Abstract
Although tobacco use has been recognized as one of the leading causes of cancer morbidity and mortality, a role of smoking in the occurrence of prostate cancer has not been established. However, evidence indicates that factors that influence the incidence of prostate cancer may differ from those that influence progression and fatality from the disease. Thus, we reviewed and summarized results from prospective cohort studies that assessed the relation between smoking and fatal prostate cancer risk, as well as epidemiological and clinical studies that focused on aggressive behavior in prostate cancer, such as poorer survival, advanced stage, or poorer differentiation at diagnosis. The majority of the prospective cohort studies showed that current smoking is associated with a moderate increase of ~30% in fatal prostate cancer risk compared to never/non-smokers. This association is likely to be an underestimate of the effect of smoking because most studies had a single assessment of smoking at baseline and long follow-up times, and the association was considerably stronger in some sub-groups of heaviest smokers, or when smoking was assessed in a relatively short period (within 10 years) prior to cancer mortality. Using aggressive behavior of prostate cancer as outcome, current smoking was associated with significantly elevated risk, ranging from around twofold to threefold or higher. Although alternative explanations, such as publication bias, residual confounding, screening bias, and the influence of smoking-related comorbidities cannot be ruled out entirely, these findings suggest that smoking is associated with aggressive behavior of prostate cancers or with a sub-group of rapidly progressing prostate cancer. Based on evidence presented in this review, cigarette smoking is likely to be a risk factor for prostate cancer progression and should be considered as a relevant exposure in prostate cancer research and prevention of mortality from this cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the most common cancer in men in the United States, excluding non-melanoma skin cancer [1]. The process of prostate carcinogenesis is characterized by a long latency of 20–40 years. Most prostate cancers remain symptomless for years, even though they are categorized as malignant histologically [2]. During the last decade, the routine use of serum prostate-specific antigen (PSA) screening for prostate cancer in some populations has led to early detection of the disease. However, based on recent evidence, PSA screening is unlikely to substantially reduce prostate cancer mortality [3, 4]. Due to the heterogeneous nature of this disease, a great challenge remains to differentiate those tumors that will become clinically significant and will lead, if left untreated, to death, and those that are relatively indolent.
Smoking has been identified as the most preventable cause of cancer morbidity and mortality. However, epidemiological evidence regarding the relation between smoking and prostate cancer incidence has been generally unsupportive [5, 6]. Hickey et al. [5] conducted a systematic review on this topic based on 23 prospective cohort studies, five nested case–control studies, one retrospective cohort study, and 36 case–control studies. The majority of the cohort studies, with the exception of two, found no association between smoking and prostate cancer incidence, and most case–control studies produced null results as well. These studies therefore provided strong evidence that smoking is not a relevant risk factor for prostate cancer. Indeed, the International Agency of Cancer Research does not consider prostate cancer to be tobacco related.
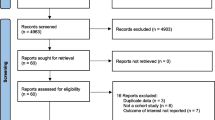
Recently, an increasing body of evidence suggests that risk factors for prostate cancer incidence may differ from those for progression of the disease, leading to mortality [7]. However, reviews of smoking and prostate cancer have generally not considered the influence of smoking on aggressive prostate cancer or cancer progression. Through Medline literature search, we identified all published prospective cohort studies that have examined smoking in relation to fatal prostate cancer risk. The results of these cohort studies are briefly presented in Table 1. We also searched for studies that have examined the association of smoking on prostate cancer survival, which are summarized in Table 2. In addition, we considered studies that examined aggressive behavior in prostate cancer defined by various methods, including poorer differentiation or advanced stage at diagnosis.
Studies examining cigarette smoking in relation to prostate cancer mortality
Table 1 shows results of studies for smoking during lifetime and within 10 years prior to death and risk of fatal prostate cancer. When death from prostate cancer was used as the outcome, in contrast to incident prostate cancer, the majority of the cohort studies yielded a positive association between current smoking and prostate cancer mortality [8–20]. This observed association is moderate, ~30% increase in risk for current smokers as a group, but may be higher in the sub-group of heaviest smokers and particularly for smoking 10 years prior to death. These studies are briefly summarized next.
Studies showing an overall association with smoking
Most of the studies showed an association with smoking regardless of the follow-up period. The Six-Prefecture Cohort Study in Japan [9] followed 122,261 men from 1966 to 1981; smoking status was assessed by a baseline questionnaire. A null association between smoking and prostate cancer mortality was yielded, but among those who consumed no less than 35 cigarettes daily, a threefold increased risk was observed.
The Lutheran Brotherhood Study [10], a cohort of men selected for mortality follow-up in 1966, used a baseline questionnaire to collect information on tobacco habits. The study found that, compared to non-smokers, the relative risk of fatal prostate cancer was significantly elevated among cigarette smokers, although there was no clear dose–response for amount of cigarettes smoked. In addition, users of smokeless tobacco (relative risk, 4.5; 95% confidence interval (CI), 2.1–9.7), and users of both cigarettes and smokeless tobacco (relative risk, 2.9; 95% CI, 1.3–6.5) had increased risks. Age, race, and dietary fat were controlled in the data analysis.
