Abstract
Purpose
Over the past half century, the annual age-adjusted breast cancer incidence in the USA has fluctuated, potentially influenced by changes in mammography screening, obesity, and menopausal hormone therapy. As the relative contributions of these factors on breast cancer incidence have not been resolved, we assembled reliable sources of year-to-year changes in mammography, obesity, and hormone therapy to graphically display their relationship to breast cancer incidence through 50 years.
Methods
Year-to-year trends were assembled: for mammography from the Center for Disease Control National Health Interviews; for hormone therapy from the Collaborative Group on Hormonal Factors in Breast Cancer report; for obesity from the NCD (Non-Communicable Diseases) Risk Factor Collaboration; and for breast cancer for US women 50–64 years of age from Surveillance, Epidemiology, and End Results (SEER) registry findings.
Results
Increases in age-adjusted breast cancer incidence trend from about 1982 to 2002 track both mammography and hormone therapy use but not obesity. However, the sudden decrease in breast cancer incidence in 2003, subsequently sustained at a lower incidence level, only tracks the parallel reduction in hormone therapy use.
Conclusion
The sustained reduction in hormone therapy use from 2003 provides a plausible explanation for most of the lower breast cancer incidence seen in US postmenopausal women during the last two decades. The strong observational study obesity association with higher breast cancer risk is not reflected in breast cancer incidence trends.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Purpose
Over the past half century, breast cancer incidence in the USA has undergone considerable fluctuation, potentially influenced by implementation of mammography screening [1], increasing obesity [2], and changes in hormone therapy use [3, 4]. The relative contributions of these factors to breast cancer incidence have not been resolved. As breast cancer is the most common cancer in US women [5], clarification of these relationships has implications for future clinical and health policy decisions.
Methods
Annual breast cancer incidence trends (1975–2015) for US women 50–64 years of age were assembled from nine of the national cancer institute’s surveillance, epidemiology, and end results (SEER) registries. Annual incidence rates were age adjusted to the US standard population in 2000 (19 age groups; Census P25-1130 series) and were adjusted for reporting delays. Trends in mammography among women aged 50–64 years were from Table 33 [1] mammography use among women aged ≥ 50, from the center for disease control national health interview survey, and conducted 15 times between 1987 and 2018 combined with estimates of 0% through 1980; before mammographic screening was generally available [1]. Trends in hormone therapy use were based on findings from the collaborative group on hormonal factors in breast cancer report [6]. Annual obesity prevalence estimates (BMI ≥ 30 kg/m2) were from the non-communicable diseases (NCD) Risk Factor Collaboration, a global network providing data on risk factors for diseases including obesity trends from 1975 to 2016 from 3,300 population-based studies with nearly 200 million participants [7].
Results
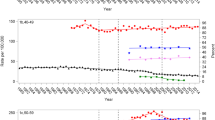
Findings regarding the annual breast cancer incidence by trends in hormone therapy use, mammography screening, and obesity as backdrop are depicted in Fig. 1. Visual inspection of the year-to-year trend in age-adjusted annual breast cancer incidence indicates a modest reduction in breast cancer incidence beginning in 1975, coincident with reduced hormone therapy use (Fig. 1) following the estrogen-alone association with higher endometrial cancer incidence [8]. Around 1982, a sustained 20-year increase in breast cancer incidence began, coincident with the transitional phase of mammogram use, shortly followed by wide-scale implementation of mammogram screening beginning around 1992 [9].
Annual incidence of breast cancer using trends in hormone therapy use, mammography screening, and obesity as a backdrop. Incident breast cancer rates (95% CI; dot whiskers) among women 50 − 64 years old and number of menopausal hormone therapy users in the U.S.A. (black line) are shown over time during distinct phases of mammographic screening (pre-screening, transitional, screening) as indicated by the dotted vertical lines and quantified by mammography rates (red-connected dots), during which time obesity rates (blue line) steadily increased
The year-to-year, age-adjusted increase in breast cancer incidence peaked around 1999 as mammography screening continued at a high level which has largely persisted, with modest decrease, to current time [1]. After presentation of findings in 2002 [10] and 2003 [11] from the Women’s Health Initiative (WHI) randomized trial, where estrogen plus progestin increased breast cancer incidence and impaired breast cancer detection, a substantial and sustained decrease in menopausal hormone therapy use was seen [3, 6].
