Abstract
Objective
Internationally, there have recently been reports of declining incidence rates for breast cancer. Decreased use of hormone therapy and decreased use of mammography has been put forward as possible reasons for this decline. The aim of this study was to analyse breast cancer incidence trends in Denmark, and to evaluate if these trends could be explained by changes in use of hormone therapy and screening with mammography.
Method
Data was obtained from the Danish Cancer Register, the Danish Medicines Agency, the Danish National Board of Health and the organised screening programmes.
Results
Incidence had been decreasing since 2003 with an annual percent change (APC) of −0.40. The proportion of women treated with hormone therapy dropped from 11.9% in 2002 to 8.8% in 2008, with a 67% drop in the use of oestrogens and progestogens combined, during the same period.
Conclusion
Danish data show a slight decease in the incidence, and while showing a significant drop in hormone therapy use, these results are coherent with a comparatively low initial use of hormone therapy. Mammography use increased over the period, and hence does not explain the decrease in incidence, but might have caused an underestimate of the effect of decreased use of hormone therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer in women, with the highest incidence rates found in Northern America, Australia, Western and Northern Europe [1]. Incidence rates have been continuously increasing [2], until more recently, when there have been reports of decline [3–12]. Possible reasons for the lately reported declines have been examined and discussed, not without controversy. Marked drops in hormone therapy use have been put forward as a reason for the decline in breast cancer incidence [3–5, 8, 10, 11, 13–15], as have a possible decrease in use of screening mammography [9, 12, 16].
Hormone therapy use increased during the 1980s and/or 1990s in most industrialised countries, commonly used as oestrogens alone, or oestrogens and progestogens combined, and primarily prescribed for climacteric symptoms but also as a preventive measure for osteoporosis and cardiovascular disease. In 2002, the Women’s Health Initiative (WHI) reported findings from a large randomised controlled trial, showing an increase in risk of breast cancer in women using combined oestrogens and progestogens [17]. As a result, there has been a significant decline in use of hormone therapy in many countries [3, 11, 14, 18–21].
The primary aim with this study was to analyse breast cancer incidence trends in Denmark. The secondary aim was to evaluate if these trends could be explained by changes in the use of hormone therapy and mammography.
Materials and methods
Data on breast cancer incidence have been obtained from the Danish Cancer Register. The register contains information about all cancer cases and other related diseases in Denmark, diagnosed since 1943. The Danish Cancer Register is nowadays based on reports from hospital doctors via The National Patient Register, and from general practitioners and specialists through the National Board of Health’s electronic reporting system.
Cancer incidence reported to the Danish Cancer Register was until 1978 classified according to the International Classification of Disease no. 7 (ICD-7), from 1978 until 2004 according to the International Classification of Disease for Oncology no. 1 (ICDO-1), and there after according to ICDO-3. The Danish Board of Health has reclassified all cases to ICD-10. This study includes breast cancer, C50 and carcinoma in situ, D05 from 1978 to 2007. Incidence rates have been age-standardised to the Danish population in 2000 (DK-2000).
Linear regressions and annual percent change (APC) in breast cancer incidence have been calculated with joinpoint regression (Joinpoint Regression Programme 3.3.1) with a 95% confidence interval (CI).
Data on hormone use, available from 1997 to 2008, were obtained from the Danish Medicines Agency, which includes data on all sold prescription drugs in Denmark. Anatomical therapeutic chemical (ATC) groups G03C (oestrogens), G03D (progestogens), G03F (oestrogens and progestogens combined), G03HB01 (cyproteron and oestrogen) and G03XC01 (raloxifen) were included in the analysis. Anatomical Therapeutic Chemical classification is an international drug classification system for drug utilisation research. Data were reported as (a) number of women treated per 1,000 women and type of hormone therapy and (b) total number of women treated with hormone therapy.
Data on mammography use were obtained and divided into data on screening mammography and data on clinical mammography. Data on screening mammography are registered separately from clinical mammography by the respective health services.