A cohort of 293,916 U.S. veterans [11], who responded to a questionnaire regarding the use of tobacco, was followed up for 26 years and 4,607 deaths from prostate cancer were recorded. This study provides the largest number of cases to date for evaluating the association of tobacco habits on prostate cancer mortality. Compared to never smokers, current cigarette smokers had a significant higher relative risk of 1.18 and a dose–response with number of cigarettes per day was observed (p for trend, <0.001). Ex-smokers also had an elevated relative risk of 1.13.
The longitudinal cardiovascular disease studies in Norway [12] reported mortality data in relation to smoking history in 13 years’ follow-up of 68,000 men. Only 32 deaths from prostate cancer were identified. An overall association was noted, but no dose–response was observed.
In a Swedish study [14], high-quality smoking information, including amount and duration of smoking, was collected in a large cohort of construction workers. Current smokers were shown to have a significantly elevated relative risk of 1.26 for prostate cancer mortality compared with never smokers. A statistically significant rising trend was found with increasing years of smoking among current smokers (p = 0.03) but not with increasing numbers of cigarettes smoked per day.
Another prospective mortality study done in men who were screened as part of the multiple risk factor intervention trial (MRFIT) [15] also reported a significant association between cigarette smoking status and fatal prostate cancer (relative risk, 1.31; p < 0.01). Elevated relative risks were found in all smoking quintiles (cigarettes per day), though a clear dose–response was not present.
The relation between smoking and the risk of fatal prostate cancer was examined in the Cancer Prevention Study II [16]. Smoking status was assessed in the baseline questionnaire. During 9 years of follow-up, 1,748 men died from prostate cancer. Current cigarette smoking was significantly associated with fatal prostate cancer, while past cigarette smoking was not. Although elevated relative risks were present in most smoking categories, a statistically significant trend was not established either with number of cigarettes smoked per day or with duration of years. Age, race, family history, dietary fat, and vasectomy were controlled in the data analysis.
The Health Professionals Follow-up Study [17] was unique in its up-to-date assessment of exposure status based on biennial questionnaires. Age, race, family history, dietary fat, and vasectomy were controlled in the data analysis. Current smokers were found to be at elevated risk of fatal prostate cancer, although it was not statistically significant. Past smokers were at significantly increased risk.
The Whitehall Study [20] was a prospective cohort in which 17,363 London-based government employees aged 40–69 years participated in a medical examination in the 1960s and were followed up for a maximum of 38 years. Increased risk of prostate cancer death was significantly associated with current smoking status at baseline. No association was present between duration of smoking and prostate cancer mortality. However, a 10-cigarette-per-day increment for current smokers conferred a hazard ratio of 1.12 (95% CI, 0.96–1.31), suggestive of a dose–response of smoking intensity for prostate cancer death.
Studies showing an overall association with smoking within 10 years of death
Four of the studies examined smoking within ~10 years prior to death from prostate cancer (Table 1). In all of these analyses, cigarette smoking was associated with an increased risk of fatal prostate cancer. In the Cancer Prevention Study II [16], which showed an increased risk overall had only 9 years of follow-up after the assessment of smoking; as described earlier, this study showed an association between smoking and prostate cancer mortality. In the cohort of 293,916 U.S. veterans [11], which showed a significant but moderate association overall (relative risk, 1.51), a considerably stronger association was observed within the first 8.5 years of follow-up (relative risk, 2.42) for >30 cigarettes per day.
In the Health Professionals Follow-up Study [17], recent smoking history was found to be associated with fatal prostate cancer; men who had quit more than 10 years before were no longer at elevated risk (relative risk, 1.04; 95% CI, 0.66–1.64). Total lifetime cigarette pack-years smoked was a risk factor for fatal prostate cancer (relative risk, 1.18; 95% CI, 1.01–1.37 for a 20 pack-year increment). However, when recent smoking history (the previous decade) was controlled for, the lifetime cigarette pack-years smoked was no longer statistically significant (relative risk, 1.07; 95% CI, 0.85–1.36), suggesting only relatively recent smoking history is etiologically relevant. A dose–response relation existed between total pack-years of cigarettes smoked over the prior 10 years and risk for fatal prostate cancer (Table 1; p for trend = 0.02).
The relationship between smoking and the risk of fatal prostate cancer was examined in two census cohorts in Washington County, MD [19]. The two censuses were conducted in 1963 and in 1975, in which 26,810 and 28,292 adult men provided information on their smoking habits and were followed up for 37 and 25 years respectively. No association between risk of prostate cancer and smoking was found in either cohort. However, in a sub-analysis using data from the first 10 years of follow-up, past and current cigarette smokers were found to have a greater risk of prostate cancer mortality in the 1963 census cohort; the elevations in risk of death from prostate cancer associated with past and current cigarette smoking were weaker in the 1975 census cohort, but consistent with twofold elevations in risk.
