Abstract
Objective
Epidemiologic studies have reported conflicting results relating alcohol intake to bladder cancer risk. A meta-analysis of cohort and case–control studies was conducted to pool the risk estimates of the association between alcohol intake and bladder cancer.
Methods
Eligible studies were retrieved via both computer searches and review of references. We analyzed abstracted data with random effects models to obtain the summary risk estimates. Dose–response meta-analysis was performed for studies reporting categorical risk estimates for a series of exposure levels.
Results
Nineteen studies met the inclusion criteria of the meta-analysis. No association with bladder cancer was observed in either overall alcohol intake group (OR = 1.00, 95% CI 0.89–1.10) or subgroups stratified by sex, study design, geographical region, or smoking status. However, in the analysis by specific beverages, both beer (OR = 0.86, 95% CI 0.76–0.96) and wine (OR = 0.85, 95% CI 0.71–1.00) consumption exhibited a negative dose–response relationship with bladder cancer.
Conclusion
The overall current literature on alcohol consumption and the risk of bladder cancer suggested no association, while the consumption of beer and wine was associated with reduced risk of bladder cancer. Further efforts should be made to confirm these findings and clarify the underlying biological mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol is a major correlate of health and disease and is estimated to account for 3.6% of all cancer cases and 6% of cancer death worldwide [1, 2]. Although alcohol is not known to be carcinogenic in animal experimentation, considerable evidence from epidemiologic studies suggests that increased alcohol is a risk factor for cancers of the upper alimentary tract, liver, colorectum, and female breast [3]. Modifying alcohol consumption could be part of a prevention strategy of cancer through lifestyle changes.
Bladder cancer is the fourth most common cancer in the USA, with an expected 71,000 newly diagnosed cases and 14,300 deaths [4] in 2009. Many epidemiologic studies support a positive association between bladder cancer and chemical or environmental exposures, such as cigarette smoking, aromatic amines and Schistosoma haematobium infestation [5]. However, the findings on the association between alcohol intake and the risk of bladder cancer are inconsistent. A meta-analysis conducted in 1999 suggested a weak elevated but insignificant risk of urinary tract cancer from alcohol consumption for men [6], while the risk for women and the influence of the amount and type of alcohol remained unclear because of limited data. There have been other reviews of this association, but they have not combined risk estimates for an overall estimate of the effect size [7, 8].
The purpose of the present study was to update and quantitatively assess the association between alcohol consumption and the risk of bladder cancer by summarizing the results of published cohort and case–control studies. We also sought to address the unresolved issue of whether this relationship differs across the specific alcoholic beverages.
Materials and methods
Literature research
We identified publications in MEDLINE database using PubMed, Web of Science and the Cochrane Library. “Alcohol” and “bladder cancer” were used as keywords in the free text words. The articles evaluating the relationship of urinary tract cancer and alcohol consumption were also retrieved, because the overwhelming majority of tumors occurred in the bladder, and the renal pelvis and ureter are covered by the same urothelium. The term bladder cancer was used as a synonym for these neoplasms. Additionally, we performed hand searches via cited references in the abstracted articles and previous reviews on alcohol and cancer. Each identified publication was reviewed and included in the analysis if all the following criteria were met: (1) case–control or cohort study published as an original article; (2) papers reported in English between 1980 and 2009 December; (3) findings expressed as odds ratio (OR) or relative risk (RR) and its 95% confidence intervals (95% CI) adjusted for at least age, sex and smoking, or sufficient information allowing us to compute them.
Data extraction
We extracted the name of the first author, the year of publication, the country in which the study was conducted, study design, sample size, anatomical site of the neoplasm, adjusted effects estimates, exposure assessment and adjusted covariates. Considering that bladder cancer is a rare disease, the RR was assumed approximately the same as OR, and the OR was used as the study outcome. Adjusted ORs were extracted directly from the original reports. If studies reported sex-stratified age- and smoking-adjusted ORs, we calculated the overall age-, smoking- and sex-adjusted OR by combining these estimates with the method of Mantel and Haenszel [9]. For studies that reported separate adjusted odds ratios for several consumption strata, we estimated the exposed versus non-exposed adjusted OR using the exposure-specific prevalence of the non-cases as weight [10].