Screening mammography, targeting women 50–69 years old biennially, was in Denmark and first introduced in Copenhagen municipality in 1991, and was followed by programmes in Fyn County, 1993, Frederiksberg municipality, 1994 and the county of Bornholm in 2001. A limited amount of screening had also taken part in the counties of Vestsjælland and Aarhus, from 2004 and 2005, respectively. Hence, in Fig. 3, data from before 1991 only refer to clinical mammography, while data from 1991 onwards include both screening and clinical mammograms. Some estimates were made to achieve total coverage.
Data on use of screening mammography were provided by the organised screening programmes for Copenhagen municipality 1994–2005, county of Fyn 1993–2005, Frederiksberg municipality 1994–2005, and for the county of Bornholm 2001–2005. Apart from the abovementioned programmes, only the county of Vestsjælland (2004–2005) and the county of Aarhus (2003–2005) had some limited organised screening, and data for these counties were provided by the National Board of Health. Data for 2006–2007 were estimated based on population data and participation rates for the specific programmes.
Data on use of clinical mammography were compiled from the National Board of Health for the years 1983–1987 [22] and 1995 [23], and for the years 2003–2005 [24]. For 1983–1987 and 1995, data on number of women examined in both hospitals and private clinics were available. For 2003–2005, data on number of women examined with clinical mammography in hospital were estimated from number of breast examinations using a weight of 0.51, the weight derived from Jensen et al. (2006) [25]. Data on use of clinical mammography for 1990–1991 were compiled from Andreasen et al. (1994) [26], and for 2000 from Jensen et al. (2006) [25].
Separate data on number of women examined with clinical mammography in private clinics were available for the year 2000, and else estimated as equal to 13% of all women examined with clinical mammography, the proportion derived from Jensen et al. (2006) [25].
Results
A total of 96,304 women were diagnosed with invasive breast cancer from 1978 until 2007 and 4,164 women were diagnosed with breast carcinoma in situ (CIS) within the same period, Table 1.
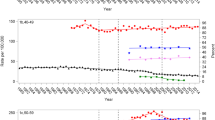
Breast cancer incidence rate
The age-standardised incidence rate of breast cancer increased from 103/100,000 women years to 137/100,000 women years in the period 1978–2007. The increase was fairly linear in the period 1978–2002, after which the rate decreased slightly. For women aged 40–74, the annual percent change (APC) was 1.53 (95% CI, 1.4; 1.7) from 1978 to 2003, after which the trend was negative, −0.40 (95% CI, −2.3; 1.5), Fig. 1. For age groups 40–44 and 45–49, the incidence rates have fluctuated over time, with large random variation. The 50–54-year-olds and the 55–59-year-olds had a negative APC onwards from 1997 and 2002, respectively. The 60–64-, 65–69- and 70–74-year-olds have had a positive APC through out the period, although decreasing from 1996 for the 60–64 year olds, Table 2.
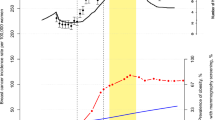
Use of hormone therapy
The proportion of women using hormone therapy was fairly stable until 2003 when it dropped from 11.1% in 2003 to 9.7% in 2004, and further to 9.0% in 2005 (p ≤ 0.000 for APC 1997–2008), Table 3. The number of women using oestrogens only (G03C) increased from 54/1,000 in 1997 to 59/1,000 in 2002, then dropped slightly and increased again to 59/1,000 in 2008. The number of women using progestogens and oestrogens in combination (G03F) dropped from 39/1,000 women in 2002 to 13/1,000 women in 2008. The number of women using progestin alone dropped from 14/1,000 in 1997 to 7/1,000 in 2008, while the total number of women using cyproterone and oestrogen combined or raloxifene has been relatively low and stable during the entire period, Fig. 2.
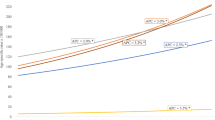
Use of mammography
The number of women annually examined with mammography increased from 39,000 in 1983 to close to 123,000 in 2007. These figures include both clinical mammograms and mammograms taken within the organised screening programmes, Fig. 3.
Comparative results in absolute figures
In absolute figures, the number of breast cancer incidences had been stable since 2002, with around 4,100 cases per year, the total amount of women using hormone therapy dropped from 324,000 in 2002 to 246,000 in 2005, while the use of mammography continued rising, Fig. 3.