Studies not showing an overall association with smoking
The Physicians’ Health Study [18] enrolled 22,071 U.S. male physicians in 1982 and the average follow-up time was 12.5 years. Smoking habits were assessed through two questionnaires and a total of 113 fatal prostate cancer cases were recorded. The study did not yield a statistically significant association between cigarette smoking and fatal prostate cancer. No dose–response was found either with number of cigarettes smoked per day or with pack-years of smoking, which was used as a measure of cumulative smoking. Notably, the prevalence of cigarette smoking was low at baseline; ~10% of the cohort was composed of current smokers, while past smokers composed nearly 40%. The relative risk of fatal prostate cancer for past smokers was 1.34, suggestive of a positive association.
The British Physician Study reported its 40-year follow-up results on mortality in relation to smoking habits more than a decade ago [13]. A null association was found in current and ex-smokers for death from prostate cancer. A rising trend, statistically insignificant but compatible with results from the positive studies, was observed with increasing numbers of cigarettes smoked per day (mortality rates per 100,000 person-years, 54, 73, and 84 for 1–14, 15–24, and ≥25 cigarettes per day respectively). In a recent follow-up report of the study [27], the nature of these results did not change (mortality rates per 105 person-years, 66.7, 99.6, and 113.3 for 1–14, 15–24, and ≥25 cigarettes per day respectively).
A random sample of 25,129 Swedish men in 1963 were followed for cause-specific mortality through 1979 [8]. Past smokers at baseline did not have a higher death rate from prostate cancer than never smokers (age and residence-standardized relative death rate, 1.0). The dose of current smoking did not influence prostate cancer mortality either; the relative death rates for 1–7, 8–15, and >5 g any tobacco per day were 1.1, 0.8, and 0.9 respectively.
Studies examining cigarette smoking in relation to survival in men with prostate cancer
Some studies examined cigarette smoking at the time of diagnosis and survival from prostate cancer. Smokers who develop prostate cancer also tended to have poorer survival from the disease [21–26].The findings of these studies are presented in Table 2 and summarized briefly in the following paragraphs.
A study of patients with newly diagnosed prostate cancer [21] showed that smoking was associated with being diagnosed with stage D disease (odds ratio, 2.1; 95% CI, 1.3–4.3; p = 0.015). The 5-year tumor-specific mortality rate was greater among smokers than non-smokers with stage D2 disease (p < 0.05), or with non-stage A disease (p < 0.001) (Table 2).
A hospital cancer registry study investigated the effect of smoking history on survival of cancer patients [22]. The risk ratio of mortality associated with ever smoking was 1.98 (95% CI, 1.1–3.7) for non-drinking prostate cancer patients, after adjusting for age, gender, race, and grade. In addition, whites experienced a higher fatality rate of prostate cancer due to smoking (risk ratio, 1.53). Smoking was also associated with higher risk of regional (risk ratio, 3.07; 95% CI, 1.2–7.9) and distant disease at diagnosis (risk ratio, 1.29; 95% CI, 0.7–2.3).
One study in men with advanced prostate cancer on androgen deprivation therapy [23] showed that tobacco use correlated independently with shorter time to development of hormone refractory prostate cancer (p for log-rank test = 0.00002) and with poorer survival in a dose-dependent manner (p for log-rank test = 0.00001).
A study investigating the effect of smoking on biochemical outcome after radiotherapy [24] reported that Houston biochemical relapse rates projected at 5 years were significantly worse in current smokers when compared to non-smokers (odds ratio, 1.68; 95% CI, 1.11–2.56; p for log-rank test = 0.0019). The any cause-mortality was significantly worse (p for log-rank test = 0.009) among current smokers; the tumor-specific mortality was also worse for current smokers (relative risk = 2.7), though it was not statistically significant (p for log-rank test = 0.08).
A recently published study [25] conducted a retrospective review of 434 prostate cancer patients treated with radical radiotherapy. Smoking significantly increased the risk of metastatic disease in current smokers (hazard ratio, 5.24; 95% CI, 1.75–15.72), as well as in former smokers (hazard ratio, 2.90; 95% CI, 1.09–7.67). Increased risks, though not statistically significant, for biochemical failure (relative risk, 1.49; 95% CI, 0.88–2.40) and overall survival (relative risk, 1.72; 95% CI, 0.94–3.15) were also reported.
One study enrolled 752 prostate cancer patients aged 40–64 years and followed them for mortality [26]. Current smoking at the time of diagnosis was strongly associated with prostate cancer death (hazard ratio, 2.66; 95% CI, 1.10–6.43; p = 0.03). In addition, for men who had quit smoking for less than 10 years before cancer diagnosis, a non-significant increase in prostate cancer-specific mortality rate was observed (hazard ratio, 1.48; 95% CI, 0.50–4.37; p = 0.48). Notably, the risk of prostate cancer death increased with total pack-years smoked during the 10 years preceding diagnosis (hazard ratio, 2.70, 2.95, and 5.82 for 1–9, 10–14, and >14 pack-years respectively; p for trend = 0.0002).
