Abstract
Purpose
Side effects as a result of breast cancer treatment may have a lasting detrimental impact on quality of life. Exercise has been shown to be an effective intervention in post-treatment care. This study aimed to gain a better understanding of breast cancer treatment-related side effects through identifying potential patient characteristic associations, including current levels of exercise.
Methods
Four hundred and thirty-two breast cancer patients completed an online survey covering their treatment and demographic background, current exercise levels, and self-reported treatment side effects. Side effects were considered in a binary logistic regression against age, surgery, currently undergoing treatment, and exercise levels to ascertain significant relationships (p < 0.05) and associative values (Odds Ratio).
Results
Lumpectomy patients were less likely to report aching muscles (OR 0.61, 95 % CI 0.39–0.96), hot flushes (OR 0.60, 95 % CI 0.38–0.96), and weight gain (OR 0.59, 95 % CI 0.38–0.92) than mastectomy patients. Women currently undergoing treatment were more likely to report hot flushes (OR 3.77, 95 % CI 2.34–6.08), aching muscles (OR 1.62, 95 % CI 1.02–2.57), and weight gain (OR 1.89, 95 % CI 1.19–2.99) than women finished treatment. Sedentary women were more likely to experience shoulder limitations (OR 1.77, 95 % CI 1.14–2.77), muscular chest wall pain (OR 1.69, 95 % CI 1.07–2.65), weight gain (OR 2.29, 95 % CI 1.44–3.64), lymphedema (OR 1.68, 95 % CI 1.04–2.71), and breathlessness (OR 2.30 95 % CI 1.35–3.92) than their physically active counterparts.
Conclusions
Patient characteristics may inform interventions to improve care post-breast cancer treatment. Sufficient levels of exercise were consistently associated fewer side effects and should be encouraged.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary treatment following a breast cancer diagnosis is surgery. Post-surgery, many women will also undergo radiotherapy, together with systemic adjuvant therapies, including chemotherapy, hormonal or endocrine therapy, or a combination of these. Although increasingly effective in terms of disease control, negative side effects of these breast cancer treatments are common [1]. These side effects are often treatment specific and manifest in a range of symptoms. Local complications such as pain or numbness in the breast or chest wall, restricted arm motion, arm lymphedema, and skin sensitivity are worse with more extensive surgery, more extensive radiation, or both [2, 3]. Compounding these local complications are common side effects of systemic adjuvant therapy including vasomotor symptoms such as hot flushes; neuropsychiatric symptoms such as a lack of energy or fatigue; gastrointestinal symptoms such as weight gain and nausea; and gynecological symptoms such as breast sensitivity or tenderness [4]. In some cases, these side effects can become a major cause of morbidity and treatment discontinuation and may have prolonged negative effects on a breast cancer survivor’s quality of life (QOL) [1, 4].
Breast cancer treatment side effects have been shown to impact upon QOL dimensions, suggesting that reducing these side effects will have a positive effect on QOL [1]. Greater side effects during breast cancer treatment have also predicted greater post-treatment distress [5]. For example, fatigue as a treatment effect has emerged as a strong predictor of QOL within 1 year of treatment and may continue to compromise QOL as long as 5 years post-diagnosis [6, 7]. Impairments in upper-body functioning as a result of breast cancer treatment have also been significantly related to reductions in QOL [8, 9], and experiencing persistent arm lymphedema is related to worse general mental health and physical function [1]. It has been suggested that all currently available endocrine therapies have side effect profiles that can affect patient-related QOL outcomes [10].
Compounding the detrimental impact side effects have on QOL, unpleasant side effects as a result of taking medication are also significantly predictive of adherence to medication plans [4, 11]. Breast cancer treatment side effects as a reason for non-adherence provide a compelling argument to better understand the mechanisms of these adverse events, as restricting or cessation of treatment could severely diminish opportunities for health gains. It is expected that better management of treatment-related side effects may trigger a “cascade effect,” through improving QOL outcomes, in turn improving medication adherence, and ultimately resulting in better patient outcomes [4].
Exercise is one of the most effective interventions that can assist in the management of breast cancer treatment side effects through enhanced improvements in cardio-respiratory fitness, immune function during recovery, self-esteem, and other psychological health parameters [12–14]. Breast cancer patients who exercise have reported decreased levels of anxiety and depression, and research reviews have also suggested that physical activity during treatment and recovery may enhance breast cancer survival [15, 16]. Despite the well-established benefits of exercise, the effect of exercise on a broader range of breast cancer treatment side effects is generally unknown. Review authors have therefore called for more attention to be focused on how exercise affects the multitude of frequently experienced, persistent side effects of breast cancer treatment [13, 14].