Statistical analysis
We pooled data using the DerSimonian and Laird [11] random effects models, which consider both within-study and between-study variation. Subgroup analyses were performed according to sex (male or female), study design (cohort or case–control studies), the study location (USA/Canada, Europe or Asia), smoking status (non-smokers and smokers) and type of alcohol beverages (beer, wine, or spirits).
For the dose–response meta-analysis, we included studies considering at least 3 levels of alcohol consumption and providing the number of case patients and control subjects in each exposure category. We used the method proposed by Greenland [12] and Orsini [13] to back-calculate and pool the risk estimates. We converted all measures into gram alcohol per day on the widely used estimation that a standard drink contains 12 g of alcohol regardless of alcohol type unless it was defined in the study population or the geographical area. We assigned the level of alcohol consumption from each study to these categories based on the calculated midpoint of alcohol consumption. When the highest category was open-ended, we assumed the width of the interval to be the same as in the preceding category.
We quantified the extent of heterogeneity using Q test [11] and I 2 score [14] and statistical significance was considered while P < 0.05. Meta-regression analysis was used to explore the influence of study design, geographical region, alcohol assessment, and publication years in the heterogeneity. Publication bias was assessed using the tests of Egger [15] and Begg [16]. All statistical analyses were done with Stata Statistical Software, version 10.0.
Results
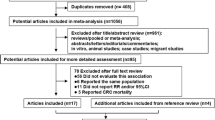
We identified 35 articles that examined the risk of bladder cancer with alcohol consumption published between 1980 and 2009 December. Upon closer examination, sixteen articles did not provide sufficient information to estimate a summary odds ratio and its 95% confidence intervals [17–22], or a summary odds ratio adjusted for at least age, sex and smoking [23–32]. The remaining 19 articles [33–51] were chosen for detailed review. Of the selected studies, six were cohort [38, 42, 43, 45, 50, 51], six were hospital-based case–control [34, 39, 41, 44, 46, 49], and seven population-based case–control studies [33, 35–37, 40, 47, 48] (Table 1). Eleven of these studies were conducted in the United States/Canada [34–38, 40, 45, 47, 48], while six were in Europe [33, 39, 41–44] and two in Asia [46, 49]. Thirteen articles reported the associations between consumption of specific alcoholic beverages (beer, wine or spirits) and the risk of bladder cancer [37, 38, 40–45, 47–51]. Information on alcohol consumption was obtained by interview, self-administered questionnaire or both techniques.
Among six cohort studies, five reported no significant association in drinkers as compared with nondrinkers [38, 43, 45, 50, 51], whereas one study found an increased risk for men but not in women [42]. Most case–control studies found no significant association between alcohol drinking and bladder cancer, whereas two studies reported significantly increased risks [33, 39], and one found inverse associations [47]. A study conducted by Hemelt et al. [49] provided odds ratios for three alcohol beverages but no data on overall alcohol intake.
Figure 1 plots the pooled risk estimates for overall alcohol intake by study design. When all these studies were analyzed together, we observed alcohol intake was not associated with bladder cancer risk (OR = 1.00, 95% CI 0.89–1.10) and the summary ORs were similar across study design and source of the controls in case–control studies. There was no evidence of heterogeneity in cohort and hospital-based case–control studies, but some evidence in population-based case–control studies.
In Table 2, we pooled the OR estimates by sex (men and women), geographical region (USA/Canada, Europe and Asia), and smoking status (smokers and non-smokers). The OR estimates from subgroup analysis varied little, showing alcohol consumption was not associated with the likelihood of bladder cancer when separately analyzed by sex, geographical regions or smoking status. In analyses by specific beverages (Fig. 2), we found a significantly decreased risk of bladder cancer for intake of beer (OR = 0.86, 95% CI 0.76–0.96) and wine (OR = 0.85, 95% CI 0.71–1.00), but no association with spirits (OR = 1.01, 95% CI 0.87–1.15). Most of the results are heterogeneous. There was no evidence of significant publication bias either with the Egger’s or Begg’s test in any subgroup.