Studies examining cigarette smoking in relation to aggressive behavior in prostate cancer
Several studies did not evaluate mortality from prostate cancer, but assessed indicators of aggressive behavior at the time of diagnosis [28–34]. In a medical records review study [28], 670 patients who had undergone radiation therapy and/or surgery from 1980 to 1990 for prostate cancer, tumor grade was evaluated consistently. A statistically significant difference was found in tumor grade between smokers and non-smokers. Among smokers, 15.0, 27.1, and 57.9% had well, moderate, and poorly differentiated tumor respectively; while in non-smokers, the distribution was 37.1% for well, 45.2% for moderate, and 17.7% for poorly differentiated tumor (p ≤ 0.00005). Smokers were also more likely to have stage D cancer compared to non-smokers (68.3 vs. 53.3%, p = 0.01).
In the Iowa 65+ Rural Health Study [29], smoking status, particularly current heavy smoking, was found to be associated with higher risk of prostate cancer. The associations were stronger for regional or distant disease at diagnosis [relative risk, 1.8, 4.7, and 8.7 for former smoking, current smoking (<1 pack/day), and current smoking (≥1 pack/day) respectively; p for trend = 0.004].
In a study of prostate cancer patients before age 55 years who had undergone radical prostatectomy, men with low-volume prostate tumors (≤0.5 ml) were compared to age- and ethnicity-matched men with clinically relevant prostate cancer (volume > 0.5 ml or extracapsular extension) to identify epidemiological determinants of clinically significant prostate cancer [30]. Patients with clinically relevant tumors were more likely to be current smokers, and to report more pack-years smoked, than patients with low-volume tumors. Among men with low-volume tumors, those with combined Gleason score of 7 (4+3) or higher were more likely to be current smokers compared to those with combined Gleason score of 7 (3+4) or lower.
A study evaluating the relationship between cancer stage at diagnosis and smoking history [31], also reported higher risks of regional (relative risk, 1.53; 95% CI, 1.17–2.02) and metastatic prostate cancer (relative risk, 1.83; 95% CI, 1.09–3.06) for current smokers when compared to never smokers.
A recent population-based case–control study of men with prostate cancer [32] reported that current smokers had an increased risk of prostate cancer (odds ratio, 1.4; 95% CI, 1.0–2.0) relative to non-smokers, and a dose–response relationship was observed with number of pack-years smoked (p for trend = 0.03). The odds ratio was 1.6 (95% CI 1.1–2.2) for men with >40 pack-years of smoking, but a stronger association was observed in men with more aggressive prostate cancer defined as regional or distant stage or Gleason score 8–10 (odds ratio, 2.0; 95% CI, 1.3–3.1. Smoking cessation was associated with a decline in risk (p for trend = 0.02) compared with current smokers.
In a retrospective medical record review study, the association of cigarette smoking with extraprostatic prostate cancer was assessed among patients who underwent radical retropubic prostatectomy [33]. Compared to never smokers former smokers had higher risk of extraprostatic disease at diagnosis (odds ratio, 1.49; 95% CI, 0.92–2.42); the risk of extraprostatic prostate cancer was the highest among current smokers (odds ratio, 3.85; 95% CI, 1.44–10.33). This risk also increased with the reported amount of pack-years smoked (odds ratio, 1.23, 2.29, 1.45, 3.01, and 3.66 for 1–10, 11–20, 21–30, 31–40, and >40 pack-years respectively; p for trend = 0.005).
In a study assessing the effect of cigarette smoking on biochemical outcome after permanent prostate brachytherapy, a trend (though not statistically significant) for more biochemical failure was demonstrated in current smokers [34], but death was not assessed.
Discussion
Smokers are not at appreciably higher risk of developing prostate cancer [5]. However, based on the evidence from studies examining aggressive or fatal prostate cancer summarized in this review, smokers appear to have more advanced disease at diagnosis, a worse prognosis, and a greater risk of fatal prostate cancer. Some evidence also suggests more poorly differentiated cancers, but this requires confirmation. An approximate 30% increase in risk of prostate cancer-specific mortality for current smokers, compared to non/never smokers, was observed in the majority of the prospective cohort studies. Furthermore, in the analyses that focused on a shorter time period after the smoking assessment (e.g., within 10 years) [11, 16, 17, 19] or used aggressive behavior of prostate cancer as outcome [21–23, 25, 29, 31–33], the elevation in risk associated with smoking was considerably higher, ranging from around twofold to threefold or higher. Most studies did not show a clear dose–response with smoking intensity, though the largest study comprising almost half of the total cases did [11]. Because all studies, except for one [17], were based on a single assessment of smoking followed by long follow-up periods, up to 40 years, and recent smoking closer to the time of diagnosis appears to be most relevant, the dose–response relationship could have been obscured by measurement error of the etiologically relevant time period in many studies. Of note, in some studies with long follow-up periods after a single assessment of smoking status, associations were considerably stronger and displayed a clear dose–response when the analysis was limited to the earlier follow-up period [11, 19]. Also, although most studies did not find past smokers to be at elevated risk, studies that isolated recent past quitters (within 10 years), did find an elevation in mortality [16, 17]. Furthermore, duration of smoking generally did not predict risk, further supporting that a relatively short time period before diagnosis is the critical time period for assessing the effect of smoking.