Given the potential negative impact on QOL and prognosis, a better understanding of the prevalence of patient-determined side effects is warranted, and the association of patient characteristics with these side effects should be explored. Some studies have suggested that the experience of breast cancer treatment side effects may vary as a function of age, stage of disease, and body mass index [17], whereas other studies have suggested that socio-demographic characteristics generally do not help identify women who will have greater or lesser symptom experience [1, 6, 18]. Patient characteristics may provide a useful initial step toward developing intervention strategies to improve care for women living with a breast cancer diagnosis.
Intervention strategies involving exercise have been identified as being effective, and further investigation into the influence of exercise on a wider range of breast cancer treatment side effects is required. Therefore, the purpose of this study was to gain a better understanding of breast cancer treatment side effects through identifying potential patient characteristic associations with age, type of surgery, currently undergoing treatment, and levels of exercise. We hypothesized that (i) patient characteristics would hold moderate associative values for side effect experience and (ii) lower exercise levels would be associated with a greater side effect experience.
Participants and methods
Participants and survey implementation
Breast cancer patients who had a registered email address with the Breast Cancer Network Australia (BCNA) Review and Survey group or the Cancer Councils of Victoria or Western Australia were invited by email to complete an online survey. Inclusion criteria were any women, over 18 years of age, with a breast cancer diagnosis prior to the survey distribution date. The survey invitation contained a brief introduction to the investigators and the study, as well as a direct link to the uniform resource location (URL) containing the internet-based survey. The URL was open to responses for 4 months and closed when continued promotion of the survey did not illicit any further responses. Due to the anonymity of the data collection procedures, and the “sharing” nature of the internet, the survey’s response rate could not be tracked. However, of the 482 women who visited the initial URL, 432 completed the survey (89.6 % completion rate). Participant’s informed consent was obtained whereby the first page of the survey was a participant information sheet to which participants clicked “I agree” in order to progress with the online survey. The University Human Research Ethics Committee approved all data collection procedures (HREC08/326).
Online survey instrument
The online survey instrument was based on a previously validated paper-based questionnaire [19]. To validate the online version, seven focus groups with breast cancer patients were conducted (total participants = 20) at community centers around the greater Sydney area. During these groups, the think-aloud technique was employed [20] and participants were queried about their understanding and about the relevance and sensitivity of each question which lead to changes to facilitate the participants’ understanding and ease in navigating the electronic version.
The final survey instrument included 68 closed-ended and 11 open-ended items covering background variables such as health status, location, disease timelines, treatment methods, surgery types, treatment complications, and each respondent’s current exercise habits. Duplicate surveys were prevented by firstly checking internet protocol (IP) addresses embedded in the responses, and secondly reviewing the respondent’s date of birth. No identical IP addresses were submitted, and checking responses from women with the same date of birth also indicated no duplicates.
Independent analytical variables
Age
Participant’s age was an open-ended response to “What is your date of birth?,” calculated with respect to the survey submission date (providing age at time of survey completion). Following this calculation, participants were split into categories of being “Under 50 years old” or “50 years and over” for the purpose of the binary logistic regression (see Table 1).
Surgery type
Participant surgery type was assessed by a closed-ended question for which the responses were either a lumpectomy or a mastectomy of either the right or left breast. Responses were presented in a 2 × 2 button grid (lumpectomy and mastectomy by left and right breast) and were not mutually exclusive, permitting participants to indicate if they had undergone surgery on both breasts or had a lumpectomy, followed by a mastectomy. Women were instructed to skip the question if they had not undergone surgery. Only three participants did not respond with a surgery type. Participants were then grouped into categories of a “Lumpectomy” or a “Mastectomy” for the binary logistic regression (see Table 1).
Current treatment
Participants were asked “Are you CURRENTLY undergoing any of the following treatments for your breast cancer?” with closed-ended response categories of chemotherapy, radiotherapy, and hormonal treatment. Examples of hormonal treatments were provided, and responses were not mutually exclusive. Women were also asked the date of their last treatment ever if they had finished these categories of treatment. The difference between the survey completion date and the treatment completion date was calculated to give a time since treatment completion, which is summarized in Table 1. For the purpose of the binary logistic regression, participants were divided into categories of “current treatment” versus “finished treatment.”