Subsequently, the first decrease in breast cancer incidence in two decades emerged for women ≥ 50 years old and was attributed to reduced hormone therapy use [4], a controversial hypothesis, corroborated with both longer follow-up of the WHI trial (n = 16,608) comparing estrogen plus progestin to placebo influence on breast cancer incidence and a comparable observational cohort of WHI women (n = 41,449), consisting of participants that reported no use of menopausal hormone therapy and those that reported use of estrogen plus progestin at baseline. All trial participants were instructed to immediately stop taking study pills (active or placebo) in a letter coincident with the publication of the trial results on July 8, 2002 [10]. Subsequently, a sudden decrease in breast cancer incidence was seen only in the combined hormone therapy group and not in the placebo group [12]. Similar patterns were also observed for the observational cohort [12]. Lower incidence in the U.S.A., beginning in 2003, has been largely maintained through 2020 at levels last seen in 1993 [5, 6], despite continued high mammography participation. While obesity prevalence had year-to-year increases over this nearly five-decade period, increasing obesity did not track changes in breast cancer incidence (Fig. 1).
Discussion
There have been substantial changes in year-to-year age-adjusted breast cancer incidence rates for women 50 to 65 years of age over the past 50 years. The introduction and increasing use of mammography track the incident breast cancer rate from the transitional phase of mammography introduction in the mid-1980s through 2002. However, the subsequent continued high mammogram adherence rate does not track the substantial decline in breast cancer seen beginning in 2003. Menopausal hormone therapy use does track the modest decline in breast cancer incident rates seen from about 1975 to 1980 and tracts the sudden, substantial decline, and the maintained lower breast cancer incidence seen beginning in 2003 and maintained subsequently. The year-to-year increase in obesity prevalence seen from 1975 does not appear related to major changes in breast cancer incidence rates.
The decades long increase in breast cancer incidence seen with estrogen plus progestin use [13] likely were mediated by a progestin-induced breast epithelium stem cell pool increase, resulting in a persistent cell population at higher breast cancer risk [14]. Thus, the sustained lower breast cancer incidence in the US population seen since 2003 could be related to fewer women who would otherwise initiate estrogen plus progestin and subsequently be at long-term, higher breast cancer risk. By one estimate, in comparison to 2002, there have been 126,000 fewer breast cancers through 2012 in the USA than would have occurred without the WHI findings [15]. Because the lower age-adjusted breast cancer incidence has persisted for another decade, there were likely 10,000 fewer breast cancers yearly from 2003 through 2022 related to the WHI reports.
This report did not consider the influence of breast cancer prevention programs. However, despite the success of endocrine-targeting agents to reduce breast cancer incidence in randomized trials [16, 17], the uptake of incorporating these agents in breast cancer prevention programs in clinical practice has been limited [18]. Also not addressed were trends in breast cancer mortality. While age-adjusted breast cancer incidence was increasing from the mid-1980s to 2002, then suddenly decreased in 2003 to a lower incidence level, breast cancer mortality has been steadily decreasing In US women since about 1990 [5, 19] largely related to screening mammography early detection and adjuvant therapy advances including neoadjuvant therapy to define additional therapy needs and biomarkers to guide adjuvant endocrine and chemotherapy. Thus, trends in breast cancer incidence and breast cancer mortality are driven by different factors.
Study strengths include the use of reliable sources for changes in breast cancer incidence, mammography, hormone therapy, and obesity. Limitations relate to visual rather than statistical comparisons, across population-level summaries, for associations of trends in mammography, obesity, and hormone therapy to trends in breast cancer incidence.
Conclusion
Based on consideration of trends in mammography, obesity, and menopausal hormone therapy, the sustained reduction in hormone therapy use beginning in 2003 provides a plausible explanation for most of the lower age-adjusted breast cancer incidence seen in US postmenopausal women during the last two decades. The strong observational study association of obesity with higher breast cancer risk is not reflected in population trends.
Data availability
All the data are available from the sources cited in the manuscript.