Potential causal and non-causal explanations of the association between smoking and aggressive prostate cancer are summarized in Table 3. Although the existence of publication bias cannot be ruled out entirely, this positive association between smoking and prostate cancer mortality is unlikely to be a chance finding. We identified 26 studies that examined some aspect of smoking and aggressive prostate cancer and almost all found support, or at least suggestive evidence, of a relationship. Among studies of prostate cancer mortality, the null findings are mostly in small studies with low power, and in studies with a single assessment of smoking and a long follow-up period. The three largest studies [ [11] (n = 4,607 deaths), [16] (n = 1,748 deaths), [15] (n = 826 deaths)], which comprised about two-thirds of all the fatal prostate cancer cases for all the studies combined, showed similar elevated risks of about 30% associated with current smoking at baseline. The British Physician Study did not report a positive relationship between smoking and prostate cancer mortality, which cannot be attributed to small number of deaths. However, the smoking status was assessed at baseline in this study and was not updated during 40 years of follow-up. During the course of the study, the smoking prevalence among the physician participants dropped dramatically [13]. Therefore, at the time of the analysis, a very limited number of recent smokers remained in the cohort, which likely severely reduced power to detect any effect of recent smoking.
Residual or uncontrolled confounding is also a potential alternative explanation, which cannot be ruled out definitively. However, it is unlikely to entirely account for the associations given the relatively strong magnitude of the association in some circumstances, and controlling for multiple factors in some of the cohorts did not change the results for smoking.
An alternative explanation for the positive association between smoking and aggressive prostate cancer may be screening bias: smokers may be less health-conscious than non-smokers; therefore, they may tend to avoid medical contacts, leading to a later diagnosis of the disease. The influence of potentially differential behaviors of seeking medical surveillance between smokers and non-smokers was examined in the Health Professional Follow-up Cohort [17]. No evidence suggesting substantial differential screening behaviors among smokers and non-smokers was found. Additionally, the study investigators also assessed the potential differential screening behaviors between smokers and non-smokers, which may result in a delay in diagnosis and treatment, and consequently the increase in mortality among smokers. In an analysis limited to men who had reported a negative digital rectal examination in the prior 2 years, the only common screening test at the time, even stronger associations were found between smoking and metastatic [relative risk (≥15 cigarettes per day), 4.2; 95% CI, 1.6, 10.9] and fatal prostate cancers [relative risk (≥15 cigarettes per day), 5.8; 95% CI, 1.9, 17.2]. This finding suggests that smoking is associated with a sub-group of rapidly progressing prostate cancer that are fatal shortly after diagnosis, which is a relatively uncommon scenario for prostate cancer. Further, the majority of studies with positive results were conducted before the PSA test was widely available. Results from recent randomized prostate cancer screening trials [3, 4] showed that prostate cancer-specific mortality rate did not differ significantly between the screening and the control groups, especially in the first 10 years of follow-up. Given the above evidence, it is unlikely that screening bias is entirely responsible for the positive association of smoking and prostate cancer mortality.
Another possible explanation of the findings is that smokers with prostate cancer die of smoking-related comorbidities, but the cause of death was attributed to prostate cancer. In the Health Professional Follow-up Study [17], study physicians, blinded to the exposure data, re-examined medical records to determine the accurate cause of death. Among men diagnosed with prostate cancer, smoking-related conditions (coronary heart disease, angina, cerebral vascular disease, other heart disease, and diabetes mellitus) predicted death from causes other than prostate cancer, but not death attributed to prostate cancer. Therefore, deaths attributed to prostate cancer were likely to be truly prostate cancer specific. Moreover, many studies of smoking and aggressive prostate cancer behavior found that smoking is associated with characteristics of prostate cancer (e.g., advanced stage or higher grade at diagnosis, or more biochemical or distant failure) that all predict fatal prostate cancer, suggesting that the link between smoking and prostate cancer mortality is prostate cancer mediated rather than through a generalized weakened health status.
The pathophysiological mechanisms underlying the positive association between smoking and aggressive prostate cancer are unclear. Cigarette smoking significantly increases plasma levels of total and free testosterone in men [35, 36]. Testosterone and its metabolite dihydrotestosterone (DHT) are known to play an important role in prostatic carcinogenesis. Moreover, cigarettes contain a variety of carcinogens, including N-nitroso compounds and cadmium, both of which can promote tumorigenesis in the prostate [37, 38]. In addition to the carcinogens in tobacco smoke, smoking is likely to affect the progression of prostate cancer through non-mutagenic effects. Angiogenesis, a process that is pivotal to cancer progression and metastasis, is a possible target of smoking. In laboratory experiments, nicotine has been shown to stimulate neovascularization, increase capillary growth, and accelerate tumor growth in association with enhanced vascularity [39–41]. A clinical study in Sweden [42] examined the association between smoking habits and fluid absorption during transurethral prostatic resection in 1,160 patients. Compared with patients who never smoked, past and current smokers are more prone to large-scale fluid absorption during the procedure with relative risks of 2.1 (95% CI, 1.1–4.3) and 2.8 (95% CI, 1.3–5.9) respectively. The investigator hypothesized that the increased risk of large-scale fluid absorption among smokers is likely due to increased blood vessel growth in the prostate gland. This hypothesis is further supported by the finding that plasma vascular endothelial growth factor level is higher in current smokers than in other patients [42].