Exercise
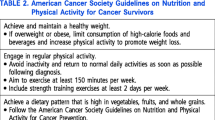
The Recreational Activities domain of the Global Physical Activity Questionnaire Version 2 (GPAQ2) [21] was used to assess recreational exercise intensity and duration. The GPAQ2 calculates metabolic equivalents (METs) to express the intensity of reported physical activities [21]. The total time spent in physical activity during a typical week, the numbers of days, as well as the intensity of the physical activity are taken into account to calculate three categorical indicators (low, moderate, and high). The criteria for these levels are shown in Table 2, along with the number of women who met each criterion and the percentage these women formed of the total sample. For the purpose of the binary logistic regression, all women meeting either the moderate or high levels of exercise (n = 158) were classified as “sufficiently active.”
Dependent analytical variables
Breast cancer treatment side effects
Side effects were reported as those experienced in the 2 weeks prior to completing the survey and were evaluated by a closed-ended list of possible complications (see Table 3). Participants were asked to respond regarding their experience of that side effect on a 5-point Likert scale (from none to severe; see Table 3). For the purpose of binary logistic regressions, women were divided into categories of “no symptom experience” (Likert response = 1) versus “any level of experience” (Likert response = 2–5).
Statistical analysis
Descriptive analysis
Answers to the closed-ended side effects items were coded and counted to determine the frequency response for each item. The number of responses to different questions may vary as respondents were given the option to skip questions to minimize participant burden. Study population proportions were then calculated as a percentage of the number of women who answered that question. To provide an accurate representation of the data, non-responses were not assumed to represent not experiencing a particular side effect, but rather data were analyzed based only on the women who provided a response to that question. The mean of responses for each side effect question was also calculated to show where most participants responded on the continuum of not experiencing that particular side effect to experiencing it severely. The closer the mean score was to “5,” the more severely participants experienced that side effect.
Relationship analysis (binary logistic regression model)
Each side effect was considered in a binary logistic regression to ascertain any associated variables and significant relationships. Whether a participant reported experiencing a side effect (none vs. any level of experience) was inserted as a dependent variable against the independent variables of age (<50 vs. ≥50 years), type of surgery (lumpectomy vs. mastectomy), currently undergoing treatment (current vs. finished treatment), and exercise levels (not sufficiently active vs. sufficiently active). This method of analysis has been successfully used in a previous cross-sectional survey data with a breast cancer population [22] and ensures each independent variable is analyzed while controlling for the other three independent variables. All statistical analyses were completed using SPSS for Windows software (Version 17.0, SPSS Inc, Chicago, USA).
Results
Participant characteristics
Participants were 432 female breast cancer patients and survivors aged 23–77 years (mean 53.3 ± 9.8 years). Table 1 provides information on the participant’s characteristics with comparisons to Australia population data. In brief, the self-reported health status of the survey sample was comparable to that of the general Australian female population, and the survey sample was spread across Australian States and Territories in similar proportions to the wider breast cancer population, with the exception of the Australian Capital Territory, which formed 10 % of the sample and only 2 % of the national spread. The age spread of the sample was generally lower than the age of the wider Australian breast cancer population, which may skew results toward a younger breast cancer population. The proportion of women deemed sufficiently active in the survey sample was very comparable to an age-matched general Australian female population (37.4 vs. 37.6 %). Table 1 also provides a summary of the binary logistic regression groups used for statistical analysis as related to the sample’s age, surgery, whether they were currently undergoing treatment, and recreational exercise levels.
Side effects: descriptive and relationship results
Table 3 provides a summary of the side effects examined, the number of participants who responded to the question (out of a potential 432 participants), the mean of the Likert scores in response to each side effect, and the percentage of the sample who experienced each side effect. Hot flushes, sleep disorders, aching muscles, and fatigue were the most commonly experienced side effects with approximately two-thirds of respondents reporting each (66.3, 65.3, 64.3, and 62.7 %, respectively). Table 4 indicates the significance of each side effect against age, surgery, current treatment, and exercise participation, as determined by a binary logistic regression with odds ratios (OR) and 95 % confidence intervals (95 % CI). Approximately half of the side effects (7 of 15) were associated with at least once of the independent variables. Weight gain was significantly related to all the independent variables except age.
