics, natural history and the demise of childhood leukaemia. Eur J Cancer 35(2):173–185
Greaves M (2006) Infection, immune responses and the aetiology of childhood leukaemia. Nat Rev Cancer 6(3):193–203
Roman E, Simpson J, Ansell P, Lightfoot T, Smith A (2009) Infectious proxies and childhood leukaemia: findings from the United Kingdom Childhood Cancer Study (UKCCS). Blood Cells Mol Dis 42(2):126–128
Roman E, Simpson J, Ansell P, Kinsey S, Mitchell CD, McKinney PA, Birch JM, Greaves M (2007) Eden T; United Kingdom Childhood Cancer Study Investigators. Childhood acute lymphoblastic leukemia and infections in the first year of life: a report from the United Kingdom Childhood Cancer Study. Am J Epidemiol 165(5):496–504
Simpson J, Smith A, Ansell P, Roman E (2007) Childhood leukaemia and infectious exposure: a report from the United Kingdom Childhood Cancer Study (UKCCS). Eur J Cancer 43(16):2396–2403
Bernstein L, Depue RH, Ross RK, Judd HL, Pike MC, Henderson BE (1986) Higher maternal levels of free estradiol in first compared to second pregnancy: early gestational differences. J Natl Cancer Inst 76(6):1035–1039
Maccoby EE, Doering CH, Jacklin CN, Kraemer H (1979) Concentrations of sex hormones in umbilical-cord blood: their relation to sex and birth order of infants. Child Dev 50(3):632–642
Cook MB, Akre O, Forman D, Madigan MP, Richiardi L, McGlynn KA (2009) A systematic review and meta-analysis of perinatal variables in relation to the risk of testicular cancer–experiences of the mother. Int J Epidemiol 38(6):1532–1542
Juntunen KS, Läärä EM, Kauppila AJ (1997) Grand grand multiparity and birth weight. Obstet Gynecol 90:495–499
Harder T, Plagemann A, Harder A (2008) Birth weight and subsequent risk of childhood primary brain tumors: a meta-analysis. Am J Epidemiol 168(4):366–373
Harder T, Plagemann A, Harder A (2010) Birth weight and risk of neuroblastoma: a meta-analysis. Int J Epidemiol 39(3):746–756
Jones M, Jeal H, Harris JM, Smith JD, Rose ML, Taylor AN, Cullinan P (2013) Association of maternal anti-HLA class II antibodies with protection from allergy in offspring. Allergy 68(9):1143–1149
Schüz J, Forman MR (2007) Birthweight by gestational age and childhood cancer. Cancer Causes Control 18(6):655–663
Schüz J (2003) Non-response bias as a likely cause of the association between young maternal age at the time of delivery and the risk of cancer in the offspring. Paediatr Perinat Epidemiol 17(1):106–112
Thygesen LC, Daasnes C, Thaulow I, Bronnum-Hansen H (2011) Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health 39(7 Suppl):12–16
Gjerstorff ML (2011) The Danish Cancer Registry. Scand J Public Health 39(7 Suppl):42–45
Nguyen-Nielsen M, Svensson E, Vogel I, Ehrenstein V, Sunde L (2013) Existing data sources for clinical epidemiology: Danish registries for studies of medical genetic diseases. Clin Epidemiol. 5:249–262
Birch JM, Marsden HB (1987) A classification scheme for childhood cancer. Int J Cancer 40(5):620–624
Steliarova-Foucher E, Stiller C, Lacour B, Kaatsch P (2005) International classification of childhood cancer, third edition. Cancer 103(7):1457–1467
SAS/STAT software, Version 9.3 of the SAS System for Windows. Copyright © 2002–2010 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA
Raaschou-Nielsen O, Obel J, Dalton S, Tjønneland A, Hansen J (2004) Socioeconomic status and risk of childhood leukaemia in Denmark. Scand J Public Health. 32(4):279–286
Westergaard T, Andersen PK, Pedersen JB, Olsen JH, Frisch M, Sørensen HT, Wohlfahrt J, Melbye M (1997) Birth characteristics, sibling patterns, and acute leukemia risk in childhood: a population-based cohort study. J Natl Cancer Inst 89:939–947
Crump C, Sundquist J, Sieh W, Winkleby MA, Sundquist K (2015) Perinatal and familial risk factors for acute lymphoblastic leukemia in a Swedish national cohort. Cancer 121:1040–1047
Petersen AN (editor). Børns levevilkår [Childrens living conditions]. Statistics Denmark 2002; Statistics Denmark Printing, Copenhagen; ISBN 87-501-1286-4
Jones M, Jeal H, Harris JM, Smith JD, Rose ML, Taylor AN, Cullinan P (2013) Association of maternal anti-HLA class II antibodies with protection from allergy in offspring. Allergy 68:1143–1149
Karmaus W, Arshad SH, Sadeghnejad A, Twiselton R (2004) Does maternal immunoglobulin E decrease with increasing order of live offspring? Investigation into maternal immune tolerance. Clin Exp Allergy 34:853–859
Puumala SE, Ross JA, Aplenc R, Spector LG (2013) Epidemiology of childhood acute myeloid leukemia. Pediatr Blood Cancer 60(5):728–733
Westergaard T, Melbye M, Pedersen JB, Frisch M, Olsen JH, Andersen PK (1997) Birth order, sibship size and risk of Hodgkin’s disease in children and young adults: a population-based study of 31 million person-years. Int J Cancer 72:977–981
Heck JE, Ritz B, Hung RJ, Hashibe M, Boffetta P (2009) The epidemiology of neuroblastoma: a review. Paediatr Perinat Epidemiol 23(2):125–143
Acknowledgments
No specific funding was obtained for this study. Costs for data retrieval were covered by the collaboration agreement between the IARC and the Danish Cancer Society Research Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors declared any conflict of interest.
Human and animal rights
The study did not involve personal contact with human subjects and no animals. The study is based on record linkage of various registers in Denmark and was therefore approved by “Datatilsynet” (the Danish Data Protection Board). No informed consent from individuals was required.
Rights and permissions
About this article
Cite this article
Schüz, J., Luta, G., Erdmann, F. et al. Birth order and risk of childhood cancer in the Danish birth cohort of 1973–2010. Cancer Causes Control 26, 1575–1582 (2015). https://doi.org/10.1007/s10552-015-0651-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-015-0651-z