Epigenetic mechanisms are also possible. In one study [43], current smoking status was significantly correlated with aberrant CpG hypermethylation of adenomatous polyposis coli (APC), glutathione S-transferase pi (GSTP1), and multidrug resistance one (MDR1) in prostate cancer cases (p = 0.03). Such aberrant methylation profiles were correlated with several prognostic markers including high tumor stages, high Gleason score, high preoperative PSA, and advanced pathological features.
From recent evidence provided by genetic association studies [44–50], it is likely that the effect of smoking on prostate cancer risk is modified by genetic polymorphisms in the xenobiotic metabolism pathway. Although the sample sizes of these studies were limited, the results for the glutathione S-transferase mu (GSTM1) polymorphism and smoking were fairly consistent: smokers with a GSTM1 null phenotype appear to have elevated risk for prostate cancer. Nock et al. [49] reported that this interaction was significant only in highly aggressive prostate cancer, suggesting this pathway may affect the progression of malignant lesions in the prostate. Additionally, the cytochrome p450 (CYP) family enzymes are also involved in hormone metabolism, particularly estrogen and testosterone [51]. Prostate cancer is a hormone-related malignancy; therefore, the occurrence, progression, and survival of this disease may be influenced through changes in hormone profiles associated with smoking [35, 36]. Therefore, genetic polymorphisms in these enzymes are likely to affect prostate cancer survival.
Interactions between smoking and environmental factors are likely to exist as well. The Alpha-Tocopherol, Beta Carotene Cancer Prevention study, a study of male smokers, reported a 34% reduction in prostate cancer incidence in men randomized to daily 50 mg alpha-tocopherol supplementation compared to those who received a placebo [52]. A further report from this study [53] showed the association was greater for prostate cancer mortality than incidence. Mortality from prostate cancer was 41% significantly lower among men who received alpha-tocopherol. The Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial [54] also reported that, among current and recent (quit within the previous 10 years) smokers, decreasing risks of advanced prostate cancer (Gleason score ≥ 7 or stage III or IV) were associated with increasing dose (for >400 IU/day vs. non-user: relative risk, 0.29; p for trend = 0.01), as well as prolonging duration (for ≥10 years vs. non-user: relative risk, 0.30; p for trend = 0.01) of vitamin E supplementation. Also, in a recent randomized controlled trial [55], supplementation with antioxidants (including 400 IU vitamin E) was found to decrease the risk of prostate cancer compared to the placebo group (relative risk, 0.6; 95% CI, 0.49–0.86). Subgroup analysis revealed that this decrease in risk was only significant among smokers. In the Health Professionals Follow-up Study, among current smokers and recent quitters, men who consumed at least 100 IU of supplemental vitamin E per day had a borderline statistically significant relative risk of 0.44 for metastatic or fatal prostate cancer compared with non-users [56]. Among non-smokers, no association with metastatic or fatal prostate cancer was found with vitamin E. These results suggest long-term vitamin E supplementation may offer smokers certain protection against aggressive prostate cancer. A recent randomized trial of vitamin E and prostate cancer did not show a benefit on total prostate cancer, but any effect on aggressive prostate cancer among smokers could not be examined [57].
In conclusion, although smoking is not likely to be an important risk factor for prostate cancer incidence, men who are smoking cigarettes within approximately a decade before diagnosis appear to have a worse prognosis and greater fatality from the disease. Although the reasons for this association are not clear, the overall evidence suggests that smoking directly contributes to a more aggressive prostate cancer phenotype, rather than increasing risk indirectly such as through delayed diagnosis. Thus, smoking should be considered as a relevant exposure in prostate cancer research and prevention of mortality from this cancer. To better understand the underlying mechanisms and the consequences of smoking on tissue molecular markers of aggressive behavior in prostate cancer, future studies using survival from prostate cancer as outcome are needed, in which detailed, preferably updated information on smoking habits and screening behavior should be collected. From a public health perspective, prevention of smoking or cessation even relatively late in life may have benefits in reducing mortality from prostate cancer.