References
(US) NCfHS: Table 33, Use of mammography among women aged 40 and over, byselected characteristics: United States, selected years 1987–2018, in Health US, 2019 [Internet] (ed). Hyattsville (MD), 2019
Neuhouser ML, Aragaki AK, Prentice RL et al (2015) Overweight, Obesity, and Postmenopausal Invasive Breast Cancer Risk: A Secondary Analysis of the Women’s Health Initiative Randomized Clinical Trials. JAMA Oncol 1:611–621
Hersh AL, Stefanick ML, Stafford RS (2004) National use of postmenopausal hormone therapy: annual trends and response to recent evidence. JAMA 291:47–53
Ravdin PM, Cronin KA, Howlader N et al (2007) The decrease in breast-cancer incidence in 2003 in the United States. N Engl J Med 356:1670–1674
Siegel RL, Miller KD, Fuchs HE et al (2022) Cancer statistics, 2022. CA Cancer J Clin 72:7–33
Collaborative Group on Hormonal Factors in Breast Cancer (2019) Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Lancet 394:1159–1168
Worldwide trends in body-mass index (2017) underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390:2627–2642
Smith DC, Prentice R, Thompson DJ et al (1975) Association of exogenous estrogen and endometrial carcinoma. N Engl J Med 293:1164–1167
Verdial FC, Etzioni R, Duggan C et al (2017) Demographic changes in breast cancer incidence, stage at diagnosis and age associated with population-based mammographic screening. J Surg Oncol 115:517–522
Rossouw JE, Anderson GL, Prentice RL et al (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA 288:321–333
Chlebowski RT, Hendrix SL, Langer RD et al (2003) Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative Randomized Trial. JAMA 289:3243–3253
Chlebowski RT, Kuller LH, Prentice RL et al (2009) Breast cancer after use of estrogen plus progestin in postmenopausal women. N Engl J Med 360:573–587
Chlebowski RT, Anderson GL, Aragaki AK et al (2020) Association of Menopausal Hormone Therapy With Breast Cancer Incidence and Mortality During Long-term Follow-up of the Women’s Health Initiative Randomized Clinical Trials. JAMA 324:369–380
Joshi PA, Goodwin PJ, Khokha R (2015) Progesterone Exposure and Breast Cancer Risk: Understanding the Biological Roots. JAMA Oncol 1:283–285
Roth JA, Etzioni R, Waters TM et al (2014) Economic return from the Women’s Health Initiative estrogen plus progestin clinical trial: a modeling study. Ann Intern Med 160:594–602
Chlebowski RT, Col N, Winer EP et al (2002) American Society of Clinical Oncology technology assessment of pharmacologic interventions for breast cancer risk reduction including tamoxifen, raloxifene, and aromatase inhibition. J Clin Oncol 20:3328–3343
Cuzick J, Sestak I, Bonanni B et al (2013) Selective oestrogen receptor modulators in prevention of breast cancer: an updated meta-analysis of individual participant data. Lancet 381:1827–1834
Chlebowski RT, Aragaki AK, Pan K (2021) Breast Cancer Prevention: Time for Change. JCO Oncol Pract 17:709–716
Giaquinto AN, Sung H, Miller KD et al (2022) Breast Cancer Statistics, 2022. CA Cancer J Clin 72:524–541
Acknowledgements
We acknowledge the commitment of the WHI investigators, staff, and the trial participants. Program Office: Jacques Roscoe, Shari Ludlum, Dale Burden, Joan McGowan, Leslie Ford, and Nancy Geller (National Heart, Lung, and Blood Institute, Bethesda, MD). Clinical Coordinating Center: Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kopperberg (Fred Hutchinson Cancer Research Center, Seattle, WA). Investigators and Academic Centers: JoAnn E. Manson (Brigham and Women’s Hospital, Harvard Medical School, Boston, MA); Barbara V. Howard (MedStar Health Research Institute/Howard University, Washington, DC); Marcia L. Stefanick (Stanford Prevention Research Center, Stanford, CA); Rebecca Jackson (The Ohio State University, Columbus, OH); Cynthia A. Thompson (University of Arizona, Tucson/Phoenix, AZ); Jean Wactawski-Wende (University at Buffalo, Buffalo, NY); Marian Limacher (University of Florida, Gainesville/Jacksonville, FL); Robert Wallace (University of Iowa, Iowa City/Davenport, IA); Lewis Kuller (University of Pittsburgh, Pittsburgh, PA); Rowan T. Chlebowski (The Lundquist Institute, Torrance, CA; and Sally Shumaker (Wake Forest University School of Medicine, Winston-Salem, NC). A full list of all the investigators who have contributed to WHI science can be retrieved at: https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf.
Funding
The development of this paper is partially supported by the National Cancer Institute grants R01 CA119171 and R01 CA10921. The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201600018C, HHSN268201600001C. Cancer Research Institute, R01 CA119171, Rowan Chlebowski, R01 CA10921, Rowan Chlebowski
Author information
Authors and Affiliations
Contributions
Both Rowan Chlebowski and Aaron Aragaki contributed to the study concept and design. Aaron Aragaki performed data collection. Both Rowan Chlebowski and Aaron Aragaki contributed to the first draft of the manuscript and both read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr Chlebowski has been a consultant or advisor and received personal fees from Novartis, AstraZeneca, and UpToDate. No other conflicts of Interest were reported.
Ethical approval
Not applicable, as all data used were from published sources.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chlebowski, R.T., Aragaki, A.K. Long-term breast cancer incidence trends by mammography, obesity, and menopausal hormone therapy. Breast Cancer Res Treat 203, 121–124 (2024). https://doi.org/10.1007/s10549-023-07113-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07113-9