Side effects and surgery
Compared to women who had undergone a mastectomy, women who had undergone a lumpectomy were less likely to report fatigue (OR = 0.60; 95 % CI 0.38–0.96; p = 0.05), aching muscles (OR = 0.61; 95 % CI 0.39–0.96; p = 0.023), and weight gain (OR = 0.59; 95 % CI 0.38–0.92; p = 0.02) while controlling for age, current treatment, and exercise levels.
Side effects and current treatment
Compared to women who were finished all treatment, women who were still taking medication for their breast cancer were more likely to report experiencing weight gain (OR = 1.89; 95 % CI 1.19–2.99; p = 0.007), hot flushes (OR = 3.77; 95 % CI (2.34–6.08); p < 0.001), and aching muscles (OR = 1.62; 95 % CI 1.02–2.57; p = 0.031) while controlling for age, surgery type, and exercise level.
Side effects and exercise
Compared to women who were sufficiently active, sedentary women were more likely to report experiencing weight gain (OR = 2.29; 95 % CI 1.44–3.64; p < 0.001), shoulder limitations OR = 1.77; 95 % CI (1.14–2.77; p = 0.012), breathlessness (OR = 2.30; 95 % CI 1.35–3.92; p = 0.002), muscular chest wall pain (OR = 1.69; 95 % CI 1.07–2.65; p = 0.023), and arm lymphedema (OR = 1.68; 95 % CI 1.04–2.71; p = 0.034) while controlling for age, current treatment, and surgery type.
Discussion
The present study sought to gain a better understanding of the side effect experience of women following breast cancer treatment. It did so through a binary logistic regression analysis of selected patient characteristics against self-reported side effects. Of 15 listed side effects, 7 were significantly associated with at least one patient characteristic, confirming our first hypothesis that these characteristics have a moderate association with side effect experience.
Age
Age did not emerge as being strongly associated with the side effects experienced by breast cancer survivors and was not linked to any of the examined side effects. The study cohort is younger than the wider breast cancer population, which may have limited our ability to elicit an association with this variable.
Surgery
Women who had undergone a mastectomy were more likely to experience aching muscles, weight gain, and hot flushes than women who had undergone a lumpectomy. Findings from previous research regarding relationships between surgery type and symptom experience have been mixed. For example, whereas Janz et al. [1] found no clinically meaningful differences in symptom experience between women who received a mastectomy and those who received breast conserving surgery, Rabin et al. [26] found women who underwent a mastectomy indicated lower QOL scores in the physical and psychological domains than their breast conserving surgery counterparts.
The finding of an association between aching muscles and having a mastectomy is not unexpected. Pain and numbness in the breast, chest wall, or axilla are common complications of breast cancer surgery, affecting 15–75 % of survivors, and are often related to the extent of surgery performed [2].
Unexpectedly, weight gain also emerged as being significantly related to undergoing a mastectomy. As a side effect, weight gain is of particular importance as it can predispose breast cancer survivors to other morbidities, such as cardiovascular diseases and orthopedic problems [27]. Weight gain can also negatively impact upon self-esteem and other psychological aspects of QOL [28]. Furthermore, weight gain and obesity have been significantly linked to higher relapses and poorer survival [13], arm swelling and symptoms of persistent lymphedema [2, 17]. Previous research has indicated that weight gain is more common in women receiving adjuvant chemotherapy, particularly for extended treatment durations, and appears to be more pronounced in premenopausal women [27]. No research could be located which explored the link between specific surgery types and weight gain, making this the first study to suggest this association.
Finding an association between hot flushes and surgery was also unexpected, particularly as in the absence of ovarian ablation, the primary treatment responsible for hot flushes is adjuvant endocrine therapy, not surgery. Although the binary logistic regression model used in this analysis controlled for age and whether women were currently undergoing adjuvant endocrine therapy, it was not possible to control for the extent of adjuvant endocrine therapy, or menopausal status, which may have influenced this outcome. Nevertheless, it is possible that although surgery per se is not responsible for experiencing hot flushes, the experience of other adverse events linked to surgery may play a significant role. Particularly, correlations between weight gain and experiencing hot flushes exist [29], and given the significant association between weight gain and surgery in the present study, it is possible that these events are inter-related in their link to experiencing hot flushes. Therefore, rehabilitation efforts for women post-surgery should also be aware of the associations between weight gain and hot flushes, and the risk a greater extent of surgery poses toward experiencing these side effects.