References
Jemal A, Siegel R, Ward E et al (2008) Cancer statistics, 2008. CA Cancer J Clin 58:71–96
Assikis V, Brawley OW (2004) Chemoprevention in prostate cancer. Curr Probl Cancer 28:218–230
Andriole GL, Crawford ED, Grubb RLIII et al (2009) Mortality results from a randomized prostate-cancer screening trial. N Engl J Med 360:1310–1319
Schroder FH, Hugosson J, Roobol MJ et al (2009) Screening and prostate-cancer mortality in a randomized European study. N Engl J Med 360:1320–1328
Hickey K, Do KA, Green A (2001) Smoking and prostate cancer. Epidemiol Rev 23:115–125
Levi F, La Vecchia C (2001) Tobacco smoking and prostate cancer: time for an appraisal. Ann Oncol 12:733–738
Giovannucci E, Liu Y, Platz EA, Stampfer MJ, Willett WC (2007) Risk factors for prostate cancer incidence and progression in the health professionals follow-up study. Int J Cancer 121:1571–1578
Carstensen JM, Pershagen G, Eklund G (1987) Mortality in relation to cigarette and pipe smoking: 16 years’ observation of 25, 000 Swedish men. J Epidemiol Community Health 41:166–172
Akiba S, Hirayama T (1990) Cigarette smoking and cancer mortality risk in Japanese men and women–results from reanalysis of the six-prefecture cohort study data. Environ Health Perspect 87:19–26
Hsing AW, McLaughlin JK, Schuman LM et al (1990) Diet, tobacco use, and fatal prostate cancer: results from the Lutheran Brotherhood Cohort Study. Cancer Res 50:6836–6840
Hsing AW, McLaughlin JK, Hrubec Z, Blot WJ, Fraumeni JF Jr (1991) Tobacco use and prostate cancer: 26-year follow-up of US veterans. Am J Epidemiol 133:437–441
Tverdal A, Thelle D, Stensvold I, Leren P, Bjartveit K (1993) Mortality in relation to smoking history: 13 years’ follow-up of 68, 000 Norwegian men and women 35–49 years. J Clin Epidemiol 46:475–487
Doll R, Peto R, Wheatley K, Gray R, Sutherland I (1994) Mortality in relation to smoking: 40 years’ observations on male British doctors. BMJ 309:901–911
Adami HO, Bergstrom R, Engholm G et al (1996) A prospective study of smoking and risk of prostate cancer. Int J Cancer 67:764–768
Coughlin SS, Neaton JD, Sengupta A (1996) Cigarette smoking as a predictor of death from prostate cancer in 348, 874 men screened for the multiple risk factor intervention trial. Am J Epidemiol 143:1002–1006
Rodriguez C, Tatham LM, Thun MJ, Calle EE, Heath CW Jr (1997) Smoking and fatal prostate cancer in a large cohort of adult men. Am J Epidemiol 145:466–475
Giovannucci E, Rimm EB, Ascherio A et al (1999) Smoking and risk of total and fatal prostate cancer in United States health professionals. Cancer Epidemiol Biomark Prev 8:277–282
Lotufo PA, Lee IM, Ajani UA, Hennekens CH, Manson JE (2000) Cigarette smoking and risk of prostate cancer in the physicians’ health study (United States). Int J Cancer 87:141–144
Rohrmann S, Genkinger JM, Burke A et al (2007) Smoking and risk of fatal prostate cancer in a prospective U.S. study. Urology 69:721–725
Batty GD, Kivimaki M, Gray L, Smith GD, Marmot MG, Shipley MJ (2008) Cigarette smoking and site-specific cancer mortality: testing uncertain associations using extended follow-up of the original Whitehall study. Ann Oncol 19:996–1002
Daniell HW (1995) A worse prognosis for smokers with prostate cancer. J Urol 154:153–157
Yu GP, Ostroff JS, Zhang ZF, Tang J, Schantz SP (1997) Smoking history and cancer patient survival: a hospital cancer registry study. Cancer Detect Prev 21:497–509
Oefelein MG, Resnick MI (2004) Association of tobacco use with hormone refractory disease and survival of patients with prostate cancer. J Urol 171:2281–2284
Pickles T, Liu M, Berthelet E, Kim-Sing C, Kwan W, Tyldesley S (2004) The effect of smoking on outcome following external radiation for localized prostate cancer. J Urol 171:1543–1546
Pantarotto J, Malone S, Dahrouge S, Gallant V, Eapen L (2007) Smoking is associated with worse outcomes in patients with prostate cancer treated by radical radiotherapy. BJU Int 99:564–569
Gong Z, Agalliu I, Lin DW, Stanford JL, Kristal AR (2008) Cigarette smoking and prostate cancer-specific mortality following diagnosis in middle-aged men. Cancer Causes Control 19:25–31
Doll R, Peto R, Boreham J, Sutherland I (2005) Mortality from cancer in relation to smoking: 50 years observations on British doctors. Br J Cancer 92:426–429
Hussain F, Aziz H, Macchia R, Avitable M, Rotman M (1992) High grade adenocarcinoma of prostate in smokers of ethnic minority groups and Caribbean Island immigrants. Int J Radiat Oncol Biol Phys 24:451–461
Cerhan JR, Torner JC, Lynch CF et al (1997) Association of smoking, body mass, and physical activity with risk of prostate cancer in the Iowa 65+ Rural Health Study (United States). Cancer Causes Control 8:229–238
Spitz MR, Strom SS, Yamamura Y et al (2000) Epidemiologic determinants of clinically relevant prostate cancer. Int J Cancer 89:259–264
Kobrinsky NL, Klug MG, Hokanson PJ, Sjolander DE, Burd L (2003) Impact of smoking on cancer stage at diagnosis. J Clin Oncol 21:907–913