Discussion
Data indicate a slight decrease in breast cancer incidence in Denmark from 2003 to 2007. The decrease occurred in the age group 40–59 years, but significantly only for the 45–49-year-olds. We found a significant drop in use of hormone therapy from 2003 to 2008, and this decrease was largely carried by the decrease in users of oestrogens and progestogens combined. The use of mammography had increased throughout the period.
The drop in hormone therapy use in 2003 is in line with the development in other countries after the publication of the Women’s Health Initiative data, and it can further be noted that the Danish Society of Obstetrics and Gynaecology (DSOG) published guidelines on April 2004 [27], which might have caused a further drop.
However, in 2002 only 11.9% of the female population were hormone therapy users, and by 2008, this figure was 8.8%. This means that Denmark has been a low-use country in comparison with, for example, USA with around 38% for women 50–74 in 1995 [28, 29], or France with around 30% for women 50–64 in 1998 [13].
From the USA, Ravdin et al. (2007) report a decline in breast cancer incidence between 2001 and 2004, in women ≥50 years of age, of 8.6% (95% CI, 6.8–10.4). The authors attribute this to be a consequence of a dramatic drop in hormone therapy use [10]. According to the results from a large study [4], the use of oestrogens and progestogens combined peaked in 1999 at 21.8% of women 45 years or older and had decreased to around 5% in 2006, which suggests that a decrease in the use of combined oestrogens and progestogens is associated with a decrease in breast cancer incidence. Similar results have been reported from Australia [3], where results for 2001–2003 showed a 6.7% decline in invasive breast cancer in women ≥50 years. Simultaneously, 21% of women 50 years or older reported being current hormone therapy users in 2001 while 11% of women 45 years or older reported being users in 2004–2005.
The Nordic countries have showed varied results, as reported by Hemminki et al. (2008). Results from Sweden show a significant decline in breast cancer incidence from 2002 to 2003, mainly in the age group 50–59, and a decline in sold hormone therapy Defined Daily Doses (DDDs) by 61% from 1998 to 2005. In Norway, breast cancer incidence levelled off, or slightly declined, from 2001 to 2002, while the sales dropped 51% from 1999 to 2005. In Finland, there was no drop in breast cancer incidence but a slight reduction of sold hormone therapy drugs [5]. It is notable that in amount of sold DDDs/1000 women/day, Finland, Iceland, Norway and Sweden sold, in 1999, almost the double amount of hormone therapy drugs than Denmark (data not shown), and while this difference had by 2003 substantially decreased for Iceland, Norway and Sweden, it had not for Finland. However, this result can probably be explained by studying the sales of oestrogens alone and combined oestrogens and progestogens separately, where Finland’s sales of oestrogens and progestogens combined had only been slightly higher than Denmark’s throughout the period, while this had not been the case for the other Nordic countries [30]. In line with the results from Denmark, this would indicate that a large decline in incidence is associated with a large absolute decrease in use of oestrogens and progestogens combined.
Analogous, Germany had in 1999 a similar use of hormone therapy as Denmark in terms of sold DDDs, with an approximate sale of 70 DDDs/1000 women/day. However, the use of oestrogens and progestogens combined was more than double that of oestrogens alone [14]. In 2006, the hormone therapy use had decreased to approximately 25 DDDs/1,000 women/day, with around 50% more oestrogens and progestogens combined than oestrogens alone. Katalinic et al. [6] found a correlation coefficient of 0.99 between breast cancer incidence and hormone therapy use in 2001 to 2005. Similar results have been reported from Belgium [11].
In the United Kingdom, the proportion of women aged 45–69 using any form of hormone therapy increased from 15 to 25% between 1992 and 2000. In 1992, approximately 9% used combined hormone therapy and 3% oestrogens alone. In 2000, these figures were around 12 and 8%, respectively, and the use of both preparations had then decreased to 4–5% each by 2006. Since 1999 the breast cancer incidence decreased with around 0.8% per year for the 50–59-year-olds, a small decline was also seen for the 60–64-year-olds, while there was still increasing incidence for the 65–69-year-olds. The latter phenomenon can possibly be explained by the extension of screening to this age group [8].