Current treatment
Women who were currently taking medication for their breast cancer were more likely to experience hot flushes, weight gain, and aching muscles than women who had completed all breast cancer treatment. However, the finding that 12 of the 15 listed side effects were not significantly associated with treatment completion is also clinically relevant, as it suggests that side effects as a result of treatment can present a lasting burden for some women, due to these side effects being experienced equally by women undergoing treatment, and those who are not (average 4.3 years post-treatment completion).
The present study found that women were more likely to experience hot flushes while currently undergoing breast cancer treatment, which supports previous research suggesting a strong link between hot flushes and primary breast cancer treatment [30]. These treatment-induced hot flushes have been linked to abrupt and premature menopause (among premenopausal women) as a result of chemotherapy and ovarian ablation, and commonly used adjuvant therapies in breast cancer, such as tamoxifen and aromatase inhibitors [30]. Estrogen withdrawal as a result of these treatments is thought to be an initiator of hot flushes, as changes in estrogen levels may affect functioning of the thermoregulatory centers in the hypothalamus [30]. Up to 65 % of women report hot flushes during or following breast cancer treatment and 64–82 % of these patients rate these episodes as moderate to severe [31]. In the present study, hot flushes were the most commonly reported side effect, experienced by 66.3 % of participants.
Current breast cancer treatment was also significantly associated with weight gain. These results are similar to a study in which 1 year after treatment began, 62.5 % of study participants experienced a significant weight gain of five pounds (2.27 kg) or more [28]. After 2 years, 68 % of those women who gained weight in the initial year maintained a clinically significant weight gain. This percentage was reduced to 40 % after 3 years, suggesting, as with the present study, that the greatest effect of weight gain was experienced in the initial stages of breast cancer treatment. Furthermore, the vast majority of women undergoing treatment in the present study were undertaking hormonal therapies (n = 226, which was 95 % of the women currently undergoing treatment). Decreased serum estradiol levels are a significant factor in weight gain and are commonly linked to hormonal therapies, although evidence is mixed [32, 33]. It is likely that menopausal status contributes to inconsistent evidence regarding weight gain and hormonal therapies because common treatments such as Tamoxifen have both antiestrogenic and estrogenic properties, depending on the natural hormonal environment of the target patient [33]. Although menopausal status was not controlled for in the present study, the strong association between weight gain and currently taking medication, predominantly hormonal therapies, still poses a significant link that health professionals who are assisting women in long-term management of their breast cancer treatment side effects need to be aware of.
Exercise
Previous research has confirmed that exercise can reduce the burden of some side effects of breast cancer treatment such as fatigue and pain [6], as well as have positive effects on physical function, physical capacity, and muscular fitness, during and after cancer treatment [12–14]. Confirming our second hypothesis, women who were insufficiently active were more likely to experience a range of side effects, including shoulder limitations, muscular chest wall pain, weight gain, lymphedema, or breathlessness. Previous research has noted improvements in shoulder limitations, weight gain, and arm lymphedema among breast cancer patients who exercise [34–36], but no research could be located which directly considered the side effects of breathlessness or muscular chest wall pain.
Upper limb dysfunction including a reduced range of motion in the shoulder, muscle weakness, and pain and numbness are common postoperative complications for breast cancer patients [35, 37]. These dysfunctions not only impact on physical health, as breast cancer survivors with clinically defined arm/shoulder problems also have significantly poorer QOL than survivors without arm/shoulder pain [9]. A comprehensive Cochrane Review recently concluded that “exercise can result in significant and clinically meaningful improvements in shoulder ROM [range of motion] in women with breast cancer” [35]. As such, the result that shoulder limitations are less likely to occur among breast cancer survivors who were sufficiently active is not surprising.
Muscular chest wall pain was also significantly associated with not being sufficiently active. Pain as a result of breast cancer treatment is an ill-defined syndrome ranging from mild pain to significant nociceptive pain and neuromas [38, 39]. Upper-body pain is a commonly experienced breast cancer treatment side effect, and the extent of pain experienced is generally linked to more invasive surgery and aggressive radiation treatments [22, 37, 40]. Although evidence is limited, commonly used clinical approaches to upper-body morbidities such as muscular chest wall pain include gentle exercises, which promote normal muscular recruitment patterns and enhance tissue extensibility [37]. Therefore, it is postulated that women who sufficiently exercise, and particularly promote controlled use of pectoralis, serratus anterior, and latissimus dorsi musculature, would also be less likely to experience muscular chest wall pain.