Plaskon LA, Penson DF, Vaughan TL, Stanford JL (2003) Cigarette smoking and risk of prostate cancer in middle-aged men. Cancer Epidemiol Biomark Prev 12:604–609
Roberts WW, Platz EA, Walsh PC (2003) Association of cigarette smoking with extraprostatic prostate cancer in young men. J Urol 169:512–516
Merrick GS, Butler WM, Wallner KE, Galbreath RW, Lief JH, Adamovich E (2004) Effect of cigarette smoking on biochemical outcome after permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys 58:1056–1062
Zmuda JM, Cauley JA, Kriska A, Glynn NW, Gutai JP, Kuller LH (1997) Longitudinal relation between endogenous testosterone and cardiovascular disease risk factors in middle-aged men. A 13-year follow-up of former multiple risk factor intervention trial participants. Am J Epidemiol 146:609–617
Dai WS, Gutai JP, Kuller LH, Cauley JA (1988) Cigarette smoking and serum sex hormones in men. Am J Epidemiol 128:796–805
Waalkes MP, Rehm S (1994) Cadmium and prostate cancer. J Toxicol Environ Health 43:251–269
Pour PM (1983) Prostatic cancer induced in MRC rats by N-nitrosobis(2-oxopropyl)-amine and N-nitrosobis(2-hydroxypropyl)amine. Carcinogenesis 4:49–55
Heeschen C, Jang JJ, Weis M et al (2001) Nicotine stimulates angiogenesis and promotes tumor growth and atherosclerosis. Nat Med 7:833–839
Jain RK (2001) Clearing the smoke on nicotine and angiogenesis. Nat Med 7:775–777
Villablanca AC (1998) Nicotine stimulates DNA synthesis and proliferation in vascular endothelial cells in vitro. J Appl Physiol 84:2089–2098
Hahn RG (2001) Smoking increases the risk of large scale fluid absorption during transurethral prostatic resection. J Urol 166:162–165
Enokida H, Shiina H, Urakami S et al (2006) Smoking influences aberrant CpG hypermethylation of multiple genes in human prostate carcinoma. Cancer 106:79–86
Yang J, Qian LX, Wu HF et al (2006) Genetic polymorphisms in the cytochrome P450 1A1 and 2E1 genes, smoking, drinking and prostate cancer susceptibility: a case–control study in a Han nationality population in Southern China. Int J Urol 13:773–780
Mao GE, Morris G, Lu QY et al (2004) Glutathione S-transferase P1 Ile105Val polymorphism, cigarette smoking and prostate cancer. Cancer Detect Prev 28:368–374
Quinones LA, Irarrazabal CE, Rojas CR et al (2006) Joint effect among p53, CYP1A1, GSTM1 polymorphism combinations and smoking on prostate cancer risk: an exploratory genotype-environment interaction study. Asian J Androl 8:349–355
Hamasaki T, Inatomi H, Katoh T et al (2003) N-acetyltransferase-2 gene polymorphism as a possible biomarker for prostate cancer in Japanese men. Int J Urol 10:167–173
Wadelius M, Autrup JL, Stubbins MJ et al (1999) Polymorphisms in NAT2, CYP2D6, CYP2C19 and GSTP1 and their association with prostate cancer. Pharmacogenetics 9:333–340
Nock NL, Liu X, Cicek MS et al (2006) Polymorphisms in polycyclic aromatic hydrocarbon metabolism and conjugation genes, interactions with smoking and prostate cancer risk. Cancer Epidemiol Biomark Prev 15:756–761
Kelada SN, Kardia SL, Walker AH, Wein AJ, Malkowicz SB, Rebbeck TR (2000) The glutathione S-transferase-mu and -theta genotypes in the etiology of prostate cancer: genotype-environment interactions with smoking. Cancer Epidemiol Biomark Prev 9:1329–1334
Agundez JA (2004) Cytochrome P450 gene polymorphism and cancer. Curr Drug Metab 5:211–224
Anonymous (1994) The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. The Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group. N Engl J Med 330:1029–1035
Heinonen OP, Albanes D, Virtamo J et al (1998) Prostate cancer and supplementation with alpha-tocopherol and beta-carotene: incidence and mortality in a controlled trial. J Natl Cancer Inst 90:440–446
Kirsh VA, Hayes RB, Mayne ST et al (2006) Supplemental and dietary vitamin E, beta-carotene, and vitamin C intakes and prostate cancer risk. J Natl Cancer Inst 98:245–254
Johnson AR, Munoz A, Gottlieb JL, Jarrard DF (2007) High dose zinc increases hospital admissions due to genitourinary complications. J Urol 177:639–643
Chan JM, Stampfer MJ, Ma J, Rimm EB, Willett WC, Giovannucci EL (1999) Supplemental vitamin E intake and prostate cancer risk in a large cohort of men in the United States. Cancer Epidemiol Biomark Prev 8:893–899
Lippman SM, Klein EA, Goodman PJ et al (2009) Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the selenium and vitamin E cancer prevention trial (SELECT). JAMA 301:39–51
Acknowledgments
This project was funded by E.G.’s Research and Teaching Funds from the Department of Nutrition at the Harvard School of Public Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zu, K., Giovannucci, E. Smoking and aggressive prostate cancer: a review of the epidemiologic evidence. Cancer Causes Control 20, 1799–1810 (2009). https://doi.org/10.1007/s10552-009-9387-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-009-9387-y