Because the consumption of beer and wine was associated with reduced risk of bladder cancer, we further performed the dose–response analysis for these alcoholic beverages. The dose–response meta-analysis included seven studies [41, 43, 45, 47–49, 51] for beer and eight studies [41, 43–45, 47–49, 51] for wine. Figure 3 shows the dose–response relationship between risk of bladder cancer and alcohol consumption from beer and wine. An increase in alcohol consumption of 10 g/day from beer (approximately 300 ml per day) was statistically significantly associated with a 5.7% (95% CI 1.8, 9.4%, P heterogenity = 0.002). Similarly a 3.3% decrease risk of bladder cancer for a 10 g/day increase for alcohol consumption from wine (approximately 125 ml per day, 95% CI 0.9, 5.7%, P heterogenity = 0.02) was observed.
In meta-regression analysis, we explored the influence of publication year, geographical region, study design, and method of alcohol assessment in the heterogeneity. However, none of these above was identified as a possible source of heterogeneity among all the included studies.
We also performed sensitivity analyses by sequentially excluding one study in each turn to examine the influence of a single study on the overall estimate or in any strata. The results showed that none of the study could considerably affect the summary of risk estimates in our meta-analysis (data not shown).
Discussion
In this pooled analysis of published cohort and case–control studies, no significant association was observed for alcohol intake overall with bladder cancer. This finding is consistent with the results from the previous meta-analysis by Zeegers et al. [6]. However, our study has several strengths. All studies included in our meta-analysis provided OR estimates controlled for a common set of variables (age, sex and smoking) that are known to be related to bladder cancer, thereby underscoring the independence of association of alcohol consumption with bladder cancer. We included 10 studies published after 1999 that were not included in the previous meta-analysis. A completely novel finding of the present study was that we found support for a negative relationship between beer and wine consumption and the likelihood of bladder cancer, and an increase in alcohol consumption of 10 g ethanol per day from beer (approximately 300 ml per day) or wine (approximately 125 ml per day) was statistically significantly associated with a 5.7 or 3.3% decrease in risk.
The results of the studies included in this analysis were heterogeneous, likely reflecting differences among study populations, model selection, analytic methodology, exposure assessment. We conducted a meta-regression analysis to assess the effect of publication year, geographical region, study design, and alcohol assessment on the heterogeneity. However, none of the confounding factors could explain heterogeneity between the individual studies. Our results from subgroup analysis also could not demonstrate any stratified association. It’s been known for a while that smoking is the greatest risk factor for bladder cancer. Although all the risk estimates in this meta-analysis have been adjusted for smoking, how each study controlled for cigarette smoking is different (Table 1). The ORs from older studies may not be adjusted for smoking properly, reflecting that the ORs reported in older studies seems to be higher than those reported in recently published studies, even though publication year was not identified as a source of heterogeneity. Although we cannot reject the possibility that our estimates were distorted because of residual confounding, the overall current literature on alcohol consumption and the risk of bladder cancer suggests no association. Further research is required to elucidate the roles of genetic and environmental factors that may modify the alcohol–bladder cancer association.
The negative associations of bladder cancer with beer and wine, which have lower alcohol content, may attribute to certain ingredients rather than ethanol intake itself. Xanthohumol, the major prenylated flavonoid present in the hops and a common ingredient of beer, has gained considerable interest due to its potential cancer chemo-preventive effect [52]. In our previous study, a poly-phenol named Resveratrol, which is abundant in red wine, has been demonstrated to inhibit bladder cancer cells both in vitro and in vivo [53].
As a meta-analysis of previously published observational studies, our study has several limitations that need to be taken into account when considering its contributions. First, because we did not attempt to uncover unpublished observations and not include studies with insufficient information to estimate an adjusted OR, which could bring publication bias even though no significant evidence of publication bias was observed in Egger’s and Begg’s test. Second, both volume of alcohol consumption and patterns of drinking have been shown to influence alcohol-related burden of disease, while most of the included studies did not provided data on alcohol intake over time or life drinking patterns. Consequently, we did not have sufficient data to evaluate the risk of bladder cancer associated with these other dimensions of alcohol intake. Third, the limited number of studies and the heterogeneity in the dose–response meta-analysis could possibly result in inaccurate estimates.
In summary, this study applied a detailed meta-analytic approach for combining OR estimates from studies on the relationship between bladder cancer incidence and alcohol consumption. Overall, no association between alcohol consumption and bladder cancer was observed, even stratified by sex, study design, and geographical region, while beer and wine intake could decrease risk for bladder cancer in a dose–response manner. Future research to confirm these findings, and to determine the likely biological mechanism, is warranted.