The present study also found weight gain was significantly related to not being sufficiently active. For women undergoing breast cancer treatment, evidence suggests that weight gain occurs without concurrent gains in lean body mass and is not caused by overeating but rather is a result of reduced physical activity [34]. Previous research concluded that exercise is an effective intervention for managing or preventing weight gain in women undergoing breast cancer treatment [34], which is consistent with the current finding.
Arm lymphedema is caused by an accumulation of fluid in interstitial space and occurs in 10–25 % of women treated for breast cancer [2]. The risk of arm lymphedema is directly related to the extent of surgery, or radiation treatment or both [2], and it is regarded as a persistent or chronic condition [37]. Even when symptoms appear resolved, a patient remains at an increased risk of redeveloping lymphedema [37]. Traditionally, clinicians have been cautious with the prescription of exercise, particularly weight lifting, to women who may be at risk of developing arm lymphedema, as increases in resistance within the muscle, along with increased blood flow as experienced during exercise, may increase lymph production in the arm [37]. However, a recent randomized controlled trial concluded that weight lifting did not significantly affect arm lymphedema, but rather, resulted in a decreased incidence of exacerbations of lymphedema, reduced symptoms, and increased strength [36]. Other studies have also concluded no evidence of negative effects from upper-body exercise on the incidence of arm lymphedema, and slowly progressive resistance training is protective against lymphedema flare-ups among women at risk [14, 41]. These findings agree with the present study in that sufficiently active women were less likely to report arm lymphedema.
Finally, women who were sufficiently active were less likely to report breathlessness than their more sedentary counterparts. This may be linked to an improved or maintained state of cardio-respiratory fitness. We postulate that breast cancer treatment could itself impact upon a patient’s cardio-respiratory system or, alternatively, experiences of other treatment-related side effects, could lead to sedentary behaviors and consequential cardio-respiratory de-conditioning. Studies examining the effects of exercise during breast cancer treatment have concluded that exercise can have a positive influence on cardio-respiratory outcomes [12, 13, 42]. Similar to improvements in shoulder limitations, these effects go beyond exclusively physical benefits, with cardio-respiratory improvements having also been positively correlated with QOL scores in a breast cancer cohort [43].
Limitations and recommendations
Although a validated survey instrument was used, this study was limited in the use of self-reported data and by its cross-sectional design, and therefore, we cannot draw conclusions regarding causality. Furthermore, it was not possible to analyze side effects against chemotherapy or radiotherapy because almost all the women in the study had undergone some form of either chemotherapy or radiotherapy, making the split into groups for a binary logistic regression unfeasible. This also inhibited an in-depth separation of chemotherapy, radiation, and surgical treatments for analysis with respect to the specific side effects likely to be linked to these specific treatments. Future studies with a larger study population, which can draw meaningful sample sizes for exclusive treatment groups, would be required to achieve this type of analysis. Health status also provides insight into patient outcomes, and future studies should consider including this in analysis. The present study was also limited in a lack of menopausal status data for the participants. Considering the mean sample age was 53 years, it is likely some women were peri-/menopausal. Therefore, it is possible that side effect experiences such as weight gain or hot flushes were linked to natural menopause, rather than being treatment-induced menopausal symptoms. Finally, as most of the sample consisted of members of the BCNA Review and Survey group, these women may be more motivated to participate in research and were younger than the general Australian breast cancer population, which may limit the generalizability of the study results.
Strengths
Despite the aforementioned limitations, this study holds much merit as an investigation into how patient characteristics and exercise may be associated with self-reported side effects to breast cancer treatment. To our knowledge, this is the largest cross-sectional study on the side effects of breast cancer in an Australian population, and one of the most comprehensive lists of self-reported side effects of breast cancer published to date. The project engaged a multi-state and multi-center recruitment strategy, although it is acknowledged that it was limited to women who were part of a support system for their breast cancer. Despite this, the sample was closely matched to an Australian population in terms of location spread, health status, and physical activity levels. Finally, by using an online questionnaire, the study was able to randomize the list of side effects presented in each survey, thereby eliminating any list ordering biases, as well as limiting any potential transcription errors during analysis.