From northern Italy, Zanetti et al., [12] reported in 2008 an average yearly decline (1999 to 2003) in breast cancer incidence of 2.6%. Also here was the decrease concentrated to the age groups 50–69. However, even though the use of hormone therapy decreased in 2002 and 2003, the use was limited to start with, peaking at 15% of the female population in the 1990s, and the decline in breast cancer incidence was more likely a consequence of the prevalence peak caused by the onset of organised mammography screening.
Several authors have studied the possibility that a decline in use of mammography screening rather than hormone therapy could explain the changes in breast cancer incidence, but not come up with conclusive evidence to support that hypothesis [15, 31, 32]. In Denmark, there had been a steady increase in the use of mammography over the period; hence, this cannot explain the decrease in breast cancer incidence, but might have eliminated some effect of reduction of hormone therapy use.
In conclusion, we find a slight decrease in breast cancer incidence in Denmark. Hormone therapy use has dropped significantly, but was on a relatively low level to start with. The results from Denmark are coherent with evidence from other countries which indicate that if the use of hormone therapy, and then specifically oestrogens and progestogens combined, have been high, as in France, the USA or Germany, then a significant drop in use will cause a significant decline in breast cancer incidence, whereas the impact on incidence by decreased hormone therapy use will be small in low-use countries [5, 15, 33]. Increased use of examination with mammography might, however, have caused an underestimate of the effect on incidence by decreased use of hormone therapy.
References
GLOBOCAN 2002 Database Available from: URL:http://www-dep.iarc.fr/globocan/database.htm. Date accessed:10 Feb 2009
Cancer Incidence in Five Continents (CI5), Volume I-VIII Available from: URL:http://www-dep.iarc.fr/. Date accessed:10 Feb 2009
Canfell K, Banks E, Moa AM, Beral V (2008) Decrease in breast cancer incidence following a rapid fall in use of hormone replacement therapy in Australia. Med J Aust 188(11):641–644
Glass AG, Lacey JV Jr, Carreon JD, Hoover RN (2007) Breast cancer incidence, 1980–2006: combined roles of menopausal hormone therapy, screening mammography, and estrogen receptor status. J Natl Cancer Inst 99(15):1152–1161
Hemminki E, Kyyronen P, Pukkala E (2008) Postmenopausal hormone drugs and breast and colon cancer: nordic countries 1995–2005. Maturitas 61(4):299–304
Katalinic A, Rawal R (2008) Decline in breast cancer incidence after decrease in utilisation of hormone replacement therapy. Breast Cancer Res Treat 107(3):427–430
Kumle M (2008) Declining breast cancer incidence and decreased HRT use. Lancet 372(9639):608–610
Parkin DM (2009) Is the recent fall in incidence of post-menopausal breast cancer in UK related to changes in use of hormone replacement therapy? Eur J Cancer
Ponti A, Rosso S, Zanetti R, Ricceri F, Tomatis M, Segnan N (2007) Re: breast cancer incidence, 1980–2006: combined roles of menopausal hormone therapy, screening mammography, and estrogen receptor status. J Natl Cancer Inst 99(23):1817–1818
Ravdin PM, Cronin KA, Howlader N et al (2007) The decrease in breast-cancer incidence in 2003 in the United States. N Engl J Med 356(16):1670–1674
Vankrunkelsven P, Kellen E, Lousbergh D et al. (2009) Reduction in hormone replacement therapy use and declining breast cancer incidence in the Belgian province of Limburg. Breast Cancer Res Treat
Zanetti R, Ponti A, Rosso S, Ricceri F, Pitarella S, Segnan N (2008) The beginning of a decline in breast cancer incidence in Italy? Tumori 94(3):293–296
Allemand H, Seradour B, Weill A, Ricordeau P (2008) Decline in breast cancer incidence in 2005 and 2006 in France: a paradoxical trend. Bull Cancer 95(1):11–15