References
Boffetta P, Hashibe M (2006) Alcohol and cancer. Lancet Oncol 7:149–156
Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M (2005) Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. Lancet 366:1784–1793
Poschl G, Seitz HK (2004) Alcohol and cancer. Alcohol Alcohol 39:155–165
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ (2009) Cancer statistics, 2009. CA Cancer J Clin 59:225–249
Murta-Nascimento C, Schmitz-Drager BJ, Zeegers MP et al (2007) Epidemiology of urinary bladder cancer: from tumor development to patient’s death. World J Urol 25:285–295
Zeegers MP, Tan FE, Verhagen AP, Weijenberg MP, van den Brandt PA (1999) Elevated risk of cancer of the urinary tract for alcohol drinkers: a meta-analysis. Cancer Causes Control 10:445–451
Zeegers MP, Kellen E, Buntinx F, van den Brandt PA (2004) The association between smoking, beverage consumption, diet and bladder cancer: a systematic literature review. World J Urol 21:392–401
Pelucchi C, La Vecchia C (2009) Alcohol, coffee, and bladder cancer risk: a review of epidemiological studies. Eur J Cancer Prev 18:62–68
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22:719–748
Tan FE, Zeegers MP (2001) An asymptotically unbiased estimator of exposed versus non-exposed odds ratio from reported dose-response data. Stat Methods Med Res 10:311–323
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135:1301–1309
Orsini N, Bellocco R, Greenland S (2006) Generalized least squares for trend estimation of summarized dose-response data. Stata J 6:40–57
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Akdas A, Kirkali Z, Bilir N (1990) Epidemiological case-control study on the etiology of bladder cancer in Turkey. Eur Urol 17:23–26
Kunze E, Claude J, Frentzel-Beyme R, Paczkowski K, Schneider G, Schubert H (1986) Association of cancer of the lower urinary tract with consumption of alcoholic beverages. A case-control study. Carcinogenesis 7:163–165
Yu Y, Hu J, Wang PP et al (1997) Risk factors for bladder cancer: a case-control study in northeast China. Eur J Cancer Prev 6:363–369
La Vecchia C, Negri E, Decarli A, D’Avanzo B, Liberati C, Franceschi S (1989) Dietary factors in the risk of bladder cancer. Nutr Cancer 12:93–101
Wynder EL, Dieck GS, Hall NE, Lahti H (1985) A case-control study of diesel exhaust exposure and bladder cancer. Environ Res 37:475–489
Claude J, Kunze E, Frentzel-Beyme R, Paczkowski K, Schneider J, Schubert H (1986) Life-style and occupational risk factors in cancer of the lower urinary tract. Am J Epidemiol 124:578–589
Probert JL, Persad RA, Greenwood RP, Gillatt DA, Smith PJ (1998) Epidemiology of transitional cell carcinoma of the bladder: profile of an urban population in the south-west of England. Br J Urol 82:660–666
Baena AV, Allam MF, Del Castillo AS et al (2006) Urinary bladder cancer risk factors in men: a Spanish case-control study. Eur J Cancer Prev 15:498–503
Demirel F, Cakan M, Yalcinkaya F, Topcuoglu M, Altug U (2008) The association between personal habits and bladder cancer in Turkey. Int Urol Nephrol 40:643–647
Najem GR, Louria DB, Seebode JJ et al (1982) Life time occupation, smoking, caffeine, saccharine, hair dyes and bladder carcinogenesis. Int J Epidemiol 11:212–217
Thomas DB, Uhl CN, Hartge P (1983) Bladder cancer and alcoholic beverage consumption. Am J Epidemiol 118:720–727
Bravo MP, Del Rey Calero J, Conde M (1987) Bladder cancer and the consumption of alcoholic beverages in Spain. Eur J Epidemiol 3:365–369
Iscovich J, Castelletto R, Esteve J et al (1987) Tobacco smoking, occupational exposure and bladder cancer in Argentina. Int J Cancer 40:734–740
Murata M, Takayama K, Choi BC, Pak AW (1996) A nested case-control study on alcohol drinking, tobacco smoking, and cancer. Cancer Detect Prev 20:557–565
Lu CM, Chung MC, Huang CH, Ko YC (2005) Interaction effect in bladder cancer between N-acetyltransferase 2 genotype and alcohol drinking. Urol Int 75:360–364