Conclusions
The objective of this research was to gain a better understanding of breast cancer treatment-related side effects through identifying their association with patient characteristics such as age, type of surgery, whether women were currently undergoing treatment, and exercise levels. Given that 7 out of 15 listed side effects were significantly associated with at least one patient characteristic, these characteristics may hold moderate value as potential indictors of a greater or lesser side effect experience and may therefore be useful when planning supportive care following breast cancer treatment. Targeting individuals who are at a high risk of developing breast cancer treatment side effects could help improve the focus of resources to those patients most likely to benefit [17]. However, patient characteristics such as age, surgery, and current treatment are not readily changeable and, while awareness of symptom experiences and high-risk groups may assist in better targeting clinical resources, deviations from required treatments are limited. On the other hand, exercise was associated with a lesser symptom experience for shoulder limitations, muscular chest wall pain, weight gain, lymphedema, and breathlessness. Combined with the growing body of knowledge regarding the positive effects of exercise on QOL and breast cancer survival, this finding supports the call for further research into the adherence to, and promotion of, physician-approved exercise for women living with a breast cancer diagnosis.
References
Janz NK, Mujahid M, Chung LK et al (2007) Symptom experience and quality of life of women following breast cancer treatment. J Women’s Health 16:1348–1361
Burstein HJ, Winer EP (2000) Primary care for survivors of breast cancer. New Engl J Med 343:1086–1094
Shapiro CL, Recht A (2001) Drug therapy—side effects of adjuvant treatment of breast cancer. New Engl J Med 344:1997–2008
Cella D, Fallowfield LJ (2008) Recognition and management of treatment-related side effects for breast cancer patients receiving adjuvant endocrine therapy. Breast Cancer Res Tr 107:167–180
Jim H, Andrykowski M, Munster P, Jacobsen P (2007) Physical symptoms/side effects during breast cancer treatment predict posttreatment distress. Ann Behavioral Med 34:200–208
Meeske K, Smith A, Alfano C et al (2007) Fatigue in breast cancer survivors two to five years post diagnosis: a HEAL Study report. Qual Life Res 16:947–960
Arndt V, Stegmaier C, Ziegler H, Brenner H (2006) A population-based study of the impact of specific symptoms on quality of life in women with breast cancer 1 year after diagnosis. Cancer 107:2496–2503
Hayes SC, Rye S, Battistutta D, DiSipio T, Newman B (2010) Upper-body morbidity following breast cancer treatment is common, may persist longer-term and adversely influences quality of life. Health Qual Life Out 8:92–98
Nesvold I, Reinertsen K, Fosså S, Dahl A (2010) The relation between arm/shoulder problems and quality of life in breast cancer survivors: a cross-sectional and longitudinal study. J Cancer Surviv 5(1):62–72
Buijs C, de Vries EGE, Mourits MJE, Willemse PHB (2008) The influence of endocrine treatments for breast cancer on health-related quality of life. Cancer Treat Rev 34:640–655
Atkins L, Fallowfield L (2006) Intentional and non-intentional non-adherence to medication amongst breast cancer patients. Eur J Cancer 42:2271–2276
McNeely ML, Campbell KL, Rowe BH, Klassen TP, Mackey JR, Courneya KS (2006) Effects of exercise on breast cancer patients and survivors: a systemic review and meta-analysis. Can Med Assoc J 175:34–41
Markes M, Brockow T, Resch KL (2006) Exercise for women receiving adjuvant therapy for breast cancer. Cochrane Db Syst Rev [serial online] 4. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD005001.pub2/full. Accessed May 5th 2012
Schmitz KH, Speck RM (2010) Risks and benefits of physical activity among breast cancer survivors who have completed treatment. Women’s Health 6:221–238
Carmichael AR, Daley AJ, Rea DW, Bowden SJ (2010) Physical activity and breast cancer outcome: a brief review of evidence, current practice and future direction. Eur J Surg Oncol 36:1139–1148
Barbaric M, Brooks E, Moore L, Cheifetz O (2010) Effects of physical activity on cancer survival: a systematic review. Physiother Can 62:25–34
Clough-Gorr KM, Ganz PA, Silliman RA (2010) Older breast cancer survivors: factors associated with self-reported symptoms of persistent lymphedema over 7 years of follow-up. Breast J 16:147–155
Servaes P, Verhagen C, Bleijenberg G (2002) Fatigue in cancer patients during and after treatment: prevalence, correlates and interventions. Eur J Cancer 38:27–43