Katalinic A, Lemmer A, Zawinell A, Rawal R, Waldmann A (2009) Trends in hormone therapy and breast cancer incidence—results from the German network of cancer registries. Pathobiology 76(2):90–97
Verkooijen HM, Koot VC, Fioretta G et al (2008) Hormone replacement therapy, mammography screening and changing age-specific incidence rates of breast cancer: an ecological study comparing two European populations. Breast Cancer Res Treat 107(3):389–395
Waller M, Moss S, Watson J, Møller H (2007) The effect of mammographic screening and hormone replacement therapy use on breast cancer incidence in England and Wales. Cancer Epidemiol Biomarkers Prev 16:2257–2261
Rossouw JE, Anderson GL, Prentice RL et al (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the women’s health initiative randomized controlled trial. JAMA 288(3):321–333
Clarke CA, Glaser SL, Uratsu CS, Selby JV, Kushi LH, Herrinton LJ (2006) Recent declines in hormone therapy utilization and breast cancer incidence: clinical and population-based evidence. J Clin Oncol 24(33):e49–e50
Kliewer EV, Demers AA, Nugent ZJ (2007) A decline in breast-cancer incidence. N Engl J Med 357(5):509–510
Lokkegaard E, Lidegaard O, Moller LN, Agger C, Andreasen AH, Jorgensen T (2007) Hormone replacement therapy in Denmark, 1995–2004. Acta Obstet Gynecol Scand 86(11):1342–1351
Watson J, Wise L, Green J (2007) Prescribing of hormone therapy for menopause, tibolone, bisphosphonates in women in the UK between 1991 and 2005. Eur J Clin Pharmacol 63(9):843–849
Mammografiudvalget (1989) Mammography screening: use and organisation (in Danish). Sundhedsstyrelsen, Copenhagen
Sundhedsstyrelsen (1997) Early diagnose and treatment of breast cancer. Status report (in Danish). Sundhedsstyrelsen, Copenhagen
National Board of Health, Radiologic exams Available from: URL:http://www.sst.dk/Indberetning%20og%20statistik/Sundhedsdata/Download_sundhedsstatistik/Behandling_ved_sygehuse/DSNM.aspx. Date accessed: 3 May 2010
Jensen A, Vejborg I, Severinsen N et al (2006) Performance of clinical mammography: a nationwide study from Denmark. Int J Cancer 119(1):183–191
Andreasen AH, Andersen KW, Madsen M, Mouridsen HT, Olesen KP, Lynge E (1994) [Mammographic examinations in Denmark, 1990–1991] (in Danish). Ugeskr Laeger 156:6517–6520
Hormones and breast cancer (in Danish) Available from: URL:http://www.lidegaard.dk/Instrukser%20mv/HT-BC%2004-08-13.pdf
Hersh AL, Stefanick ML, Stafford RS (2004) National use of postmenopausal hormone therapy: annual trends and response to recent evidence. JAMA 291(1):47–53
Keating NL, Cleary PD, Rossi AS, Zaslavsky AM, Ayanian JZ (1999) Use of hormone replacement therapy by postmenopausal women in the United States. Ann Intern Med 130(7):545–553
Medicines Consumption in the Nordic Countries 1999-2003. (2004) Nordic Medico Statistical Committee, Copenhagen
Clarke CA, Glaser SL (2007) Declines in breast cancer after the WHI: apparent impact of hormone therapy. Cancer Causes Control 18(8):847–852
Berry DA, Ravdin PM (2007) Breast cancer trends: a marriage between clinical trial evidence and epidemiology. J Natl Cancer Inst 99(15):1139–1141
Soerjomataram I, Coebergh JW, Louwman MW, Visser O, Van Leeuwen FE (2007) Does the decrease in hormone replacement therapy also affect breast cancer risk in the Netherlands? J Clin Oncol 25(31):5038–5039
Acknowledgments
The author wishes to thank Laura Elisabeth Espenhain for providing professional assistance with the data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
von Euler-Chelpin, M. Breast cancer incidence and use of hormone therapy in Denmark 1978–2007. Cancer Causes Control 22, 181–187 (2011). https://doi.org/10.1007/s10552-010-9685-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9685-4