Momas I, Daures JP, Festy B, Bontoux J, Gremy F (1994) Relative importance of risk factors in bladder carcinogenesis: some new results about Mediterranean habits. Cancer Causes Control 5:326–332
Mommsen S, Aagaard J, Sell A (1983) An epidemiological study of bladder cancer in a predominantly rural district. Scand J Urol Nephrol 17:307–312
Brownson RC, Chang JC, Davis JR (1987) Occupation, smoking, and alcohol in the epidemiology of bladder cancer. Am J Public Health 77:1298–1300
Slattery ML, West DW, Robison LM (1988) Fluid intake and bladder cancer in Utah. Int J Cancer 42:17–22
Risch HA, Burch JD, Miller AB, Hill GB, Steele R, Howe GR (1988) Dietary factors and the incidence of cancer of the urinary bladder. Am J Epidemiol 127:1179–1191
Nomura A, Kolonel LN, Yoshizawa CN (1989) Smoking, alcohol, occupation, and hair dye use in cancer of the lower urinary tract. Am J Epidemiol 130:1159–1163
Chyou PH, Nomura AM, Stemmermann GN (1993) A prospective study of diet, smoking, and lower urinary tract cancer. Ann Epidemiol 3:211–216
Donato F, Boffetta P, Fazioli R, Aulenti V, Gelatti U, Porru S (1997) Bladder cancer, tobacco smoking, coffee and alcohol drinking in Brescia, northern Italy. Eur J Epidemiol 13:795–800
Bruemmer B, White E, Vaughan TL, Cheney CL (1997) Fluid intake and the incidence of bladder cancer among middle-aged men and women in a three-county area of western Washington. Nutr Cancer 29:163–168
Pohlabeln H, Jockel KH, Bolm-Audorff U (1999) Non-occupational risk factors for cancer of the lower urinary tract in Germany. Eur J Epidemiol 15:411–419
Zeegers MP, Volovics A, Dorant E, Goldbohm RA, van den Brandt PA (2001) Alcohol consumption and bladder cancer risk: results from The Netherlands Cohort Study. Am J Epidemiol 153:38–41
Geoffroy-Perez B, Cordier S (2001) Fluid consumption and the risk of bladder cancer: results of a multicenter case-control study. Int J Cancer 93:880–887
Pelucchi C, Negri E, Franceschi S, Talamini R, La Vecchia C (2002) Alcohol drinking and bladder cancer. J Clin Epidemiol 55:637–641
Djousse L, Schatzkin A, Chibnik LB, D’Agostino RB, Kreger BE, Ellison RC (2004) Alcohol consumption and the risk of bladder cancer in the Framingham Heart Study. J Natl Cancer Inst 96:1397–1400
Wakai K, Hirose K, Takezaki T et al (2004) Foods and beverages in relation to urothelial cancer: case-control study in Japan. Int J Urol 11:11–19
Jiang X, Castelao JE, Groshen S et al (2007) Alcohol consumption and risk of bladder cancer in Los Angeles County. Int J Cancer 121:839–845
Benedetti A, Parent ME, Siemiatycki J (2009) Lifetime consumption of alcoholic beverages and risk of 13 types of cancer in men: results from a case-control study in Montreal. Cancer Detect Prev 32:352–362
Hemelt M, Hu Z, Zhong Z et al (2009) Fluid intake and the risk of bladder cancer: results from the South and East China case-control study on bladder cancer. Int J Cancer (epub ahead of print)
Mills PK, Beeson WL, Phillips RL, Fraser GE (1991) Bladder cancer in a low risk population: results from the Adventist Health Study. Am J Epidemiol 133:230–239
Michaud DS, Spiegelman D, Clinton SK et al (1999) Fluid intake and the risk of bladder cancer in men. N Engl J Med 340:1390–1397
Gerhauser C (2005) Beer constituents as potential cancer chemopreventive agents. Eur J Cancer 41:1941–1954
Bai Y, Mao QQ, Qin J et al (2010) Resveratrol induces apoptosis and cell cycle arrest of human T24 bladder cancer cells in vitro and inhibits tumor growth in vivo. Cancer Sci 101:488–493
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mao, Q., Lin, Y., Zheng, X. et al. A meta-analysis of alcohol intake and risk of bladder cancer. Cancer Causes Control 21, 1843–1850 (2010). https://doi.org/10.1007/s10552-010-9611-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9611-9