Gho S, Steele J, Munro B (2010) Is bra discomfort a barrier to exercise for breast cancer patients? Support Care Cancer 18:735–741
Whitney P, Budd D (1996) Think-aloud protocols and the study of comprehension. Discourse Process 21:341–351
Global Physical Activity Questionaire (GPAQ). World Health Organisation. http://www.who.int/chp/steps/resources/GPAQ_Analysis_Guide.pdf. Accessed March 11, 2011
Warmuth MA, Bowen G, Prosnitz LR et al (1998) Complications of axillary lymph node dissection for carcinoma of the breast—a report based on a patient survey. Cancer 83:1362–1368
AIHW, Australia’s health. Australian Institute of Health and Welfare. Canberra: AIHW, 2010. Cat No. AUS 122
AIHW, CA, and AACR, Cancer survival and prevalence in Australia: cancers diagnosed from 1982 to 2004. Australian Institute of Health and Welfare, Cancer Australia & Australasian Association of Cancer Registries, 2008. Cancer Series no. 42: p. Cat. no. CAN 38
ABS, Physical Activity in Australia: A Snapshot, 2007–08. 2011, Australian Bureau of Statistics
Rabin EG, Heldt E, Hirakata VN, Fleck MP (2008) Quality of life predictors in breast cancer women. Eur J Oncol Nurs 12:53–57
Vance V, Mourtzakis M, McCargar L, Hanning R (2011) Weight gain in breast cancer survivors: prevalence, pattern and health consequences. Obes Rev 12:282–294
McInnes JA, Knobf MT (2001) Weight gain and quality of life in women treated with adjuvant chemotherapy for early-stage breast cancer. Oncol Nurs Forum 28:675–684
Su H et al (2010) Weight gain is associated with increased risk of hot flashes in breast cancer survivors on aromatase inhibitors. Breast Cancer Res Tr 124(1):205–211
Mom CH, Buijs C, Willemse PHB, Mourits MJE, de Vries EGE (2006) Hot flushes in breast cancer patients. Crit Rev Oncol Hemat 57:63–77
Savard M, Savard J, Quesnel C, Ivers H (2009) The influence of breast cancer treatment on the occurrence of hot flashes. J Pain Symptom Manag 37:687–697
Rock CL et al (1999) Factors associated with weight gain in women after diagnosis of breast cancer. J Am Diet Assoc 99(10):1212–1218
McInnes JA, Knobf MT (2001) Weight gain and quality of life in women treated with adjuvant chemotherapy for early-stage breast cancer. Oncol Nurs Forum 28(4):675–684
Demark-Wahnefried W, Peterson BL, Winer EP et al (2001) Changes in weight, body composition, and factors influencing energy balance among premenopausal breast cancer patients receiving adjuvant chemotherapy. J Clin Oncol 19:2381–2389
McNeely ML, Campbell K, Ospina M et al (2010) Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Db Syst Rev [serial online] 6. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD005211.pub2/full. Accessed May 10th 2012
Schmitz KH et al (2009) Weight lifting in women with breast-cancer-related lymphedema. New Engl J Med 361(7):664–673
Hayes SC, Johansson K, Stout NL et al (2012) Upper-body morbidity after breast cancer. Cancer 118:2237–2249
Jung BF et al (2003) Neuropathic pain following breast cancer surgery: proposed classification and research update. Pain 104(1–2):1–13
Wallace MS et al (1996) Pain after breast surgery: a survey of 282 women. Pain 66(2–3):195–205
Hack TF et al (1999) Physical and psychological morbidity after axillary lymph node dissection for breast cancer. J Clin Oncol 17(1):143–149
Chan DNS, Lui LYY, So WKW (2010) Effectiveness of exercise programmes on shoulder mobility and lymphoedema after axillary lymph node dissection for breast cancer: systematic review. J Adv Nurs 66(9):1902–1914
Schmitz KH et al (2005) Controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. Cancer Epidem Biomar 14(7):1588–1595
Tolentino GP, Battaglini CL, Araújo SS et al (2010) Cardiorespiratory fitness and quality-of-life analysis posttreatment in breast cancer survivors. J Psychosoc Oncol 28:381–398
Acknowledgments
This project was funded by the National Breast Cancer Foundation with the support of Cancer Australia. No other funding sources supported this work, and there are no financial disclosures from any of the authors. We also acknowledge the support of the BCNA and Cancer Councils of Victoria and Western Australia throughout the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gho, S.A., Steele, J.R., Jones, S.C. et al. Self-reported side effects of breast cancer treatment: a cross-sectional study of incidence, associations, and the influence of exercise. Cancer Causes Control 24, 517–528 (2013). https://doi.org/10.1007/s10552-012-0142-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-012-0142-4